The Effects of MELD-Based Liver Allocation on Patient Survival and Waiting List Mortality in a Country with a Low Donation Rate
Abstract
:1. Introduction
2. Patients and Methods
2.1. Retrospective Single-Center Analysis
2.2. Analysis of the Development in the ET Region and Germany
2.3. Statistical Analysis
3. Results
3.1. Retrospective Single-Center Analysis
Patient Demographics
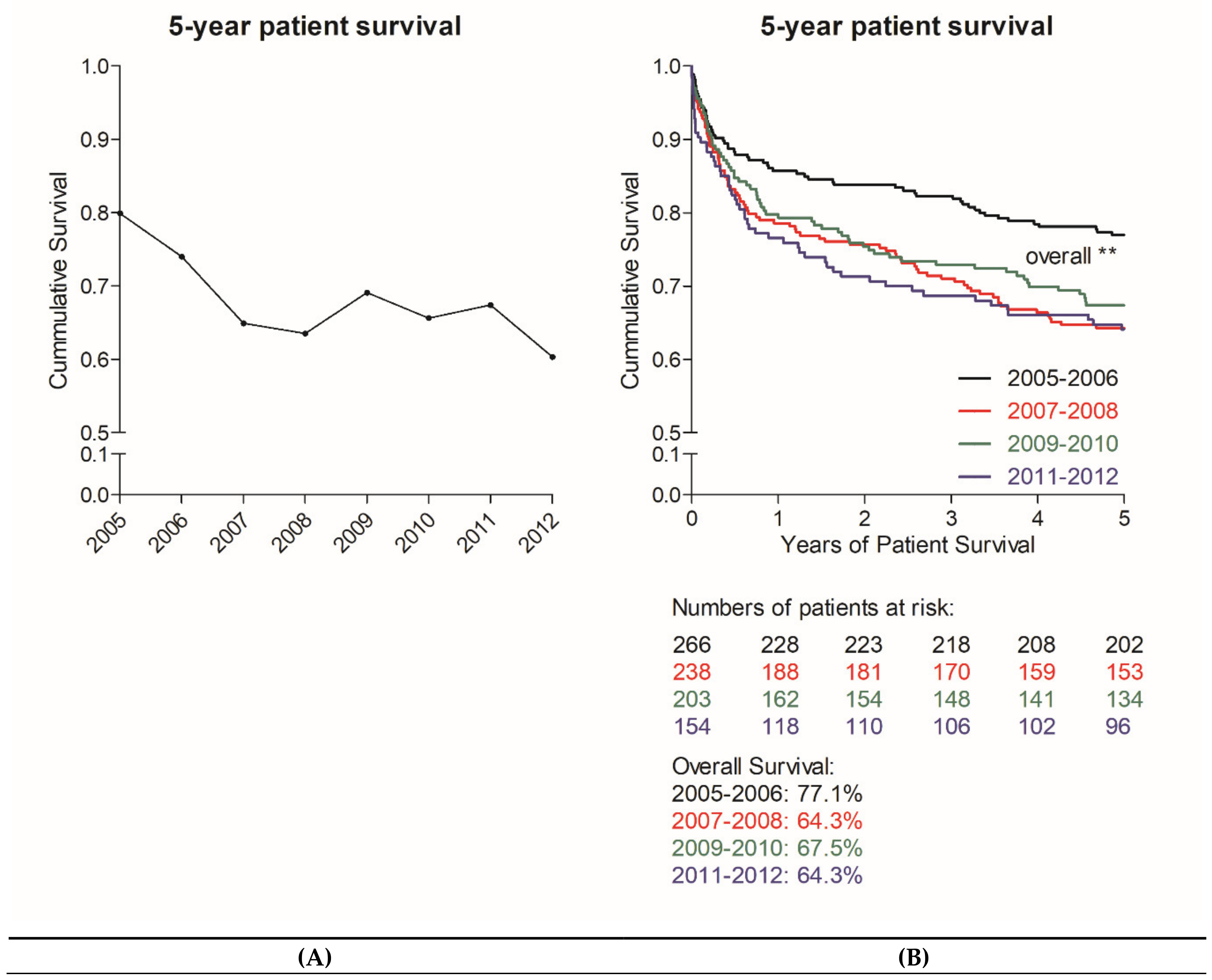
3.2. Development of Patient Survival
3.3. Analysis of the Development in Germany Compared to the ET Region
3.3.1. MELD Development and Patient Survival
3.3.2. Waiting List Development in Germany
3.4. Donor and Organ Recovery Development in Germany Compared to the ET Region
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| BMI | body mass index |
| CI | confidence interval |
| CIT | cold ischemia time |
| CVA | cerebrovascular accident |
| DSO | German Organ Transplantation Foundation |
| ET | Eurotransplant |
| FFP | fresh frozen plasma |
| HU | high urgency |
| ICH | intracranial hemorrhage |
| ICU | intensive care unit |
| IQR | interquartile range |
| ITBL | ischemic type biliary lesions |
| LT | liver transplantation |
| MELD | Model for End-Stage Liver Disease |
| SAH | subarachnoid hemorrhage |
| TBI | traumatic brain injury |
| WIT | warm ischemia time |
References
- Schulte, K.; Borzikowsky, C.; Rahmel, A.; Kolibay, F.; Polze, N.; Frankel, P.; Mikle, S.; Alders, B.; Kunzendorf, U.; Feldkamp, T. Decline in Organ Donation in Germany. Dtsch. Arztebl. Int. 2018, 115, 463–468. [Google Scholar] [CrossRef]
- Dutkowski, P.; Oberkofler, C.E.; Bechir, M.; Mullhaupt, B.; Geier, A.; Raptis, D.A.; Clavien, P.A. The model for end-stage liver disease allocation system for liver transplantation saves lives, but increases morbidity and cost: A prospective outcome analysis. Liver Transpl. 2011, 17, 674–684. [Google Scholar] [CrossRef]
- Schilsky, M.L.; Moini, M. Advances in liver transplantation allocation systems. World J. Gastroenterol. 2016, 22, 2922–2930. [Google Scholar] [CrossRef]
- Schlitt, H.J.; Loss, M.; Scherer, M.N.; Becker, T.; Jauch, K.W.; Nashan, B.; Schmidt, H.; Settmacher, U.; Rogiers, X.; Neuhaus, P.; et al. Current developments in liver transplantation in Germany: MELD-based organ allocation and incentives for transplant centres. Z. Gastroenterol. 2011, 49, 30–38. [Google Scholar] [CrossRef]
- Tacke, F.; Kroy, D.C.; Barreiros, A.P.; Neumann, U.P. Liver transplantation in Germany. Liver Transpl. 2016, 22, 1136–1142. [Google Scholar] [CrossRef]
- Wiesner, R.; Edwards, E.; Freeman, R.; Harper, A.; Kim, R.; Kamath, P.; Kremers, W.; Lake, J.; Howard, T.; Merion, R.M.; et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology 2003, 124, 91–96. [Google Scholar] [CrossRef] [Green Version]
- Weismuller, T.J.; Fikatas, P.; Schmidt, J.; Barreiros, A.P.; Otto, G.; Beckebaum, S.; Paul, A.; Scherer, M.N.; Schmidt, H.H.; Schlitt, H.J.; et al. Multicentric evaluation of model for end-stage liver disease-based allocation and survival after liver transplantation in Germany—limitations of the ‘sickest first’-concept. Transpl. Int. 2011, 24, 91–99. [Google Scholar] [CrossRef]
- Rana, A.; Hardy, M.A.; Halazun, K.J.; Woodland, D.C.; Ratner, L.E.; Samstein, B.; Guarrera, J.V.; Brown, R.S., Jr.; Emond, J.C. Survival outcomes following liver transplantation (SOFT) score: A novel method to predict patient survival following liver transplantation. Am. J. Transpl. 2008, 8, 2537–2546. [Google Scholar] [CrossRef]
- Cywinski, J.B.; Mascha, E.J.; You, J.; Sessler, D.I.; Kapural, L.; Argalious, M.; Parker, B.M. Pre-transplant MELD and sodium MELD scores are poor predictors of graft failure and mortality after liver transplantation. Hepatol. Int. 2011, 5, 841–849. [Google Scholar] [CrossRef]
- Schaubel, D.E.; Guidinger, M.K.; Biggins, S.W.; Kalbfleisch, J.D.; Pomfret, E.A.; Sharma, P.; Merion, R.M. Survival benefit-based deceased-donor liver allocation. Am. J. Transpl. 2009, 9, 970–981. [Google Scholar] [CrossRef] [Green Version]
- Eurotransplant Statistics Report Library. Available online: http://statistics.eurotransplant.org/ (accessed on 3 May 2020).
- Tätigkeitsberichte und Qualitätsberichte. Available online: https://www.dso.de/servicecenter/krankenhaeuser/transplantationszentren.html (accessed on 3 May 2020).
- Annual Reports. Available online: https://www.eurotransplant.org/cms/index.php?page=annual_reports (accessed on 3 May 2020).
- Peschel, G.; Kraft, I.C.; Scherer, M.; Sinner, B.; Huber, K.; Müller-Schilling, M.; Weigand, K. Wartelistenmortalität bei der Lebertransplantation—the dark side of liver transplantation. Z. Gastroenterol. 2018, 56, e15. [Google Scholar] [CrossRef]
- Linecker, M.; Krones, T.; Berg, T.; Niemann, C.U.; Steadman, R.H.; Dutkowski, P.; Clavien, P.A.; Busuttil, R.W.; Truog, R.D.; Petrowsky, H. Potentially inappropriate liver transplantation in the era of the “sickest first” policy—A search for the upper limits. J. Hepatol. 2018, 68, 798–813. [Google Scholar] [CrossRef] [Green Version]
- Branger, P.; Samuel, U. Eurotransplant International Foundation; Annual Report; Eurotransplant: Leiden, The Netherlands, 2017; p. 2301. [Google Scholar]
- Benckert, C.; Quante, M.; Thelen, A.; Bartels, M.; Laudi, S.; Berg, T.; Kaisers, U.; Jonas, S. Impact of the MELD allocation after its implementation in liver transplantation. Scand. J. Gastroenterol. 2011, 46, 941–948. [Google Scholar] [CrossRef]
- Weismuller, T.J.; Negm, A.; Becker, T.; Barg-Hock, H.; Klempnauer, J.; Manns, M.P.; Strassburg, C.P. The introduction of MELD-based organ allocation impacts 3-month survival after liver transplantation by influencing pretransplant patient characteristics. Transpl. Int. 2009, 22, 970–978. [Google Scholar] [CrossRef]
- Agopian, V.G.; Petrowsky, H.; Kaldas, F.M.; Zarrinpar, A.; Farmer, D.G.; Yersiz, H.; Holt, C.; Harlander-Locke, M.; Hong, J.C.; Rana, A.R.; et al. The evolution of liver transplantation during 3 decades: Analysis of 5347 consecutive liver transplants at a single center. Ann. Surg. 2013, 258, 409–421. [Google Scholar] [CrossRef]
- Palmiero, H.O.; Kajikawa, P.; Boin, I.F.; Coria, S.; Pereira, L.A. Liver recipient survival rate before and after model for end-stage liver disease implementation and use of donor risk index. Transpl. Proc. 2010, 42, 4113–4115. [Google Scholar] [CrossRef]
- Freeman, R.B.; Wiesner, R.H.; Edwards, E.; Harper, A.; Merion, R.; Wolfe, R. United Network for Organ Sharing Organ Procurement and Transplantation Network Liver and Transplantation Committee. Results of the first year of the new liver allocation plan. Liver Transpl. 2004, 10, 7–15. [Google Scholar] [CrossRef]
- De la Mata, M.; Cuende, N.; Huet, J.; Bernardos, A.; Ferron, J.A.; Santoyo, J.; Pascasio, J.M.; Rodrigo, J.; Solorzano, G.; Martin-Vivaldi, R.; et al. Model for end-stage liver disease score-based allocation of donors for liver transplantation: A spanish multicenter experience. Transplantation 2006, 82, 1429–1435. [Google Scholar] [CrossRef]
- Waitlist Mortality Rate. Available online: https://www.srtr.org/about-the-data/guide-to-key-transplant-program-metrics/txguidearticles/waitlist-mortality-rate/ (accessed on 26 November 2018).





| All | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | Correlation | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 861 | n = 139 | n = 127 | n = 134 | n = 104 | n = 110 | n = 93 | n = 86 | n = 68 | Method p-Value | ||
| Age at LT * | 53.1 (±10.3) | 49.9 (±11.0) | 51.1 (±11.1) | 55.0 (±7.4) | 55.9 (±9.8) | 53.2 (±10.6) | 53.6 (±10.3) | 53.7 (±10.1) | 54.2 (±10.4) | R 0.108 | 0.001 |
| Male sex *** | 560 (65.0%) | 83 (59.7%) | 83 (65.4%) | 87 (64.9%) | 72 (69.2%) | 67 (60.9%) | 57 (61.3%) | 64 (74.4%) | 47 (69.1%) | Rho | 0.149 |
| BMI (kg/m2) * | 26.4 (±4.9) | 25.2 (±4.2) | 25.5 (±4.9) | 26.9 (±4.6) | 25.8 (±4.7) | 27.3 (±4.7) | 27.0 (±5.9) | 27.0 (±5.0) | 27.0 (±5.0) | R 0.133 | <0.001 |
| Indication *** | |||||||||||
| Cirrhosis | 347 (40.3%) | 47 (33.8%) | 50 (39.4%) | 63 (47.0%) | 41 (39.4%) | 46 (41.8%) | 42 (45.2%) | 33 (38.4%) | 25 (36.8%) | ||
| Virus-related | 77 (8.9%) | 16 (11.5%) | 18 (14.2%) | 14 (10.4%) | 7 (6.5%) | 6 (5.4%) | 8 (8.6%) | 3 (3.5%) | 5 (7.6%) | ||
| Alcoholism | 205 (23.8%) | 22 (15.8%) | 27 (21.3%) | 41 (31.6%) | 30 (28.8%) | 23 (20.9%) | 26 (28.0%) | 23 (26.7%) | 13 (19.1%) | ||
| Combined viral + alcoholic | 9 (1.0%) | 2 (1.4%) | 0 | 1 (0.7%) | 1 (1.0%) | 2 (1.8%) | 1 (1.1%) | 0 | 2 (2.9%) | ||
| Other | 71 (6.4%) | 7 (5.0%) | 5 (3.9%) | 7 (5.2%) | 3 (2.9%) | 15 (13.6%) | 7 (7.5%) | 7 (8.1%) | 5 (7.6%) | ||
| Liver tumor | 241 (28.0%) | 28 (20.1%) | 30 (23.6%) | 34 (25.4%) | 38 (36.5%) | 36 (32.7%) | 28 (30.1%) | 26 (30.2%) | 21 (30.9%) | ||
| Retransplantation | 120 (13.9%) | 30 (21.6%) | 19 (15.0%) | 18 (13.4%) | 11 (10.6%) | 11 (10.0%) | 13 (14.0%) | 10 (11.6%) | 8 (11.8%) | ||
| Primary non-function | 28 (3.3%) | 9 (6.5%) | 4 (3.1%) | 2 (1.5%) | 3 (2.9%) | 3 (2.7%) | 4 (4.3%) | 3 (3.5%) | 0 | ||
| Hepatic artery thrombosis | 29 (3.4%) | 11 (7.9%) | 7 (5.5%) | 3 (2.2%) | 1 (1.0%) | 1 (0.9%) | 3 (3.2%) | 1 (1.2%) | 2 (2.9%) | ||
| ITBL | 26 (2.4%) | 4 (2.9%) | 0 | 7 (5.2%) | 3 (2.9%) | 3 (2.7%) | 2 (2.2%) | 1 (1.2%) | 1 (1.5%) | ||
| Recurrent disease | 16 (1.9%) | 2 (1.4%) | 4 (3.1%) | 2 (1.5%) | 1 (1.0%) | 0 | 1 (1.1%) | 4 (4.7%) | 2 (2.9%) | ||
| Rejection | 9 (1.0%) | 2 (1.4%) | 1 (0.8%) | 0 | 2 (1.9%) | 2 (1.8%) | 1 (1.1%) | 0 | 1 (1.5%) | ||
| Other | 17 (1.4%) | 2 (1.4%) | 3 (2.4%) | 4 (3.0%) | 1 (1.0%) | 2 (1.8%) | 2 (2.2%) | 1 (1.2%) | 2 (2.9%) | ||
| Cholestatic disease | 65 (7.5%) | 19 (13.7%) | 9 (7.1%) | 10 (7.5%) | 7 (6.7%) | 5 (4.5%) | 6 (6.5%) | 6 (7.0%) | 3 (4.4%) | ||
| Acute liver failure | 34 (3.9%) | 3 (2.2%) | 9 (7.1%) | 6 (4.5%) | 2 (1.9%) | 7 (6.4%) | 1 (1.1%) | 5 (5.8%) | 1 (1.5%) | ||
| Other | 54 (6.3%) | 12 (8.6%) | 7 (5.5%) | 3 (2.2%) | 5 (4.8%) | 5 (4.5%) | 3 (3.2%) | 6 (7.0%) | 10 (14.7%) | ||
| Listing details | |||||||||||
| Waiting time in days ** | 106 (17.5–327.5) | 182 (56–471) | 141 (24–441) | 61 (12.75–275) | 102 (29–228.5) | 77.5 (8.75–242) | 96 (20–325.5) | 111 (19–324.25) | 47 (11.5–227) | Rho −0.127 | <0.001 |
| Allocation labMELD * | 19.5 (±10.2) | 15.8 (±6.7) | 18.3 (±9.1) | 20.3 (±10.3) | 19.2 (±10.3) | 21.6 (±11.8) | 20.9 (±10.5) | 20.2 (±11.4) | 20.1 (±10.7) | R 0.121 | <0.001 |
| matchMELD * | 23.3 (±10.6) | 19.3 (±11.0) | 19.6 (±10.8) | 21.6 (±10.5) | 23.4 (±9.7) | 27.6 (±9.2) | 26.1 (±9.6) | 26.6 (±10.1) | 25.5 (±9.5) | R 0.259 | <0.001 |
| labMELD prior OLT * | 19.7 (±10.2) | 18.8 (±9.0) | 19.2 (±9.6) | 19.9 (±10.0) | 19.0 (±10.0) | 21.4 (±11.6) | 20.1 (±9.8) | 20.0 (±11.1) | 19.8 (±10.6) | R | 0.248 |
| High urgency status *** | 133 (12.1%) | 22 (15.8%) | 20 (15.7%) | 9 (6.7%) | 7 (6.7%) | 13 (11.8%) | 9 (9.7%) | 8 (9.3%) | 6 (8.8%) | Rho −0.069 | 0.043 |
| Retransplantation *** | 120 (13.9%) | 30 (21.6%) | 19 (15.0%) | 18 (13.4%) | 11 (10.6%) | 11 (10.0%) | 13 (14.0%) | 10 (11.6%) | 8 (11.8%) | Rho −0.079 | 0.02 |
| First retransplant | 103(12.0%) | 26 (18.7%) | 15 (11.8%) | 16 (11.9%) | 11 (10.6%) | 11 (10.0%) | 11 (11.8%) | 7 (8.1%) | 6 (8.8%) | ||
| Second retransplant | 16 (1.9%) | 4 (2.9%) | 4 (3.1%) | 2 (1.5%) | 2 (2.2%) | 2 (2.3%) | 2 (2.9%) | ||||
| Third retransplant | 1 (0.1%) | 1 (1.2%) | |||||||||
| Graft and surgical parameters | |||||||||||
| CIT (min) * | 578.1 (±166.3) | 585.1 (±142.1) | 554.5 (±173.8) | 601.2 (±164.6) | 626.8 (±172.7) | 574.5 (±154.1) | 556.9 (±170.6) | 546.3 (±195.7) | 562.6 (±147.9) | R | 0.122 |
| Operating time (min) * | 316 (±86.1) | 330 (±94.3) | 316.5 (±73.2) | 310.5 (±84.4) | 332.9 (±82.7) | 337.7 (±80.2) | 337.6 (±87.1) | 336.5 (±91.3) | 365.3 (±90.2) | R 0.119 | <0.001 |
| WIT (min) * | 46.4 (±12.1) | 45.7 (±10.7) | 42.4 (±10.0) | 41.0 (±9.2) | 45.0 (±13.3) | 50.2 (±12.5) | 48.7 (±12.8) | 50.5 (±10.7) | 50.1 (±14.5) | R 0.218 | <0.001 |
| Erythrocyte concentrate ** | 6 (3–10) | 4 (2–6) | 4 (2–6) | 6 (3–10) | 7 (4–13) | 6 (3–10) | 6 (4–11.75) | 6.5 (3–12) | 9.5 (6–14) | Rho 0.272 | <0.001 |
| FFP ** | 18 (13–28) | 12 (8–17) | 13 (10–20) | 19 (13–27) | 22 (16–35) | 21 (16–30) | 22.5 (15–32) | 20 (14–28.5) | 22 (15.25–38.75) | Rho 0.351 | <0.001 |
| Post-transplant ICU stay ** | 9 (6–19) | 8 (6–14) | 9 (6–20) | 7 (4.75–16.5) | 9 (6–15) | 9 (5–22) | 11 (6–23) | 10.5 (6–26.5) | 13 (7–22.75) | Rho 0.10 | 0.003 |
| Post-transplant hospital stay ** | 30 (22–52.5) | 30 (25–44) | 28 (22–49) | 27.5 (22–54.25) | 29.5 (21–49.75) | 36 (25–56.25) | 35 (21.5–50) | 33.5 (21.75–56) | 33 (18.25–60.5) | Rho | 0.336 |
| Donor characteristics | |||||||||||
| Age * | 52.6 (±17.1) | 50.1 (±16.7) | 50.1 (±17.9) | 51.9 (±18.1) | 52.0 (±16.5) | 56.5 (±15.0) | 51.4 (±18.3) | 55.0 (±16.0) | 57.2 (±16.6) | R 0.118 | 0.001 |
| Male sex *** | 427 (49.6%) | 62 (44.6%) | 67 (52.8%) | 67 (50.0%) | 49 (47.1%) | 53 (48.2%) | 50 (53.8%) | 44 (51.2%) | 35 (51.5%) | Rho | 0.39 |
| BMI (kg/m2) * | 26.0 (±4.5) | 25.7 (±4.6) | 25.6 (±4.3) | 26.3 (±4.6) | 26.3 (±4.7) | 26.5 (±3.6) | 25.5 (±4.2) | 26.5 (±5.9) | 25.4 (±3.5) | R | 0.578 |
| ICU stay ** | 3 (2–7) | 3 (1.5–8) | 4 (2–6.25) | 3 (1–7) | 4 (2–8) | 3 (2–5) | 3 (1–7.5) | 4 (2–9) | 2.5 (1–5.5) | Rho | 0.667 |
| Reanimation *** | 153 (17.8%) | 20 (14.4%) | 20 (15.7%) | 15 (11.2%) | 27 (26.0%) | 28 (25.5%) | 19 (20.4%) | 13 (15.1%) | 11 (16.2%) | Rho | 0.167 |
| Cause of death *** | |||||||||||
| SAH | 433 (50.3%) | 80 (57.6%) | 62(48.8%) | 65 (48.5%) | 52 (50.0%) | 60 (54.5%) | 38 (40.9%) | 39 (45.3%) | 37 (54.4%) | ||
| TBI | 132 (15.3%) | 18 (12.9%) | 24 (18.9%) | 27 (20.1%) | 12 (11.5%) | 13 (11.8%) | 15 (16.1%) | 15 (17.4%) | 8 (11.8%) | ||
| Hypoxia | 114 (13.2%) | 18 (12.9%) | 14 (11.0%) | 13 (9.7%) | 21 (20.2%) | 13 (11.8%) | 17 (18.3%) | 11 (12.8%) | 7 (10.3%) | ||
| CVA | 91 (10.6%) | 11 (7.9%) | 13 (10.2%) | 13 (9.7%) | 10 (9.6%) | 14 (12.7%) | 9 (9.7%) | 13 (15.1%) | 8 (11.8%) | ||
| ICH | 50 (5.8%) | 7 (5.0%) | 9 (6.7%) | 8 (6.3%) | 4 (3.8%) | 5 (4.5%) | 8 (8.6%) | 4 (4.8%) | 5 (7.4%) | ||
| Other | 41 (4.7%) | 5 (3.6%) | 6 (4.7%) | 7 (5.2%) | 5 (4.8%) | 5 (4.5%) | 6 (6.5%) | 4 (4.8%) | 3 (4.4%) | ||
| 5-Year Survivors | 5-Year Non-Survivors | p-Value | |
|---|---|---|---|
| n = 594 | n = 267 | ||
| Age at LT * | 52.7 (±10.4) | 54.1 (±9.9) | 0.063 |
| Male sex *** | 365 (61.4%) | 195 (73.0%) | 0.001 |
| BMI (kg/m2) * | 26.5 (±4.9) | 26.2 (±5.0) | 0.399 |
| Indication *** | <0.001 | ||
| Liver tumor | 154 (25.9%) | 87 (32.6%) | |
| Cirrhosis | 263 (44.3%) | 84 (31.5%) | |
| Retransplantation | 63 (10.6%) | 57 (21.3%) | |
| Acute liver failure | 26 (4.4%) | 8 (3.0%) | |
| Other | 88 (14.8%) | 31 (11.6%) | |
| Listing Details | |||
| labMELD * | 18.8 (±9.8) | 21.0 (±10.9) | 0.02 |
| matchMELD * | 22.6 (±10.3) | 25.0 (±11.0) | 0.005 |
| High urgency status *** | 64 (10.8%) | 30 (11.2%) | 0.841 |
| Place *** | |||
| Home | 438 (73.7%) | 155 (58.1%) | <0.001 |
| Regular ward | 60 (10.1%) | 46 (17.2%) | |
| ICU | 96 (16.2%) | 66 (24.7%) | |
| Dialysis prior to transplantation *** | 64 (10.8%) | 67 (25.1%) | <0.001 |
| Graft and surgical parameters | |||
| Cold ischemia time * | 569.2 (±167.7) | 598.1 (±161.8) | 0.018 |
| Erythrocyte concentrate ** | 5 (2–8) | 7 (4–12) | <0.001 |
| FFP ** | 17 (12–25) | 20 (15–31) | <0.001 |
| Donor Characteristics | |||
| Age * | 51.8 (±17.3) | 54.4 (±16.5) | 0.036 |
| BMI (kg/m2) * | 26.0 (±4.6) | 26.0 (±4.2) | 0.874 |
| Risk Scores | |||
| D-MELD * | 956 (±574) | 1099 (±624) | <0.001 |
| Donor risk index * | 2.4 (±0.5) | 2.5 (±0.5) | 0.008 |
| Balance of risk score * | 8.0 (±5.5) | 10.5 (±6.7) | <0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ritschl, P.V.; Wiering, L.; Dziodzio, T.; Jara, M.; Kruppa, J.; Schoeneberg, U.; Raschzok, N.; Butz, F.; Globke, B.; Seika, P.; et al. The Effects of MELD-Based Liver Allocation on Patient Survival and Waiting List Mortality in a Country with a Low Donation Rate. J. Clin. Med. 2020, 9, 1929. https://doi.org/10.3390/jcm9061929
Ritschl PV, Wiering L, Dziodzio T, Jara M, Kruppa J, Schoeneberg U, Raschzok N, Butz F, Globke B, Seika P, et al. The Effects of MELD-Based Liver Allocation on Patient Survival and Waiting List Mortality in a Country with a Low Donation Rate. Journal of Clinical Medicine. 2020; 9(6):1929. https://doi.org/10.3390/jcm9061929
Chicago/Turabian StyleRitschl, Paul V., Leke Wiering, Tomasz Dziodzio, Maximilian Jara, Jochen Kruppa, Uwe Schoeneberg, Nathanael Raschzok, Frederike Butz, Brigitta Globke, Philippa Seika, and et al. 2020. "The Effects of MELD-Based Liver Allocation on Patient Survival and Waiting List Mortality in a Country with a Low Donation Rate" Journal of Clinical Medicine 9, no. 6: 1929. https://doi.org/10.3390/jcm9061929
APA StyleRitschl, P. V., Wiering, L., Dziodzio, T., Jara, M., Kruppa, J., Schoeneberg, U., Raschzok, N., Butz, F., Globke, B., Seika, P., Maurer, M., Biebl, M., Schöning, W., Schmelzle, M., Sauer, I. M., Tacke, F., Öllinger, R., & Pratschke, J. (2020). The Effects of MELD-Based Liver Allocation on Patient Survival and Waiting List Mortality in a Country with a Low Donation Rate. Journal of Clinical Medicine, 9(6), 1929. https://doi.org/10.3390/jcm9061929








