Assessing ICD-11 Gaming Disorder in Adolescent Gamers: Development and Validation of the Gaming Disorder Scale for Adolescents (GADIS-A)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.2.1. Gaming Disorder
2.2.2. Gaming Pattern
2.2.3. Emotional Dysregulation
2.2.4. Academic Functioning
2.3. Analysis
2.3.1. Data Management and Analytic Strategies
2.3.2. Factor Structure
2.3.3. Internal Consistency
2.3.4. Criterion Validity
2.3.5. Classification
2.3.6. Sensitivity and Specificity
3. Results
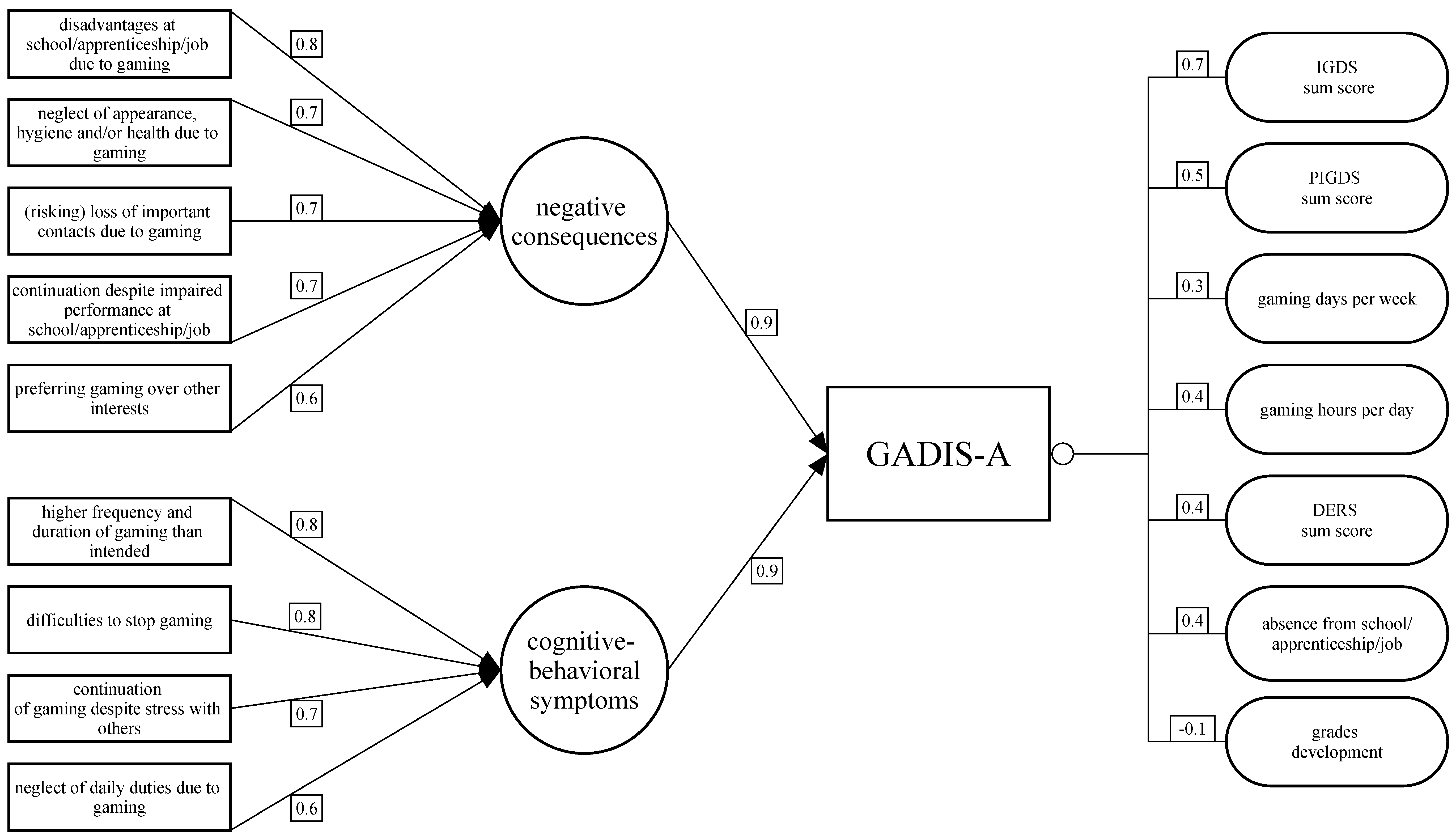
3.1. Factor Structure
3.2. Internal Consistency
3.3. Criterion Validity
3.4. Classification
3.5. Sensitivity and Specificity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Weinstein, A.; Livny, A.; Weizman, A. New developments in brain research of internet and gaming disorder. Neurosci. Biobehav. Rev. 2017, 75, 314–330. [Google Scholar] [CrossRef] [PubMed]
- Konrad, K.; Firk, C.; Uhlhaas, P.J. Brain development during adolescence: Neuroscientific insights into this developmental period. Dtsch. Arztebl. Int. 2013, 110, 425. [Google Scholar] [PubMed] [Green Version]
- Yuan, K.; Qin, W.; Yu, D.; Bi, Y.; Xing, L.; Jin, C.; Tian, J. Core brain networks interactions and cognitive control in internet gaming disorder individuals in late adolescence/early adulthood. Brain Struct. Funct. 2016, 221, 1427–1442. [Google Scholar] [CrossRef] [PubMed]
- Sugaya, N.; Shirasaka, T.; Takahashi, K.; Kanda, H. Bio-psychosocial factors of children and adolescents with internet gaming disorder: A systematic review. Biopsychosoc. Med. 2019, 13, 3. [Google Scholar] [CrossRef]
- Kökönyei, G.; Kocsel, N.; Király, O.; Griffiths, M.D.; Galambos, A.; Magi, A.; Paksi, B.; Demetrovics, Z. The Role of Cognitive Emotion Regulation Strategies in Problem Gaming Among Adolescents: A Nationally Representative Survey Study. Front. Psychiatry 2019, 10, 273. [Google Scholar] [CrossRef] [Green Version]
- Wichstrøm, L.; Stenseng, F.; Belsky, J.; von Soest, T.; Hygen, B.W. Symptoms of Internet Gaming Disorder in Youth: Predictors and Comorbidity. J. Abnorm. Child. Psychol. 2019, 47, 71–83. [Google Scholar] [CrossRef] [Green Version]
- Dreier, M.; Wölfling, K.; Duven, E.; Giralt, S.; Beutel, M.E.; Müller, K.W. Free-to-play: About addicted Whales, at risk Dolphins and healthy Minnows. Monetarization design and Internet Gaming Disorder. Addict. Behav. 2017, 64, 328–333. [Google Scholar] [CrossRef]
- Rosenkranz, T.; Müller, K.W.; Dreier, M.; Beutel, M.E.; Wölfling, K. Addictive Potential of Internet Applications and Differential Correlates of Problematic Use in Internet Gamers versus Generalized Internet Users in a Representative Sample of Adolescents. EAR 2017, 23, 148–156. [Google Scholar] [CrossRef]
- Available online: https://www.statista.com/statistics/276705/ios-app-releases-worldwide/ (accessed on 24 February 2020).
- Available online: https://de.statista.com/statistik/daten/studie/217342/umfrage/beliebteste-kategorien-im-app-store-nach-anzahl-der-apps/ (accessed on 24 February 2020).
- Available online: https://www.statista.com/statistics/276623/number-of-apps-available-in-leading-app-stores/ (accessed on 24 February 2020).
- Feierabend, S.; Rathgeb, T.; Reutter, T. JIM 2018 Jugend, Information, Medien—Basisstudie zum Medienumgang 12- bis 19-Jähriger in Deutschland; Medienpädagogischer Forschungsverband Südwest: Stuttgart, Germany, 2018. [Google Scholar]
- Veissière, S.P.L.; Stendel, M. Hypernatural Monitoring: A Social Rehearsal Account of Smartphone Addiction. Front. Psychol. 2018, 9, 141. [Google Scholar] [CrossRef] [Green Version]
- Rehbein, F.; Psych, G.; Kleimann, M.; Mediasci, G.; Mößle, T. Prevalence and Risk Factors of Video Game Dependency in Adolescence: Results of a German Nationwide Survey. Cyberpsychol. Behav. Soc. Netw. 2010, 13, 269–277. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5), 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Petry, N.M.; Rehbein, F.; Ko, C.H.; O’Brien, C.P. Internet Gaming Disorder in the DSM-5. Curr. Psychiatry Rep. 2015, 17, 72. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Diseases for Mortality and Morbidity Statistics (11th Revision). 2018. Available online: https://icd.who.int/browse11/l-m/en (accessed on 21 January 2020).
- Reed, G.M.; First, M.B.; Kogan, C.S.; Hyman, S.E.; Gureje, O.; Gaebel, W.; Maj, M.; Stein, D.J.; Maercker, A.; Tyrer, P.; et al. Innovations and changes in the ICD-11 classification of mental, behavioural and neurodevelopmental disorders. World Psychiatry 2019, 18, 3–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- King, D.L.; Chamberlain, S.R.; Carragher, N.; Billieux, J.; Stein, D.; Mueller, K.; Potenza, M.N.; Rumpf, H.J.; Saunders, J.; Starcevic, V.; et al. Screening and assessment tools for gaming disorder: A comprehensive systematic review. Clin. Psychol. Rev. 2020, 101831. [Google Scholar] [CrossRef] [PubMed]
- Montag, C.; Schivinski, B.; Sariyska, R.; Kannen, C.; Demetrovics, Z.; Pontes, H.M. Psychopathological Symptoms and Gaming Motives in Disordered Gaming-A Psychometric Comparison between the WHO and APA Diagnostic Frameworks. J. Clin. Med. 2019, 8, 1691. [Google Scholar] [CrossRef] [Green Version]
- Lemmens, J.S.; Valkenburg, P.M.; Gentile, D.A. The Internet Gaming Disorder Scale. Psychol. Assess. 2015, 27, 567–582. [Google Scholar] [CrossRef]
- Ko, C.-H.; Lin, H.-C.; Lin, P.-C.; Yen, J.-Y. Validity, functional impairment and complications related to Internet gaming disorder in the DSM-5 and gaming disorder in the ICD-11. Aust. New Zealand J. Psychiatry 2019. [Google Scholar] [CrossRef]
- Jo, Y.S.; Bhang, S.Y.; Choi, J.S.; Lee, H.K.; Lee, S.Y.; Kweon, Y.-S. Clinical Characteristics of Diagnosis for Internet Gaming Disorder: Comparison of DSM-5 IGD and ICD-11 GD Diagnosis. J. Clin. Med. 2019, 8, 945. [Google Scholar] [CrossRef] [Green Version]
- Colder Carras, M.; Kardefelt-Winther, D. When addiction symptoms and life problems diverge: A latent class analysis of problematic gaming in a representative multinational sample of European adolescents. Eur. Child. Adolesc. Psychiatry 2018, 27, 513–525. [Google Scholar] [CrossRef]
- Pontes, H.M.; Schivinski, B.; Sindermann, C.; Li, M.; Becker, B.; Zhou, M.; Montag, C. Measurement and conceptualization of Gaming Disorder according to the World Health Organization framework: The development of the Gaming Disorder Test. Int. J. Ment. Health Addict. 2019, 3, 1–21. [Google Scholar] [CrossRef] [Green Version]
- Lemmens, J.S.; Valkenburg, P.M.; Peter, J. Development and validation of a game addiction scale for adolescents. Media Psychol. 2009, 12, 77–95. [Google Scholar] [CrossRef]
- Wartberg, L.; Zieglmeier, M.; Kammerl, R. Accordance of Adolescent and Parental Ratings of Internet Gaming Disorder and Their Associations with Psychosocial Aspects. Cyberpsychol. Behav. Soc. Netw. 2019, 22, 264–270. [Google Scholar] [CrossRef]
- Wartberg, L.; Kriston, L.; Thomasius, R. The Prevalence and Psychosocial Correlates of Internet Gaming Disorder—Analysis in a nationally representative sample of 12- to 25-year-olds. Dtsch. Arztebl. Int. 2017, 114, 419–424. [Google Scholar] [PubMed] [Green Version]
- Wartberg, L.; Kriston, L.; Zieglmeier, M.; Lincoln, T.; Kammerl, R. A longitudinal study on psychosocial causes and consequences of Internet gaming disorder in adolescence. Psychol. Med. 2019, 49, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Wartberg, L.; Kriston, L.; Kramer, M.; Schwedler, A.; Lincoln, T.M.; Kammerl, R. Internet gaming disorder in early adolescence: Associations with parental and adolescent mental health. Eur. Psychiatry 2017, 43, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Aldao, A.; Nolen-Hoeksema, S.; Schweizer, S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin. Psychol. Rev. 2010, 30, 217–237. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, K.C.; Jazaieri, H.; Gross, J.J. Emotion Regulation: A Transdiagnostic Perspective on a New RDoC Domain. Cogn. Res. 2016, 40, 426–440. [Google Scholar] [CrossRef] [Green Version]
- Estévez, A.; Jáuregui, P.; Sánchez-Marcos, I.; López-González, H.; Griffiths, M.D. Attachment and emotion regulation in substance addictions and behavioral addictions. J. Behav. Addict. 2017, 6, 534–544. [Google Scholar] [CrossRef]
- Kaufman, E.A.; Xia, M.; Fosco, G.; Yaptangco, M.; Skidmore, C.R.; Crowell, S.E. The difficulties in emotion regulation scale short form (DERS-SF): Validation and replication in adolescent and adult samples. J. Psychopathol. Behav. Assess. 2016, 38, 443–455. [Google Scholar] [CrossRef]
- Gratz, K.L.; Roemer, L. Multidimensional Assessment of Emotion Regulation and Dysregulation: Development, Factor Structure, and Initial Validation of the Difficulties in Emotion Regulation Scale. J. Psychopathol. Behav. Assess. 2004, 26, 41–54. [Google Scholar] [CrossRef]
- Gutzweiler, R.; In-Albon, T. Überprüfung der Gütekriterien der deutschen Version der Difficulties in Emotion Regulation Scale in einer klinischen und einer Schülerstichprobe Jugendlicher. Z. Für Klin. Psychol. Und Psychother. 2018, 47, 274–286. [Google Scholar] [CrossRef]
- Van Buuren, S.; Groothuis-Oudshoorn, K. mice: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef] [Green Version]
- R Core Team R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019.
- Kuhn, M.; Chow, F.; Wickham, H. Rsample: General Resampling Infrastructure. 2019. Available online: https://CRAN.R-project.org/package=rsample (accessed on 11 January 2020).
- Revelle, W. Psych: Procedures for Psychological, Psychometric, and Personality Research; Northwestern University: Evanston, IL, USA, 2018. [Google Scholar]
- Rosseel, Y. lavaan: An R Package for Structural Equation Modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.-Y. Statistical notes for clinical researchers: Assessing normal distribution (2) using skewness and kurtosis. Restor. Dent. Endod. 2013, 38, 52. [Google Scholar] [CrossRef] [PubMed]
- Muthén, B. A general structural equation model with dichotomous, ordered categorical, and continuous latent variable indicators. Psychometrika 1984, 49, 115–132. [Google Scholar] [CrossRef] [Green Version]
- Browne, M.W.; Cudeck, R. Alternative Ways of Assessing Model Fit. Sociol. Methods Res. 1992, 21, 230–258. [Google Scholar] [CrossRef]
- Hooper, D.; Coughlan, J.; Mullen, M.R. Structural Equation Modelling: Guidelines for Determining Model Fit. Electron. J. Bus. Res. Methods 2008, 6, 53–60. [Google Scholar]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Modeling: A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Nunnally, J. Psychometric Theory; Mc Graw-Hill Publishing Co.: New York, NY, USA, 1978. [Google Scholar]
- Dancey, P.C.; Reidy, J. Statistics without Maths for Psychology, 5th ed.; Prentice Hall: Harlow, UK; New York, NY, USA, 2011; ISBN 978-0-273-72602-9. [Google Scholar]
- Scrucca, L.; Fop, M.; Murphy, T.B.; Raftery, A.E. mclust 5: Clustering, classification and density estimation using Gaussian finite mixture models. R J. 2016, 8, 205–233. [Google Scholar] [CrossRef] [Green Version]
- Rosenberg, J.M.; Beymer, P.N.; Anderson, D.J.; Schmidt, J.A. tidyLPA: An R Package to Easily Carry Out Latent Profile Analysis (LPA) Using Open-Source or Commercial Software. J. Open Source Softw. 2018, 3, 978. [Google Scholar] [CrossRef] [Green Version]
- Nylund, K.L.; Asparouhov, T.; Muthén, B.O. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Struct. Equ. Modeling: A Multidiscip. J. 2007, 14, 535–569. [Google Scholar] [CrossRef]
- Jedidi, K.; Jagpal, H.S.; DeSarbo, W.S. Finite-Mixture Structural Equation Models for Response-Based Segmentation and Unobserved Heterogeneity. Mark. Sci. 1997, 16, 39–59. [Google Scholar] [CrossRef]
- Yang, C.-C. Evaluating latent class analysis models in qualitative phenotype identification. Comput. Stat. Data Anal. 2006, 50, 1090–1104. [Google Scholar] [CrossRef]
- Cohen, J. The effect size index: D. Stat. Power Anal. Behav. Sci. 1988, 2, 284–288. [Google Scholar]
- Robin, X.; Turck, N.; Hainard, A.; Tiberti, N.; Lisacek, F.; Sanchez, J.-C.; Müller, M. pROC: An open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform. 2011, 12, 77. [Google Scholar] [CrossRef] [PubMed]
- Michels, R.; Siebel, U.; Freyberger, H.J.; Schönell, H.; Dilling, H. Evaluation of the Multiaxial System of ICD-10 (Preliminary Draft): Correlations between Multiaxial Assessment and Clinical Judgements of Aetiology, Treatment Indication and Prognosis. PSP 2001, 34, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Mezzich, J.E. International Surveys on the Use of ICD-10 and Related Diagnostic Systems. Psychopathology 2002, 35, 72–75. [Google Scholar] [CrossRef]
- Wakefield, J.C. DSM-5 substance use disorder: How conceptual missteps weakened the foundations of the addictive disorders field. Acta Psychiatr. Scand. 2015, 132, 327–334. [Google Scholar] [CrossRef] [Green Version]
- Hawi, N.S.; Samaha, M.; Griffiths, M.D. The Digital Addiction Scale for Children: Development and Validation. Cyberpsychol. Behav. Soc. Netw. 2019, 22, 771–778. [Google Scholar] [CrossRef]
- Mihara, S.; Higuchi, S. Cross-sectional and longitudinal epidemiological studies of Internet gaming disorder: A systematic review of the literature. Psychiatry Clin. Neurosci. 2017, 71, 425–444. [Google Scholar] [CrossRef] [Green Version]
- Lau, J.T.F.; Wu, A.M.S.; Gross, D.L.; Cheng, K.M.; Lau, M.M.C. Is Internet addiction transitory or persistent? Incidence and prospective predictors of remission of Internet addiction among Chinese secondary school students. Addict. Behav. 2017, 74, 55–62. [Google Scholar] [CrossRef]
- Wartberg, L.; Lindenberg, K. Predictors of Spontaneous Remission of Problematic Internet Use in Adolescence: A One-Year Follow-Up Study. Int. J. Environ. Res. Public Health 2020, 17, 448. [Google Scholar] [CrossRef] [Green Version]
- Cha, S.-S.; Seo, B.-K. Smartphone use and smartphone addiction in middle school students in Korea: Prevalence, social networking service, and game use. Health Psychol. Open 2018, 5, 205510291875504. [Google Scholar] [CrossRef] [PubMed]
- Haug, S.; Castro, R.P.; Kwon, M.; Filler, A.; Kowatsch, T.; Schaub, M.P. Smartphone use and smartphone addiction among young people in Switzerland. J. Behav. Addict. 2015, 4, 299–307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Menon, G. The Effects of Accessibility of Information in Memory on Judgments of Behavioral Frequencies. J. Consum. Res. 1993, 20, 431–440. [Google Scholar] [CrossRef]
- Coughlin, S.S. Recall bias in epidemiologic studies. J. Clin. Epidemiol. 1990, 43, 87–91. [Google Scholar] [CrossRef]
- Stanton, W.R.; McCLELLAND, M.; Elwood, C.; Ferry, D.; Silva, P.A. Prevalence, reliability and bias of adolescents’ reports of smoking and quitting. Addiction 1996, 91, 1705–1714. [Google Scholar] [CrossRef] [PubMed]
- Bickham, D.S.; Hswen, Y.; Rich, M. Media use and depression: Exposure, household rules, and symptoms among young adolescents in the USA. Int. J. Public Health 2015, 60, 147–155. [Google Scholar] [CrossRef] [Green Version]
- Brink, M.V.D.; Bandell-Hoekstra, E.N.G.; Abu-Saad, H.H. The Occurrence of Recall Bias in Pediatric Headache: A Comparison of Questionnaire and Diary Data. Headache: J. Head Face Pain 2001, 41, 11–20. [Google Scholar] [CrossRef]
- Available online: https://de.statista.com/statistik/daten/studie/153257/umfrage/haushalte-mit-internetzugang-in-deutschland-seit-2002/ (accessed on 14 February 2020).
- Becker, A.; Hagenberg, N.; Roessner, V.; Woerner, W.; Rothenberger, A. Evaluation of the self-reported SDQ in a clinical setting: Do self-reports tell us more than ratings by adult informants? Eur. Child. Adolesc. Psychiatry 2004, 13, ii17–ii24. [Google Scholar] [CrossRef]
- Morgan, C.J.; Cauce, A.M. Predicting DSM-III-R Disorders From the Youth Self-Report: Analysis of Data From a Field Study. J. Am. Acad. Child. Adolesc. Psychiatry 1999, 38, 1237–1245. [Google Scholar] [CrossRef]
| ICD-11 Criteria | GADIS-A Items | ||
|---|---|---|---|
| Corresponding DSM-5 Item | Thinking of the Last 12 Months, How Strongly Do You Agree with the Following Statements? | ||
| A | Impaired control over gaming (e.g., onset, frequency, intensity, duration, termination, context). | 1. | I often play games more frequently and longer than I planned to or agreed upon with my parents. 1 |
| Unsuccessful attempts to reduce or stop gaming. | 2. | I often cannot stop gaming even though it would be sensible to do so or for example my parents have told me to stop. 1 | |
| B | Increasing priority given to gaming to the extent that gaming takes precedence over other life interests and daily activities. | 3. | I often do not pursue interests outside the digital world (e.g., meeting friends or partner in real life, attending sports clubs/societies, reading books, making music) because I prefer gaming. 1 |
| Giving up other activities. | 4. | I neglect daily duties (e.g., grocery shopping, cleaning, tidying up after myself, tidying my room, obligations for school/apprenticeship/job) because I prefer gaming. 1 | |
| C | Continuation or escalation of gaming despite the occurrence of negative consequences. | 5. | I often continue gaming even though it causes me stress with others (e.g., my parents, siblings, friends, partner, teachers). 1 |
| Continuation of gaming despite problems. | 6. | I continue gaming although it harms my performance at school/apprenticeship/job (e.g., by being late, not participating in class, neglecting homework, worse grades). 1 | |
| D | The behavior pattern is of sufficient severity to result in significant impairment in personal, family, social, educational, occupational or other important areas of functioning. | 7. | Due to gaming, I neglect my appearance, my personal hygiene, and/or my health (e.g., sleep, nutrition, exercise). 1 |
| 8. | Due to gaming, I risk losing important relationships (friends, family, partner) or have lost them already. 1 | ||
| Risking or losing relationships or career opportunities due to excessive gaming. | 9. | Due to gaming I have disadvantages at school/apprenticeship/job (e.g., bad [final] grades, inability to continue to the next grade/no graduation, no apprenticeship or university spot, poor reference, warning/dismissal). 1 | |
| E | The pattern of gaming behavior may be continuous or episodic and recurrent and normally evident over a period of at least 12 months. | 10. | How often did you experience such problems, conflicts, or difficulties due to gaming during the past year? Did this only occur on single days, during longer periods of several days to weeks, or was it almost daily? 2 |
| GADIS-A Item a | Factor 1 | Factor 2 | Communalities |
|---|---|---|---|
| Item 1 EFA | 0.17 | 0.82 | 0.70 |
| Item 1 CFA | 0.93 | ||
| Item 2 EFA | 0.22 | 0.80 | 0.69 |
| Item 2 CFA | 1.00 | ||
| Item 3 EFA | 0.63 | 0.47 | 0.61 |
| Item 3 CFA | 0.92 | ||
| Item 4 EFA | 0.47 | 0.60 | 0.58 |
| Item 4 CFA | 0.94 | ||
| Item 5 EFA | 0.39 | 0.74 | 0.69 |
| Item 5 CFA | 1.02 | ||
| Item 6 EFA | 0.72 | 0.40 | 0.68 |
| Item 6 CFA | 0.98 | ||
| Item 7 EFA | 0.75 | 0.20 | 0.60 |
| Item 7 CFA | 0.95 | ||
| Item 8 EFA | 0.73 | 0.24 | 0.59 |
| Item 8 CFA | 1.00 | ||
| Item 9 EFA | 0.84 | 0.21 | 0.74 |
| Item 9 CFA | 1.00 | ||
| Proportion Variance | 0.35 | 0.30 |
| Construct | r/ϱ |
|---|---|
| IGDS sum score | 0.70 *** |
| PIGDS sum score | 0.54 *** |
| Gaming days per week | 0.28 *** |
| Gaming hours per day | 0.43 *** |
| DERS sum score (and subscale scores) | 0.50 *** (0.38–0.41 ***) |
| Days of absence | 0.20 *** |
| Grade sum score | 0.08 * |
| Grade development | −0.15 *** |
| Latent Classes | Log Likelihood | AIC | BIC | ICL | LRTS |
|---|---|---|---|---|---|
| 1 | −2921.85 | 5861.69 | −5904.07 | −5904.07 | - |
| 2 | −2924.51 | 5881.03 | −5956.36 | −5975.72 | −5.33 |
| 3 | −2052.60 | 4151.19 | −4259.48 | −4259.48 | 1743.84 *** |
| 4 | −1892.55 | 3845.10 | −3986.34 | −3986.75 | 320.09 *** |
| 5 | −1892.55 | 3859.10 | −4033.30 | −4371.93 | 0.00 |
| Variables | Hazardous Gamers (HG) | Intensive Gamers (IG) | Pathological Gamers (PG) | Light Gamers (LG) | Post-Hoc Tests (χ2/Scheffé) a | Cramér’s V/Cohen’s d |
|---|---|---|---|---|---|---|
| Absolute frequency | 16 | 481 | 46 | 276 | --- | --- |
| Relative frequency in % [95%-CI] | 1.95 [1.0; 2.9] | 58.73 [55.4; 62.1] | 5.62 [4.0; 7.2] | 33.7 [30.5; 36.9] | --- | --- |
| Age mean (SE) | 11.81 (0.55) | 12.98 (0.11) | 12.91 (0.28) | 13.10 (0.15) | --- | --- |
| Female sex in % [95%-CI] | 25.00 [3.8;46.2] | 34.72 [30.5;39.0] | 30.43 [17.14;43.7] | 52.17 [46.3;58.1] | 0.29 n.s. | --- |
| 0.01 n.s. | --- | |||||
| n.s. | --- | |||||
| 0.18 n.s. | --- | |||||
| 21.36 *** | 0.17 | |||||
| 6.61 puncorr = 0.01 | 0.15 | |||||
| GADIS-A factor 1 score mean (SE) | 1.50 (0.38) | 2.90 (0.15) | 11.00 (0.11) | 0.55 (0.08) | 1.40 n.s. | --- |
| 9.50*** | 2.12 | |||||
| −0.95 n.s. | --- | |||||
| 8.10 *** | 2.27 | |||||
| −2.35 *** | 0.84 | |||||
| −10.45 *** | 4.67 | |||||
| GADIS-A factor 2 score mean (SE) | 8.19 (0.84) | 6.79 (0.14) | 11.98 (0.44) | 1.30 (0.08) | −1.40 n.s. | --- |
| 3.79 *** | 1.23 | |||||
| −6.89 *** | 4.62 | |||||
| 5.19 *** | 1.72 | |||||
| −5.49 *** | 2.16 | |||||
| −0.68 *** | 6.48 | |||||
| Frequency of GD symptoms score mean (SE) | 2.44 (0.13) | 1.00 (0.00) | 2.48 (0.07) | 0.00 (0.00) | −1.43 *** | 14.38 |
| 0.04 | --- | |||||
| −2.44 *** | 20.92 | |||||
| 1.48 *** | 9.58 | |||||
| −1.00 *** | 27.56 | |||||
| −2.48 *** | 13.09 | |||||
| IGDS sum score mean (SE) | 5 (0.65) | 2.75 (0.11) | 6.7 (6.33) | 0.55 (1.88) | −2.25 *** | 0.96 |
| 1.70 n.s. | --- | |||||
| −4.45 *** | 3.67 | |||||
| 3.95 *** | 1.68 | |||||
| −2.20 *** | 1.11 | |||||
| −6.15 *** | 4.54 | |||||
| PIGDS sum score mean (SE) | 5.56 (0.59) | 3.04 (0.11) | 6.33 (0.42) | 1.18 (0.11) | −2.52 *** | 1.01 |
| 0.76 n.s. | --- | |||||
| −4.38 *** | 2.36 | |||||
| 3.29 *** | 1.3 | |||||
| −1.86 *** | 0.82 | |||||
| −5.15 *** | 2.57 | |||||
| Gaming days per week mean (SE) | 5.88 (0.33) | 5.54 (0.99) | 5.93 (0.28) | 4.42 (0.13) | −0.34 n.s. | --- |
| 0.06 n.s. | --- | |||||
| −1.45 puncorr = 0.04 | 0.68 | |||||
| 0.40 n.s. | --- | |||||
| −1.12 *** | 0.56 | |||||
| −1.51 *** | 0.71 | |||||
| Gaming hours per day mean (SE) | 171.75 (41.91) | 136.76 (5.03) | 215.55 (25.27) | 76.76 (3.84) | −34.99 n.s. | --- |
| 43.80 n.s. | --- | |||||
| −94.99 * | 1.3 | |||||
| 78.80 *** | 0.67 | |||||
| −60.00 *** | 0.62 | |||||
| −138.79 *** | 1.59 | |||||
| DERS sum score mean (SE) | 49.69 (3.39) | 41.88 (0.53) | 54.89 (1.79) | 34.02 (0.61) | −7.81 n.s. | --- |
| 5.20 n.s. | --- | |||||
| −15.67 *** | 1.52 | |||||
| 13.01 *** | 1.11 | |||||
| −7.86 *** | 0.7 | |||||
| −20.87 *** | 2 | |||||
| Days of absence mean (SE) | 2.38 (0.75) | 1.89 (0.19) | 5.61 (1.19) | 1.51 (0.18) | −0.48 n.s. | --- |
| 3.23 n.s. | --- | |||||
| −0.87 n.s. | --- | |||||
| 3.72 *** | 0.8 | |||||
| −0.38 n.s. | --- | |||||
| −4.10 *** | 1 | |||||
| Grades sum mean (SE) | 6.06 (0.55) | 6.37 (0.11) | 6.70 (0.43) | 6.06 (0.14) | --- | --- |
| Grades development mean (SE) | 3.38 (0.18) | 3.14 (0.03) | 2.78 (0.11) | 3.28 (0.04) | −0.23 n.s. | --- |
| −0.59 puncor r = 0.02 | 0.79 | |||||
| −0.10 n.s. | 0.14 | |||||
| −0.36 * | 0.56 | |||||
| 0.14 puncorr = 0.05 | 0.21 | |||||
| 0.50 *** | 0.73 |
| Variables | No GD | GD | χ2/Scheffé | Cramer’s V/Cohen’s d |
|---|---|---|---|---|
| Absolute frequency | 789 | 30 | - | - |
| Relative frequency [95% CI] | 96.34 [95.05, 97.62] | 3.66 [2.38; 4.95] | - | - |
| Mean age (SE) | 12.98 (0.08) | 13.30 (0.36) | - | - |
| Female sex [95% CI] | 40.68 [37.26, 44.11] | 26.67 [10.84; 42.49] | - | - |
| GADIS-A factor 1 score mean (SE) | 2.13 (0.11) | 13.30 (0,78) | 11.17 *** | 3.57 |
| GADIS-A factor 2 score mean (SE) | 4.94 (0.13) | 13.53 (0.39) | 8.59 *** | 2.34 |
| Frequency score of GD symptoms mean (SE) | 0.70 (0.02) | 2.63 (0.09) | 1.93 *** | 3.31 |
| IGDS sum score mean (SE) | 2.08 (0.08) | 7.47 (0.39) | 5.39 *** | 2.32 |
| PIGDS sum score mean (SE) | 2.50 (0.09) | 6.47 (0.55) | 3.97 *** | 1.55 |
| Gaming days per week mean (SE) | 5.15 (0.07) | 6.33 (0.29) | 1.19 ** | 0.58 |
| Gaming hours per day mean (SE) | 117.7 (19.4) | 225.52 (26.01) | 107.82 *** | 1.00 |
| DERS sum score mean (SE) | 39.47 (0.43) | 57.00 (2.31) | 17.53 *** | 1.46 |
| Days of absence mean (SE) | 1.79 (0.13) | 7.03 (1.72) | 5.24 *** | 1.28 |
| Grades sum mean (SE) | 6.26 (0.09) | 6.83 (0.59) | - | - |
| Grades development mean (SE) | 3.19 (0.02) | 2.67 (0.12) | −0.52 *** | 0.81 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paschke, K.; Austermann, M.I.; Thomasius, R. Assessing ICD-11 Gaming Disorder in Adolescent Gamers: Development and Validation of the Gaming Disorder Scale for Adolescents (GADIS-A). J. Clin. Med. 2020, 9, 993. https://doi.org/10.3390/jcm9040993
Paschke K, Austermann MI, Thomasius R. Assessing ICD-11 Gaming Disorder in Adolescent Gamers: Development and Validation of the Gaming Disorder Scale for Adolescents (GADIS-A). Journal of Clinical Medicine. 2020; 9(4):993. https://doi.org/10.3390/jcm9040993
Chicago/Turabian StylePaschke, Kerstin, Maria Isabella Austermann, and Rainer Thomasius. 2020. "Assessing ICD-11 Gaming Disorder in Adolescent Gamers: Development and Validation of the Gaming Disorder Scale for Adolescents (GADIS-A)" Journal of Clinical Medicine 9, no. 4: 993. https://doi.org/10.3390/jcm9040993





