Radiographic Sagittal Tibio-Talar Offset in Ankle Arthrodesis—Accuracy and Reliability of Measurements
Abstract
1. Introduction
2. Materials and Methods
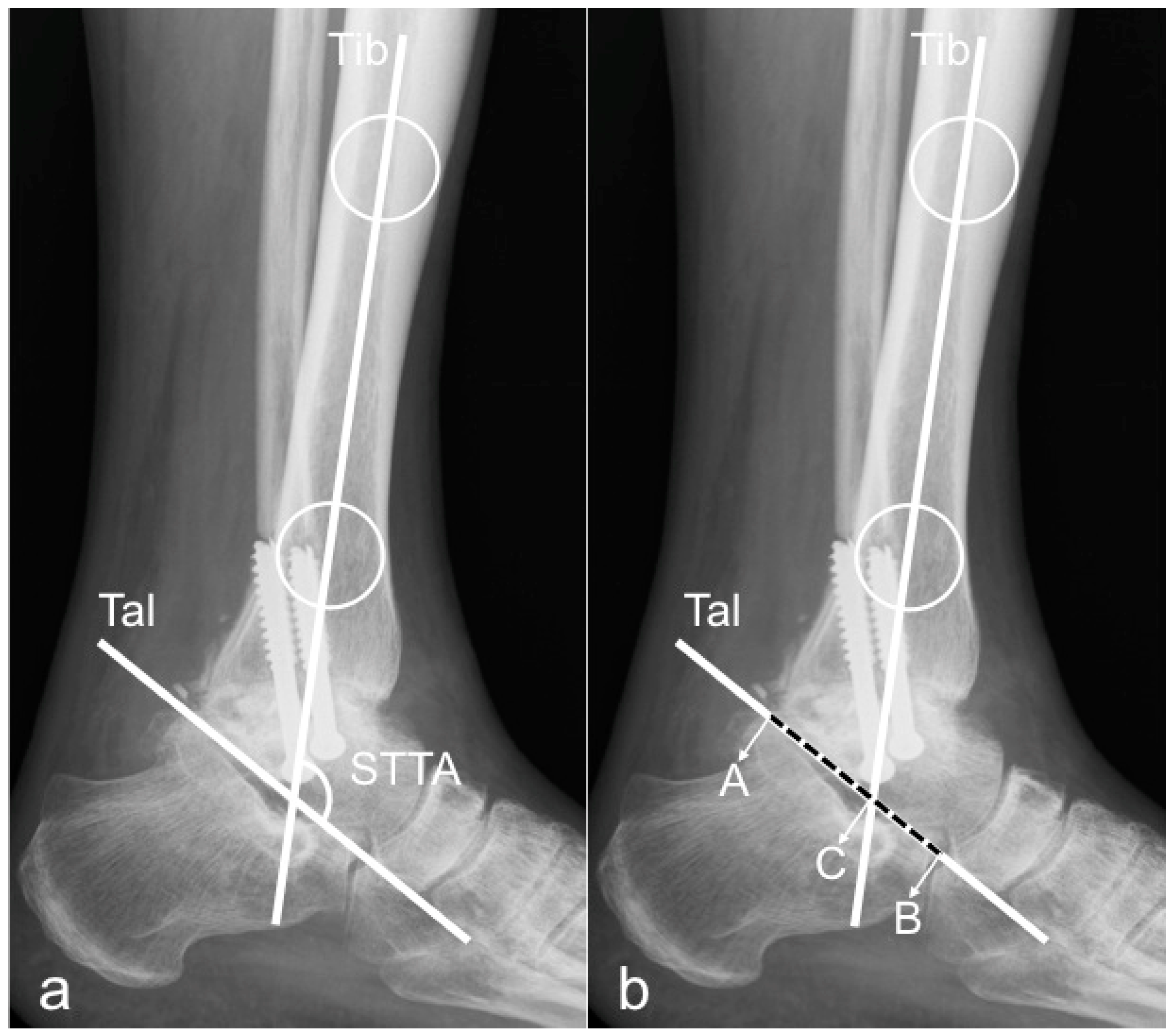
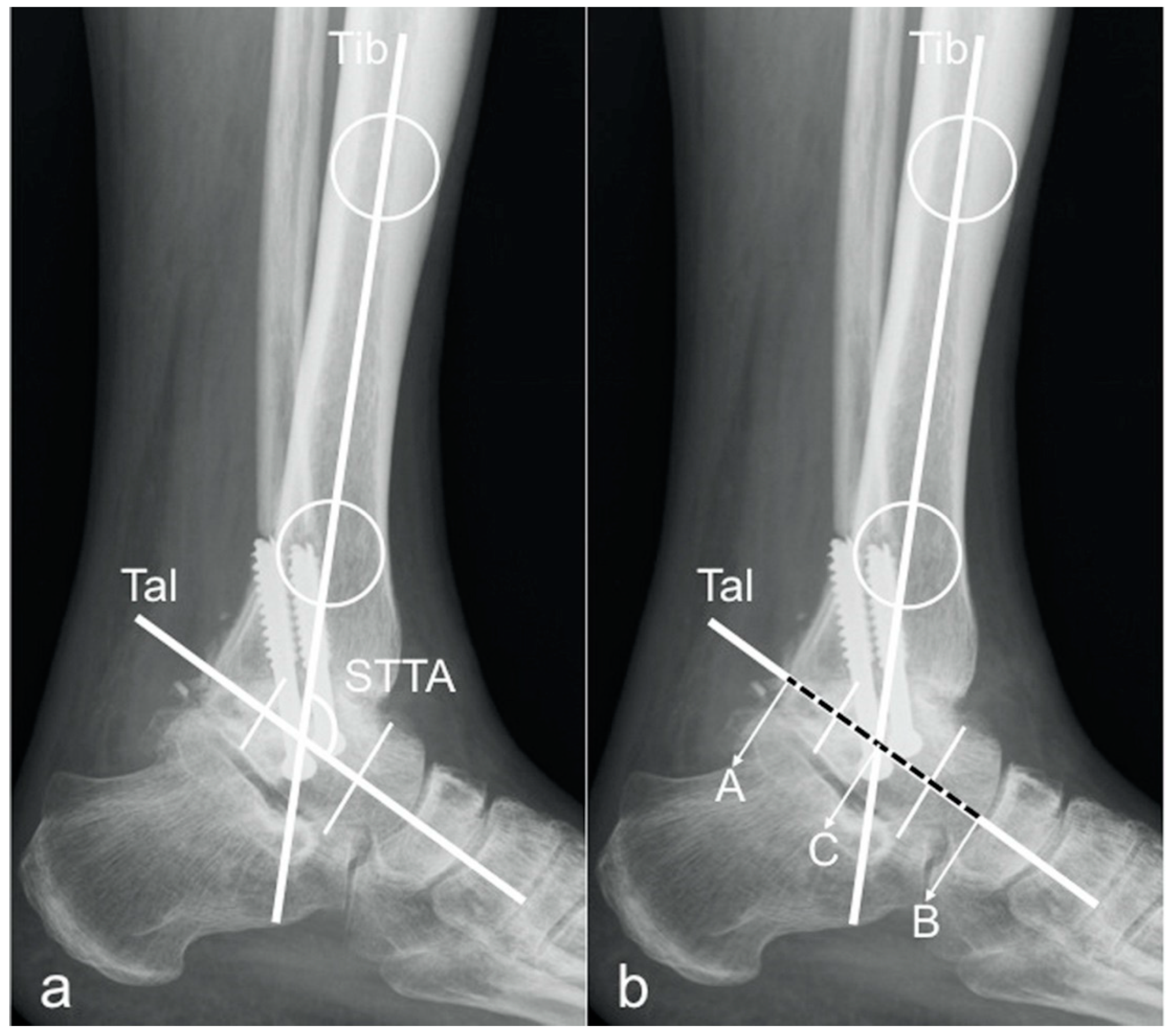
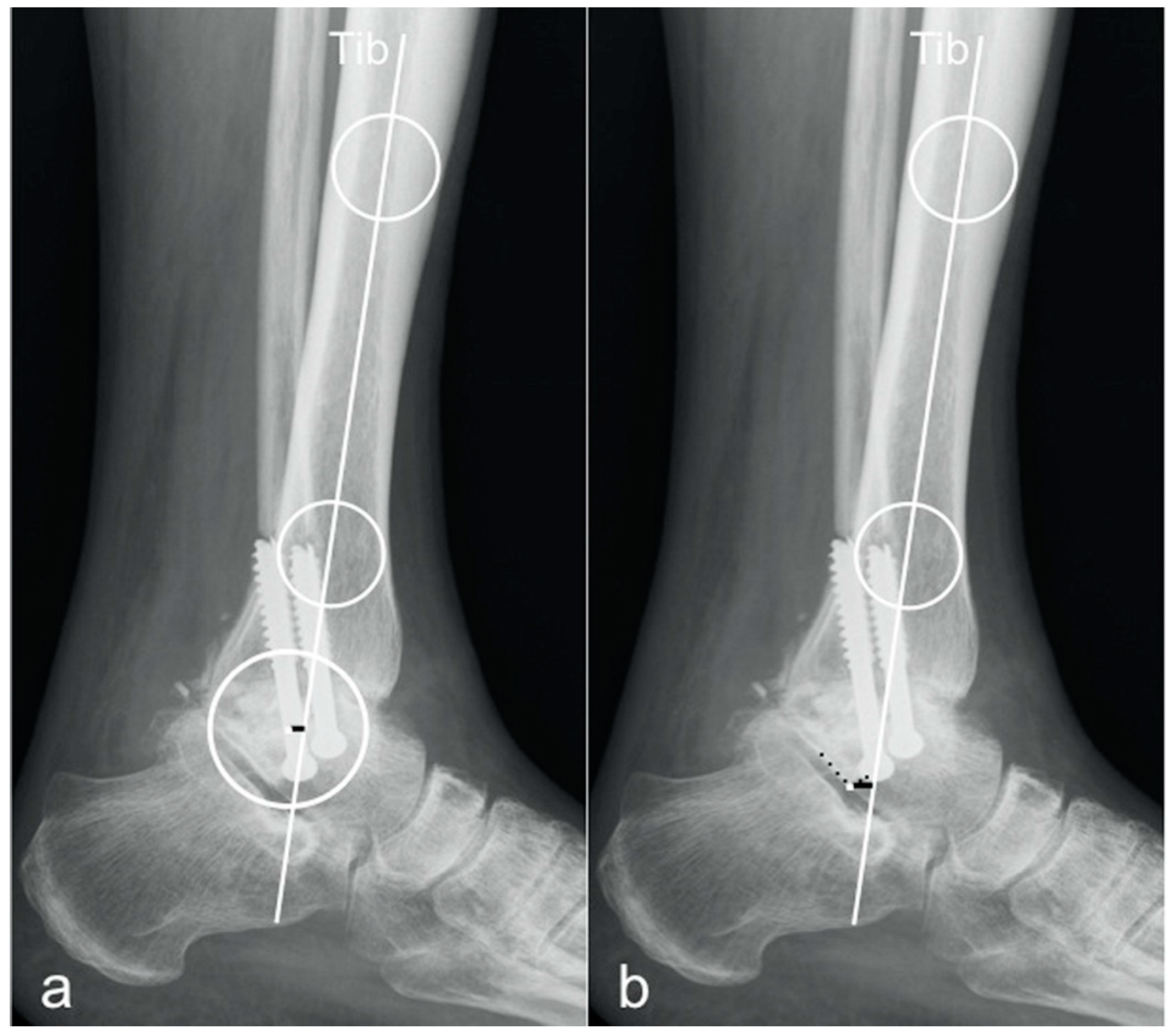
2.1. Radiographic Measurements
- tibCOR:
- procLAT:
- the distance from the tip of the lateral process of the talus to the longitudinal axis of the tibia [9].
2.2. Assessment of Measurement Reliability, Accuracy, and Agreement
2.3. Statistical Analysis
3. Results
3.1. Intraobserver Reliability
3.2. Interobserver Reliability
3.3. Accuracy
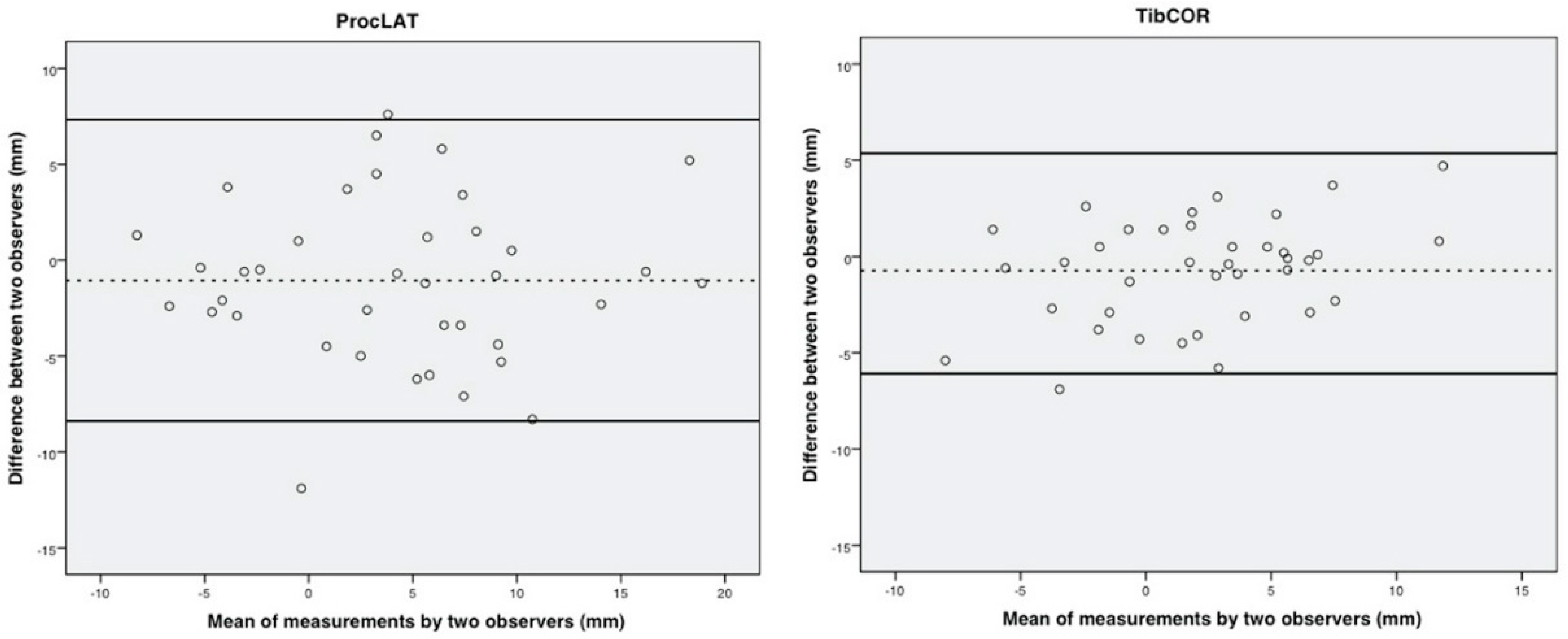
3.4. Agreement
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Buck, P.; Morrey, B.F.; Chao, E.Y. The optimum position of arthrodesis of the ankle. A gait study of the knee and ankle. J. Bone Jt. Surg. Am. Vol. 1987, 69, 1052–1062. [Google Scholar] [CrossRef]
- Tochigi, Y.; Suh, J.S.; Amendola, A.; Pedersen, D.R.; Saltzman, C.L. Ankle alignment on lateral radiographs. Part 1: Sensitivity of measuRes. to perturbations of ankle positioning. Foot Ankle Int. 2006, 27, 82–87. [Google Scholar] [CrossRef]
- Coester, L.M.; Saltzman, C.L.; Leupold, J.; Pontarelli, W. Long-term results following ankle arthrodesis for post-traumatic arthritis. J. Bone Jt. Surg. Am. Vol. 2001, 83, 219–228. [Google Scholar] [CrossRef] [PubMed]
- Kwon, D.G.; Chung, C.Y.; Park, M.S.; Sung, K.H.; Kim, T.W.; Lee, K.M. Arthroplasty versus arthrodesis for end-stage ankle arthritis: Decision analysis using Markov model. Int. Orthop. 2011, 35, 1647–1653. [Google Scholar] [CrossRef] [PubMed]
- Mazur, J.M.; Schwartz, E.; Simon, S.R. Ankle arthrodesis. Long-term follow-up with gait analysis. J. Bone Jt. Surg. Am. Vol. 1979, 61, 964–975. [Google Scholar] [CrossRef]
- Schuh, R.; Hofstaetter, J.; Krismer, M.; Bevoni, R.; Windhager, R.; Trnka, H.J. Total ankle arthroplasty versus ankle arthrodesis. Comparison of sports, recreational activities and functional outcome. Int. Orthop. 2012, 36, 1207–1214. [Google Scholar] [CrossRef]
- Barg, A.; Elsner, A.; Chuckpaiwong, B.; Hintermann, B. Insert position in three-component total ankle replacement. Foot Ankle Int. 2010, 31, 754–759. [Google Scholar] [CrossRef]
- McKellop, H.A.; Llinas, A.; Sarmiento, A. Effects of tibial malalignment on the knee and ankle. Orthop. Clin. N. Am. 1994, 25, 415–423. [Google Scholar]
- Paley, D.; Herzenberg, J.E.; Tetsworth, K.; McKie, J.; Bhave, A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop. Clin. N. Am. 1994, 25, 425–465. [Google Scholar]
- Veljkovic, A.; Norton, A.; Salat, P.; Saltzman, C.; Femino, J.; Phisitkul, P.; Amendola, A. Lateral talar station: A clinically reproducible measure of sagittal talar position. Foot Ankle Int. 2013, 34, 1669–1676. [Google Scholar] [CrossRef]
- Adams, S.B., Jr.; Demetracopoulos, C.A.; Viens, N.A.; DeOrio, J.K.; Easley, M.E.; Queen, R.M.; Nunley, J.A., 2nd. Comparison of extramedullary versus intramedullary referencing for tibial component alignment in total ankle arthroplasty. Foot Ankle Int. 2013, 34, 1624–1628. [Google Scholar] [CrossRef] [PubMed]
- Barg, A.; Amendola, R.L.; Henninger, H.B.; Kapron, A.L.; Saltzman, C.L.; Anderson, A.E. Influence of Ankle Position and Radiographic Projection Angle on Measurement of Supramalleolar Alignment on the Anteroposterior and Hindfoot Alignment Views. Foot Ankle Int. 2015, 36, 1352–1361. [Google Scholar] [CrossRef] [PubMed]
- Braito, M.; Dammerer, D.; Reinthaler, A.; Kaufmann, G.; Huber, D.; Biedermann, R. Effect of Coronal and Sagittal Alignment on Outcome After Mobile-Bearing Total Ankle Replacement. Foot Ankle Int. 2015, 36, 1029–1037. [Google Scholar] [CrossRef] [PubMed]
- Tochigi, Y.; Suh, J.S.; Amendola, A.; Saltzman, C.L. Ankle alignment on lateral radiographs. Part 2: Reliability and validity of measures. Foot Ankle Int. 2006, 27, 88–92. [Google Scholar] [CrossRef] [PubMed]
- Imsdahl, S.I.; Stender, C.J.; Cook, B.K.; Pangrazzi, G.; Patthanacharoenphon, C.; Sangeorzan, B.J.; Ledoux, W.R. Anteroposterior Translational Malalignment of Ankle Arthrodesis Alters Foot Biomechanics in Cadaveric Gait Simulation. J. Orthop. Res. 2019. [Google Scholar] [CrossRef] [PubMed]
- McKearney, D.A.; Stender, C.J.; Cook, B.K.; Moore, E.S.; Gunnell, L.M.; Monier, B.C.; Sangeorzan, B.J.; Ledoux, W.R. Altered Range of Motion and Plantar Pressure in Anterior and Posterior Malaligned Total Ankle Arthroplasty: A Cadaveric Gait Study. J. Bone Jt. Surg. Am. Vol. 2019, 101, e93. [Google Scholar] [CrossRef]
- Usuelli, F.G.; Manzi, L.; Brusaferri, G.; Neher, R.E.; Guelfi, M.; Maccario, C. Sagittal tibiotalar translation and clinical outcomes in mobile and fixed-bearing total ankle replacement. Foot Ankle Surg. 2017, 23, 95–101. [Google Scholar] [CrossRef]
- Usuelli, F.G.; Maccario, C.; Indino, C.; Manzi, L.; Gross, C.E. Tibial slope in total ankle arthroplasty: Anterior or lateral approach. Foot Ankle Surg. 2017, 23, 84–88. [Google Scholar] [CrossRef]
- Sealey, R.J.; Myerson, M.S.; Molloy, A.; Gamba, C.; Jeng, C.; Kalesan, B. Sagittal plane motion of the hindfoot following ankle arthrodesis: A prospective analysis. Foot Ankle Int. 2009, 30, 187–196. [Google Scholar] [CrossRef]
- van der Plaat, L.W.; van Engelen, S.J.; Wajer, Q.E.; Hendrickx, R.P.; Doets, K.H.; Houdijk, H.; van Dijk, C.N. Hind- and Midfoot Motion After Ankle Arthrodesis. Foot Ankle Int. 2015, 36, 1430–1437. [Google Scholar] [CrossRef]
- Willegger, M.; Holinka, J.; Nemecek, E.; Bock, P.; Wanivenhaus, A.H.; Windhager, R.; Schuh, R. Reliability of the Radiographic Sagittal and Frontal Tibiotalar Alignment after Ankle Arthrodesis. PLoS ONE 2016, 11, e0154224. [Google Scholar] [CrossRef] [PubMed]
- Mann, R.A.; Van Manen, J.W.; Wapner, K.; Martin, J. Ankle fusion. Clin Orthop. Relat Res. 1991, 49–55. [Google Scholar]
- Schneider, W.; Csepan, R.; Knahr, K. Reproducibility of the radiographic metatarsophalangeal angle in hallux surgery. J. Bone Jt. Surg. Am. Vol. 2003, 85, 494–499. [Google Scholar] [CrossRef] [PubMed]
- Magerkurth, O.; Knupp, M.; Ledermann, H.; Hintermann, B. Evaluation of hindfoot dimensions: A radiological study. Foot Ankle Int. 2006, 27, 612–616. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- Thomas, R.H.; Daniels, T.R. Ankle arthritis. J. Bone Jt. Surg. Am. 2003, 85, 923–936. [Google Scholar] [CrossRef] [PubMed]
- Morrey, B.F.; Wiedeman, G.P., Jr. Complications and long-term results of ankle arthrodeses following trauma. J. Bone Jt. Surg. Am. 1980, 62, 777–784. [Google Scholar] [CrossRef]
- Pellegrini, M.J.; Schiff, A.P.; Adams, S.B.; Queen, R.M.; DeOrio, J.K.; Nunley, J.A. Conversion of Tibiotalar Arthrodesis to Total Ankle Arthroplasty. J. Bone Jt. Surg. Am. 2015, 15, 2004–2013. [Google Scholar] [CrossRef]
- Hefti, F.L.; Baumann, J.U.; Morscher, E.W. Ankle joInt. fusion—Determination of optimal position by gait analysis. Arch Orthop. Trauma Surg. 1980, 31, 187–195. [Google Scholar] [CrossRef]
- Steel, M.W., 3rd; Johnson, K.A.; DeWitz, M.A.; Ilstrup, D.M. Radiographic measurements of the normal adult foot. Foot Ankle 1980, 1, 151–158. [Google Scholar] [CrossRef]
- Usuelli, F.G.; Maccario, C.; Pantalone, A.; Serra, N.; Tan, E.W. Identifying the learning curve for total ankle replacement using a mobile bearing prosthesis. Foot Ankle Surg. 2017, 23, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Usuelli, F.G.; Di Silvestri, C.A.; D’Ambrosi, R.; Orenti, A.; Randelli, F. Total ankle replacement: Is pre-operative varus deformity a predictor of poor survival rate and clinical and radiological outcomes? Int. Orthop. 2019, 43, 243–249. [Google Scholar] [CrossRef] [PubMed]
| ICC INTRAOBSERVER RELIABILITY | ||||||
| STTA Method 1 | 95% CI lower | upper | STTA Method 2 | 95% CI lower | upper | |
| Observer 1 | 0.966 | 0.935 | 0.982 | 0.852 | 0.687 | 0.927 |
| Observer 2 | 0.881 | 0.77 | 0.938 | 0.892 | 0.793 | 0.944 |
| Observer 3 | 0.853 | 0.698 | 0.926 | 0.832 | 0.64 | 0.917 |
| mT-T ratio Method 1 | 95% CI lower | upper | mT-T ratio Method 2 | 95% CI lower | upper | |
| Observer 1 | 0.922 | 0.847 | 0.96 | 0.768 | 0.515 | 0.885 |
| Observer 2 | 0.93 | 0.859 | 0.965 | 0.846 | 0.703 | 0.92 |
| Observer 3 | 0.771 | 0.556 | 0.881 | 0.83 | 0.675 | 0.911 |
| tibCOR | 95% CI lower | upper | procLAT | 95% CI lower | upper | |
| Observer 1 | 0.938 | 0.881 | 0.967 | 0.937 | 0.879 | 0.967 |
| Observer 2 | 0.96 | 0.916 | 0.98 | 0.981 | 0.96 | 0.991 |
| Observer 3 | 0.878 | 0.758 | 0.937 | 0.83 | 0.673 | 0.912 |
| ICC INTEROBSERVER RELIABILITY | ||||||
| STTA Method 1 | 95% CI lower | upper | STTA Method 2 | 95% CI lower | upper | |
| 0.924 | 0.862 | 0.959 | 0.849 | 0.726 | 0.919 | |
| mT-T ratio Method 1 | 95% CI lower | upper | mT-T ratio Method 2 | 95% CI lower | upper | |
| 0.836 | 0.721 | 0.909 | 0.731 | 0.542 | 0.851 | |
| tibCOR | 95% CI lower | upper | procLAT | 95% CI lower | upper | |
| 0.89 | 0.812 | 0.939 | 0.878 | 0.791 | 0.932 | |
| Mean | Range | SD | 95% CI Lower | Upper | p-Value | |
|---|---|---|---|---|---|---|
| STTA | ||||||
| Method 1 | 109.11° | 78.1–131.8 | 8.54 | 107.99 | 110.22 | |
| Method 2 | 107.86° | 72.8–129.7 | 10 | 106.56 | 109.17 | |
| All | 108.49° | 72.8–131.8 | 9.31 | 107.63 | 109.34 | |
| difference | 1.25° | 0.46 | 2.96 | 0.154 | ||
| mT-T ratio | ||||||
| Method 1 | 46.53% | 9.82–141.83 | 14.1 | 44.69 | 48.37 | |
| Method 2 | 31.59% | 7.99–70.23 | 11.02 | 30.15 | 33.03 | |
| all | 39.06% | 7.99–141.83 | 14.69 | 37.7 | 40.41 | |
| tibCOR | 1.96 mm | −10.7–16.9 | 4.54 | 1.36 | 2.55 | |
| procLAT | 3.97 mm | −10.6–20.9 | 7.13 | 3.04 | 4.9 | |
| difference | −2.01 mm | −3.11 | 0.91 | <0.000 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schieder, S.; Nemecek, E.; Schuh, R.; Kolb, A.; Windhager, R.; Willegger, M. Radiographic Sagittal Tibio-Talar Offset in Ankle Arthrodesis—Accuracy and Reliability of Measurements. J. Clin. Med. 2020, 9, 801. https://doi.org/10.3390/jcm9030801
Schieder S, Nemecek E, Schuh R, Kolb A, Windhager R, Willegger M. Radiographic Sagittal Tibio-Talar Offset in Ankle Arthrodesis—Accuracy and Reliability of Measurements. Journal of Clinical Medicine. 2020; 9(3):801. https://doi.org/10.3390/jcm9030801
Chicago/Turabian StyleSchieder, Sophie, Elena Nemecek, Reinhard Schuh, Alexander Kolb, Reinhard Windhager, and Madeleine Willegger. 2020. "Radiographic Sagittal Tibio-Talar Offset in Ankle Arthrodesis—Accuracy and Reliability of Measurements" Journal of Clinical Medicine 9, no. 3: 801. https://doi.org/10.3390/jcm9030801
APA StyleSchieder, S., Nemecek, E., Schuh, R., Kolb, A., Windhager, R., & Willegger, M. (2020). Radiographic Sagittal Tibio-Talar Offset in Ankle Arthrodesis—Accuracy and Reliability of Measurements. Journal of Clinical Medicine, 9(3), 801. https://doi.org/10.3390/jcm9030801





