Insomnia as a Symptom of Rapid Eye Movement-Related Obstructive Sleep Apnea
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Approval
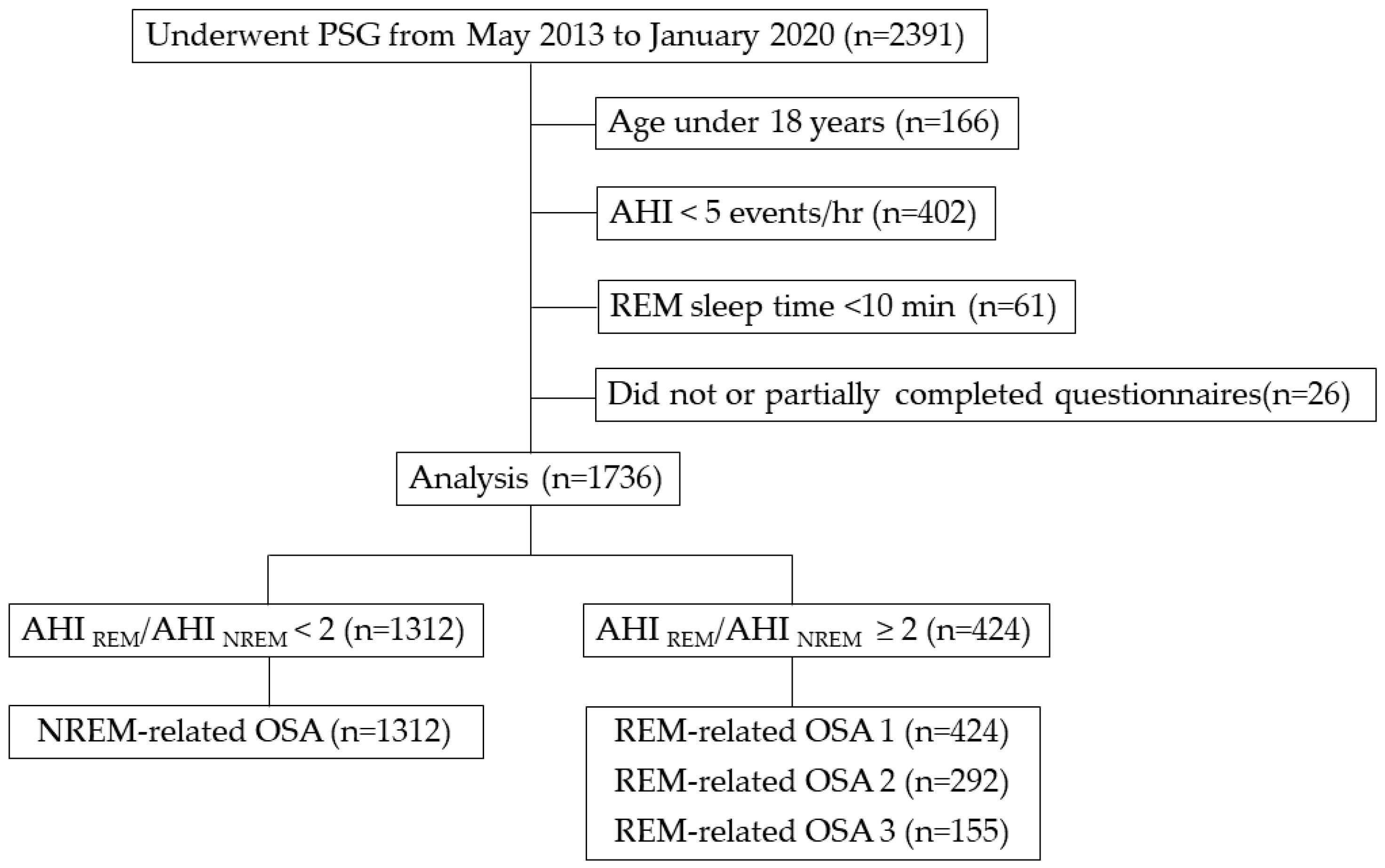
2.2. Study Population
2.3. Data Collection
- REM-related OSA 1: overall AHI ≥ 5 and AHI during REM (AHIREM)/AHI during NREM (AHINREM) ≥ 2;
- REM-related OSA 2: overall AHI ≥ 5, AHIREM/AHINREM ≥ 2, and AHINREM < 15;
2.4. Questionnaires
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Nieto, F.J.; Young, T.; Lind, B.K.; Shahar, E.; Samet, J.M.; Redline, S.; D’Agostino, R.B.; Newman, A.B.; Lebowitz, M.D.; Pickering, T.G.; et al. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. JAMA 2000, 283, 1829–1836. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mano, M.; Hoshino, T.; Sasanabe, R.; Murotani, K.; Nomura, A.; Hori, R.; Konishi, N.; Baku, M.; Shiomi, T. Impact of gender and age on rapid eye movement-related obstructive sleep apnea: A clinical study of 3234 Japanese OSA patients. Int. J. Environ. Res. Public Heal. 2019, 16, 1068. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Conwell, W.; Patel, B.; Doeing, D.; Pamidi, S.; Knutson, K.L.; Ghods, F.; Mokhlesi, B. Prevalence, clinical features, and CPAP adherence in REM-related sleep-disordered breathing: A cross-sectional analysis of a large clinical population. Sleep Breath. 2011, 16, 519–526. [Google Scholar] [CrossRef]
- Mokhlesi, B.; Hagen, E.W.; Finn, L.A.; Hla, K.M.; Carter, J.R.; Peppard, P.E. Obstructive sleep apnoea during REM sleep and incident non-dipping of nocturnal blood pressure: A longitudinal analysis of the Wisconsin Sleep Cohort. Thorax 2015, 70, 1062–1069. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Acosta-Castro, P.; Hirotsu, C.; Marti-Soler, H.; Marques-Vidal, P.; Tobback, N.; Andries, D.; Waeber, G.; Preisig, M.; Vollenweider, P.; Haba-Rubio, J.; et al. REM-associated sleep apnoea: Prevalence and clinical significance in the HypnoLaus cohort. Eur. Respir. J. 2018, 52, 1702484. [Google Scholar] [CrossRef]
- Geckil, A.A.; Ermis, H. The relationship between anxiety, depression, daytime sleepiness in the REM-related mild OSAS and the NREM-related mild OSAS. Sleep Breath. 2019, 24, 1–5. [Google Scholar] [CrossRef]
- Koo, B.B.; Dostal, J.; Ioachimescu, O.C.; Budur, K. The effects of gender and age on REM-related sleep-disordered breathing. Sleep Breath. 2007, 12, 259–264. [Google Scholar] [CrossRef]
- Guilleminault, C.; Eldridge, F.L.; Dement, W.C. Insomnia with Sleep Apnea: A New Syndrome. Science 1973, 181, 856–858. [Google Scholar] [CrossRef]
- Luyster, F.S.; Buysse, D.J.; Strollo, P.J. Comorbid insomnia and obstructive sleep apnea: Challenges for clinical practice and research. J. Clin. Sleep Med. 2010, 6, 196–204. [Google Scholar] [CrossRef] [Green Version]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. Neuroimaging 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Fichtenberg, N.L.; Zafonte, R.D.; Putnam, S.; Mann, N.R.; Millard, A.E. Insomnia in a post-acute brain injury sample. Brain Inj. 2002, 16, 197–206. [Google Scholar] [CrossRef]
- Aloba, O.O.; Adewuya, A.O.; Ola, B.; Mapayi, B. Validity of the Pittsburgh Sleep Quality Index (PSQI) among Nigerian university students. Sleep Med. 2007, 8, 266–270. [Google Scholar] [CrossRef] [PubMed]
- Berry, R.B.; Brooks, R.; Gamaldo, C.E.; Harding, S.M.; Marcus, C.L.; Vaughn, B.V.; Tangredi, M.M. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications; Version 2.0; American Academy of Sleep Medicine: Darien, IL, USA, 2012. [Google Scholar]
- American Academy of Sleep Medicine. International Classification of Sleep Disorders. Diagnostic and Coding Manual (ICSD-2), 2nd ed.; American Academy of Sleep Medicine: Westchester, IL, USA, 2005. [Google Scholar]
- Haba-Rubio, J.; Janssens, J.P.; Rochat, T.; Sforza, E.; Haba-Rubio, J. Rapid eye movement-related disordered breathing. Chest 2005, 128, 3350–3357. [Google Scholar] [CrossRef] [Green Version]
- Hoshino, T.; Sasanabe, R.; Tanigawa, T.; Murotani, K.; Arimoto, M.; Ueda, H.; Shiomi, T. Effect of rapid eye movement-related obstructive sleep apnea on adherence to continuous positive airway pressure. J. Int. Med. Res. 2018, 46, 2238–2248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Su, C.-S.; Liu, K.-T.; Panjapornpon, K.; Andrews, N.; Foldvary-Schaefer, N. Functional outcomes in patients with REM-Related obstructive sleep apnea treated with positive airway pressure therapy. J. Clin. Sleep Med. 2012, 8, 243–247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johns, M.W. Reliability and factor analysis of the epworth sleepiness scale. Sleep 1992, 15, 376–381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Montgomery, D.C.; Peck, E.A.; Vining, G.G. Introduction to Linear Regression Analysis; John Wiley & Sons: Hoboken, NJ, USA, 2012. [Google Scholar]
- Sakao, S.; Sakurai, T.; Yahaba, M.; Sakurai, Y.; Terada, J.; Tanabe, N.; Tatsumi, K. Features of REM-related sleep disordered breathing in the Japanese population. Intern. Med. 2015, 54, 1481–1487. [Google Scholar] [CrossRef] [Green Version]
- Pamidi, S.; Knutson, K.L.; Ghods, F.; Mokhlesi, B. Depressive symptoms and obesity as predictors of sleepiness and quality of life in patients with REM-related obstructive sleep apnea: Cross-sectional analysis of a large clinical population. Sleep Med. 2011, 12, 827–831. [Google Scholar] [CrossRef]
- Lee, S.-A.; Paek, J.-H.; Han, S.-H. REM-related sleep-disordered breathing is associated with depressive symptoms in men but not in women. Sleep Breath. 2016, 20, 995–1002. [Google Scholar] [CrossRef]
- Armitage, R. Sleep and circadian rhythms in mood disorders. Acta Psychiatr. Scand. 2007, 115, 104–115. [Google Scholar] [CrossRef] [Green Version]
- Eckert, D.J. Phenotypic approaches to obstructive sleep apnoea—New pathways for targeted therapy. Sleep Med. Rev. 2018, 37, 45–59. [Google Scholar] [CrossRef]
- McSharry, D.G.; Saboisky, J.; Deyoung, P.; Jordan, A.S.; Trinder, J.; Smales, E.; Hess, L.; Chamberlin, N.L.; Malhotra, A. Physiological mechanisms of upper airway hypotonia during REM sleep. Sleep 2014, 37, 561–569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Y.; Su, C.; Liu, R.; Lei, G.; Zhang, W.; Yang, T.; Miao, J.; Li, Z. NREM-AHI greater than REM-AHI versus REM-AHI greater than NREM-AHI in patients with obstructive sleep apnea: Clinical and polysomnographic features. Sleep Breath. 2010, 15, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Subramani, Y.; Singh, M.; Wong, J.; Kushida, C.A.; Malhotra, A.; Chung, F. Understanding phenotypes of obstructive sleep apnea. Anesth. Analg. 2017, 124, 179–191. [Google Scholar] [CrossRef] [PubMed]
- Eckert, D.J.; Malhotra, A.; Lo, Y.L.; White, D.P.; Jordan, A.S. The influence of obstructive sleep apnea and gender on genioglossus activity during rapid eye movement sleep. Chest 2008, 135, 957–964. [Google Scholar] [CrossRef] [Green Version]
- Grandner, M.A.; Malhotra, A. Connecting insomnia, sleep apnoea and depression. Respirology 2017, 22, 1249–1250. [Google Scholar] [CrossRef] [Green Version]
- Almeneessier, A.S.; Almousa, Y.; Hammad, O.; Olaish, A.H.; Alanbay, E.T.; Bahammam, A.S. Long-term adherence to continuous positive airway pressure in patients with rapid eye movement-only obstructive sleep apnea: A prospective cohort study. J. Thorac. Dis. 2017, 9, 3755–3765. [Google Scholar] [CrossRef] [Green Version]
- Sweetman, A.; Lack, L.C.; Catcheside, P.; Antic, N.A.; Chai-Coetzer, C.-L.; Smith, S.; Douglas, J.A.; McEvoy, R.D. Developing a successful treatment for co-morbid insomnia and sleep apnoea. Sleep Med. Rev. 2017, 33, 28–38. [Google Scholar] [CrossRef]
- Chami, H.; Baldwin, C.; Silverman, A.; Zhang, Y.; Rapoport, D.; Punjabi, N.M.; Gottlieb, D.J. Sleepiness, quality of life, and sleep maintenance in REM versus non-REM sleep-disordered breathing. Am. J. Respir. Crit. Care Med. 2010, 181, 997–1002. [Google Scholar] [CrossRef] [Green Version]
- Bastien, C. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Soldatos, C.R.; Dikeos, D.G.; Paparrigopoulos, T.J. Athens insomnia scale: Validation of an instrument based on ICD-10 criteria. J. Psychosom. Res. 2000, 48, 555–560. [Google Scholar] [CrossRef]

| (1) NREM-Related OSA (n = 1,312) | (2) REM-Related OSA 1 (n = 424) | (3) REM-Related OSA 2 (n = 292) | (4) REM-Related OSA 3 (n = 155) | p Value | |||
|---|---|---|---|---|---|---|---|
| (1) vs. (2) | (1) vs. (3) | (1) vs. (4) | |||||
| Age | 58 (48–70) | 58 (46–70) | 59 (46–70) | 59 (45–71) | 0.727 | 0.923 | 0.811 |
| Female (%) | 252 (19.2) | 174 (41.0) | 124 (42.5) | 76 (49.0) | <0.001 * | <0.001 * | <0.001 * |
| BMI (kg/m2) | 24.9 (22.5–28.3) | 25.0 (22.3–28.6) | 24.2 (21.9–27.5) | 23.3 (21.5–26.8) | 0.888 | 0.003 * | <0.001 * |
| TST (min) | 460.5 (439.5–489.0) | 456.0 (435.5–490.4) | 459.0 (436.5–494.3) | 463.0 (441.0–493.5) | 0.149 | 0.560 | 0.823 |
| Sleep latency (min) | 6.5 (3.5–12.0) | 7.5 (3.5–13.5) | 7.5 (4.0–14.5) | 7.5 (4.0–17.5) | 0.032 * | 0.021 * | 0.006 * |
| Sleep efficiency (%) | 80.3 (70.1–88.2) | 83.5 (72.8–90.8) | 84.1 (72.3–90.9) | 82.0 (70.2–90.6) | <0.001 * | 0.001 * | 0.147 |
| Stage REM (%) | 15.9 (11.8–20.5) | 17.0 (12.1–21.5) | 17.6 (12.6–21.7) | 17.6 (11.6–21.5) | 0.025 * | 0.005 * | 0.074 |
| Stage N1 (%) | 46.4 (32.9–64.2) | 28.4 (18.9–41.4) | 24.9 (17.2–38.5) | 23.0 (16.2–36.5) | <0.001 * | <0.001 * | <0.001 * |
| Stage N2 (%) | 35.8 (20.0–48.0) | 52.2 (40.8–61.8) | 53.9 (41.7–63.4) | 55.0 (44.9–64.2) | <0.001 * | <0.001 * | <0.001 * |
| Stage N3 (%) | 0 (0–0.1) | 0 (0–0.4) | 0 (0–0.5) | 0 (0–0.2) | 0.064 | 0.053 | 0.363 |
| AHI (events/h) | 35.2 (18.7–55.6) | 15.6 (9.1–22.6) | 11.3 (7.8–15.9) | 8.0 (6.8–9.6) | <0.001 * | <0.001 * | <0.001 * |
| AHI REM (events/h) | 34.3 (13.8–53.8) | 37.9 (25.8–52.8) | 30.0 (20.7–40.6) | 23.7 (17.4–34.4) | <0.001 * | 0.368 | 0.002 * |
| AHI NREM (events/h) | 35.0 (19.2–56.2) | 10.8 (5.9–17.1) | 7.4 (5.1–11.0) | 5.2 (3.8–6.3) | <0.001 * | <0.001 * | <0.001 * |
| Lowest SpO2 (%) | 82.0 (74.0–87.0) | 84.0 (79.0–88.0) | 86.0 (82.0–89.0) | 88.0 (83.0–91.0) | <0.001 * | <0.001 * | <0.001 * |
| CT90 (%) | 1.4 (0.1–7.1) | 0.5 (0.1–2.0) | 0.3 (0–0.9) | 0.1 (0–0.5) | <0.001 * | <0.001 * | <0.001 * |
| Arousal Index (events/h) | 38.2 (27.1–54.5) | 23.3 (16.9–31.7) | 20.9 (15.3–27.1) | 18.8 (13.7–26.4) | <0.001 * | <0.001 * | <0.001 * |
| PLMI (events/h) | 0 (0–7.7) | 0 (0–11.0) | 0 (0–12.4) | 0 (0–10.8) | 0.057 | 0.042 * | 0.117 |
| ESS | 8 (5–12) | 8 (5–11) | 8 (5–11) | 8 (5–12) | 0.094 | 0.310 | 0.356 |
| Male | 8 (5–12) | 8 (5–12) | 8 (5–11) | 8 (5–12) | 0.782 | 0.723 | 0.903 |
| Female | 7 (5–12) | 7 (4–11) | 8 (4–11) | 7 (4–11.8) | 0.118 | 0.520 | 0.469 |
| PSQI | 6 (4–9) | 7 (5–11) | 8 (5–12) | 9 (5–12) | <0.001 * | <0.001 * | <0.001 * |
| Male | 6 (4–9) | 6 (4–10) | 7 (4–10) | 7 (4–12) | 0.089 | 0.044 * | 0.035 * |
| Female | 7 (4–10) | 10 (6–13) | 10 (7–13) | 10.5 (7–13) | <0.001 * | <0.001 * | <0.001 * |
| REM-Related OSA 1 | REM-Related OSA 2 | REM-Related OSA 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p Value | Coefficient | 95% CI | p Value | Coefficient | 95% CI | p Value | |
| Unadjusted | 1.217 | 0.786–1.646 | <0.0001 * | 1.492 | 0.994–1.989 | <0.0001 * | 1.968 | 1.318–2.618 | <0.0001 |
| Model 1 | 0.938 | 0.500–1.376 | <0.0001 * | 1.221 | 0.715–1.726 | <0.0001 * | 1.679 | 1.013–2.344 | <0.0001 |
| Model 2-a | 0.968 | 0.529–1.406 | <0.0001 * | 1.195 | 0.689–1.702 | <0.0001 * | 1.637 | 0.968–2.304 | <0.0001 |
| Model 2-b | 0.563 | 0.070–1.057 | 0.025 * | 0.832 | 0.261–1.402 | 0.004 * | 1.260 | 0.538–1.981 | 0.001 |
| REM-Related OSA 1 | REM-Related OSA 2 | REM-Related OSA 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p Value | Coefficient | 95% CI | p Value | Coefficient | 95% CI | p Value | |
| Unadjusted | 0.500 | −1.054–1.027 | 0.063 | 0.684 | 0.061–1.307 | 0.032 | 1.057 | 0.183–1.932 | 0.018 |
| Model 1 | 0.426 | −0.103–0.955 | 0.114 | 0.637 | 0.013–1.262 | 0.045 | 1.048 | 0.168–1.927 | 0.020 |
| Model 2-a | 0.463 | −0.066–0.992 | 0.086 | 0.592 | −0.033–1.216 | 0.063 | 0.970 | 0.090–1.851 | 0.031 |
| Model 2-b | −0.030 | −0.624–0.564 | 0.922 | 0.152 | −0.547–0.850 | 0.670 | 0.424 | −0.516–1.363 | 0.376 |
| REM-Related OSA 1 | REM-Related OSA 2 | REM-Related OSA 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p Value | Coefficient | 95% CI | p Value | Coefficient | 95% CI | p Value | |
| Unadjusted | 1.828 | 1.039–2.617 | <0.0001 | 2.155 | 1.279–3.031 | <0.0001 | 2.436 | 1.393–3.480 | <0.0001 |
| Model 1 | 1.775 | 0.985–2.565 | <0.0001 | 2.113 | 1.233–2.992 | <0.0001 | 2.382 | 1.333–3.432 | <0.0001 |
| Model 2-a | 1.778 | 0.984–2.572 | <0.0001 | 2.126 | 1.244–3.008 | <0.0001 | 2.410 | 1.353–3.468 | <0.0001 |
| Model 2-b | 1.548 | 0.646–2.450 | 0.001 | 1.930 | 0.906–2.954 | 0.001 | 2.185 | 0.992–3.378 | 0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hoshino, T.; Sasanabe, R.; Murotani, K.; Hori, R.; Mano, M.; Nomura, A.; Konishi, N.; Baku, M.; Arita, A.; Kuczynski, W.; et al. Insomnia as a Symptom of Rapid Eye Movement-Related Obstructive Sleep Apnea. J. Clin. Med. 2020, 9, 1821. https://doi.org/10.3390/jcm9061821
Hoshino T, Sasanabe R, Murotani K, Hori R, Mano M, Nomura A, Konishi N, Baku M, Arita A, Kuczynski W, et al. Insomnia as a Symptom of Rapid Eye Movement-Related Obstructive Sleep Apnea. Journal of Clinical Medicine. 2020; 9(6):1821. https://doi.org/10.3390/jcm9061821
Chicago/Turabian StyleHoshino, Tetsuro, Ryujiro Sasanabe, Kenta Murotani, Reiko Hori, Mamiko Mano, Atsuhiko Nomura, Noriyuki Konishi, Masayo Baku, Aki Arita, Wojciech Kuczynski, and et al. 2020. "Insomnia as a Symptom of Rapid Eye Movement-Related Obstructive Sleep Apnea" Journal of Clinical Medicine 9, no. 6: 1821. https://doi.org/10.3390/jcm9061821
APA StyleHoshino, T., Sasanabe, R., Murotani, K., Hori, R., Mano, M., Nomura, A., Konishi, N., Baku, M., Arita, A., Kuczynski, W., & Shiomi, T. (2020). Insomnia as a Symptom of Rapid Eye Movement-Related Obstructive Sleep Apnea. Journal of Clinical Medicine, 9(6), 1821. https://doi.org/10.3390/jcm9061821





