Accuracy of Different Indexes of Body Composition and Adiposity in Identifying Metabolic Syndrome in Adult Subjects with Prader-Willi Syndrome
Abstract
:1. Introduction
2. Patients and Methods
2.1. Study Population
2.2. Anthropometric Data
2.3. Blood Pressure Measurements and Instrumental Examinations
2.4. Laboratory Analyses
2.5. Definitions
2.6. Statistical Analysis
3. Results
Correlations
4. Discussion
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Borruel, S.; Molto, J.F.; Alpanes, M.; Fernandez-Duran, E.; Alvarez-Blasco, F.; Luque-Ramirez, M.; Escobar-Morreale, H.F. Surrogate markers of visceral adiposity in young adults: Waist circumference and body mass index are more accurate than waist hip ratio, model of adipose distribution and visceral adiposity index. PLoS ONE 2014, 9, e114112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Obesity and Overweight. 2011. Available online: http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed on 1 April 2020).
- Kim, S.H.; Després, J.P.; Koh, K.K. Obesity and cardiovascular disease: Friend or foe? Eur. Heart J. 2016, 37, 3560–3568. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allison, D.B.; Zhu, S.K.; Plankey, M.; Faith, M.S.; Heo, M. Differential associations of body mass index and adiposity with all cause mortality among men in the first and second National Health and Nutrition Examination Surveys (NHANES I and NHANES II) follow-up studies. Int. J. Obes. Relat. Metab. Disord. 2002, 26, 410–416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peterson, C.M.; Su, H.; Thomas, D.M.; Heo, M.; Golnabi, A.H.; Pietrobelli, A.; Heymsfield, S.B. Tri-Ponderal Mass Index vs Body Mass Index in Estimating Body Fat During Adolescence. JAMA Pediatr. 2017, 171, 629–636. [Google Scholar] [CrossRef]
- Rankinen, T.; Kim, S.Y.; Perusse, L.; Despres, J.P.; Bouchard, C. The prediction of abdominal visceral fat level from body composition and anthropometry: ROC analysis. Int. J. Obes. Relat. Metab. Disord. 1999, 23, 801–809. [Google Scholar] [CrossRef] [Green Version]
- Amato, M.C.; Giordano, C.; Galia, M.; Criscimanna, A.; Vitabile, S.; Midiri, M.; Galluzzo, A. Visceral Adiposity Index: A reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care 2010, 33, 920–922. [Google Scholar] [CrossRef] [Green Version]
- Browning, L.M.; Hsieh, S.D.; Ashwell, M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr. Res. Rev. 2010, 23, 247–269. [Google Scholar] [CrossRef] [Green Version]
- VanItallie, T.B.; Yang, M.U.; Heymsfield, S.B.; Funk, R.C.; Boileau, R.A. Height-normalized indices of the body’s fat-free mass and fat mass: Potentially useful indicators of nutritional status. Am. J. Clin. Nutr. 1990, 52, 953–959. [Google Scholar] [CrossRef] [Green Version]
- Mooney, S.J.; Baecker, A.; Rundle, A.G. Comparison of anthropometric and body composition measures as predictors of components of the metabolic syndrome in a clinical setting. Obes. Res. Clin. Pract. 2013, 7, e55–e66. [Google Scholar] [CrossRef]
- Radetti, G.; Fanolla, A.; Grugni, G.; Lupi, F.; Sartorio, A. Indexes of adiposity and body composition in the prediction of metabolic syndrome in obese children and adolescents: Which is the best? Nutr. Metab. Cardiovasc Dis. 2019, 29, 1189–1196. [Google Scholar] [CrossRef]
- Butler, M.G.; Hartin, S.N.; Hossain, W.A.; Manzardo, A.M.; Kimonis, V.; Dykens, E.; Gold, J.A.; Kim, S.J.; Weisensel, N.; Tamura, R.; et al. Molecular genetic classification in Prader-Willi syndrome: A multisite cohort study. J. Med. Genet. 2019, 56, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Cassidy, S.B.; Schwartz, S.; Miller, J.L.; Driscoll, D.J. Prader–Willi syndrome. Genet. Med. 2012, 14, 10–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Theodoro, M.F.; Talebizadeh, Z.; Butler, M.G. Body composition and fatness patterns in Prader–Willi syndrome: Comparison with simple obesity. Obesity 2006, 14, 1685–1690. [Google Scholar] [CrossRef] [PubMed]
- Grugni, G.; Crinò, A.; Bedogni, G.; Cappa, M.; Sartorio, A.; Corrias, A.; Di Candia, S.; Gargantini, L.; Iughetti, L.; Pagano, C.; et al. Metabolic syndrome in adult patients with Prader-Willi syndrome. Nutr. Metab. Cardiovasc Dis. 2013, 23, 1134–1140. [Google Scholar] [CrossRef] [PubMed]
- Angulo, M.A.; Butler, M.G.; Cataletto, M.E. Prader–Willi syndrome: A review of clinical, genetic, and endocrine findings. J. Endocrinol Invest. 2015, 38, 249–1263. [Google Scholar] [CrossRef] [Green Version]
- Shepherd, J.A.; Ng, B.K.; Sommer, M.J.; Heymsfield, S.B. Body composition by DXA. Bone 2017, 104, 101–105. [Google Scholar] [CrossRef]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S. Homeostasis model assessment: Insulin resistance and b-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef] [Green Version]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr. Harmonizing the metabolic syndrome. A Joint Interim Statement of the International Diabetes Federation Task Force on epidemiology and prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C., Jr.; et al. American Heart Association; National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: An American Heart Association/ National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [Green Version]
- American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2019. Diabetes Care 2019, 42, S13–S28. [Google Scholar] [CrossRef] [Green Version]
- Chen, C. Growth charts of body mass index (BMI) with quantile regression. In Proceedings of the international conference on algorithmic mathematics and computer science, Las Vegas, NV, USA, 20–23 July 2005; Volume 5, pp. 114–120. [Google Scholar]
- Cole, T.J.; Freeman, J.V.; Preece, M.A. British 1990 growth reference centiles for weight, height, body mass index and head circumference fitted by maximum penalized likelihood. Stat. Med. 1998, 17, 407–429. [Google Scholar] [CrossRef]
- Katzmarzyk, P.T.; Srinivasan, S.R.; Chen, W.; Malina, R.M.; Bouchard, C.; Berenson, G.S. Body mass index, waist circumference, and clustering of cardiovascular disease risk factors in a biracial sample of children and adolescents. Pediatrics 2004, 114, e198–e205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Youden, W.J. Index for rating diagnostic tests. Cancer 1950, 3, 32–35. [Google Scholar] [CrossRef]
- Proffitt, J.; Osann, K.; McManus, B.; Kimonis, V.E.; Heinemann, J.; Butler, M.G.; Stevenson, D.A.; Gold, J.A. Contributing factors of mortality in Prader-Willi syndrome. Am. J. Med. Genet. A 2019, 179, 196–205. [Google Scholar] [CrossRef] [PubMed]
- Pacoricona Alfaro, D.L.; Lemoine, P.; Ehlinger, V.; Molinas, C.; Diene, G.; Valette, M.; Pinto, G.; Coupaye, M.; Poitou-Bernert, C.; Thuilleaux, D.; et al. Causes of death in Prader-Willi syndrome: Lessons from 11 years’ experience of a national reference center. Orphanet J. Rare Dis. 2019, 14, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Neill, S.; O’Driscoll, L. Metabolic syndrome: A closer look at the growing epidemic and its associated pathologies. Obes. Rev. 2015, 16, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Sherling, D.H.; Perumareddi, P. Hennekens CH. Metabolic Syndrome. J Cardiovasc. Pharmacol. Ther. 2017, 22, 365–367. [Google Scholar] [CrossRef]
- Brambilla, P.; Crinò, A.; Bedogni, G.; Bosio, L.; Cappa, M.; Corrias, A.; Delvecchio, M.; Di Candia, S.; Gargantini, L.; Grechi, E.; et al. Genetic Obesity Study Group of the Italian Society of Pediatric Endocrinology and Diabetology (ISPED). Metabolic syndrome in children with Prader-Willi syndrome: The effect of obesity. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 269–276. [Google Scholar]
- Coupaye, M.; Lorenzini, F.; Lloret-Linares, C.; Molinas, C.; Pinto, G.; Diene, G.; Mimoun, E.; Demeer, G.; Labrousse, F.; Jauregi, J.; et al. Growth hormone therapy for children and adolescents with Prader-Willi syndrome is associated with improved body composition and metabolic status in adulthood. J. Clin. Endocrinol. Metab. 2013, 98, E328–E335. [Google Scholar] [CrossRef] [Green Version]
- Liu, P.; Ma, F.; Lou, H.; Liu, Y. The utility of fat mass index vs. body mass index and percentage of body fat in the screening of metabolic syndrome. BMC Public Health 2013, 13, 629. [Google Scholar] [CrossRef] [Green Version]
- Barazzoni, R.; Gortan Cappellari, G.; Semolic, A.; Ius, M.; Zanetti, M.; Gabrielli, A.; Vinci, P.; Guarnieri, G.; Simon, G. Central adiposity markers, plasma lipid profile and cardiometabolic risk prediction in overweight-obese individuals. Clin. Nutr. 2019, 38, 1171–1179. [Google Scholar] [CrossRef] [PubMed]
- Powell, M.; Lara, J.; Mocciaro, G.; Prado, C.M.; Battezzati, A.; Leone, A.; Tagliabue, A.; de Amicis, R.; Vignati, L.; Bertoli, S.; et al. Association between ratio indexes of body composition phenotypes and metabolic risk in Italian adults. Clin. Obes. 2016, 6, 365–375. [Google Scholar] [CrossRef] [PubMed] [Green Version]

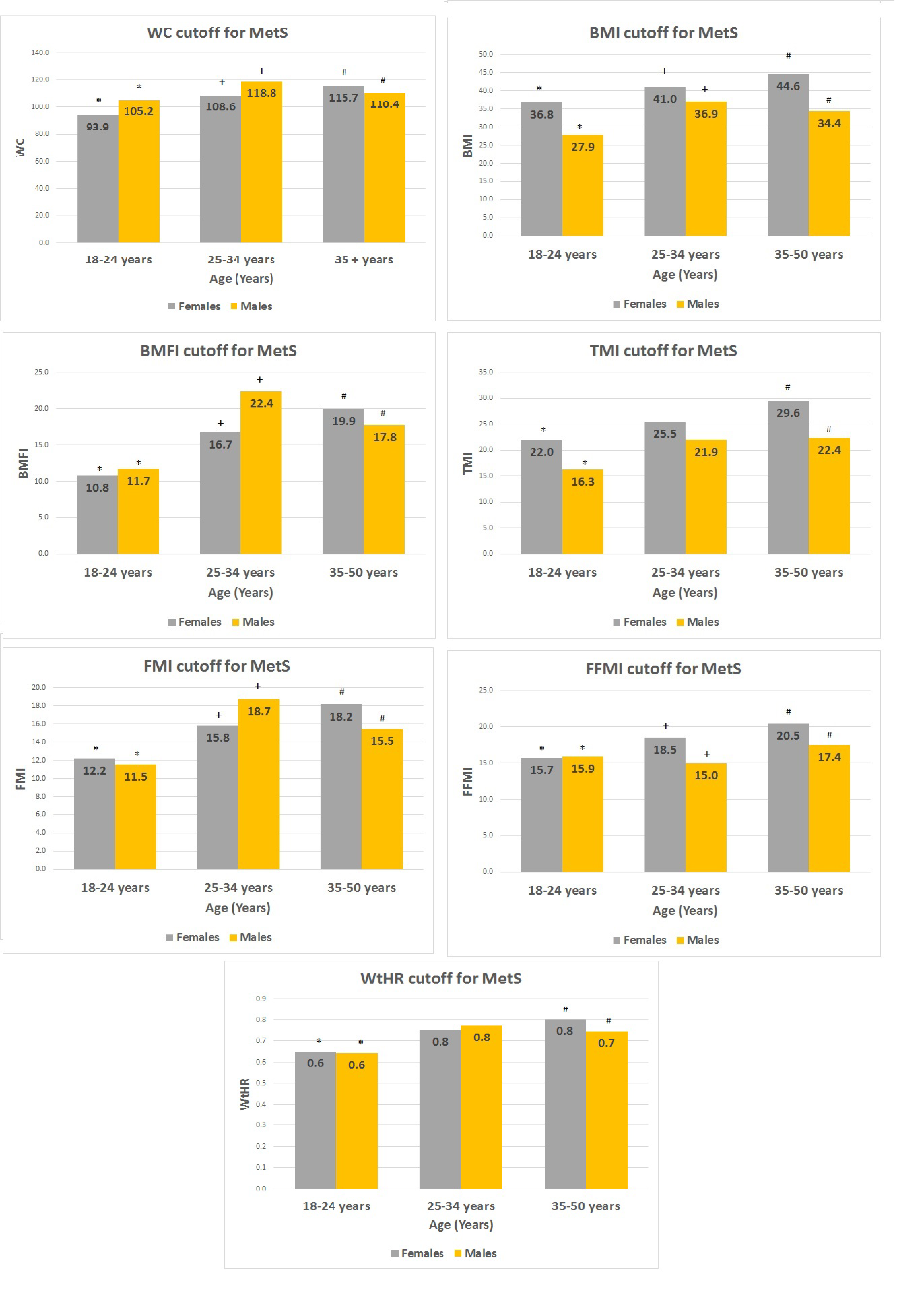
| Number of Subjects | Total | Females | Males |
|---|---|---|---|
| 120 | 69 | 51 | |
| Age yrs | 29.0 ± 9.1 | 29.5 ± 8.3 | 28.3 ± 10.1 |
| BMI | 36.7 ± 9.9 | 38.2 ± 10.5 | 34.7 ± 8.9 |
| TMI | 24.1 ± 7.2 | 25.8 ± 7.6 | 21.9 ± 5.9 ° |
| BMFI | 22.2 ± 11.2 | 23.9 ± 11.9 | 19.9 ± 9.8 |
| FMI | 18.4 ± 7.0 | 19.9 ± 7.2 | 16.3 ± 6.2 ° |
| WtHR | 0.7 ± 0.1 | 0.7 ± 0.1 | 0.7 ± 0.1 |
| FFMI | 17.0 ± 3.2 | 16.9 ± 3.4 | 17.1 ± 3.0 |
| WC (cm) | 111.0 ± 18.5 | 110.3 ± 19.8 | 112.0 ± 16.7 |
| SBP (mm/Hg) | 120.3 ± 9.5 | 119.8 ± 9.6 | 121.1 ± 9.3 |
| DBP (mm/Hg) | 76.3 ± 6.0 | 76.1 ± 6.5 | 76.7 ± 5.4 |
| HDL-C (mg/dl) | 51.9 ± 14.9 | 54.9 ± 15.2 | 47.9 ± 13.7 * |
| TG (mg/dl) | 101.2 ± 56.6 | 100.6 ± 65.5 | 101.9 ± 42.3 |
| glycemia (mg/dl) | 96.4 ± 40.3 | 102.8 ± 51.4 | 87.8 ± 11.7 * |
| HbA1c | 5.8 ± 1.2 | 6.0 ± 1.5 | 5.5 ± 0.6 * |
| Number of Subjects | No MetS | MetS | ||
|---|---|---|---|---|
| Females | Males | Females | Males | |
| 41 | 34 | 28 | 17 | |
| Age yr | 28.1 ± 8.7 | 26.5 ± 9.2 | 31.7 ± 7.4 | 31.8 ± 11.1 |
| BMI | 34.2 ± 8.7 | 32.2 ± 9.1 | 44.1 ± 10.2 | 39.8 ± 5.7 |
| TMI | 23.1 ± 6.5 | 20.2 ± 6.1 | 29.7 ± 7.5 | 25.2 ± 3.8 & |
| BMFI | 19.2 ± 9.6 | 17.2 ± 9.9 | 30.9 ± 11.6 | 25.3 ± 7.2 |
| FMI | 17.3 ± 6.4 | 14.6 ± 6.4 | 23.6 ± 6.7 | 19.6 ± 4.1 & |
| WtHR | 0.7 ± 0.1 | 0.7 ± 0.1 | 0.8 ± 0.1 | 0.8 ± 0.1 |
| FFMI | 15.5 ± 2.3 | 16.4 ± 3.0 | 19.0 ± 3.8 | 18.6 ± 2.3 |
| WC (cm) | 101.3 ± 17.2 | 107.0 ± 15.9 | 124 ± 15.8 | 121.9 ± 14.1 |
| SBP (mm/Hg) | 116.0 ± 8.0 | 117.1 ± 7.3 | 125.4 ± 9.2 | 129.1 ± 7.8 |
| DBP (mm/Hg) | 74.4 ± 7.1 | 76.0 ± 5.5 | 78.6 ± 4.5 | 77.9 ± 5.3 |
| HDL-C (mg/dl) | 60.2 ± 14.3 | 50.9 ± 12.6 * | 47.1 ± 13.1 | 41.9 ± 14.4 |
| TG (mg/dl) | 81.0 ± 34.2 | 94.3 ± 40.8 | 129.3 ± 87.3 | 117.2 ± 42.2 |
| glycemia (mg/dl) | 84.6 ± 11.1 | 85.1 ± 8.4 | 129.3 ± 72.4 | 93.2 ± 15.4 & |
| HbA1c | 5.4 ± 0.4 | 5.4 ± 0.5 | 4.4 ± 0.5 | 5.9 ± 0.6 & |
| insulin | 8.7 ± 5.6 | 9.3 ± 4.2 | 11.6 ± 5.3 | 17.4 ± 10.4 & |
| Females MetS− vs. MetS+ | Males MetS− vs. MetS+ | |
|---|---|---|
| BMI | p < 0.0001 | p < 0.01 |
| WC | p < 0.0001 | p < 0.01 |
| WHtR | p < 0.0001 | p < 0.01 |
| FMI | p < 0.001 | p < 0.01 |
| FFMI | p < 0.0001 | p < 0.05 |
| TMI | p < 0.001 | p < 0.01 |
| BMFI | p < 0.0001 | p < 0.01 |
| TG (mg/dl) | p < 0.01 | n.s. |
| HDL-C | p < 0.001 | p < 0.05 |
| HOMA-IR | p < 0.01 | p < 0.01 |
| SBP | p < 0.0001 | p < 0.0001 |
| DBP | p < 0.01 | n.s. |
| HbA1c | p < 0.001 | p < 0.01 |
| glycemia 0′ | p < 0.01 | n.s. |
| glycemia 120′ | p < 0.05 | p < 0.01 |
| insulin 0′ | p = 0.05 | p < 0.01 |
| Females | Males | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity | Specificity | PPV | NPV | LR+ | LR− | Sensitivity | Specificity | PPV | NPV | LR+ | LR− | |
| BMI | 0.61 | 0.78 | 0.65 | 0.74 | 2.77 | 0.50 | 0.88 | 0.59 | 0.52 | 0.91 | 2.14 | 0.20 |
| TMI | 0.71 | 0.66 | 0.59 | 0.77 | 2.09 | 0.43 | 0.94 | 0.56 | 0.52 | 0.95 | 2.13 | 0.11 |
| BMFI | 0.96 | 0.44 | 0.54 | 0.95 | 1.72 | 0.08 | 0.88 | 0.62 | 0.54 | 0.91 | 2.31 | 0.19 |
| FMI | 0.96 | 0.39 | 0.52 | 0.94 | 1.58 | 0.09 | 0.88 | 0.65 | 0.56 | 0.92 | 2.50 | 0.18 |
| FFMI | 0.57 | 0.90 | 0.80 | 0.76 | 5.86 | 0.47 | 0.88 | 0.53 | 0.48 | 0.90 | 1.88 | 0.22 |
| WC | 0.89 | 0.61 | 0.61 | 0.89 | 2.29 | 0.18 | 0.82 | 0.56 | 0.48 | 0.86 | 1.87 | 0.32 |
| WtHR | 0.86 | 0.66 | 0.63 | 0.87 | 2.51 | 0.22 | 0.76 | 0.65 | 0.52 | 0.85 | 2.17 | 0.36 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Radetti, G.; Fanolla, A.; Lupi, F.; Sartorio, A.; Grugni, G. Accuracy of Different Indexes of Body Composition and Adiposity in Identifying Metabolic Syndrome in Adult Subjects with Prader-Willi Syndrome. J. Clin. Med. 2020, 9, 1646. https://doi.org/10.3390/jcm9061646
Radetti G, Fanolla A, Lupi F, Sartorio A, Grugni G. Accuracy of Different Indexes of Body Composition and Adiposity in Identifying Metabolic Syndrome in Adult Subjects with Prader-Willi Syndrome. Journal of Clinical Medicine. 2020; 9(6):1646. https://doi.org/10.3390/jcm9061646
Chicago/Turabian StyleRadetti, Giorgio, Antonio Fanolla, Fiorenzo Lupi, Alessandro Sartorio, and Graziano Grugni. 2020. "Accuracy of Different Indexes of Body Composition and Adiposity in Identifying Metabolic Syndrome in Adult Subjects with Prader-Willi Syndrome" Journal of Clinical Medicine 9, no. 6: 1646. https://doi.org/10.3390/jcm9061646
APA StyleRadetti, G., Fanolla, A., Lupi, F., Sartorio, A., & Grugni, G. (2020). Accuracy of Different Indexes of Body Composition and Adiposity in Identifying Metabolic Syndrome in Adult Subjects with Prader-Willi Syndrome. Journal of Clinical Medicine, 9(6), 1646. https://doi.org/10.3390/jcm9061646






