Ischemia-Reperfusion Injury in Marginal Liver Grafts and the Role of Hypothermic Machine Perfusion: Molecular Mechanisms and Clinical Implications
Abstract
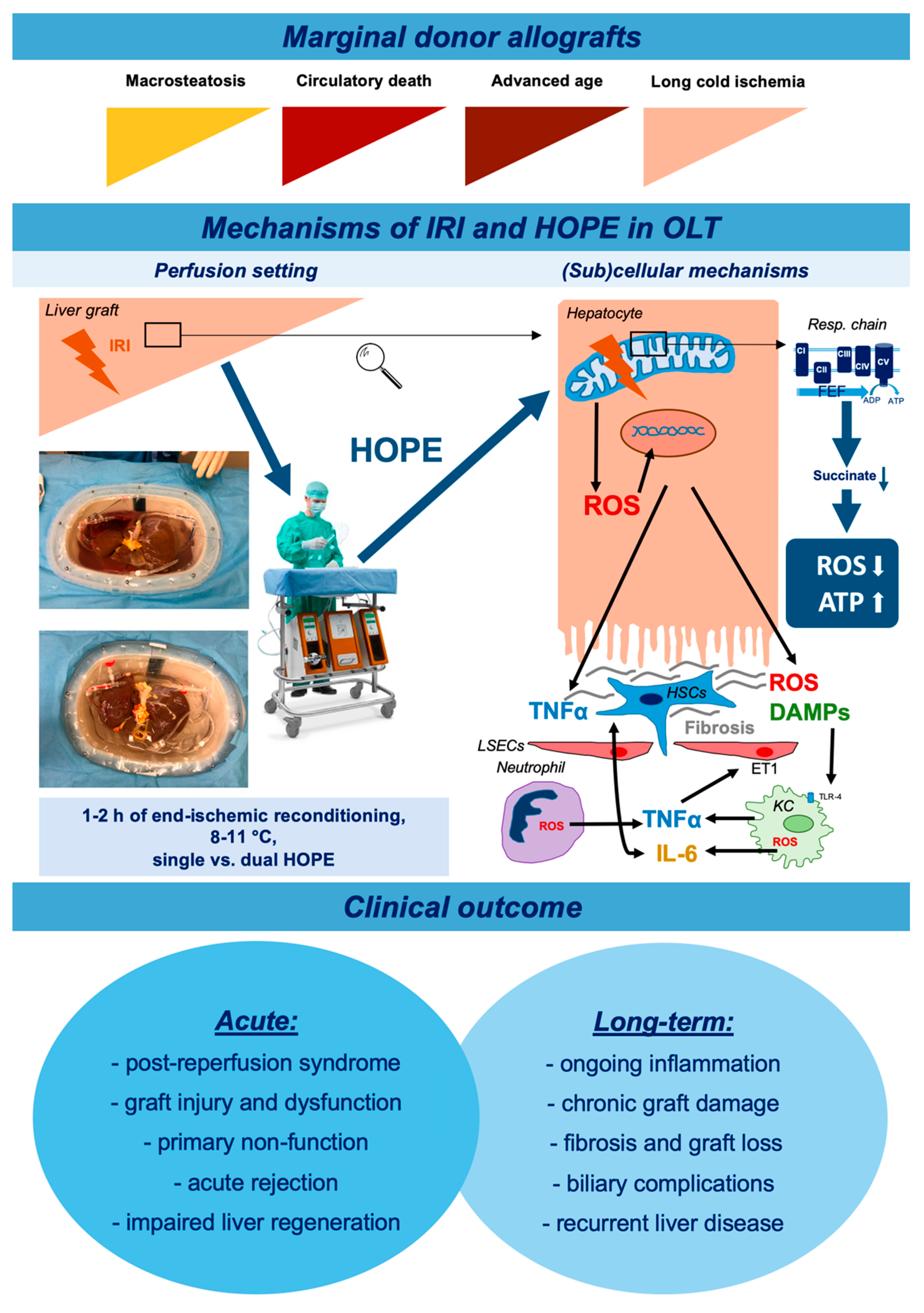
1. Introduction
2. Ischemia-Reperfusion Injury and Marginal Allografts
2.1. The Mechanism of Ischemia-Reperfusion Injury
2.2. The Heterogeneity of ECD Grafts
3. Machine Liver Perfusion Technology
3.1. History and Clinical Application
3.2. Hypothermic Machine Perfusion
3.3. Hypothermic Oxygenated Perfusion (HOPE)
3.4. Multimodal Perfusion Approaches
3.5. Viability Assessment under Hypothermic Conditions and Biomarkers of IRI
3.6. Allograft Therapies, Surgical Interventions, and On-Pump Drug Delivery
4. Molecular Effects of Hypothermic Machine Perfusion
4.1. The Role of the Endothelial Cells
4.2. The Role of Cold Oxygenation
5. Future Outlook and Remaining Challenges
Author Contributions
Funding
Conflicts of Interest
References
- Land, W.G. The role of postischemic reperfusion injury and other nonantigen-dependent inflammatory pathways in transplantation. Transplantation 2005, 79, 505–514. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Qiu, L.; Yan, S.; Wang, J.-J.; Thomas, P.M.; Kandpal, M.; Zhao, L.; Iovane, A.; Liu, X.-F.; Thorp, E.B.; et al. A clinically relevant murine model unmasks a “two-hit” mechanism for reactivation and dissemination of cytomegalovirus after kidney transplant. Am. J. Transplant. 2019, 19, 2421–2433. [Google Scholar] [CrossRef] [PubMed]
- Tacke, F.; Kroy, D.C.; Barreiros, A.P.; Neumann, U.P. Liver transplantation in Germany. Liver Transplant. 2016. [Google Scholar] [CrossRef] [PubMed]
- Eurotransplant. Waiting List Mortality in 2015, by Country, by Organ. Available online: https://statistics.eurotransplant.org/ (accessed on 18 March 2020).
- Czigany, Z.; Schoning, W.; Ulmer, T.F.; Bednarsch, J.; Amygdalos, I.; Cramer, T.; Rogiers, X.; Popescu, I.; Botea, F.; Fronek, J.; et al. Hypothermic oxygenated machine perfusion (HOPE) for orthotopic liver transplantation of human liver allografts from extended criteria donors (ECD) in donation after brain death (DBD): A prospective multicentre randomised controlled trial (HOPE ECD-DBD). BMJ Open 2017, 7, e017558. [Google Scholar] [CrossRef] [PubMed]
- Czigany, Z.; Lurje, I.; Tolba, R.H.; Neumann, U.P.; Tacke, F.; Lurje, G. Machine perfusion for liver transplantation in the era of marginal organs-New kids on the block. Liver Int. 2018. [Google Scholar] [CrossRef]
- Merion, R.M.; Goodrich, N.P.; Feng, S. How can we define expanded criteria for liver donors? J. Hepatol. 2006, 45, 484–488. [Google Scholar] [CrossRef]
- Ploeg, R.J.; D’Alessandro, A.M.; Knechtle, S.J.; Stegall, M.D.; Pirsch, J.D.; Hoffmann, R.M.; Sasaki, T.; Sollinger, H.W.; Belzer, F.O.; Kalayoglu, M. Risk factors for primary dysfunction after liver transplantation--a multivariate analysis. Transplantation 1993, 55, 807–813. [Google Scholar] [CrossRef]
- Busquets, J.; Xiol, X.; Figueras, J.; Jaurrieta, E.; Torras, J.; Ramos, E.; Rafecas, A.; Fabregat, J.; Lama, C.; Ibanez, L.; et al. The impact of donor age on liver transplantation: Influence of donor age on early liver function and on subsequent patient and graft survival. Transplantation 2001, 71, 1765–1771. [Google Scholar] [CrossRef]
- Piratvisuth, T.; Tredger, J.M.; Hayllar, K.A.; Williams, R. Contribution of true cold and rewarming ischemia times to factors determining outcome after orthotopic liver transplantation. Liver Transplant. Surg. 1995, 1, 296–301. [Google Scholar] [CrossRef]
- Czigany, Z.; Bleilevens, C.; Beckers, C.; Stoppe, C.; Mohring, M.; Fulop, A.; Szijarto, A.; Lurje, G.; Neumann, U.P.; Tolba, R.H. Limb remote ischemic conditioning of the recipient protects the liver in a rat model of arterialized orthotopic liver transplantation. PLoS ONE 2018, 13, e0195507. [Google Scholar] [CrossRef]
- Emontzpohl, C.; Stoppe, C.; Theissen, A.; Beckers, C.; Neumann, U.P.; Lurje, G.; Ju, C.; Bernhagen, J.; Tolba, R.H.; Czigany, Z. The Role of Macrophage Migration Inhibitory Factor in Remote Ischemic Conditioning Induced Hepatoprotection in A Rodent Model of Liver Transplantation. Shock 2018. [Google Scholar] [CrossRef] [PubMed]
- Gao, W.; Bentley, R.C.; Madden, J.F.; Clavien, P.A. Apoptosis of sinusoidal endothelial cells is a critical mechanism of preservation injury in rat liver transplantation. Hepatology 1998, 27, 1652–1660. [Google Scholar] [CrossRef] [PubMed]
- Ploeg, R.J.; van Bockel, J.H.; Langendijk, P.T.; Groenewegen, M.; van der Woude, F.J.; Persijn, G.G.; Thorogood, J.; Hermans, J. Effect of preservation solution on results of cadaveric kidney transplantation. The European Multicentre Study Group. Lancet 1992, 340, 129–137. [Google Scholar] [CrossRef]
- Jaeschke, H. Molecular mechanisms of hepatic ischemia-reperfusion injury and preconditioning. Am. J. Physiol. Gastrointest. Liver Physiol. 2003, 284, G15–G26. [Google Scholar] [CrossRef]
- Hessheimer, A.J.; Garcia-Valdecasas, J.C.; Fondevila, C. Abdominal regional in-situ perfusion in donation after circulatory determination of death donors. Curr. Opin. Organ Transplant. 2016, 21, 322–328. [Google Scholar] [CrossRef]
- Stewart, R.K.; Dangi, A.; Huang, C.; Murase, N.; Kimura, S.; Stolz, D.B.; Wilson, G.C.; Lentsch, A.B.; Gandhi, C.R. A novel mouse model of depletion of stellate cells clarifies their role in ischemia/reperfusion- and endotoxin-induced acute liver injury. J. Hepatol. 2014, 60, 298–305. [Google Scholar] [CrossRef]
- Belzer, F.O.; Southard, J.H. Principles of solid-organ preservation by cold storage. Transplantation 1988, 45, 673–676. [Google Scholar] [CrossRef]
- Chouchani, E.T.; Pell, V.R.; James, A.M.; Work, L.M.; Saeb-Parsy, K.; Frezza, C.; Krieg, T.; Murphy, M.P. A Unifying Mechanism for Mitochondrial Superoxide Production during Ischemia-Reperfusion Injury. Cell Metab. 2016, 23, 254–263. [Google Scholar] [CrossRef]
- Peralta, C.; Bartrons, R.; Riera, L.; Manzano, A.; Xaus, C.; Gelpi, E.; Rosello-Catafau, J. Hepatic preconditioning preserves energy metabolism during sustained ischemia. Am. J. Physiol. Gastrointest. Liver Physiol. 2000, 279, G163–G171. [Google Scholar] [CrossRef]
- Carini, R.; Bellomo, G.; Benedetti, A.; Fulceri, R.; Gamberucci, A.; Parola, M.; Dianzani, M.U.; Albano, E. Alteration of Na+ homeostasis as a critical step in the development of irreversible hepatocyte injury after adenosine triphosphate depletion. Hepatology 1995, 21, 1089–1098. [Google Scholar]
- Zaouali, M.A.; Ben Abdennebi, H.; Padrissa-Altes, S.; Mahfoudh-Boussaid, A.; Rosello-Catafau, J. Pharmacological strategies against cold ischemia reperfusion injury. Expert Opin. Pharmacother. 2010, 11, 537–555. [Google Scholar] [CrossRef] [PubMed]
- Niatsetskaya, Z.V.; Sosunov, S.A.; Matsiukevich, D.; Utkina-Sosunova, I.V.; Ratner, V.I.; Starkov, A.A.; Ten, V.S. The oxygen free radicals originating from mitochondrial complex I contribute to oxidative brain injury following hypoxia-ischemia in neonatal mice. J. Neurosci. 2012, 32, 3235–3244. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Moghaddas, S.; Hoppel, C.L.; Lesnefsky, E.J. Reversible blockade of electron transport during ischemia protects mitochondria and decreases myocardial injury following reperfusion. J. Pharmacol. Exp. Ther. 2006, 319, 1405–1412. [Google Scholar] [CrossRef] [PubMed]
- Hoyer, D.P.; Mathe, Z.; Gallinat, A.; Canbay, A.C.; Treckmann, J.W.; Rauen, U.; Paul, A.; Minor, T. Controlled Oxygenated Rewarming of Cold Stored Livers Prior to Transplantation: First Clinical Application of a New Concept. Transplantation 2016, 100, 147–152. [Google Scholar] [CrossRef] [PubMed]
- van Golen, R.F.; Reiniers, M.J.; Olthof, P.B.; van Gulik, T.M.; Heger, M. Sterile inflammation in hepatic ischemia/reperfusion injury: Present concepts and potential therapeutics. J. Gastroenterol. Hepatol. 2013, 28, 394–400. [Google Scholar] [CrossRef]
- Essani, N.A.; McGuire, G.M.; Manning, A.M.; Jaeschke, H. Endotoxin-induced activation of the nuclear transcription factor kappa B and expression of E-selectin messenger RNA in hepatocytes, Kupffer cells, and endothelial cells in vivo. J. Immunol. 1996, 156, 2956–2963. [Google Scholar]
- Essani, N.A.; Fisher, M.A.; Jaeschke, H. Inhibition of NF-kappa B activation by dimethyl sulfoxide correlates with suppression of TNF-alpha formation, reduced ICAM-1 gene transcription, and protection against endotoxin-induced liver injury. Shock 1997, 7, 90–96. [Google Scholar] [CrossRef]
- Jaeschke, H.; Farhood, A. Neutrophil and Kupffer cell-induced oxidant stress and ischemia-reperfusion injury in rat liver. Am. J. Physiol. 1991, 260, G355–G362. [Google Scholar] [CrossRef]
- Perry, B.C.; Soltys, D.; Toledo, A.H.; Toledo-Pereyra, L.H. Tumor necrosis factor-alpha in liver ischemia/reperfusion injury. J. Investig. Surg. 2011, 24, 178–188. [Google Scholar] [CrossRef]
- van Golen, R.F.; van Gulik, T.M.; Heger, M. Mechanistic overview of reactive species-induced degradation of the endothelial glycocalyx during hepatic ischemia/reperfusion injury. Free Radic. Biol. Med. 2012, 52, 1382–1402. [Google Scholar] [CrossRef]
- Cywes, R.; Packham, M.A.; Tietze, L.; Sanabria, J.R.; Harvey, P.R.; Phillips, M.J.; Strasberg, S.M. Role of platelets in hepatic allograft preservation injury in the rat. Hepatology 1993, 18, 635–647. [Google Scholar] [CrossRef] [PubMed]
- Koo, A.; Komatsu, H.; Tao, G.; Inoue, M.; Guth, P.H.; Kaplowitz, N. Contribution of no-reflow phenomenon to hepatic injury after ischemia-reperfusion: Evidence for a role for superoxide anion. Hepatology 1992, 15, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Clemens, M.G. Nitric oxide in liver injury. Hepatology 1999, 30, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Boecker, J.; Czigany, Z.; Bednarsch, J.; Amygdalos, I.; Meister, F.; Santana, D.A.M.; Liu, W.J.; Strnad, P.; Neumann, U.P.; Lurje, G. Potential value and limitations of different clinical scoring systems in the assessment of short- and long-term outcome following orthotopic liver transplantation. PLoS ONE 2019, 14, e0214221. [Google Scholar] [CrossRef]
- Boteon, Y.L.; Boteon, A.; Attard, J.; Mergental, H.; Mirza, D.F.; Bhogal, R.H.; Afford, S.C. Ex situ machine perfusion as a tool to recondition steatotic donor livers: Troublesome features of fatty livers and the role of defatting therapies. A systematic review. Am. J. Transplant. 2018, 18, 2384–2399. [Google Scholar] [CrossRef] [PubMed]
- Ijaz, S.; Yang, W.; Winslet, M.C.; Seifalian, A.M. Impairment of hepatic microcirculation in fatty liver. Microcirculation 2003, 10, 447–456. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, L.; Carrasco-Chaumel, E.; Serafin, A.; Xaus, C.; Grande, L.; Rimola, A.; Rosello-Catafau, J.; Peralta, C. Is ischemic preconditioning a useful strategy in steatotic liver transplantation? Am. J. Transplant. 2004, 4, 888–899. [Google Scholar] [CrossRef] [PubMed]
- Ben Mosbah, I.; Alfany-Fernandez, I.; Martel, C.; Zaouali, M.A.; Bintanel-Morcillo, M.; Rimola, A.; Rodes, J.; Brenner, C.; Rosello-Catafau, J.; Peralta, C. Endoplasmic reticulum stress inhibition protects steatotic and non-steatotic livers in partial hepatectomy under ischemia-reperfusion. Cell Death Dis. 2010, 1, e52. [Google Scholar] [CrossRef] [PubMed]
- Ijaz, S.; Yang, W.; Winslet, M.C.; Seifalian, A.M. The role of nitric oxide in the modulation of hepatic microcirculation and tissue oxygenation in an experimental model of hepatic steatosis. Microvasc. Res. 2005, 70, 129–136. [Google Scholar] [CrossRef]
- Hayashi, M.; Tokunaga, Y.; Fujita, T.; Tanaka, K.; Yamaoka, Y.; Ozawa, K. The effects of cold preservation on steatotic graft viability in rat liver transplantation. Transplantation 1993, 56, 282–287. [Google Scholar] [CrossRef]
- Kron, P.; Schlegel, A.; Mancina, L.; Clavien, P.A.; Dutkowski, P. Hypothermic oxygenated perfusion (HOPE) for fatty liver grafts in rats and humans. J. Hepatol. 2017. [Google Scholar] [CrossRef] [PubMed]
- Jay, C.L.; Lyuksemburg, V.; Ladner, D.P.; Wang, E.; Caicedo, J.C.; Holl, J.L.; Abecassis, M.M.; Skaro, A.I. Ischemic cholangiopathy after controlled donation after cardiac death liver transplantation: A meta-analysis. Ann. Surg. 2011, 253, 259–264. [Google Scholar] [CrossRef]
- Foley, D.P.; Fernandez, L.A.; Leverson, G.; Anderson, M.; Mezrich, J.; Sollinger, H.W.; D’Alessandro, A. Biliary complications after liver transplantation from donation after cardiac death donors: An analysis of risk factors and long-term outcomes from a single center. Ann. Surg. 2011, 253, 817–825. [Google Scholar] [CrossRef]
- Dawson, P.A.; Lan, T.; Rao, A. Bile acid transporters. J. Lipid Res. 2009, 50, 2340–2357. [Google Scholar] [CrossRef] [PubMed]
- Hertl, M.; Harvey, P.R.C.; Swanson, P.E.; West, D.D.; Howard, T.K.; Shenoy, S.; Strasberg, S.M. Evidence of preservation injury to bile ducts by bile salts in the pig and its prevention by infusions of hydrophilic bile salts. Hepatology 1995, 21, 1130–1137. [Google Scholar] [CrossRef] [PubMed]
- Durand, F.; Levitsky, J.; Cauchy, F.; Gilgenkrantz, H.; Soubrane, O.; Francoz, C. Age and liver transplantation. J. Hepatol. 2019, 70, 745–758. [Google Scholar] [CrossRef] [PubMed]
- Bertuzzo, V.R.; Cescon, M.; Odaldi, F.; Di Laudo, M.; Cucchetti, A.; Ravaioli, M.; Del Gaudio, M.; Ercolani, G.; D’Errico, A.; Pinna, A.D. Actual Risk of Using Very Aged Donors for Unselected Liver Transplant Candidates: A European Single-center Experience in the MELD Era. Ann. Surg. 2017, 265, 388–396. [Google Scholar] [CrossRef]
- Detelich, D.; Markmann, J.F. The dawn of liver perfusion machines. Curr. Opin. Organ Transplant. 2018, 23, 151–161. [Google Scholar] [CrossRef]
- Diaz Jaime, F.; Berenguer, M. Pushing the donor limits: Deceased donor liver transplantation using organs from octogenarian donors. Liver Transplant. 2017, 23, S22–S26. [Google Scholar] [CrossRef]
- Starzl, T.E.; Groth, C.G.; Brettschneider, L.; Penn, I.; Fulginiti, V.A.; Moon, J.B.; Blanchard, H.; Martin, A.J., Jr.; Porter, K.A. Orthotopic homotransplantation of the human liver. Ann. Surg. 1968, 168, 392–415. [Google Scholar] [CrossRef]
- Vogel, T.; Brockmann, J.G.; Coussios, C.; Friend, P.J. The role of normothermic extracorporeal perfusion in minimizing ischemia reperfusion injury. Transplant. Rev. 2012, 26, 156–162. [Google Scholar] [CrossRef] [PubMed]
- Reddy, S.P.; Bhattacharjya, S.; Maniakin, N.; Greenwood, J.; Guerreiro, D.; Hughes, D.; Imber, C.J.; Pigott, D.W.; Fuggle, S.; Taylor, R.; et al. Preservation of porcine non-heart-beating donor livers by sequential cold storage and warm perfusion. Transplantation 2004, 77, 1328–1332. [Google Scholar] [CrossRef] [PubMed]
- Mergental, H.; Laing, R.W.; Kirkham, A.J.; Perera, T.P.R.; Boteon, Y.; Attard, J.; Barton, D.; Wilkhu, M.; Curbishley, S.; Neil, D.A.; et al. Transplantation after Viability Testing of Discarded Livers with Normothermic Machine Perfusion (NMP): The Vittal (VIability Testing and Transplantation of mArginal Livers) Trial 90-Day Outcomes. Hepatology 2018, 68. [Google Scholar] [CrossRef]
- Nasralla, D.; Coussios, C.C.; Mergental, H.; Akhtar, M.Z.; Butler, A.J.; Ceresa, C.D.L.; Chiocchia, V.; Dutton, S.J.; Garcia-Valdecasas, J.C.; Heaton, N.; et al. A randomized trial of normothermic preservation in liver transplantation. Nature 2018, 557, 50–56. [Google Scholar] [CrossRef]
- Czigany, Z.; Tacke, F.; Lurje, G. Evolving Trends in Machine Liver Perfusion: Comments on Clinical End Points and Selection Criteria. Gastroenterology 2019, 157, 1166–1167. [Google Scholar] [CrossRef]
- Eshmuminov, D.; Becker, D.; Bautista Borrego, L.; Hefti, M.; Schuler, M.J.; Hagedorn, C.; Muller, X.; Mueller, M.; Onder, C.; Graf, R.; et al. An integrated perfusion machine preserves injured human livers for 1 week. Nat. Biotechnol. 2020. [Google Scholar] [CrossRef]
- op den Dries, S.; Karimian, N.; Sutton, M.E.; Westerkamp, A.C.; Nijsten, M.W.; Gouw, A.S.; Wiersema-Buist, J.; Lisman, T.; Leuvenink, H.G.; Porte, R.J. Ex vivo normothermic machine perfusion and viability testing of discarded human donor livers. Am. J. Transplant. 2013, 13, 1327–1335. [Google Scholar] [CrossRef]
- Guarrera, J.V.; Henry, S.D.; Samstein, B.; Reznik, E.; Musat, C.; Lukose, T.I.; Ratner, L.E.; Brown, R.S., Jr.; Kato, T.; Emond, J.C. Hypothermic machine preservation facilitates successful transplantation of “orphan” extended criteria donor livers. Am. J. Transplant. 2015, 15, 161–169. [Google Scholar] [CrossRef]
- Moers, C.; Smits, J.M.; Maathuis, M.H.; Treckmann, J.; van Gelder, F.; Napieralski, B.P.; van Kasterop-Kutz, M.; van der Heide, J.J.; Squifflet, J.P.; van Heurn, E.; et al. Machine perfusion or cold storage in deceased-donor kidney transplantation. N. Engl. J. Med. 2009, 360, 7–19. [Google Scholar] [CrossRef]
- Guarrera, J.V.; Henry, S.D.; Samstein, B.; Odeh-Ramadan, R.; Kinkhabwala, M.; Goldstein, M.J.; Ratner, L.E.; Renz, J.F.; Lee, H.T.; Brown, J.R.S.; et al. Hypothermic Machine Preservation in Human Liver Transplantation: The First Clinical Series. Am. J. Transplant. 2010, 10, 372–381. [Google Scholar] [CrossRef]
- Henry, S.D.; Nachber, E.; Tulipan, J.; Stone, J.; Bae, C.; Reznik, L.; Kato, T.; Samstein, B.; Emond, J.C.; Guarrera, J.V. Hypothermic machine preservation reduces molecular markers of ischemia/reperfusion injury in human liver transplantation. Am. J. Transplant. 2012, 12, 2477–2486. [Google Scholar] [CrossRef] [PubMed]
- Balzan, S.; Belghiti, J.; Farges, O.; Ogata, S.; Sauvanet, A.; Delefosse, D.; Durand, F. The “50-50 Criteria” on Postoperative Day 5: An Accurate Predictor of Liver Failure and Death After Hepatectomy. Ann. Surg. 2005, 242, 824–829. [Google Scholar] [CrossRef] [PubMed]
- de Rougemont, O.; Breitenstein, S.; Leskosek, B.; Weber, A.; Graf, R.; Clavien, P.A.; Dutkowski, P. One hour hypothermic oxygenated perfusion (HOPE) protects nonviable liver allografts donated after cardiac death. Ann. Surg. 2009, 250, 674–683. [Google Scholar] [CrossRef] [PubMed]
- Dutkowski, P.; Schlegel, A.; de Oliveira, M.; Mullhaupt, B.; Neff, F.; Clavien, P.A. HOPE for human liver grafts obtained from donors after cardiac death. J. Hepatol. 2014, 60, 765–772. [Google Scholar] [CrossRef]
- Dutkowski, P.; Polak, W.G.; Muiesan, P.; Schlegel, A.; Verhoeven, C.J.; Scalera, I.; DeOliveira, M.L.; Kron, P.; Clavien, P.A. First Comparison of Hypothermic Oxygenated PErfusion Versus Static Cold Storage of Human Donation After Cardiac Death Liver Transplants: An International-matched Case Analysis. Ann. Surg. 2015, 262, 764–771. [Google Scholar] [CrossRef]
- Schlegel, A.; Muller, X.; Kalisvaart, M.; Muellhaupt, B.; Perera, M.; Isaac, J.R.; Clavien, P.A.; Muiesan, P.; Dutkowski, P. Outcomes of DCD liver transplantation using organs treated by hypothermic oxygenated perfusion before implantation. J. Hepatol. 2019, 70, 50–57. [Google Scholar] [CrossRef]
- van Rijn, R.; Karimian, N.; Matton, A.P.M.; Burlage, L.C.; Westerkamp, A.C.; van den Berg, A.P.; de Kleine, R.H.J.; de Boer, M.T.; Lisman, T.; Porte, R.J. Dual hypothermic oxygenated machine perfusion in liver transplants donated after circulatory death. Br. J. Surg. 2017, 104, 907–917. [Google Scholar] [CrossRef] [PubMed]
- van Rijn, R.; van Leeuwen, O.B.; Matton, A.P.M.; Burlage, L.C.; Wiersema-Buist, J.; van den Heuvel, M.C.; de Kleine, R.H.J.; de Boer, M.T.; Gouw, A.S.H.; Porte, R.J. Hypothermic oxygenated machine perfusion reduces bile duct reperfusion injury after transplantation of donation after circulatory death livers. Liver Transplant. 2018, 24, 655–664. [Google Scholar] [CrossRef]
- Patrono, D.; Surra, A.; Catalano, G.; Rizza, G.; Berchialla, P.; Martini, S.; Tandoi, F.; Lupo, F.; Mirabella, S.; Stratta, C.; et al. Hypothermic Oxygenated Machine Perfusion of Liver Grafts from Brain-Dead Donors. Sci. Rep. 2019, 9, 9337. [Google Scholar] [CrossRef]
- Brüggenwirth, I.M.A.; Burlage, L.C.; Porte, R.J.; Martins, P.N. Is single portal vein perfusion the best approach for machine preservation of liver grafts? J. Hepatol. 2016, 64, 1194–1195. [Google Scholar] [CrossRef]
- van Rijn, R.; van den Berg, A.P.; Erdmann, J.I.; Heaton, N.; van Hoek, B.; de Jonge, J.; Leuvenink, H.G.D.; Mahesh, S.V.K.; Mertens, S.; Monbaliu, D.; et al. Study protocol for a multicenter randomized controlled trial to compare the efficacy of end-ischemic dual hypothermic oxygenated machine perfusion with static cold storage in preventing non-anastomotic biliary strictures after transplantation of liver grafts donated after circulatory death: DHOPE-DCD trial. BMC Gastroenterol. 2019, 19, 40. [Google Scholar] [CrossRef]
- van Leeuwen, O.B.; de Vries, Y.; Fujiyoshi, M.; Nijsten, M.W.N.; Ubbink, R.; Pelgrim, G.J.; Werner, M.J.M.; Reyntjens, K.; van den Berg, A.P.; de Boer, M.T.; et al. Transplantation of High-risk Donor Livers After Ex Situ Resuscitation and Assessment Using Combined Hypo- and Normothermic Machine Perfusion: A Prospective Clinical Trial. Ann. Surg. 2019, 270, 906–914. [Google Scholar] [CrossRef] [PubMed]
- Boteon, Y.L.; Laing, R.W.; Schlegel, A.; Wallace, L.; Smith, A.; Attard, J.; Bhogal, R.H.; Reynolds, G.; Pr Perera, M.T.; Muiesan, P.; et al. The impact on the bioenergetic status and oxidative-mediated tissue injury of a combined protocol of hypothermic and normothermic machine perfusion using an acellular haemoglobin-based oxygen carrier: The cold-to-warm machine perfusion of the liver. PLoS ONE 2019, 14, e0224066. [Google Scholar] [CrossRef] [PubMed]
- Mergental, H.; Stephenson, B.T.F.; Laing, R.W.; Kirkham, A.J.; Neil, D.A.H.; Wallace, L.L.; Boteon, Y.L.; Widmer, J.; Bhogal, R.H.; Perera, M.; et al. Development of Clinical Criteria for Functional Assessment to Predict Primary Nonfunction of High-Risk Livers Using Normothermic Machine Perfusion. Liver Transplant. 2018, 24, 1453–1469. [Google Scholar] [CrossRef] [PubMed]
- Brockmann, J.; Reddy, S.; Coussios, C.; Pigott, D.; Guirriero, D.; Hughes, D.; Morovat, A.; Roy, D.; Winter, L.; Friend, P.J. Normothermic perfusion: A new paradigm for organ preservation. Ann. Surg. 2009, 250, 1–6. [Google Scholar] [CrossRef]
- Selten, J.; Schlegel, A.; de Jonge, J.; Dutkowski, P. Hypo- and normothermic perfusion of the liver: Which way to go? Best Pract. Res. Clin. Gastroenterol. 2017, 31, 171–179. [Google Scholar] [CrossRef]
- Muller, X.; Schlegel, A.; Kron, P.; Eshmuminov, D.; Wurdinger, M.; Meierhofer, D.; Clavien, P.A.; Dutkowski, P. Novel Real-time Prediction of Liver Graft Function During Hypothermic Oxygenated Machine Perfusion Before Liver Transplantation. Ann. Surg. 2019, 270, 783–790. [Google Scholar] [CrossRef]
- Bhogal, R.H.; Mirza, D.F.; Afford, S.C.; Mergental, H. Biomarkers of Liver Injury during Transplantation in an Era of Machine Perfusion. Int. J. Mol. Sci. 2020, 21. [Google Scholar] [CrossRef]
- Boteon, Y.L.; Wallace, L.; Boteon, A.; Mirza, D.F.; Mergental, H.; Bhogal, R.H.; Afford, S. An effective protocol for pharmacological defatting of primary human hepatocytes which is non-toxic to cholangiocytes or intrahepatic endothelial cells. PLoS ONE 2018, 13, e0201419. [Google Scholar] [CrossRef]
- Yagi, S.; Nagai, K.; Kadaba, P.; Afify, M.; Teramukai, S.; Uemoto, S.; Tolba, R.H. A novel organ preservation for small partial liver transplantations in rats: Venous systemic oxygen persuf fl ation with nitric oxide gas. Am. J. Transplant. 2013, 13, 222–228. [Google Scholar] [CrossRef]
- Jochmans, I.; O’Callaghan, J.M.; Pirenne, J.; Ploeg, R.J. Hypothermic machine perfusion of kidneys retrieved from standard and high-risk donors. Transplant. Int. 2015, 28, 665–676. [Google Scholar] [CrossRef] [PubMed]
- Yao, C.G.; Martins, P.N. Nanotechnology Applications in Transplantation Medicine. Transplantation 2019. [Google Scholar] [CrossRef] [PubMed]
- Tietjen, G.T.; Hosgood, S.A.; DiRito, J.; Cui, J.; Deep, D.; Song, E.; Kraehling, J.R.; Piotrowski-Daspit, A.S.; Kirkiles-Smith, N.C.; Al-Lamki, R.; et al. Nanoparticle targeting to the endothelium during normothermic machine perfusion of human kidneys. Sci. Transl. Med. 2017, 9. [Google Scholar] [CrossRef]
- Gillooly, A.R.; Perry, J.; Martins, P.N. First Report of siRNA Uptake (for RNA Interference) During Ex Vivo Hypothermic and Normothermic Liver Machine Perfusion. Transplantation 2019, 103, e56–e57. [Google Scholar] [CrossRef] [PubMed]
- Thijssen, M.F.; Bruggenwirth, I.M.A.; Gillooly, A.; Khvorova, A.; Kowalik, T.F.; Martins, P.N. Gene Silencing With siRNA (RNA Interference): A New Therapeutic Option During Ex Vivo Machine Liver Perfusion Preservation. Liver Transplant. 2019, 25, 140–151. [Google Scholar] [CrossRef] [PubMed]
- Van Raemdonck, D.; Neyrinck, A.; Rega, F.; Devos, T.; Pirenne, J. Machine perfusion in organ transplantation: A tool for ex-vivo graft conditioning with mesenchymal stem cells? Curr. Opin. Organ Transplant. 2013, 18, 24–33. [Google Scholar] [CrossRef]
- Kalenski, J.; Mancina, E.; Paschenda, P.; Beckers, C.; Bleilevens, C.; Tothova, L.; Boor, P.; Gross, D.; Tolba, R.H.; Doorschodt, B.M. Comparison of Aerobic Preservation by Venous Systemic Oxygen Persufflation or Oxygenated Machine Perfusion of Warm-Ischemia-Damaged Porcine Kidneys. Eur. Surg. Res. Eur. Chir. Forsch. Rech. Chir. Eur. 2016, 57, 10–21. [Google Scholar] [CrossRef]
- Karimian, N.; Yeh, H. Opportunities for Therapeutic Intervention During Machine Perfusion. Curr. Transplant. Rep. 2017, 4, 141–148. [Google Scholar] [CrossRef]
- Huang, V.; Karimian, N.; Detelich, D.; Raigani, S.; Geerts, S.; Beijert, I.; Fontan, F.M.; Aburawi, M.M.; Ozer, S.; Banik, P.; et al. Split-Liver Ex Situ Machine Perfusion: A Novel Technique for Studying Organ Preservation and Therapeutic Interventions. J. Clin. Med. 2020, 9. [Google Scholar] [CrossRef]
- Schlegel, A.; de Rougemont, O.; Graf, R.; Clavien, P.A.; Dutkowski, P. Protective mechanisms of end-ischemic cold machine perfusion in DCD liver grafts. J. Hepatol. 2013, 58, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Peralta, C.; Jimenez-Castro, M.B.; Gracia-Sancho, J. Hepatic ischemia and reperfusion injury: Effects on the liver sinusoidal milieu. J. Hepatol. 2013, 59, 1094–1106. [Google Scholar] [CrossRef] [PubMed]
- Upadhya, G.A.; Topp, S.A.; Hotchkiss, R.S.; Anagli, J.; Strasberg, S.M. Effect of cold preservation on intracellular calcium concentration and calpain activity in rat sinusoidal endothelial cells. Hepatology 2003, 37, 313–323. [Google Scholar] [CrossRef] [PubMed]
- Abudhaise, H.; Davidson, B.R.; DeMuylder, P.; Luong, T.V.; Fuller, B. Evolution of dynamic, biochemical, and morphological parameters in hypothermic machine perfusion of human livers: A proof-of-concept study. PLoS ONE 2018, 13, e0203803. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Mier, G.; Toledo-Pereyra, L.H.; Ward, P.A. Adhesion molecules in liver ischemia and reperfusion. J. Surg. Res. 2000, 94, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Lazeyras, F.; Buhler, L.; Vallee, J.P.; Hergt, M.; Nastasi, A.; Ruttimann, R.; Morel, P.; Buchs, J.B. Detection of ATP by “in line” 31P magnetic resonance spectroscopy during oxygenated hypothermic pulsatile perfusion of pigs’ kidneys. MAGMA 2012, 25, 391–399. [Google Scholar] [CrossRef]
- Schlegel, A.; Kron, P.; Graf, R.; Clavien, P.A.; Dutkowski, P. Hypothermic Oxygenated Perfusion (HOPE) downregulates the immune response in a rat model of liver transplantation. Ann. Surg. 2014, 260, 931–937. [Google Scholar] [CrossRef]
- Schlegel, A.; Muller, X.; Dutkowski, P. Hypothermic Machine Preservation of the Liver: State of the Art. Curr. Transplant. Rep. 2018, 5, 93–102. [Google Scholar] [CrossRef]
- Mitchell, P. Coupling of phosphorylation to electron and hydrogen transfer by a chemi-osmotic type of mechanism. Nature 1961, 191, 144–148. [Google Scholar] [CrossRef]
- Gallinat, A.; Hoyer, D.P.; Sotiropoulos, G.; Treckmann, J.; Benkoe, T.; Belker, J.; Saner, F.; Paul, A.; Minor, T. Oxygen Persufflation in Liver Transplantation Results of a Randomized Controlled Trial. Bioengineering 2019, 6. [Google Scholar] [CrossRef]
- Koetting, M.; Luer, B.; Efferz, P.; Paul, A.; Minor, T. Optimal time for hypothermic reconditioning of liver grafts by venous systemic oxygen persufflation in a large animal model. Transplantation 2011, 91, 42–47. [Google Scholar] [CrossRef]
- Murphy, M.P. How mitochondria produce reactive oxygen species. Biochem. J. 2009, 417, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.P. Understanding and preventing mitochondrial oxidative damage. Biochem. Soc. Trans. 2016, 44, 1219–1226. [Google Scholar] [CrossRef] [PubMed]
- Hirst, J.; King, M.S.; Pryde, K.R. The Production of Reactive Oxygen Species by Complex I; Portland Press Ltd.: London, UK, 2008. [Google Scholar]
- Luer, B.; Koetting, M.; Efferz, P.; Minor, T. Role of oxygen during hypothermic machine perfusion preservation of the liver. Transplant. Int. 2010, 23, 944–950. [Google Scholar] [CrossRef] [PubMed]
- Chouchani, E.T.; Pell, V.R.; Gaude, E.; Aksentijevic, D.; Sundier, S.Y.; Robb, E.L.; Logan, A.; Nadtochiy, S.M.; Ord, E.N.J.; Smith, A.C.; et al. Ischaemic accumulation of succinate controls reperfusion injury through mitochondrial ROS. Nature 2014, 515, 431–435. [Google Scholar] [CrossRef]
- Dutkowski, P.; Guarrera, J.V.; de Jonge, J.; Martins, P.N.; Porte, R.J.; Clavien, P.A. Evolving Trends in Machine Perfusion for Liver Transplantation. Gastroenterology 2019, 156, 1542–1547. [Google Scholar] [CrossRef]
- t Hart, N.A.; van der Plaats, A.; Faber, A.; Leuvenink, H.G.; Olinga, P.; Wiersema-Buist, J.; Verkerke, G.J.; Rakhorst, G.; Ploeg, R.J. Oxygenation during hypothermic rat liver preservation: An in vitro slice study to demonstrate beneficial or toxic oxygenation effects. Liver Transplant. 2005, 11, 1403–1411. [Google Scholar] [CrossRef]
- Meister, F.A.; Czigany, Z.; Bednarsch, J.; Bocker, J.; Amygdalos, I.; Morales Santana, D.A.; Rietzler, K.; Moeller, M.; Tolba, R.; Boor, P.; et al. Hypothermic Oxygenated Machine Perfusion of Extended Criteria Kidney Allografts from Brain Dead Donors: Protocol for a Prospective Pilot Study. JMIR Res. Protoc. 2019, 8, e14622. [Google Scholar] [CrossRef]
- Lurje, I.; Czigany, Z.; Bednarsch, J.; Roderburg, C.; Isfort, P.; Neumann, U.P.; Lurje, G. Treatment Strategies for Hepatocellular Carcinoma—A Multidisciplinary Approach. Int. J. Mol. Sci. 2019, 20. [Google Scholar] [CrossRef]
- Imber, C.J.; St Peter, S.D.; de Cenarruzabeitia, I.L.; Lemonde, H.; Rees, M.; Butler, A.; Clayton, P.T.; Friend, P.J. Optimisation of bile production during normothermic preservation of porcine livers. Am. J. Transplant. 2002, 2, 593–599. [Google Scholar] [CrossRef]
- Nativ, N.I.; Yarmush, G.; So, A.; Barminko, J.; Maguire, T.J.; Schloss, R.; Berthiaume, F.; Yarmush, M.L. Elevated sensitivity of macrosteatotic hepatocytes to hypoxia/reoxygenation stress is reversed by a novel defatting protocol. Liver Transplant. 2014, 20, 1000–1011. [Google Scholar] [CrossRef]
| Author | Groups | Design | N | Donors | Perfusion Setting | Primary Endpoint | Outcome and Main Findings |
|---|---|---|---|---|---|---|---|
| Guarrera et al., 2010 [61] | HMP/SCS | case-matched | 20 vs. 20 | DBD, ECD grafts excluded | Modified Medtronic PBS®; 4–8 °C; End-ischemic HMP, dual (PV+HA) | Incidence of PNF, EAD, and patient and graft survival at 1 month and 1 year | -No significant differences in PNF, EAD, and survival but shortened hospital stay, reduced peak serum AST levels, reduced serum creatinine levels -Trends towards lower incidence of NAS |
| Guarrera et al., 2014 [59] | HMP/SCS | case-matched | 31 vs. 30 | declined ECD grafts | Modified Medtronic PBS®; 4–8 °C; End-ischemic HMP, dual (PV+HA) | Incidence of PNF, EAD, and vascular complication, graft and patient survival at 1 year | -Similar EAD and 1 year patient survival but shortened hospital stay, reduced peak serum AST and creatinine levels, improved early renal function -Lower incidence of biliary complications within the first year -Strong correlation with the 2 h effluent AST and LDH and peak recipient AST. High portal pressure also correlated with severity of reperfusion injury |
| Dutkowski et al., 2014 [65] | HOPE/SCS | case-matched | 8 vs. 8 | DCD (Maastricht III) | LiverAssist; 10 °C; End-ischemic HOPE, PV perfusion | Proof of clinical application of HOPE; Can HOPE rescue DCD organs? | -Clinical application of HOPE feasible and safe, even in DCD transplantation and the outcome of perfused DCD grafts is similar to matched DBD graft performance -Similar 1-year graft and patient survival -No biliary strictures in the HOPE-DCD group -Higher 6-months GFR in the HOPE group -HOPE-DCD group showed lower hospital costs |
| Dutkowski et al., 2015 [66] | HOPE/SCS | case-matched | 25 vs. 50 DCD vs. 50 DBD | DCD (Maastricht III) | LiverAssist; 10 °C; End-ischemic HOPE, PV perfusion | Incidence and severity of biliary complications within 1 year after transplantation | -Decreased incidence of intrahepatic cholangiopathy and biliary complications in the HOPE group as well as lower rate of retransplantation for ischemic cholangiopathy and PNF -Improved 1-year graft survival in the HOPE group -Decreased peak ALT, AST, and bilirubine, less EAD, lower day 1 INR and intraoperative fresh-frozen plasma transfusions -Lower 3 and 6 months ALP and 6-months bilirubin -Trends in better renal function, ICU and hospital stay, HAT, acute rejection, and PNF -HOPE DCD livers achieved similar results as matched DBD livers in all investigated endpoints |
| van Rijn et al., 2017 [68] | DHOPE/SCS | prospective case-control study | 10 vs. 32 | DCD (Maastricht III) | LiverAssist; 10 °C; End-ischemic HOPE, dual (PV + HA) | Graft survival at 6 months after OLT (time from transplantation to retransplantation or death from graft failure) | -Higher 6 months graft survival in HOPE group vs. SCS -Safety and feasibility of dual HOPE -Increase of hepatic ATP content during HOPE and lower peak serum ALT and lower day 7 post-OLT bilirubin -Lower median ALT, gamma GT, ALP, and bilirubin serum levels 30 days after OLT -Trends to a lower incidence of NAS and in length of ICU or hospital stay -Higher incidence of hypokalemia after reperfusion in HOPE group |
| van Rijn et al., 2018 [69] | d-HOPE/SCS | prospective phase I stury | 10 vs. 20 | DCD | LiverAssist; 10 °C; End-ischemic HOPE, dual (PV + HA) | Histological biliary injury based on bile duct biopsies | -The reduced bile-duct injury and less injury of the deep peribiliary glands in d-HOPE-preserved livers |
| Schlegel et al., 2019 [67] | HOPE/SCS | case-matched | 50 vs. 50 DCD vs. 50 DBD | DCD (Maastricht III) | LiverAssist; 10–12 °C; End-ischemic HOPE, dual (PV + HA) | Post-transplant complications, and non-tumor-related patient death or graft loss | -Similar graft survival in HOPE-DCD livers like in DBD -Five-year graft survival was 94% after HOPE-DCD vs. 78% in untreated DCD |
| Patrono et al., 2019 [70] | d-HOPE/SCS | case-matched | 25 vs. 50 | DBD | LiverAssist; 10 °C; End-ischemic HOPE, dual (PV + HA) | Multiple clinical endpoints | -HOPE was associated with a lower severe post-reperfusion syndrome rate and stage 2–3 acute kidney injury -Lower transaminases peak and a lower early allograft dysfunction (EAD) rate after HOPE -A steeper decline in arterial graft resistance throughout perfusion was associated with lower EAD rate |
| van Leeuwen et al., 2019 [60] | d-HOPE-COR-NMP | prospective single arm | 16 | DCD | LiverAssist; 8–12 °C End-ischemic HOPE, dual (PV + HA), followed by COR and NMP | 3-months graft survival | -All livers (n = 11) which met viability criteria were transplanted successfully with 100% 6-months survival -Introduction of HOPE-COR-NMP increased the number of transplantations by 20% |
| Group/NCT | MP and Comp. | Design | N | Donors | Perfusion 1 | Primary Endpoint |
|---|---|---|---|---|---|---|
| Zurich, Switzerland NCT01317342 | HOPE/SCS | recruitment completed multicenter RCT | 85 vs. 85 | DBD | LiverAssist; 8–10 °C; end-ischemic HOPE, single (PV) perfusion | Major postoperative complications (Clavien grade ≥III) and CCI |
| Groningen, Netherlands NCT02584283 | DHOPE/SCS | recruitment completed multicenter RCT | 78 vs. 78 | DCD (Maastricht category III) | LiverAssist; 8–10 °C; end-ischemic dual (PV+HA) HOPE, 2 h | Incidence of NAS |
| Aachen, Germany NCT03124641 | HOPE/SCS | Recruiting multicenter RCT | 23 vs. 23 | ECD-DBD | LiverAssist; 8–10 °C; end-ischemic HOPE, single (PV) perfusion, 1(–2) h | Early graft injury (peak ALT level) |
| New Jersey, USA NCT03484455 | HMP/SCS | Recruiting multicenter RCT | 70 vs. 70 | Not stated | LifePort Liver Transporter, Temperature not stated; preservation HMP, dual perfusion from retrieval to implantation, no active oxygenation, 3–7 h | Early allograft dysfunction (EAD) |
| Lyon, France NCT03929523 | HMP/SCS | Recruiting multicenter RCT | 133 vs. 133 | ECD-DBD | LiverAssist; 8–10 °C; end-ischemic HOPE, single (PV) perfusion, 1(–2) h | Early allograft dysfunction (EAD) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Czigany, Z.; Lurje, I.; Schmelzle, M.; Schöning, W.; Öllinger, R.; Raschzok, N.; Sauer, I.M.; Tacke, F.; Strnad, P.; Trautwein, C.; et al. Ischemia-Reperfusion Injury in Marginal Liver Grafts and the Role of Hypothermic Machine Perfusion: Molecular Mechanisms and Clinical Implications. J. Clin. Med. 2020, 9, 846. https://doi.org/10.3390/jcm9030846
Czigany Z, Lurje I, Schmelzle M, Schöning W, Öllinger R, Raschzok N, Sauer IM, Tacke F, Strnad P, Trautwein C, et al. Ischemia-Reperfusion Injury in Marginal Liver Grafts and the Role of Hypothermic Machine Perfusion: Molecular Mechanisms and Clinical Implications. Journal of Clinical Medicine. 2020; 9(3):846. https://doi.org/10.3390/jcm9030846
Chicago/Turabian StyleCzigany, Zoltan, Isabella Lurje, Moritz Schmelzle, Wenzel Schöning, Robert Öllinger, Nathanael Raschzok, Igor M. Sauer, Frank Tacke, Pavel Strnad, Christian Trautwein, and et al. 2020. "Ischemia-Reperfusion Injury in Marginal Liver Grafts and the Role of Hypothermic Machine Perfusion: Molecular Mechanisms and Clinical Implications" Journal of Clinical Medicine 9, no. 3: 846. https://doi.org/10.3390/jcm9030846
APA StyleCzigany, Z., Lurje, I., Schmelzle, M., Schöning, W., Öllinger, R., Raschzok, N., Sauer, I. M., Tacke, F., Strnad, P., Trautwein, C., Neumann, U. P., Fronek, J., Mehrabi, A., Pratschke, J., Schlegel, A., & Lurje, G. (2020). Ischemia-Reperfusion Injury in Marginal Liver Grafts and the Role of Hypothermic Machine Perfusion: Molecular Mechanisms and Clinical Implications. Journal of Clinical Medicine, 9(3), 846. https://doi.org/10.3390/jcm9030846










