Factors Conditioning Sexual Behavior in Older Adults: A Systematic Review of Qualitative Studies
Abstract
:1. Introduction
2. Material and Methods
2.1. Protocol Review Design
2.2. Search Strategy
2.3. Study Selection
2.4. Data Extraction
2.5. Content Analysis
2.6. Assessment of Methodological Quality of Qualitative Studies
3. Results
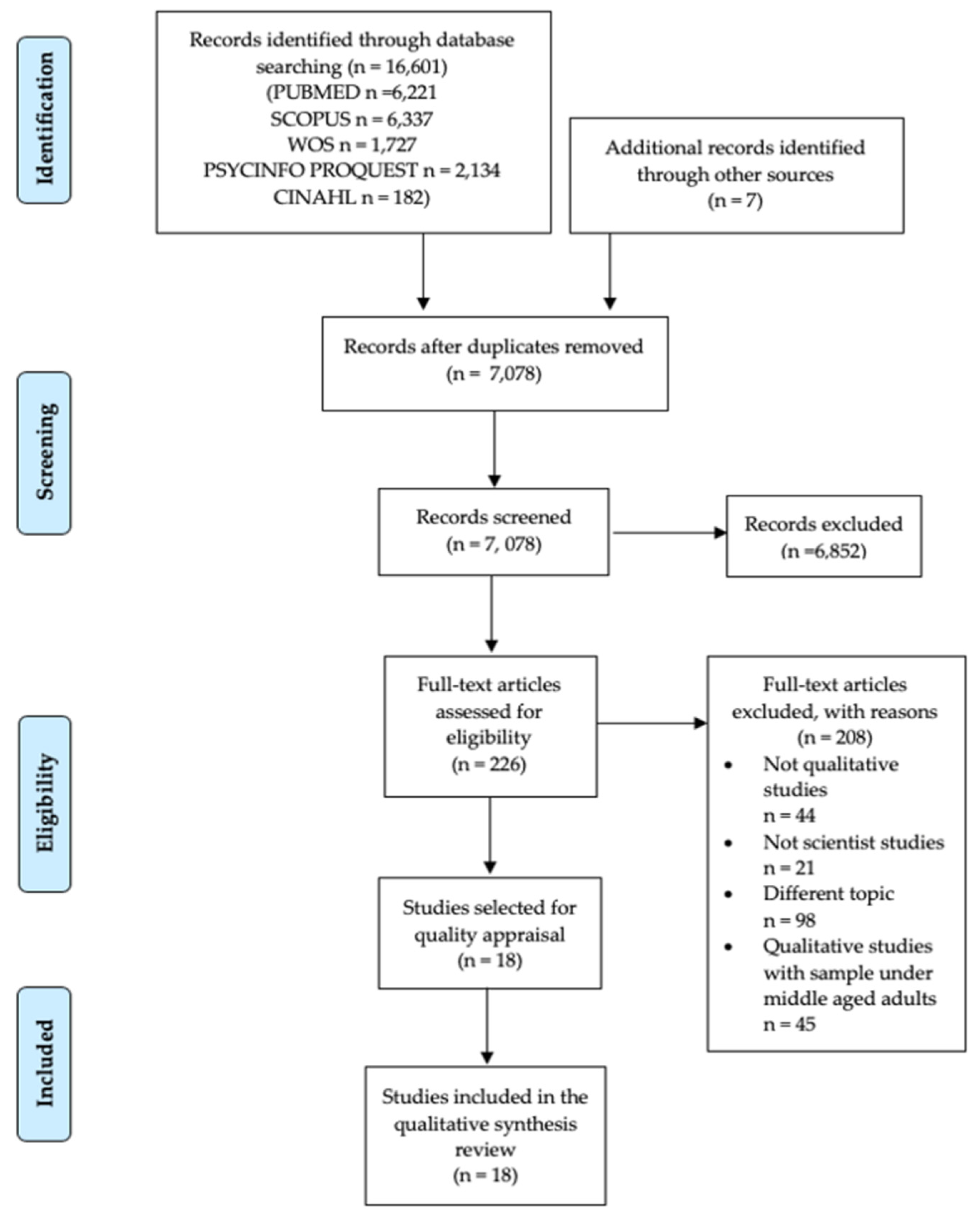
3.1. Selection Process
3.2. Characteristics of the Studies Included in the Qualitative Synthesis
3.3. Methodological Quality Assessment of Studies Included
3.4. Findings from Thematic Analysis
3.4.1. Is Sexuality Affected by Health and by Age?
3.4.2. Societal Influence and Stereotypes and the Sexuality of Older Adults
3.4.3. Factors Impacting Sexuality in the Elderly Associated with the Study
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Srithanaviboonchai, K.; Sitthi, W.; Musumari, P.M.; Tangmunkongvorakul, A.; Rerkasem, K.; Techasrivichien, T. Sexual Behavior and Attitudes Toward Sex of Older Adults Living with HIV. AIDS Behav. 2019, 24, 1825–1834. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Sexual Health, Human Rights and the Law; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Autenrieth, C.S.; Beck, E.J.; Stelzle, D.; Mallouris, C.; Mahy, M.; Ghys, P. Global and regional trends of people living with HIV aged 50 and over: Estimates and projections for 2000–2020. PLoS ONE 2018, 13, e0207005. [Google Scholar] [CrossRef]
- Srinivasan, S.; Glover, J.; Tampi, R.R.; Tampi, D.J.; Sewell, D.D. Sexuality and the Older Adult. Curr. Psychiatry Rep. 2019, 21, 97. [Google Scholar] [CrossRef]
- Allen, M.S.; Desille, A.E. Personality and sexuality in older adults. Psychol. Health 2017, 32, 843–859. [Google Scholar] [CrossRef]
- Chao, J.-K.; Lin, Y.-C.; Ma, M.-C.; Lai, C.-J.; Ku, Y.-C.; Kuo, W.-H.; Chao, I.-C. Relationship Among Sexual Desire, Sexual Satisfaction, and Quality of Life in Middle-Aged and Older Adults. J. Sex Marital Ther. 2011, 37, 386–403. [Google Scholar] [CrossRef]
- Træen, B.; Štulhofer, A.; Janssen, E.; Carvalheira, A.A.; Hald, G.M.; Lange, T.; Graham, C. Sexual Activity and Sexual Satisfaction Among Older Adults in Four European Countries. Arch. Sex. Behav. 2019, 48, 815–829. [Google Scholar] [CrossRef] [PubMed]
- Mernone, L.; Fiacco, S.; Ehlert, U. Psychobiological Factors of Sexual Functioning in Aging Women—Findings from the Women 40+ Healthy Aging Study. Front. Psychol. 2019, 10, 546. [Google Scholar] [CrossRef] [Green Version]
- Hartmann, U.; Philippsohn, S.; Heiser, K.; Rüffer-Hesse, C. Low sexual desire in midlife and older women: personality factors, psychosocial development, present sexuality. Menopause 2004, 11, 726–740. [Google Scholar] [CrossRef]
- Inelmen, E.M.; Sergi, G.; Girardi, A.; Coin, A.; Toffanello, E.D.; Cardin, F.; Manzato, E. The importance of sexual health in the elderly: breaking down barriers and taboos. Aging Clin. Exp. Res. 2012, 24, 31–34. [Google Scholar] [PubMed]
- DeLamater, J. Sexual expression in later life: A review and synthesis. J. Sex Res. 2012, 49, 125–141. [Google Scholar] [CrossRef]
- Træen, B.; Carvalheira, A.A.; Hald, G.M.; Lange, T.; Kvalem, I.L. Attitudes Towards Sexuality in Older Men and Women Across Europe: Similarities, Differences, and Associations with Their Sex Lives. Sex. Cult. 2019, 23, 1–25. [Google Scholar] [CrossRef]
- Kenny, R. A Review of the Literature on Sexual Development of Older Adults in Relation to the Asexual Stereotype of Older Adults. Can. J. Fam. Youth/ J. Can. Fam. Jeun. 2013, 5, 91–106. [Google Scholar] [CrossRef]
- Enzlin, P.; Mak, R.; Kittel, F.; Demyttenaere, K. Sexual functioning in a population-based study of men aged 40–69 years: The good news. Int. J. Impot. Res. 2004, 16, 512–520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ginsberg, T.B.; Pomerantz, S.C.; Kramer-Feeley, V. Sexuality in older adults: Behaviours and preferences. Age Ageing 2005, 34, 475–480. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morton, L. Sexuality in the Older Adult. Prim. Care 2017, 44, 429–438. [Google Scholar] [CrossRef]
- Asexuality Visibility and Education Network. The Asexual Visibility and Education Network. asexuality.org. Available online: https://www.asexuality.org/ (accessed on 3 May 2020).
- Ševčíková, A.; Sedláková, T. The Role of Sexual Activity from the Perspective of Older Adults: A Qualitative Study. Arch. Sex. Behav. 2020, 49, 969–981. [Google Scholar] [CrossRef] [PubMed]
- DeLamater, J.D.; Sill, M. Sexual desire in later life. J. Sex Res. 2005, 42, 138–149. [Google Scholar] [CrossRef] [PubMed]
- Rao, T.S.S.; Tandon, A.; Manohar, S.; Mathur, S. Clinical Practice Guidelines for management of sexual disorders in elderly. In Proceedings of the Indian Journal of Psychiatry; Medknow Publications: Mumbai, India, 2018; Volume 60, pp. S397–S409. [Google Scholar]
- Estill, A.; Mock, S.E.; Schryer, E.; Eibach, R.P. The Effects of Subjective Age and Aging Attitudes on Mid- to Late-Life Sexuality. J. Sex Res. 2018, 55, 146–151. [Google Scholar] [CrossRef]
- Ginsberg, T.B. Aging and sexuality. Med. Clin. North Am. 2006, 90, 1025–1036. [Google Scholar] [CrossRef]
- Træen, B.; Hald, G.M.; Graham, C.A.; Enzlin, P.; Janssen, E.; Kvalem, I.L.; Carvalheira, A.; Štulhofer, A. Sexuality in Older Adults (65+)—An Overview of the Literature, Part 1: Sexual Function and its Difficulties. Int. J. Sex. Heal. 2017, 29, 1–10. [Google Scholar] [CrossRef]
- Træen, B.; Carvalheira, A.; Kvalem, I.L.; Štulhofer, A.; Janssen, E.; Graham, C.A.; Hald, G.M.; Enzlin, P. Sexuality in Older Adults (65+)—An Overview of The Recent Literature, Part 2: Body Image and Sexual Satisfaction. Int. J. Sex. Heal. 2017, 29, 11–21. [Google Scholar] [CrossRef] [Green Version]
- Milaszewski, D.; Greto, E.; Klochkov, T.; Fuller-Thomson, E. A Systematic Review of Education for the Prevention of HIV/AIDS among Older Adults. J. Evid. Based. Soc. Work 2012, 9, 213–230. [Google Scholar] [CrossRef] [PubMed]
- Mahieu, L.; Gastmans, C. Older residents’ perspectives on aged sexuality in institutionalized elderly care: A systematic literature review. Int. J. Nurs. Stud. 2014, 52, 1891–1905. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Foley, S. Older Adults and Sexual Health: A Review of Current Literature. Curr. Sex. Heal. Rep. 2015, 7, 70–79. [Google Scholar] [CrossRef]
- Sinkovic, M.; Towler, L. Sexual Aging: A Systematic Review of Qualitative Research on the Sexuality and Sexual Health of Older Adults. Qual. Health Res. 2019, 29, 1239–1254. [Google Scholar] [CrossRef]
- Ambrosini, D.L.; Chackery, R.; Hategan, A. Sexuality and Sexual Dysfunction in Later Life. In Geriatric Psychiatry; Springer International Publishing: Berlin, Germany, 2018; pp. 645–658. [Google Scholar]
- Stanworth, R.D.; Jones, T.H. Testosterone for the aging male; Current evidence and recommended practice. Clin. Interv. Aging 2008, 3, 25–44. [Google Scholar]
- Baspure, P. Sexual Health in the Aging Couple. In Sexual Medicine; Springer: Singapore, Singapore, 2019; pp. 131–137. [Google Scholar]
- Christensen, B.S.; Grønbæk, M.; Pedersen, B.V.; Graugaard, C.; Frisch, M. Associations of unhealthy lifestyle factors with sexual inactivity and sexual dysfunctions in Denmark. J. Sex. Med. 2011, 8, 1903–1916. [Google Scholar] [CrossRef]
- Christensen, B.S.; Grønbæk, M.; Osler, M.; Pedersen, B.V.; Graugaard, C.; Frisch, M. Associations between physical and mental health problems and sexual dysfunctions in sexually active danes. J. Sex. Med. 2011, 8, 1890–1902. [Google Scholar] [CrossRef]
- Iveniuk, J.; Waite, L.J. The psychosocial sources of sexual interest in older couples. J. Soc. Pers. Relat. 2018, 35, 615–631. [Google Scholar] [CrossRef]
- Waite, L.J.; Iveniuk, J.; Laumann, E.O.; McClintock, M.K. Sexuality in Older Couples: Individual and Dyadic Characteristics. Arch. Sex. Behav. 2017, 46, 605–618. [Google Scholar] [CrossRef]
- Macdowall, W.; Jones, K.G.; Tanton, C.; Clifton, S.; Copas, A.J.; Mercer, C.H.; Palmer, M.J.; Lewis, R.; Datta, J.; Mitchell, K.R.; et al. Associations between source of information about sex and sexual health outcomes in Britain: Findings from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3). BMJ Open 2015, 5, e007837. [Google Scholar] [CrossRef]
- Nazarpour, S.; Simbar, M.; Tehrani, F.R. Factors affecting sexual function in menopause: A review article. Taiwan. J. Obstet. Gynecol. 2016, 55, 480–487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karraker, A.; Delamater, J.; Schwartz, C.R. Sexual frequency decline from midlife to later life. J. Gerontol. B. Psychol. Sci. Soc. Sci. 2011, 66, 502–512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Minichiello, V.; Rahman, S.; Hawkes, G.; Pitts, M. STI epidemiology in the global older population: Emerging challenges. Perspect. Public Health 2012, 132, 178–181. [Google Scholar] [CrossRef] [PubMed]
- Iveniuk, J.; Waite, L.J.; McClintock, M.K.; Teidt, A.D. Marital Conflict in Older Couples: Positivity, Personality, and Health. J. Marriage Fam. 2014, 76, 130–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McFarland, M.J.; Uecker, J.E.; Regnerus, M.D. The role of religion in shaping sexual frequency and satisfaction: evidence from married and unmarried older adults. J. Sex Res. 2011, 48, 297–308. [Google Scholar] [CrossRef]
- Cybulski, M.; Cybulski, L.; Krajewska-Kulak, E.; Orzechowska, M.; Cwalina, U.; Jasinski, M. Sexual Quality of Life, Sexual Knowledge, and Attitudes of Older Adults on the Example of Inhabitants Over 60s of Bialystok, Poland. Front. Psychol. 2018, 9, 483. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thames, A.D.; Hammond, A.; Nunez, R.A.; Mahmood, Z.; Jones, F.; Carter, S.L.; Bilder, R.M.; Fisher, S.; Bivens-Davis, T.; Jones, L. Sexual Health Behavior and Mental Health Among Older African American Women: The Sistahs, Sexuality, and Mental Health Well-Being Project. J. Womens. Health (Larchmt). 2018, 27, 1177–1185. [Google Scholar] [CrossRef]
- Mahieu, L.; de Casterle, B.D.; Acke, J.; Vandermarliere, H.; Van Elssen, K.; Fieuws, S.; Gastmans, C. Nurses’ knowledge and attitudes toward aged sexuality in Flemish nursing homes. Nurs. Ethics 2016, 23, 605–623. [Google Scholar] [CrossRef]
- Thys, K.; Mahieu, L.; Cavolo, A.; Hensen, C.; Dierckx de Casterle, B.; Gastmans, C. Nurses’ experiences and reactions towards intimacy and sexuality expressions by nursing home residents: A qualitative study. J. Clin. Nurs. 2019, 28, 836–849. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Deeks, J.J. Chapter 7: Selecting studies and collecting data. In Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons, Ltd: Chichester, UK, 2011. [Google Scholar]
- Lockwood, C.; Porrit, K.; Munn, Z.; Rittenmeyer, L.; Salmond, S.; Bjerrum, M.; Loveday, H.; Carrier, J.; Stannard, D. Chapter 2: Systematic reviews of qualitative evidence. In Joanna Briggs Institute Reviewer’s Manual; Aromataris, E., Munn, Z., Eds.; The Johanna Briggs Institute: Adelaide, SA, Australia, 2017. [Google Scholar]
- Riesenberg, L.A.; Justice, E.M. Conducting a successful systematic review of the literature, part 1. Nursing (London) 2014, 44, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Riesenberg, L.A.; Justice, E.M. Conducting a successful systematic review of the literature, part 2. Nursing (London) 2014, 44, 23–26. [Google Scholar] [CrossRef] [PubMed]
- Stern, C.; Jordan, Z.; McArthur, A. Developing the review question and inclusion criteria. Am. J. Nurs. 2014, 114, 53–56. [Google Scholar] [CrossRef]
- Butler, A.; Hall, H.; Copnell, B. A Guide to Writing a Qualitative Systematic Review Protocol to Enhance Evidence-Based Practice in Nursing and Health Care. Worldviews Evid. Based Nurs. 2016, 13, 241–249. [Google Scholar] [CrossRef]
- Thomas, J.; Harden, A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med. Res. Methodol. 2008, 8, 45. [Google Scholar] [CrossRef] [Green Version]
- Thomas, J.; Brunton, J.; Graziosi, S. EPPI-Reviewer 4.0: Software for Research Synthesis; EPPI-Centre Software; Social Science Research Unit, Institute of Education, University of London: London, UK, 2010. [Google Scholar]
- Noyes, J.; Booth, A.; Flemming, K.; Garside, R.; Harden, A.; Lewin, S.; Pantoja, T.; Hannes, K.; Cargo, M.; Thomas, J. Cochrane Qualitative and Implementation Methods Group guidance series-paper 3: Methods for assessing methodological limitations, data extraction and synthesis, and confidence in synthesized qualitative findings. J. Clin. Epidemiol. 2018, 97, 49–58. [Google Scholar] [CrossRef] [Green Version]
- Healthcare BV Critical Appraisal Skills Programme (CASP). Available online: https://casp-uk.net/casp-tools-checklists/ (accessed on 3 May 2020).
- Fullen, B.M.; Baxter, G.D.; O’Donovan, B.G.G.; Doody, C.; Daly, L.; Hurley, D.A. Doctors’ attitudes and beliefs regarding acute low back pain management: A systematic review. Pain 2008, 136, 388–396. [Google Scholar] [CrossRef]
- Ayalon, L.; Gewirtz-Meydan, A.; Levkovich, I. Older Adults’ Coping Strategies with Changes in Sexual Functioning: Results From Qualitative Research. J. Sex. Med. 2019, 16, 52–60. [Google Scholar] [CrossRef]
- Dickson, F.C.; Hughes, P.C.; Walker, K.L. An exploratory investigation into dating among later-life women. West. J. Commun. 2005, 69, 67–82. [Google Scholar] [CrossRef]
- Hinchliff, S.; Tetley, J.; Lee, D.; Nazroo, J. Older Adults’ Experiences of Sexual Difficulties: Qualitative Findings from the English Longitudinal Study on Ageing (ELSA). J. Sex Res. 2018, 55, 152–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jen, S. Older women and sexuality: Narratives of gender, age, and living environment. J. Women Aging 2017, 29, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Kasif, T.; Band-Winterstein, T. Older widows’ perspectives on sexuality: A life course perspective. J. Aging Stud. 2017, 41, 1–9. [Google Scholar] [CrossRef]
- Ravanipour, M.; Gharibi, T.; Gharibi, T. Elderly women’s views about sexual desire during old age: A qualitative study. Sex. Disabil. 2013, 31, 179–188. [Google Scholar] [CrossRef]
- Syme, M.L.; Cohn, T.J.; Stoffregen, S.; Kaempfe, H.; Schippers, D. “At My Age … ”: Defining Sexual Wellness in Mid- and Later Life. J. Sex Res. 2019, 56, 832–842. [Google Scholar] [CrossRef] [PubMed]
- Thorpe, R.; Fileborn, B.; Hawkes, G.; Pitts, M.; Minichiello, V. Old and desirable: Older women’s accounts of ageing bodies in intimate relationships. Sex. Relatsh. Ther. 2015, 30, 156–166. [Google Scholar] [CrossRef]
- Watson, W.K.; Stelle, C.; Bell, N. Older Women in New Romantic Relationships. Int. J. Aging Hum. Dev. 2017, 85, 33–43. [Google Scholar] [CrossRef] [PubMed]
- Yıldırım Varışoğlu, Y.; Yeşiltepe Oskay, Ü. The Meaning of Sexuality in Advanced Age: A Qualitative Study in Turkey. Sex. Cult. 2018, 22, 1507–1515. [Google Scholar] [CrossRef]
- Fileborn, B.; Thorpe, R.; Hawkes, G.; Minichiello, V.; Pitts, M.; Dune, T. Sex, desire and pleasure: Considering the experiences of older Australian women. Sex. Relatsh. Ther. 2015, 30, 117–130. [Google Scholar] [CrossRef] [Green Version]
- Fileborn, B.; Thorpe, R.; Hawkes, G.; Minichiello, V.; Pitts, M. Sex and the (older) single girl: Experiences of sex and dating in later life. J. Aging Stud. 2015, 33, 67–75. [Google Scholar] [CrossRef]
- Fileborn, B.; Hinchliff, S.; Lyons, A.; Heywood, W.; Minichiello, V.; Brown, G.; Malta, S.; Barrett, C.; Crameri, P. The Importance of Sex and the Meaning of Sex and Sexual Pleasure for Men Aged 60 and Older Who Engage in Heterosexual Relationships: Findings from a Qualitative Interview Study. Arch. Sex. Behav. 2017, 46, 2097–2110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fileborn, B.; Lyons, A.; Hinchliff, S.; Brown, G.; Heywood, W.; Dow, B.; Malta, S.; Minichiello, V. Improving the sexual lives of older Australians: Perspectives from a qualitative study. Australas. J. Ageing 2017, 36, E36–E42. [Google Scholar] [CrossRef] [PubMed]
- Fileborn, B.; Brown, G.; Lyons, A.; Hinchliff, S.; Heywood, W.; Minichiello, V.; Malta, S.; Barrett, C.; Crameri, P. Safer Sex in Later Life: Qualitative Interviews With Older Australians on Their Understandings and Practices of Safer Sex. J. Sex Res. 2018, 55, 164–177. [Google Scholar] [CrossRef] [PubMed]
- Freixas, A.; Luque, B.; Reina, A. Sexuality in older Spanish women: Voices and reflections. J. Women Aging 2015, 27, 35–58. [Google Scholar] [CrossRef] [PubMed]
- Gledhill, S.; Schweitzer, R.D. Sexual desire, erectile dysfunction and the biomedicalization of sex in older heterosexual men. J. Adv. Nurs. 2014, 70, 894–903. [Google Scholar] [CrossRef] [PubMed]
- Hinchliff, S.; Gott, M. Challenging social myths and stereotypes of women and aging: Heterosexual women talk about sex. J. Women Aging 2008, 20, 65–81. [Google Scholar] [CrossRef]
- Taylor, A.; Gosney, M.A. Sexuality in older age: Essential considerations for healthcare professionals. Age Ageing 2011, 40, 538–543. [Google Scholar] [CrossRef] [Green Version]
- Lindau, S.T.; Schumm, L.P.; Laumann, E.O.; Levinson, W.; O’Muircheartaigh, C.A.; Waite, L.J. A study of sexuality and health among older adults in the United States. N. Engl. J. Med. 2007, 357, 762–774. [Google Scholar] [CrossRef] [Green Version]
- Morley, J.E.; Tariq, S.H. Sexuality and disease. Clin. Geriatr. Med. 2003, 19, 563–573. [Google Scholar] [CrossRef]
- Bortz, W.M., II. A conceptual framework of frailty: A review. J. Gerontol. A. Biol. Sci. Med. Sci. 2002, 57, M283–M288. [Google Scholar] [CrossRef] [Green Version]
- Avis, N.E.; Brockwell, S.; Randolph, J.F.J.; Shen, S.; Cain, V.S.; Ory, M.; Greendale, G.A. Longitudinal changes in sexual functioning as women transition through menopause: Results from the Study of Women’s Health Across the Nation. Menopause 2009, 16, 442–452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hinchliff, S.; Gott, M.; Ingleton, C. Sex, menopause and social context: a qualitative study with heterosexual women. J. Health Psychol. 2010, 15, 724–733. [Google Scholar] [CrossRef] [PubMed]
- Bortz, W.M., II; Wallace, D.H. Physical fitness, aging, and sexuality. West. J. Med. 1999, 170, 167–169. [Google Scholar] [PubMed]
- Albaugh, J.A. Addressing and managing erectile dysfunction after prostatectomy for prostate cancer. Urol. Nurs. 2010, 30, 167–177. [Google Scholar] [CrossRef]
- Donnelly, D.W.; Kearney, T.; McCaughan, E.; Downing, A.; Weller, D.; Glaser, A.W.; Gavin, A. Treatment for erectile dysfunction among older men in Northern Ireland. Int. J. Clin. Pract. 2019, 73, e13259. [Google Scholar] [CrossRef] [Green Version]
- Fernández-Sola, C.; Martínez-Bordajandi, Á.; Puga-Mendoza, A.P.; Hernández-Padilla, J.M.; Jobim-Fischer, V.; López-Rodríguez, M.D.M.; Granero-Molina, J. Social Support in Patients With Sexual Dysfunction After Non-Nerve-Sparing Radical Prostatectomy: A Qualitative Study. Am. J. Mens. Health 2020, 14, 1557988320906977. [Google Scholar] [CrossRef] [Green Version]
- Nicolosi, A.; Laumann, E.O.; Glasser, D.B.; Moreira, E.D.J.; Paik, A.; Gingell, C. Sexual behavior and sexual dysfunctions after age 40: the global study of sexual attitudes and behaviors. Urology 2004, 64, 991–997. [Google Scholar] [CrossRef]
- Granville, L.; Pregler, J. Women’s Sexual Health and Aging. J. Am. Geriatr. Soc. 2018, 66, 595–601. [Google Scholar] [CrossRef] [Green Version]
- Hodson, D.S.; Skeen, P. Sexuality and Aging: The Hammerlock of Myths. J. Appl. Gerontol. 1994, 13, 219–235. [Google Scholar] [CrossRef]
- Kennedy, G.J.; Haque, M.; Zarankow, B. Human Sexuality in Late Life. Int. J. Ment. Health 1997, 26, 35–46. [Google Scholar] [CrossRef]
- Willert, A.; Semans, M. Knowledge and attitudes about later life sexuality: What clinicians need to know about helping the elderly. Contemp. Fam. Ther. 2000, 22, 415–435. [Google Scholar] [CrossRef]
- Hurd Clarke, L. Older women and sexuality: Experiences in marital relationships across the life course. Can. J. Aging 2006, 25, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Sandberg, L. Just feeling a naked body close to you: Men, sexuality and intimacy in later life. Sexualities 2013, 16, 261–282. [Google Scholar] [CrossRef]
- Valadares, A.L.R.; Machado, V.D.S.S.; Costa-Paiva, L.; Osis, M.J.; Sousa, M.H.D.; de Pinto-Neto, A.M. Self-perception of sexual life and associated factors: A population study conducted in women aged 50 or more years. Rev. Bras. Ginecol. Obstet. 2013, 35, 295–300. [Google Scholar] [CrossRef] [Green Version]
- de Alencar, D.L.; de Oliveira Marques, A.P.; Leal, M.C.C.; de Cássia Miguel Vieira, J. [Factors that influence the sexuality of the elderly: An integrative review]. Cien. Saude Colet. 2014, 19, 3533–3542. [Google Scholar]
- Czajkowska, K.B.; Lew-Starowicz, Z.; Szymańska, M. The prevalence of sexual activity, and sexual dysfunction and behaviours in postmenopausal woman in Poland. Prz. Menopauzalny Menopause Rev. 2016, 15, 156–164. [Google Scholar] [CrossRef] [Green Version]
- Higgins, A.B.; Follette, V.M. Frequency and Impact of Interpersonal Trauma in Older Women. J. Clin. Geropsychology 2002, 8, 215–226. [Google Scholar] [CrossRef]
- Gibson, C.J.; Lisha, N.E.; Walter, L.C.; Huang, A.J. Interpersonal trauma and aging-related genitourinary dysfunction in a national sample of older women. Am. J. Obstet. Gynecol. 2019, 220, 94.e1–94.e7. [Google Scholar] [CrossRef] [Green Version]
- Gray, P.B.; Garcia, J.R. Aging and human sexual behavior: Biocultural perspectives—A mini-review. Gerontology 2012, 58, 446–452. [Google Scholar] [CrossRef]
- Winn, R.L.; Newton, N. Sexuality in aging: A study of 106 cultures. Arch. Sex. Behav. 1982, 11, 283–298. [Google Scholar] [CrossRef]
- Laumann, E.O.; Paik, A.; Glasser, D.B.; Kang, J.-H.; Wang, T.; Levinson, B.; Moreira, E.D.J.; Nicolosi, A.; Gingell, C. A cross-national study of subjective sexual well-being among older women and men: Findings from the Global Study of Sexual Attitudes and Behaviors. Arch. Sex. Behav. 2006, 35, 145–161. [Google Scholar] [CrossRef] [PubMed]
| Database | Search Strategy |
|---|---|
| Medline | (older adult* [tiab] OR middle aged [mh] OR middle aged [tiab] OR aged [mh] OR aged [tiab] OR aged, 80 and over [mh] OR aged, 80 and over [tiab] OR elderly [tiab]) AND (sexual behavior [mh] OR sexual behavior [tiab] OR sexual behavior [tiab] OR sex behavior [tiab] OR sexuality [tiab] OR sexual activity [tiab]) AND (sexual dysfunction, physiological [mh] OR sexual dysfunction, physiological [tiab] OR physiological sexual dysfunctions [tiab] OR physiological sexual conditioning factors [tiab] OR psychosocial sexual conditioning factors [tiab] OR psychological sexual dysfunction [tiab] OR psychological sexual risk factor* [tiab] or physiological [tiab] or psychological [tiab] or psychosocial [tiab]) |
| Scopus | [TITLE-ABS-KEY (“older adults” OR “middle aged” OR “aged” OR “elderly” ) AND TITLE-ABS-KEY (“sexual behavior” OR “sexual behaviour” OR “sex behavior” OR “sexual activity” ) AND TITLE-ABS-KEY (“physiological sexual dysfunction” OR “physiological sexual conditioning factors” OR “psychological sexual conditioning factors” OR “psychological sexual risk factors” OR “physiological” OR “psychological” )] |
| Web of Science | TOPIC: [(*older adults* OR *elderly* OR * middle aged* OR * aged* OR *aged, 80 and over* OR *elderly*) AND (*sexual behavior* OR *sexual behaviour* OR *sex behavior* OR *sexual activity*) AND (*physiological sexual dysfunctions* OR * physiological sexual conditioning factors* OR *psychosocial sexual conditioning factors* OR *psychological sexual risk factors* OR *psychological sex factors* OR *physiological* OR *psychological* OR *psychosocial*)] |
| PsycINFO ProQuest | [AB(older adults) OR SU(middle aged) OR AB(middle aged) OR SU(aged) OR AB(aged) OR SU(aged, 80 and over) OR AB(aged, 80 and over) OR AB (elderly)) AND (SU(sexual behavior) OR AB(sexual behavior) OR AB(sex behavior)) AND (SU(sexual dysfunction, physiological) OR AB(sexual dysfunction, physiological) OR AB(physiological sexual dysfunctions) OR AB(physiological sexual conditioning factors) OR AB(psychological sexual dysfunctions) OR AB(psychological sexual risk factors)] |
| CINAHL | (AB older adults OR AB middle aged OR AB aged OR AB elderly) AND (AB sexual behavior OR AB sexual behaviour OR MH sexuality OR AB sexuality) AND (MH sexual dysfunctions OR AB physiological OR AB psychological) |
| Population | Older Adults |
|---|---|
| Context | Physiological and psychosocial sexual conditioning factors |
| Outcome | Sexual behavior |
| Author and Year | Place | Target Population | Data Collection Design/Method | Sample Ages | Size and Gender |
|---|---|---|---|---|---|
| Ayalon et al. 2019 | Israel | Older men and women | In-depth interviews | 60 and over | Total = 47 |
| 23–F | |||||
| 24–M | |||||
| Dickson et al. 2005 | United States | Older adults and married women | Depth interviews | 62–79 | 15–F |
| Fileborn et al. 2015 | Australia | Australian women married/with partner | Qualified semi-structured interviews | 55–81 | 43–F |
| Fileborn et al. 2015 | Australia | Older women single at the time of the interview | Qualified semi-structured interviews | 55–81 | 58–F |
| Fileborn et al. 2017 | Australia | Older men | Qualified semi-structured interviews | 60 and over | 27–M |
| Conducted by: Phone, Skype and Face to Face | |||||
| Fileborn et al. 2017 | Australia | Older men and women | Qualified semi-structured interviews | 60 and over | Total = 53 |
| 23–F | |||||
| 30–M | |||||
| Fileborn et al. 2018 | Australia | Older men and women | Qualified semi-structured interviews. | 60 and over | Total = 53 |
| Conducted by: Phone (n = 41), Skype (n = 10) and Face to face (n = 2) | 23–F | ||||
| 30–M | |||||
| Freixas et al. 2015 | Spain | Older married women | Discussion groups | 50–80 | 729–F |
| Open-closed semi-structured interviews | |||||
| Gledhill et al. 2014 | Australia | Older men and women | In-depth interviews | 65–84 | Total = 8 |
| Interviews recorded in audio | 2–F | ||||
| 6–M | |||||
| Hinchliff et al. 2008 | United Kingdom | Older married women | In depth interviews | 50 and over | 19–F |
| Hinchliff et al. 2018 | United Kingdom | Older men and women | Extraction of qualitative and qualitative data by application of SRA-Q | 50–90 | Total = 1084 |
| 680–F | |||||
| 404–M | |||||
| Jen. 2017 | United States | Older married women | Semi-structured interviews | 57–93 | 13–F |
| Kasif et al. 2017 | Israel | Widows (women) | Semi-structured interviews | 62–91 | 17–F |
| In-depth interviews | |||||
| Face to face interviews | |||||
| Ravanipour et al. 2013 | Iran | Older married women | Individual interviews | 60 and over | 15–F |
| Syme et al. 2019 | United States | Older men and women | Semi-structured interviews | 50 and over | 373–F |
| Thorpe et al. 2015 | Australia | Older married women | Semi-structured interviews | 55–72 | 20–F |
| Face to face interviews | |||||
| Watson et al. 2017 | United States | Older married women | In-depth interviews | 64–77 | 14–F |
| Face to face interviews | |||||
| Yıldırım et al. 2018 | Turkey | Older married women | Qualitative semi-structured interviews | 60 and over | 15–F |
| Face to face interviews |
| Study | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 | Score | Classification of Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ayalon et al. 2019 | Y | Y | N | Y | Y | N | Y | Y | Y | Y | 8 | High |
| Dickson et al. 2005 | Y | Y | N | Y | Y | N | N | N | N | N | 4 | Moderate |
| Fileborn et al. 2015 | Y | Y | N | Y | Y | N | N | Y | Y | Y | 7 | High |
| Fileborn et al. 2015 | Y | Y | Y | Y | Y | N | N | Y | Y | N | 7 | High |
| Fileborn et al. 2017 | Y | Y | N | N | Y | N | Y | Y | N | Y | 6 | Moderate |
| Fileborn et al. 2017 | Y | Y | N | Y | Y | N | Y | Y | Y | Y | 8 | High |
| Fileborn et al. 2018 | Y | Y | N | Y | N | N | N | Y | Y | Y | 6 | Moderate |
| Freixas et al. 2015 | Y | N | N | Y | N | N | N | N | N | N | 2 | Low |
| Gledhill et al. 2014 | Y | N | N | Y | Y | N | Y | Y | Y | Y | 7 | High |
| Hinchliff et al 2008 | Y | Y | N | N | Y | N | Y | N | Y | Y | 6 | Moderate |
| Hinchliff et al. 2018 | Y | N | Y | Y | N | N | Y | Y | Y | N | 6 | Moderate |
| Jen. 2017 | Y | Y | N | Y | Y | N | Y | N | Y | Y | 7 | High |
| Kasif et al. 2017 | Y | Y | N | N | N | N | Y | Y | Y | N | 5 | Moderate |
| Ravanipour et al. 2013 | Y | Y | Y | N | N | N | Y | N | N | N | 4 | Moderate |
| Syme et al. 2019 | Y | Y | N | Y | N | Y | Y | Y | Y | Y | 8 | High |
| Thorpe et al. 2015 | Y | Y | N | Y | N | N | Y | Y | Y | N | 6 | Moderate |
| Watson et al. 2017 | N | Y | N | N | N | N | Y | N | Y | N | 3 | Low |
| Yıldırm et al. 2018 | Y | N | N | N | N | N | Y | N | N | N | 2 | Low |
| Descriptive Themes | Analytical Focus |
|---|---|
| (A) Physiological factors affecting sexuality | Theme 1. Is sexuality affected by health and age? |
| Stage in life | |
| Influence of menopause | |
| Erectile dysfunction | |
| Old age, body image and well-being | |
| (B) Psychosocial factors affecting sexuality | Theme 2. Societal influence and stereotypes of the sexuality of older adults |
| Sociocultural influences | |
| Beliefs about asexuality among older adults | |
| Stereotypes of sexuality during old age | |
| Professional guidance | |
| Singleness and sexuality in old age | |
| Religion and sexuality | |
| (C) Sub-themes that were studied | Theme 3. Factors impacting sexuality among older adults associated with the research |
| Sexual satisfaction | |
| Sexual pleasure | |
| Sexual desire | |
| Autoerotism | |
| Older people talk about sexuality |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ricoy-Cano, A.J.; Obrero-Gaitán, E.; Caravaca-Sánchez, F.; Fuente-Robles, Y.M.D.L. Factors Conditioning Sexual Behavior in Older Adults: A Systematic Review of Qualitative Studies. J. Clin. Med. 2020, 9, 1716. https://doi.org/10.3390/jcm9061716
Ricoy-Cano AJ, Obrero-Gaitán E, Caravaca-Sánchez F, Fuente-Robles YMDL. Factors Conditioning Sexual Behavior in Older Adults: A Systematic Review of Qualitative Studies. Journal of Clinical Medicine. 2020; 9(6):1716. https://doi.org/10.3390/jcm9061716
Chicago/Turabian StyleRicoy-Cano, Adrián Jesús, Esteban Obrero-Gaitán, Francisco Caravaca-Sánchez, and Yolanda María De La Fuente-Robles. 2020. "Factors Conditioning Sexual Behavior in Older Adults: A Systematic Review of Qualitative Studies" Journal of Clinical Medicine 9, no. 6: 1716. https://doi.org/10.3390/jcm9061716
APA StyleRicoy-Cano, A. J., Obrero-Gaitán, E., Caravaca-Sánchez, F., & Fuente-Robles, Y. M. D. L. (2020). Factors Conditioning Sexual Behavior in Older Adults: A Systematic Review of Qualitative Studies. Journal of Clinical Medicine, 9(6), 1716. https://doi.org/10.3390/jcm9061716








