No Autopsies on COVID-19 Deaths: A Missed Opportunity and the Lockdown of Science
Abstract
:1. Background
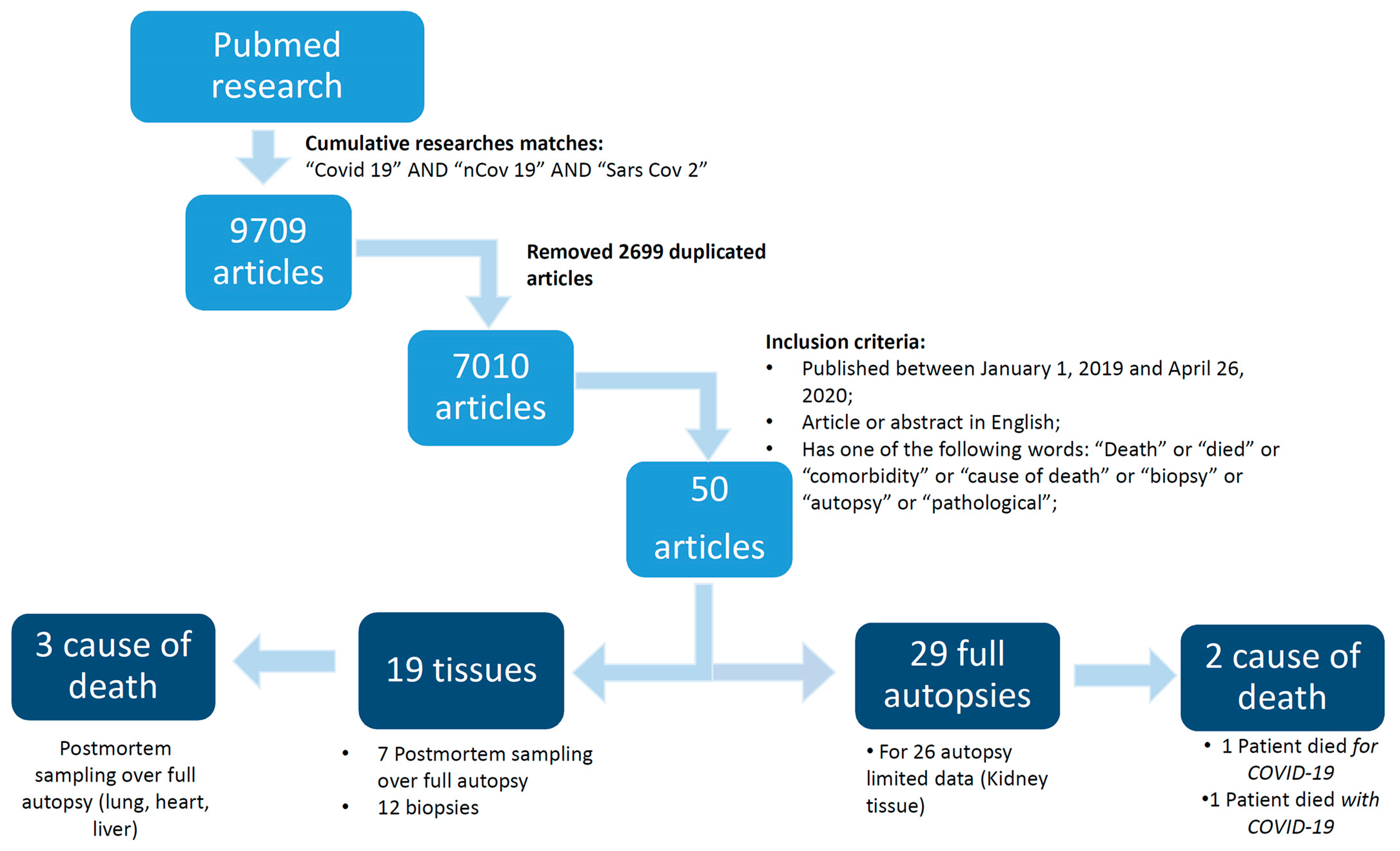
2. Methods
2.1. Database Search Terms and Timeline
2.2. Study Selection
3. Results
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chan, J.F.W.; Yuan, S.; Kok, K.H.; To, K.K.W.; Chu, H.; Yang, J.; Xing, F.; Liu, J.; Yip, C.C.Y.; Poon, R.W.S.; et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 2020. [Google Scholar] [CrossRef] [Green Version]
- Messina, G.; Polito, R.; Monda, V.; Cipolloni, L.; Di Nunno, N.; Di Mizio, G.; Murabito, P.; Carotenuto, M.; Messina, A.; Pisanelli, D.; et al. Functional Role of Dietary Intervention to Improve the Outcome of COVID-19: A Hypothesis of Work. Int. J. Mol. Sci. 2020, 21, 3104. [Google Scholar] [CrossRef] [PubMed]
- Nishiura, H.; Jung, S.M.; Linton, N.M.; Kinoshita, R.; Yang, Y.; Hayashi, K.; Kobayashi, T.; Yuan, B.; Akhmetzhanov, A.R. Akhmetzhanov The Extent of Transmission of Novel Coronavirus in Wuhan, China, 2020. J. Clin. Med. 2020, 9, 330. [Google Scholar] [CrossRef] [Green Version]
- Buja, L.M.; Barth, R.F.; Krueger, G.R.; Brodsky, S.V.; Hunter, R.L. The Importance of the Autopsy in Medicine: Perspectives of Pathology Colleagues. Acad. Pathol. 2019. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwartz, D.A.; Herman, C.J. The importance of the autopsy in emerging and reemerging infectious diseases. Clin. Infect. Dis. 1996. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng, D.L.; Al Hosani, F.; Keating, M.K.; Gerber, S.I.; Jones, T.L.; Metcalfe, M.G.; Tong, S.; Tao, Y.; Alami, N.N.; Haynes, L.M.; et al. Clinicopathologic, immunohistochemical, and ultrastructural findings of a fatal case of middle east respiratory syndrome coronavirus infection in the United Arab Emirates, April 2014. Am. J. Pathol. 2016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, L.; Callinan, L.S.; Holman, R.C.; Blau, D.M. Determinants for autopsy after unexplained deaths possibly resulting from infectious causes, United States. Emerg. Infect. Dis. 2012. [Google Scholar] [CrossRef]
- Peng, Y.D.; Meng, K.; Guan, H.Q.; Leng, L.; Zhu, R.R.; Wang, B.Y.; He, M.A.; Cheng, L.X.; Huang, K.Z.Q. Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV. Chin. J. Cardiovasc. Dis. 2020, 48. [Google Scholar] [CrossRef]
- Tian, S.; Hu, W.; Niu, L.; Liu, H.; Xu, H.; Xiao, S.-Y. Pulmonary pathology of early phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. J. Thorac. Oncol. 2020. [Google Scholar] [CrossRef]
- Guan, W.; Ni, Z.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.S.; et al. Clinical characteristics of 2019 novel coronavirus infection in China. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Xu, Z.; Shi, L.; Wang, Y.; Zhang, J.; Huang, L.; Zhang, C.; Liu, S.; Zhao, P.; Liu, H.; Zhu, L.; et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020. [Google Scholar] [CrossRef]
- Kui, L.; Fang, Y.-Y.; Deng, Y.; Liu, W.; Wang, M.-F.; Ma, J.-P.; Xiao, W.; Wang, Y.-N.; Zhong, M.-H.; Li, C.-H.; et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin. Med. J. (Engl) 2020. [Google Scholar] [CrossRef]
- Wang, W.; Tang, J.; Wei, F. Updated understanding of the outbreak of 2019 novel coronavirus (2019-nCoV) in Wuhan, China. J. Med. Virol. 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Xia, J.; Liu, H.; Wu, Y.; Zhang, L.; Yu, Z.; Fang, M.; et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 2020. [Google Scholar] [CrossRef] [Green Version]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020. [Google Scholar] [CrossRef] [Green Version]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA - J. Am. Med. Assoc. 2020. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Cao, W.; Xiao, M.; Li, Y.J.; Yang, Y.; Zhao, J.; Zhou, X.; Jiang, W.; Zhao, Y.Q.; Zhang, S.Y.; et al. Clinical and coagulation characteristics of 7 patients with critical COVID-2019 pneumonia and acro-ischemia. Zhonghua Xue Ye Xue Za Zhi 2020. [Google Scholar] [CrossRef]
- Analysis on 54 mortality cases of Coronavirus disease 2019 in the Republic of Korea from January 19 to March 10, 2020. J. Korean Med. Sci. 2020. [CrossRef] [Green Version]
- Yuan, M.; Yin, W.; Tao, Z.; Tan, W.; Hu, Y. Association of radiologic findings with mortality of patients infected with 2019 novel coronavirus in Wuhan, China. PLoS ONE 2020. [Google Scholar] [CrossRef] [Green Version]
- Guo, T.; Fan, Y.; Chen, M.; Wu, X.; Zhang, L.; He, T.; Wang, H.; Wan, J.; Wang, X.; Lu, Z. Cardiovascular Implications of Fatal Outcomes of Patients with Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Y.K.; Peng, S.; Li, L.Q.; Wang, Q.; Ping, W.; Zhang, N.; Fu, X.N. Clinical and Transmission Characteristics of Covid-19 — A Retrospective Study of 25 Cases from a Single Thoracic Surgery Department. Curr. Med. Sci. 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, T.; Wu, D.; Chen, H.; Yan, W.; Yang, D.; Chen, G.; Ma, K.; Xu, D.; Yu, H.; Wang, H.; et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study. BMJ 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020. [Google Scholar] [CrossRef]
- Deng, Y.; Liu, W.; Liu, K.; Fang, Y.Y.; Shang, J.; Zhou, L.; Wang, K.; Leng, F.; Wei, S.; Chen, L.; et al. Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 (COVID-19) in Wuhan, China: a retrospective study. Chin. Med. J. (Engl) 2020. [Google Scholar] [CrossRef]
- Rodriguez-Morales, A.J.; Cardona-Ospina, J.A.; Gutiérrez-Ocampo, E.; Villamizar-Peña, R.; Holguin-Rivera, Y.; Escalera-Antezana, J.P.; Alvarado-Arnez, L.E.; Bonilla-Aldana, D.K.; Franco-Paredes, C.; Henao-Martinez, A.F.; et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Guan, W.; Liang, W.; Zhao, Y.; Liang, H.; Chen, Z.; Li, Y.; Liu, X.; Chen, R.; Tang, C.; Wang, T.; et al. Comorbidity and its impact on 1590 patients with Covid-19 in China: A Nationwide Analysis. Eur. Respir. J. 2020. [Google Scholar] [CrossRef] [Green Version]
- Bhatraju, P.K.; Ghassemieh, B.J.; Nichols, M.; Kim, R.; Jerome, K.R.; Nalla, A.K.; Greninger, A.L.; Pipavath, S.; Wurfel, M.M.; Evans, L.; et al. Covid-19 in Critically Ill Patients in the Seattle Region — Case Series. N. Engl. J. Med. 2020. [Google Scholar] [CrossRef]
- Zhang, L.; Zhu, F.; Xie, L.; Wang, C.; Wang, J.; Chen, R.; Jia, P.; Guan, H.Q.; Peng, L.; Chen, Y.; et al. Clinical characteristics of COVID-19-infected cancer patients: A retrospective case study in three hospitals within Wuhan, China. Ann. Oncol. 2020. [Google Scholar] [CrossRef]
- Lescure, F.X.; Bouadma, L.; Nguyen, D.; Parisey, M.; Wicky, P.H.; Behillil, S.; Gaymard, A.; Bouscambert-Duchamp, M.; Donati, F.; Le Hingrat, Q.; et al. Clinical and virological data of the first cases of COVID-19 in Europe: a case series. Lancet. Infect. Dis. 2020. [Google Scholar] [CrossRef] [Green Version]
- Wu, C.; Chen, X.; Cai, Y.; Xia, J.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Zhou, X.; Du, C.; et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Antonelli, M.; Cabrini, L.; Castelli, A.; Cereda, D.; Coluccello, A.; Foti, G.; Fumagalli, R.; et al. Baseline Characteristics and Outcomes of 1591 Patients Infected with SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA - J. Am. Med. Assoc. 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mi, B.; Chen, L.; Xiong, Y.; Xue, H.; Zhou, W.; Liu, G. Characteristics and Early Prognosis of COVID-19 Infection in Fracture Patients. J. Bone Jt. Surg. 2020. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Dai, Z.; Mo, P.; Li, X.; Ma, Z.; Song, S.; Chen, X.; Luo, M.; Liang, K.; Gao, S.; et al. Clinical characteristics and outcomes of older patients with coronavirus disease 2019 (COVID-19) in Wuhan, China (2019): a single-centered, retrospective study. Journals Gerontol. Ser. A 2020. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Wang, L.; Yan, S.; Yang, F.; Xiang, L.; Zhu, J.; Shen, B.; Gong, Z. Clinical characteristics of 25 death cases with COVID-19: a retrospective review of medical records in a single medical center, Wuhan, China. Int. J. Infect. Dis. 2020. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Tu, W.J.; Cheng, W.; Yu, L.; Liu, Y.K.; Hu, X.; Liu, Q. Clinical Features and Short-term Outcomes of 102 Patients with Corona Virus Disease 2019 in Wuhan, China. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Wang, L.; He, W.; Yu, X.; Hu, D.; Bao, M.; Liu, H.; Zhou, J.; Jiang, H. Coronavirus disease 2019 in elderly patients: Characteristics and prognostic factors based on 4-week follow-up. J. Infect. 2020. [Google Scholar] [CrossRef]
- Barton, L.M.; Duval, E.J.; Stroberg, E.; Ghosh, S.; Mukhopadhyay, S. COVID-19 Autopsies, Oklahoma, USA. Am. J. Clin. Pathol. 2020. [Google Scholar] [CrossRef] [Green Version]
- Huang, J.; Lin, H.; Wu, Y.; Fang, Y.; Kumar, R.; Chen, G.; Lin, S. COVID-19 in posttransplant patients—report of 2 cases. Am. J. Transplant. 2020. [Google Scholar] [CrossRef]
- Ling, L.; So, C.; Shum, H.P.; Chan, P.K.S.; Lai, C.K.C.; Kandamby, D.H.; Ho, E.; So, D.; Yan, W.W.; Lui, G.; et al. Critically ill patients with COVID-19 in Hong Kong: A multicentre retrospective observational cohort study. Crit. Care Resusc. 2020, 32248675, Online ahead of print. [Google Scholar]
- Cheng, Y.; Luo, R.; Wang, K.; Zhang, M.; Wang, Z.; Dong, L.; Li, J.; Yao, Y.; Ge, S.; Xu, G. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020. [Google Scholar] [CrossRef] [PubMed]
- Du, R.H.; Liang, L.R.; Yang, C.Q.; Wang, W.; Cao, T.Z.; Li, M.; Guo, G.Y.; Du, J.; Zheng, C.L.; Zhu, Q.; et al. Predictors of Mortality for Patients with COVID-19 Pneumonia Caused by SARS-CoV-2: A Prospective Cohort Study. Eur. Respir. J. 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barrasa, H.; Rello, J.; Tejada, S.; Martín, A.; Balziskueta, G.; Vinuesa, C.; Fernández-Miret, B.; Villagra, A.; Vallejo, A.; Sebastián, A.S.; et al. SARS-Cov-2 in Spanish Intensive Care: Early Experience with 15-day Survival In Vitoria. Anaesth. Crit. Care Pain Med. 2020. [Google Scholar] [CrossRef]
- Lovell, N.; Maddocks, M.; Etkind, S.N.; Taylor, K.; Carey, I.; Vora, V.; Marsh, L.; Higginson, I.J.; Prentice, W.; Edmonds, P.; et al. Characteristics, symptom management and outcomes of 101 patients with COVID-19 referred for hospital palliative care. J. Pain Symptom Manage. 2020. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Liu, W.; Zhao, J.; Lu, Y.; Wang, X.; Yu, C.; Hu, S.; Shen, N.; Liu, W.; Sun, Z.; et al. Clinical characteristics of 80 hospitalized frontline medical workers infected with COVID-19 in Wuhan, China. J. Hosp. Infect. 2020. [Google Scholar] [CrossRef]
- Zhang, G.; Hu, C.; Luo, L.; Fang, F.; Chen, Y.; Li, J.; Peng, Z.; Pan, H. Clinical features and short-term outcomes of 221 patients with COVID-19 in Wuhan, China. J. Clin. Virol. 2020. [Google Scholar] [CrossRef]
- Magro, C.; Mulvey, J.J.; Berlin, D.; Nuovo, G.; Salvatore, S.; Harp, J.; Baxter-Stoltzfus, A.; Laurence, J. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Transl. Res. 2020. [Google Scholar] [CrossRef]
- Pereira, M.R.; Mohan, S.; Cohen, D.J.; Husain, S.A.; Dube, G.K.; Ratner, L.E.; Arcasoy, S.; Aversa, M.M.; Benvenuto, L.J.; Dadhani, D.; et al. COVID-19 in Solid Organ Transplant Recipients: Initial Report from the US Epicenter. Am. J. Transplant. 2020. [Google Scholar] [CrossRef]
- Li, J.; Wang, X.; Chen, J.; Zuo, X.; Zhang, H.; Deng, A. COVID-19 infection may cause ketosis and ketoacidosis. Diabetes Obes. Metab. 2020. [Google Scholar] [CrossRef]
- Yang, F.; Shi, S.; Zhu, J.; Shi, J.; Dai, K.; Chen, X. Analysis of 92 deceased patients with COVID-19. J. Med. Virol. 2020. [Google Scholar] [CrossRef] [Green Version]
- Cai, Y.; Hao, Z.; Gao, Y.; Ping, W.; Wang, Q.; Peng, S.; Zhao, B.; Sun, W.; Zhu, M.; Li, K.; et al. Coronavirus Disease 2019 in the Perioperative Period of Lung Resection: A Brief Report From a Single Thoracic Surgery Department in Wuhan, People’s Republic of China. J. Thorac. Oncol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Karami, P.; Naghavi, M.; Feyzi, A.; Aghamohammadi, M.; Novin, M.S.; Mobaien, A.; Qorbanisani, M.; Karami, A.; Norooznezhad, A.H. Mortality of a pregnant patient diagnosed with COVID-19: A case report with clinical, radiological, and histopathological findings. Travel Med. Infect. Dis. 2020, 101665. [Google Scholar] [CrossRef] [PubMed]
- Tian, S.; Xiong, Y.; Liu, H.; Niu, L.; Guo, J.; Liao, M.; Xiao, S.-Y. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod. Pathol. 2020. [Google Scholar] [CrossRef] [Green Version]
- Fabre, O.; Rebet, O.; Carjaliu, I.; Radutoiu, M.; Gautier, L.; Hysi, I. Severe Acute Proximal Pulmonary Embolism and COVID-19: A Word of Caution. Ann. Thorac. Surg. 2020. [Google Scholar] [CrossRef] [PubMed]
- Su, H.; Yang, M.; Wan, C.; Yi, L.X.; Tang, F.; Zhu, H.Y.; Yi, F.; Yang, H.C.; Fogo, A.B.; Nie, X.; et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020. [Google Scholar] [CrossRef] [PubMed]
- Edrada, E.M.; Lopez, E.B.; Villarama, J.B.; Salva Villarama, E.P.; Dagoc, B.F.; Smith, C.; Sayo, A.R.; Verona, J.A.; Trifalgar-Arches, J.; Lazaro, J.; et al. First COVID-19 infections in the Philippines: A case report. Trop. Med. Health 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hang, L.; Yan, X.; Fan, Q.; Liu, H.; Liu, X.; Liu, Z.; Zhang, Z. D-dimer levels on admission to predict in-hospital mortality in patients with Covid-19. J. Thromb. Haemost. 2020. [Google Scholar] [CrossRef]
- Zheng, Y.-Y.; Ma, Y.-T.; Zhang, J.-Y.; Xie, X. COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 2020. [Google Scholar] [CrossRef] [Green Version]
- Rotzinger, D.C.; Beigelman-Aubry, C.; von Garnier, C.; Qanadli, S.D. Pulmonary embolism in patients with COVID-19: Time to change the paradigm of computed tomography. Thromb. Res. 2020, 190, 58–59. [Google Scholar] [CrossRef]
- Klok, F.A.; Kruip, M.J.H.A.; van der Meer, N.J.M.; Arbous, M.S.; Gommers, D.A.M.P.J.; Kant, K.M.; Kaptein, F.H.J.; van Paassen, J.; Stals, M.A.M.; Huisman, M.V.; et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb. Res. 2020. [Google Scholar] [CrossRef]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 2020. [Google Scholar] [CrossRef]
- World Health Organization. Infection Prevention and Control for the safe management of a dead body in the context of COVID-19. Interim guidance: 24 March 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/331538/WHO-COVID-19-lPC_DBMgmt-2020.1-eng.pdf (accessed on 27 March 2020).
- Italian Ministry of Health. Emergency Indications Related to the COVID-19 Epidemic Concerning the Funeral Sector, Cemetery, and Cremation. Circular of General Direction of Health Prevention. 2020. Available online: http://www.trovanorme.salute.gov.it/norme/renderNormsanPdf?anno=2020&codLeg=73965&parte=1%20&serie=null (accessed on 3 May 2020).
- Hanley, B.; Lucas, S.B.; Youd, E.; Swift, B.; Osborn, M. Autopsy in suspected COVID-19 cases. J. Clin. Pathol. 2020. [Google Scholar] [CrossRef] [Green Version]
- Pomara, C.; Volti, G.L.; Cappello, F. COVID-19 Deaths: Are We Sure It Is Pneumonia? Please, Autopsy, Autopsy, Autopsy! J. Clin. Med. 2020, 9, 1259. [Google Scholar] [CrossRef] [PubMed]
- De Cock, K.M.; Zielinski-Gutiérrez, E.; Lucas, S.B. Learning from the Dead. N. Engl. J. Med. 2019. [Google Scholar] [CrossRef]
- Vetter, P.; Fischer, W.A.; Schibler, M.; Jacobs, M.; Bausch, D.G.; Kaiser, L. Ebola Virus Shedding and Transmission: Review of Current Evidence. J. Infect. Dis. 2016. [Google Scholar] [CrossRef] [PubMed]
- Castillo, P.; Martínez, M.J.; Ussene, E.; Jordao, D.; Lovane, L.; Ismail, M.R.; Carrilho, C.; Lorenzoni, C.; Fernandes, F.; Bene, R.; et al. Validity of a Minimally Invasive Autopsy for Cause of Death Determination in Adults in Mozambique: An Observational Study. PLoS Med. 2016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kreuels, B.; Wichmann, D.; Emmerich, P.; Schmidt-Chanasit, J.; De Heer, G.; Kluge, S.; Sow, A.; Renné, T.; Günther, S.; Lohse, A.W.; et al. A case of severe Ebola virus infection complicated by gram-negative septicemia. N. Engl. J. Med. 2014. [Google Scholar] [CrossRef] [PubMed]
- Kreuels, B.; Addo, M.M.; Schmiedel, S. Severe Ebola virus infection complicated by gram-negative septicemia. N. Engl. J. Med. 2015. [Google Scholar] [CrossRef]
- Petrosillo, N.; Nicastri, E.; Lanini, S.; Capobianchi, M.R.; Di Caro, A.; Antonini, M.; Puro, V.; Lauria, F.N.; Shindo, N.; Magrini, N.; et al. Ebola virus disease complicated with viral interstitial pneumonia: A case report. BMC Infect. Dis. 2015. [Google Scholar] [CrossRef] [Green Version]
- Varkey, J.B.; Shantha, J.G.; Crozier, I.; Kraft, C.S.; Lyon, G.M.; Mehta, A.K.; Kumar, G.; Smith, J.R.; Kainulainen, M.H.; Whitmer, S.; et al. Persistence of ebola virus in ocular fluid during convalescence. N. Engl. J. Med. 2015. [Google Scholar] [CrossRef] [Green Version]
- Brief Report: Persistence of Ebola Virus in Ocular Fluid during Convalescence. N. Engl. J. Med. 2015. [CrossRef]
- Francis, T.I.; Moore, D.L.; Edington, G.M.; Smith, J.A. A clinicopathological study of human yellow fever. Bull. World Health Organ. 1972, 46, 659. [Google Scholar] [PubMed]
- Duarte-Neto, A.N.; Monteiro, R.A.; Johnsson, J.; Cunha, M.; Pour, S.Z.; Saraiva, A.C.; Ho, Y.L.; da Silva, L.F.F.; Mauad, T.; Zanotto, P.M.; et al. Ultrasound-guided minimally invasive autopsy as a tool for rapid post-mortem diagnosis in the 2018 Sao Paulo yellow fever epidemic: Correlation with conventional autopsy. PLoS Negl. Trop. Dis. 2019. [Google Scholar] [CrossRef] [Green Version]
- Burton, J.L.; Underwood, J. Clinical, educational, and epidemiological value of autopsy. Lancet 2007. [Google Scholar] [CrossRef]
- Franks, T.J.; Chong, P.Y.; Chui, P.; Galvin, J.R.; Lourens, R.M.; Reid, A.H.; Selbs, E.; Mcevoy, C.P.L.; Hayden, C.D.L.; Fukuoka, J.; et al. Lung pathology of severe acute respiratory syndrome (SARS): A study of 8 autopsy cases from Singapore. Hum. Pathol. 2003. [Google Scholar] [CrossRef]
- Roosen, J.; Frans, E.; Wilmer, A.; Knockaert, D.C.; Bobbaers, H. Comparison of premortem clinical diagnoses in critically ill patients and subsequent autopsy findings. Mayo Clin. Proc. 2000. [Google Scholar] [CrossRef]
- Kotovicz, F.; Mauad, T.; Saldiva, P.H.N. Clinico-pathological discrepancies in a general university hospital in São Paulo, Brazil. Clinics 2008. [Google Scholar] [CrossRef] [Green Version]
- Combes, A.; Mokhtari, M.; Couvelard, A.; Trouillet, J.L.; Baudot, J.; Hénin, D.; Gibert, C.; Chastre, J. Clinical and Autopsy Diagnoses in the Intensive Care Unit: A Prospective Study. Arch. Intern. Med. 2004. [Google Scholar] [CrossRef] [Green Version]
- Edwards, J.E. The Autopsy: Do We Still Need It? Chest 1970, 57, 113–114. [Google Scholar] [CrossRef]

| Author | Number of Patients | Patients Who Died | Average Age (Years) | Comorbidities | Severe Complications | Tissues (Biopsy or Autopsy Samples) | Autopsy |
|---|---|---|---|---|---|---|---|
| Peng Y. D. et al. [8] | 112 | 17 | Data not available | Coronary heart disease (CHD) (100%), BMI >25 (88.24%) | Data not available | 0 | 0 |
| Tian S. et al. [9] | 2 | 2 | 78.5 | lung cancer (100%), hypertension (100%), diabetes (50%) | Respiratory failure, coma, heart failure | 2 (biopsy) | 0 |
| Guan W. J. et al. [10] | 1099 | 15 | 47 | Hypertension (15%), diabetes (7.4%), CHD (2.5%), HCV (2.1%), chronic obstructive pulmonary disease (COPD) (1.1%), cancer (0.9%) | Septic shock, acute respiratory distress syndrome (ARDS), kidney failure | 0 | 0 |
| Xu Z. et al. [11] | 1 | 1 | 50 | Data not available | Respiratory failure, ARDS | 1 (autoptic sample) | 0 |
| Kui K. et al. [12] | 137 | 16 | 57 | Hypertension (9.5%), diabetes (10.2%), CHD (7.3%), COPD (1.5%), cancer (1.5%) | Data not available | 0 | 0 |
| Wang W. et al. [13] | 571 | 17 | 73 | Hypertension (41.2%), diabetes (23.5%), CHD (17.6%), stroke (17.6%), COPD (11.7%), kidney failure (11.7%), Parkinson (11.7%), cancer (5.9%), cirrhosis (5.9%) | Data not available | 0 | 0 |
| Yang X. et al. [14] | 201 | 32 | 59.7 | CHD (9%), COPD (6%), diabetes (22%), cancer (3%), stroke (22%) | ARDS, kidney failure, heart failure, liver failure | 0 | 0 |
| Huang C. et al. [15] | 41 | 6 | 49 | Diabetes (20%), hypertension (15%), cardiovascular disease (CVD) (15%) | Respiratory distress syndrome (29%), RNAaemia (15%), acute cardiac injury (12%), secondary infection (10%) | 0 | 0 |
| Wang D. et al. [16] | 138 | 6 | 56 | Hypertension (31.2%), diabetes (10.1%), CVD (14.5%), Cancer (7.2%) | ARDS, arrhythmia, shock. | 0 | 0 |
| Chen N. et al. [17] | 99 | 11 | 55.5 | CVD and cerebrovascular diseases (40%), digestive system disease (11%), endocrine system disease (13%), cancer (1%), nervous system disease (1%), respiratory system disease (1%) | ARDS (17%), kidney failure (3%), respiratory failure (8%), Septic shock (4%) | 0 | 0 |
| Zhang et al. [18] | 7 | 5 | 59 | Not indicated | Acro-ischemia presentations including finger/toe cyanosis, skin bulla and dry gangrene (100%), definite disseminated intravascular coagulation (DIC) (4 (57%)) | 0 | 0 |
| Korean Society of Infectious Diseases et al. [19] | 54 | 54 | 75.5 | CVD (59.3%); diabetes mellitus (DM) (29.6%); neurological disease (18.5%); lung disease (13.0%); malignancy (13.0%); psychologic disease (13.0%); renal disease (9.3%); hepatic disease (3.7%); kidney transplant recipient (1.9%) | Data not available | 0 | 0 |
| Yuan et al. [20] | 27 | 10 | 60 | Hypertension (19%); diabetes (22%); CVD (11%); tumor (4%); cerebral infarction (4%); chronic gastritis (4%) | ARDS (41%) | 0 | 0 |
| Guo et al. [21] | 187 | 43 | 58.5 | Hypertension (32.6%); CHD (11.2%); cardiomyopathy (8 (4.3%)); diabetes (15.0%); COPD (2.1); malignant neoplasm (7.0%); chronic kidney disease (CKD) (3.2%) | ARDS (24.6%), malignant arrhythmias (5.9%) including ventricular tachycardia/ventricular fibrillation, acute coagulopathy (34.1%), acute liver injury (15.4%) and acute kidney injury (14.6%) | 0 | 0 |
| Yang et al. [22] | 25 | 5 | 60.2 | Hypertension (15.4%); diabetes (7.7%); COPD (38.5%); CHD (30.8%) | Data not available | 0 | 0 |
| Chen et al. [23] | 274 | 113 | 62 | Hypertension (34%); diabetes (17%); CVD (8%); CHD (<1%); COPD (7%); malignancy (3%); hepatitis B (4%); cerebrovascular disease (1%); CKD (1%); gastrointestinal diseases (1%); metabolic arthritis (1%); autoimmune disease (1%) | ARDS (72%), type I respiratory failure (27%), acute cardiac injury (44%), heart failure (24%), hypoxic encephalopathy (9%), sepsis (65%), acidosis (12%), alkalosis (28%), acute kidney injury (11%), disseminated intravascular coagulation (8%), hyperkalemia (23%), shock (17%), acute liver injury (5%), gastrointestinal bleeding (<1%). | 0 | 0 |
| Zhuo et al. [24] | 191 | 54 | Data not available | Data not available | Sepsis (59%), respiratory failure (54%), ARDS (31%), heart failure (23%), septic shock (20%), coagulopathy (19%), acute cardiac injury (17%), acute kidney injury (15%), secondary infection (15%), hypoproteinemia (12%), acidosis (9%) | 0 | 0 |
| Deng et al. [25] | 225 | 109 | 69 | Hypertension (36.7%); lung disease (20.2%); diabetes (15.6%); heart disease (11.9%); malignancy (5.5%); others (28.4%) | ARDS (7.6%), acute cardiac injury (0.8%), acute kidney injury (<1%), shock (<1%), and disseminated intravascular coagulation (DIC) (<1%) | 0 | 0 |
| Rodriguez-Morales et al. [26] | 2874 | 632 | 51.97 | Hypertension (18.6%); CVD (14.4%); diabetes (11.9%); COPD (1.8%); malignancies (2.5%); chronic liver disease (CLD) (3.0%) | 20.3% who required ICU: ARDS (32.8%), cardiac injury (13.0%), acute kidney injury (7.9%), shock (6.2%), Secondary infections (5.6%). | 0 | 0 |
| Guan et al. [27] | 1590 | 50 | 48.9 | Hypertension (16.7%); CVD (53.7%), cerebrovascular disease (1.9%), diabetes (8.2%), hepatitis B (1.8%), COPD (1.5%), CKD (1.3%), malignncy (1.1%) | Data not available | 0 | 0 |
| Bhatraju et al. [28] | 24 | 12 | 64 | Asthma (14%), CKD (21%), COPD (4%), tobacco smoker (22%), diabetes (58%), | Data not available | 0 | 0 |
| Zhang et al. [29] | 28 | 8 | 65 | Cancer (100%), diabetes 4(14.3%), COPD 1 (3.6%) | ARDS 8 (28.6%), septic shock 1 (3.6%), suspected pulmonary embolism 2 (7.1%), AMI 1 (3.6%) | 0 | 0 |
| Lescure et al. [30] | 5 | 1 | 47 | Hypertension 1 (20%), cancer 1 (20%), gout 1 (20%) | Data not available | 0 | 0 |
| Wu et al. [31] | 201 | 44 | 51 | Hypertension (19.4%) diabetes (10.9%) CVD (4.0%) liver disease (3.5%) nervous system disease (3.5%) chronic lung disease (2.5%) CKD (1.0%) endocrine system disease (1.0%) tumor (0.5%) | Data not available | 0 | 0 |
| Grasselli et al. [32] | 1591 | 405 | 63 | Hypertension (49%); CVD (21%); hypercholesterolemia (18%); DM (17); malignancy (8%); COPD (4%); CKD (3%); CLD (3%); other (20%) | Data not available | 0 | 0 |
| Bobin et al. [33] | 10 | 4 | 68.4 | Fracture (100%); hypertension (40%); diabetes (30%); COPD (10%); osteoporosis (30%); CHD (10%); cirrhosis (10%), alzheimer disease (10%); brain injury (10%) | Data not available | 0 | 0 |
| Chen et al. [34] | 203 | 26 | 54 | Hypertension (21.2%); diabetes (7.9%); CVD (7.9%); cerebrovascular disease (4.4%); malignancy (3,4%); CLD (3.9%); CKD (8 (3.9%)); COPD (8 (3.9%)); Tuberculosis (4 (2.0%)); HIV (2 (0.1%)) | Cause of Death: ARDS (14%); ARDS with MOD (22%); sepsis/Shock (4%); heart failure (2%); myocardial infarction (6%); tumor (4%); intestinal bleeding (2%); | 0 | 0 |
| Li et al. [35] | 25 | 25 | 73 | Hypertension (64%); diabetes (40%); heart diseases (32%); kidney diseases (20%); cerebral infarction (16%); COPD (8%); malignant tumors (8%); acute pancreatitis (4%) | Respiratory failure (100%) | 0 | 0 |
| Cao et al. [36] | 102 | 17 | 54 | Hypertension (27.5%); diabetes (10.8%); cerebrovascular disease (5.9%); CVD (4.9%); respiratory diseases (9.8%); malignancy (3.9%); CKD (3.9%); CLD (2.0%); | Shock (9.8%); ARDS (19.6%); acute infection (16.7%); acute cardiac injury (14.7%); arrhythmia (17.6%); acute kidney injury (19.6%); acute liver injury (33.3%); lymphopenia (76.5%); Cause of Death: multiple organ dysfunction syndrome (MODS) (58.8%); ARDS (5.9%); cardiac arrest (23.5%); respiratory failure (11.8%) | 0 | 0 |
| Wang et al. [37] | 339 | 65 | 71 | Hypertension (40.8%), diabetes (16.0%), CVD (15.7%) | Lymphocytopenia (63.2%), bacterial infection (42.8%), liver enzyme abnormalities (28.7%), acute respiratory distress syndrome (21.0%) | 0 | 0 |
| Barton et al. [38] | 2 | 2 | 77 | Hypertension, splenectomy, cholelithiasis, osteoarthritis | Cause of Death: COVID-19 (ARDS—diffuse alveolar damage (DAD)) | 0 | 2 |
| 42 | Myotonic, muscular dystrophy | Complications of hepatic cirrhosis (aspiration acute bacterial bronchopneumonia) | |||||
| Huang et al. [39] | 2 | 2 | 54.5 | Transplantation (100%) | Nosocomial bacterial infection (100%); respiratory organ failure (100%); kidney organ failure (100%); heart organ failure (50%) | 0 | 0 |
| Ling et al. [40] | 8 | 1 | 64.5 | Data not available | Respiratory failure (75%); kidney failure (25%) | 0 | 0 |
| Cheng et al. [41] | 701 | 113 | 63 | Any comorbidity (42.6%); CKD (2.0%); COPD (1.9%); hypertension (33.4%); diabetes (14.3%); tumor (4.6%) | Acute kidney injury (5.1%) | 0 | 0 |
| Du et al. [42] | 179 | 21 | 57.6 | Hypertension (32.4%); CVD or cerebrovascular diseases (16.2%); diabetes (18.4%); chronic digestive disorders (11.7%); tuberculosis (4.5%); chronic hepatic or renal insufficiency (2.2%); Peripheral vascular disease (2.2%); malignancy (2.2%) | Data not available | 0 | 0 |
| Barrasa et al. [43] | 48 | 14 | 63 | Obesity (48%); arterial hypertension (44%); COPD (37%); | Hypoxemic respiratory failure (100%) | 0 | 0 |
| Lovell et al. [44] | 101 | 75 | 82 | Hypertension (54%); diabetes (36%); dementia (31%); cancer (25%); COPD (22%); renal failure (21%); congestive heart failure (18%); stroke / neurological disorder (12%); peripheral vascular disorder (4%); liver disease (2%); | Data not available | 0 | 0 |
| Wang et al. [45] | 80 | 1 | 39 | Hypertension (12.5%); diabetes (1.25%); CVD (2.5%); cerebrovascular disease (1.25%); COPD 1 (1.25%); renal disease (3.75%); liver disease (2.5%) | Data not available | 0 | 0 |
| Zhang et al. [46] | 221 | 12 | 55 | Hypertension (24.4%), diabetes (10.0%), CVD (10.0%), cerebrovascular disease (6.8%), COPD (2.7%), CKD (2.7%), CLD (3.2%), malignancy (4.1%), immunosuppression treatment (1.4%) | ARDS (21.7); arrhythmia (10.9); acute cardiac injury (7.7); shock (6.8); AKI (4.5) | 0 | 0 |
| Magro et al. [47] | 5 | 2 | 54.6 | Coronary artery disease, diabetes mellitus, heart failure, hepatitis C virus infection, end-stage renal disease, obesity (n = 2), and pre-diabetes, | Respiratory failure (n = 5); purpuric skin rash (n = 3) | 3 cases skin biopsies | 2 Cases, limited autopsy |
| Pereira et al. [48] | 90 | 16 | 57 | HTN (64%); diabetes (46%); CKD (63%); dialysis (6%); chronic lung disease (19%); HIV (1%); active cancer (3%); BMI >40 Kg/m2 (6%) | Data not available | 0 | 0 |
| Li et al. [49] | 658 | 64 | 47 | Cerebrovascular disease (8%); coronary heart disease (8.9%); heart failure (1.21%); diabetes (19.6%); hypertension (33.4%); digestive disorder (13.22%); COPD (2.88%); cancer (2.58%); CKD (2.73%); hepatitis (1.06%) | Ketosis (6.38%); acute liver injury (5.92%); septic shock (5.31%); ARDS (14.43%); diabetic ketoacidosis (DKA) (0.4%); acidosis (4.55%) | 0 | 0 |
| Yang et al. [50] | 92 | 91 | 69.8 | Hypertension (55.43%); heart disease (17.39%); cerebrovascular (10.8%); malignancy (4.34%); CLD (3.26%); CKD (2.17%); COPD (1%) | Cause of death: ARDS (79.34%), septic shock (7.6%), myocardial infarction (6.52%), heart failure (2.17%), MODS (2.17%) | 0 | 0 |
| Cai et al. [51] | 7 | 3 | 61 | COPD (28.5%); CVD (42.8%); interstitial lung disease (14.28%); hyperlipidemia (14.28%); Malignancy (100%) | Cause of death: respiratory failure 3 | 7 Biopsies | 0 |
| Karami et al. [52] | 1 | 1 | 27 | No underlying disease | Data not available | 0 | 1 |
| Tian et al. [53] | 4 | 4 | 73 | Chronic lymphocytic leukemia (CLL), cirrhosis, hypertension, diabetes, and renal transplantation | Data not available | 4 (Autopsy samples) | 0 |
| Fabre et al. [54] | 1 | 1 | 45 | Obesity (BMI 40.4), hypertension | Pulmonary Embolism | 0 | 0 |
| Su et al. [55] | 26 | 26 | 69 | History of hypertension or diabetes or both (42.3%) | Data not available | 26 (Kidney autopsy samples) | 0 |
| Edrada et al. [56] | 2 | 2 | 42 | Data not available | Data not available | 0 | 0 |
| Zhang et al. [57] | 343 | 13 | 62 | Diabetes (13.7%), hypertension (22.15%), CHD (5.5%), COPD (2.33%), cancer (2.62%), stroke history (2.33%), CLD (1.74%) | Data not available | 0 | 0 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salerno, M.; Sessa, F.; Piscopo, A.; Montana, A.; Torrisi, M.; Patanè, F.; Murabito, P.; Li Volti, G.; Pomara, C. No Autopsies on COVID-19 Deaths: A Missed Opportunity and the Lockdown of Science. J. Clin. Med. 2020, 9, 1472. https://doi.org/10.3390/jcm9051472
Salerno M, Sessa F, Piscopo A, Montana A, Torrisi M, Patanè F, Murabito P, Li Volti G, Pomara C. No Autopsies on COVID-19 Deaths: A Missed Opportunity and the Lockdown of Science. Journal of Clinical Medicine. 2020; 9(5):1472. https://doi.org/10.3390/jcm9051472
Chicago/Turabian StyleSalerno, Monica, Francesco Sessa, Amalia Piscopo, Angelo Montana, Marco Torrisi, Federico Patanè, Paolo Murabito, Giovanni Li Volti, and Cristoforo Pomara. 2020. "No Autopsies on COVID-19 Deaths: A Missed Opportunity and the Lockdown of Science" Journal of Clinical Medicine 9, no. 5: 1472. https://doi.org/10.3390/jcm9051472
APA StyleSalerno, M., Sessa, F., Piscopo, A., Montana, A., Torrisi, M., Patanè, F., Murabito, P., Li Volti, G., & Pomara, C. (2020). No Autopsies on COVID-19 Deaths: A Missed Opportunity and the Lockdown of Science. Journal of Clinical Medicine, 9(5), 1472. https://doi.org/10.3390/jcm9051472










