Childhood Trauma Predicts Less Remission from PTSD among Patients with Co-Occurring Alcohol Use Disorder and PTSD
Abstract
1. Introduction
2. Experimental Section
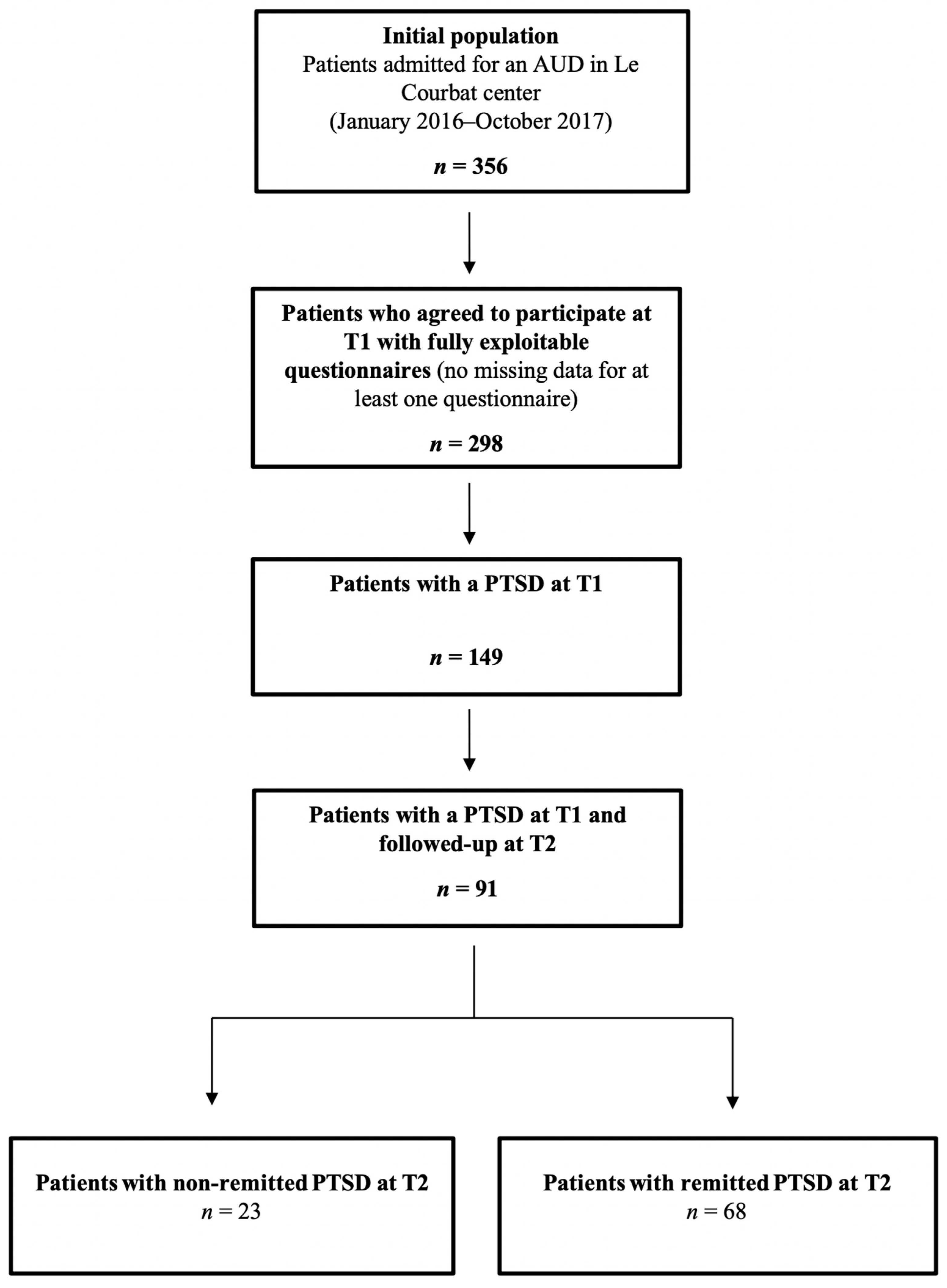
2.1. Participants and Procedure
2.2. Measures
2.2.1. Childhood Trauma
2.2.2. Lifetime Exposure to Traumatic Events
2.2.3. Post-Traumatic Stress Disorder
2.2.4. Alcohol Use Disorder
2.3. Statistical Analyses and Ethics
3. Results
3.1. Descriptive Statistics
3.2. Factors Associated with PTSD Remission in Univariate Analyses
3.3. Factors Associated with PTSD Remission in Multivariate Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Carvalho, A.F.; Heilig, M.; Perez, A.; Probst, C.; Rehm, J. Alcohol use disorders. Lancet 2019, 394, 781–792. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: Dsm-5, 5th ed.; American Psychiatric Association Publishing: Washington, DC, USA, 2013; ISBN 978-0-89042-555-8. [Google Scholar]
- Rehm, J.; Mathers, C.; Popova, S.; Thavorncharoensap, M.; Teerawattananon, Y.; Patra, J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet 2009, 373, 2223–2233. [Google Scholar] [CrossRef]
- Torrens, M.; Rossi, P.C.; Martinez-Riera, R.; Martinez-Sanvisens, D.; Bulbena, A. Psychiatric Co-Morbidity and Substance Use Disorders: Treatment in Parallel Systems or in One Integrated System? Subst. Use Misuse 2012, 47, 1005–1014. [Google Scholar] [CrossRef] [PubMed]
- Blanco, C.; Xu, Y.; Brady, K.; Pérez-Fuentes, G.; Okuda, M.; Wang, S. Comorbidity of posttraumatic stress disorder with alcohol dependence among US adults: Results from National Epidemiological Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2013, 132, 630–638. [Google Scholar] [CrossRef]
- Kessler, R.C.; Sonnega, A.; Bromet, E.; Hughes, M.; Nelson, C.B. Posttraumatic stress disorder in the National Comorbidity Survey. Arch. Gen. Psychiatry 1995, 52, 1048–1060. [Google Scholar] [CrossRef]
- Khoury, L.; Tang, Y.L.; Bradley, B.; Cubells, J.F.; Ressler, K.J. Substance use, childhood traumatic experience, and Posttraumatic Stress Disorder in an urban civilian population. Depress. Anxiety 2010, 27, 1077–1086. [Google Scholar] [CrossRef]
- Norman, S.B.; Haller, M.; Hamblen, J.L.; Southwick, S.M.; Pietrzak, R.H. The burden of co-occurring alcohol use disorder and PTSD in U.S. Military veterans: Comorbidities, functioning, and suicidality. Psychol. Addict. Behav. 2018, 32, 224–229. [Google Scholar] [CrossRef]
- Dore, G.; Mills, K.; Murray, R.; Teesson, M.; Farrugia, P. Post-traumatic stress disorder, depression and suicidality in inpatients with substance use disorders. Drug Alcohol Rev. 2012, 31, 294–302. [Google Scholar] [CrossRef]
- Drapkin, M.L.; Yusko, D.; Yasinski, C.; Oslin, D.; Hembree, E.A.; Foa, E.B. Baseline functioning among individuals with posttraumatic stress disorder and alcohol dependence. J. Subst. Abus. Treat. 2011, 41, 186–192. [Google Scholar] [CrossRef][Green Version]
- Back, S.E.; Brady, K.T.; Sonne, S.C.; Verduin, M.L. Symptom Improvement in Co-Occurring PTSD and Alcohol Dependence. J. Nerv. Ment. Dis. 2006, 194, 690–696. [Google Scholar] [CrossRef]
- Chapman, C.; Mills, K.; Slade, T.; McFarlane, A.C.; Bryant, R.A.; Creamer, M.; Silove, D.; Teesson, M. Remission from post-traumatic stress disorder in the general population. Psychol. Med. 2012, 42, 1695–1703. [Google Scholar] [CrossRef]
- Müller, M.; Ajdacic-Gross, V.; Rodgers, S.; Kleim, B.; Seifritz, E.; Vetter, S.; Egger, S.T.; Rössler, W.; Castelao, E.; Preisig, M.; et al. Predictors of remission from PTSD symptoms after sexual and non-sexual trauma in the community: A mediated survival-analytic approach. Psychiatry Res. 2018, 260, 262–271. [Google Scholar] [CrossRef]
- Rosellini, A.J.; Liu, H.; Petukhova, M.V.; Sampson, N.A.; Aguilar-Gaxiola, S.; Alonso, J.; Borges, G.; Bruffaerts, R.; Bromet, E.J.; de Girolamo, G.; et al. Recovery from DSM-IV post-traumatic stress disorder in the WHO World Mental Health surveys. Psychol. Med. 2018, 48, 437–450. [Google Scholar] [CrossRef]
- Steinert, C.; Hofmann, M.; Leichsenring, F.; Kruse, J. The course of PTSD in naturalistic long-term studies: High variability of outcomes. A systematic review. Nord. J. Psychiatry 2015, 69, 483–496. [Google Scholar] [CrossRef]
- Dworkin, E.R.; Wanklyn, S.; Stasiewicz, P.R.; Coffey, S.F. PTSD symptom presentation among people with alcohol and drug use disorders: Comparisons by substance of abuse. Addict. Behav. 2018, 76, 188–194. [Google Scholar] [CrossRef] [PubMed]
- Grundmann, J.; Lincoln, T.M.; Lüdecke, D.; Bong, S.; Schulte, B.; Verthein, U.; Schäfer, I. Traumatic Experiences, Revictimization and Posttraumatic Stress Disorder in German Inpatients Treated for Alcohol Dependence. Subst. Use Misuse 2017, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.-C.; Schwandt, M.L.; Ramchandani, V.A.; George, D.T.; Heilig, M. Impact of multiple types of childhood trauma exposure on risk of psychiatric comorbidity among alcoholic inpatients. Alcohol. Clin. Exp. Res. 2012, 36, 1099–1107. [Google Scholar] [CrossRef]
- Brady, K.T.; Back, S.E. Childhood trauma, posttraumatic stress disorder, and alcohol dependence. Alcohol Res. 2012, 34, 408–413. [Google Scholar]
- Müller, M.; Vandeleur, C.; Rodgers, S.; Rössler, W.; Castelao, E.; Preisig, M.; Ajdacic-Gross, V. Posttraumatic stress avoidance symptoms as mediators in the development of alcohol use disorders after exposure to childhood sexual abuse in a Swiss community sample. Child Abus. Negl. 2015, 46, 8–15. [Google Scholar] [CrossRef]
- Bowlby, J. Attachment: Attachment and Loss Volume One (Basic Books Classics), 2nd ed.; Basic Books: New York, NY, USA, 1983; ISBN 978-0-465-00543-7. [Google Scholar]
- Woodhouse, S.; Ayers, S.; Field, A.P. The relationship between adult attachment style and post-traumatic stress symptoms: A meta-analysis. J. Anxiety Disord. 2015, 35, 103–117. [Google Scholar] [CrossRef]
- Schäfer, I.; Najavits, L.M. Clinical challenges in the treatment of patients with posttraumatic stress disorder and substance abuse. Curr. Opin. Psychiatry 2007, 20, 614–618. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, D.P.; Stein, J.A.; Newcomb, M.D.; Walker, E.; Pogge, D.; Ahluvalia, T.; Stokes, J.; Handelsman, L.; Medrano, M.; Desmond, D.; et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abus. Negl. 2003, 27, 169–190. [Google Scholar] [CrossRef]
- Paquette, D.; Laporte, L.; Bigras, M.; Zoccolillo, M. [Validation of the French version of the CTQ and prevalence of the history of maltreatment]. Sante Ment. Que. 2004, 29, 201–220. [Google Scholar] [CrossRef] [PubMed]
- Spinhoven, P.; Penninx, B.W.; Hickendorff, M.; van Hemert, A.M.; Bernstein, D.P.; Elzinga, B.M. Childhood Trauma Questionnaire: Factor structure, measurement invariance, and validity across emotional disorders. Psychol. Assess. 2014, 26, 717. [Google Scholar] [CrossRef]
- Weathers, F.W.; Blake, D.D.; Schnurr, P.P.; Kaloupek, D.G.; Marx, B.P.; Keane, T.M. The life events checklist for DSM-5 (LEC-5). 2013. Available online: https://www.ptsd.va.gov/professional/assessment/te-measures/life_events_checklist.asp (accessed on 29 June 2020).
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef]
- Ashbaugh, A.R.; Houle-Johnson, S.; Herbert, C.; El-Hage, W.; Brunet, A. Psychometric Validation of the English and French Versions of the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5). PLoS ONE 2016, 11, e0161645. [Google Scholar] [CrossRef]
- Zohar, J.; Amital, D.; Miodownik, C.; Kotler, M.; Bleich, A.; Lane, R.M.; Austin, C. Double-blind placebo-controlled pilot study of sertraline in military veterans with posttraumatic stress disorder. J. Clin. Psychopharmacol. 2002, 22, 190–195. [Google Scholar] [CrossRef]
- Brady, K.; Pearlstein, T.; Asnis, G.M.; Baker, D.; Rothbaum, B.; Sikes, C.R.; Farfel, G.M. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: A randomized controlled trial. JAMA 2000, 283, 1837–1844. [Google Scholar] [CrossRef]
- Dunlop, B.W.; Kaye, J.L.; Youngner, C.; Rothbaum, B. Assessing treatment-resistant posttraumatic stress disorder: The Emory treatment resistance interview for PTSD (E-TRIP). Behav. Sci. 2014, 4, 511–527. [Google Scholar] [CrossRef]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; de la Fuente, J.R.; Grant, M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef]
- Gache, P.; Michaud, P.; Landry, U.; Accietto, C.; Arfaoui, S.; Wenger, O.; Daeppen, J.-B. The Alcohol Use Disorders Identification Test (AUDIT) as a screening tool for excessive drinking in primary care: Reliability and validity of a French version. Alcohol. Clin. Exp. Res. 2005, 29, 2001–2007. [Google Scholar] [CrossRef] [PubMed]
- Dragan, M.; Lis-Turlejska, M. Prevalence of posttraumatic stress disorder in alcohol dependent patients in Poland. Addict. Behav. 2007, 32, 902–911. [Google Scholar] [CrossRef] [PubMed]
- Ozen, S.; Dalbudak, E.; Topcu, M. The Relationship of Posttraumatic Stress Disorder with Childhood Traumas, Personality Characteristics, Depression and Anxiety Symptoms in Patients with Diagnosis of Mixed Anxiety-Depression Disorder. Psychiatr. Danub. 2018, 30, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Etain, B.; Mathieu, F.; Henry, C.; Raust, A.; Roy, I.; Germain, A.; Leboyer, M.; Bellivier, F. Preferential association between childhood emotional abuse and bipolar disorder. J. Trauma. Stress 2010, 23, 376–383. [Google Scholar] [CrossRef]
- Gottschalk, M.G.; Domschke, K. Genetics of generalized anxiety disorder and related traits. Dialogues Clin. Neurosci. 2017, 19, 159–168. [Google Scholar]
- Yrondi, A.; Aouizerate, B.; Bennabi, D.; Richieri, R.; D’Amato, T.; Bellivier, F.; Bougerol, T.; Horn, M.; Camus, V.; Courtet, P.; et al. Childhood maltreatment and clinical severity of treatment-resistant depression in a French cohort of outpatients (FACE-DR): One-year follow-up. Depress. Anxiety 2020, 37, 365–374. [Google Scholar] [CrossRef]
- O’Hare, C.; McCrory, C.; O’Leary, N.; O’Brien, H.; Kenny, R.A. Childhood trauma and lifetime syncope burden among older adults. J. Psychosom. Res. 2017, 97, 63–69. [Google Scholar] [CrossRef]
- Morina, N.; Wicherts, J.M.; Lobbrecht, J.; Priebe, S. Remission from post-traumatic stress disorder in adults: A systematic review and meta-analysis of long term outcome studies. Clin. Psychol. Rev. 2014, 34, 249–255. [Google Scholar] [CrossRef]
- Hingray, C.; Cohn, A.; Martini, H.; Donné, C.; El-Hage, W.; Schwan, R.; Paille, F. Impact of trauma on addiction and psychopathology profile in alcohol-dependent women. Eur. J. Trauma Dissociation 2018, 2, 101–107. [Google Scholar] [CrossRef]
- Walton, J.L.; Raines, A.M.; Cuccurullo, L.-A.J.; Vidaurri, D.N.; Villarosa-Hurlocker, M.C.; Franklin, C.L. The relationship between DSM-5 PTSD symptom clusters and alcohol misuse among military veterans. Am. J. Addict. 2018, 27, 23–28. [Google Scholar] [CrossRef]
- Hruska, B.; Pacella, M.L.; George, R.L.; Delahanty, D.L. The association between daily PTSD symptom severity and alcohol-related outcomes in recent traumatic injury victims. Psychol. Addict. Behav. 2017, 31, 326–335. [Google Scholar] [CrossRef] [PubMed]
- Sannibale, C.; Teesson, M.; Creamer, M.; Sitharthan, T.; Bryant, R.A.; Sutherland, K.; Taylor, K.; Bostock-Matusko, D.; Visser, A.; Peek-O’Leary, M. Randomized controlled trial of cognitive behaviour therapy for comorbid post-traumatic stress disorder and alcohol use disorders. Addiction 2013, 108, 1397–1410. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, I.; Chuey-Ferrer, L.; Hofmann, A.; Lieberman, P.; Mainusch, G.; Lotzin, A. Effectiveness of EMDR in patients with substance use disorder and comorbid PTSD: Study protocol for a randomized controlled trial. BMC Psychiatry 2017, 17, 95. [Google Scholar] [CrossRef] [PubMed]
| Mean ± SD or Percentage (number) | |
|---|---|
| Socio-Demographic Characteristics at T1 | |
| Age (years) | 42.9 ± 8.6 |
| Gender (male) | 82.4% (85) |
| Marital status (married or in a relationship) | 36.3% (33) |
| Alcohol use disorder severity at T1 (AUDIT total score) | 27.8 ± 7.7 |
| PTSD severity at T1 (PCL-5 total score) | 46.4 ± 10.9 |
| Lifetime exposure to a traumatic event (LEC-5) | |
| At least one traumatic event | 100% (91) |
| Natural disaster or/and accident (at least one) | 87.9% (80) |
| Physical or/and sexual aggression (at least one) | 82.4% (75) |
| War-related trauma (at least one) | 6.6% (6) |
| Illness, injury, or death experience (at least one) | 30.8% (28) |
| Any other traumatic event (at least one) | 75.8% (69) |
| Childhood trauma (CTQ sub-scores) | |
| CTQ physical abuse score | 8.3 ± 4.8 |
| CTQ emotional abuse score | 12.9 ± 5.9 |
| CTQ sexual abuse score | 6.8 ± 3.9 |
| CTQ physical negligence score | 8.9 ± 3.7 |
| CTQ emotional negligence score | 12.8 ± 5.0 |
| Non-Remitted PTSD at T2 (n = 23) | Remitted PTSD at T2 (n = 68) | Statistic Test | |
|---|---|---|---|
| Socio-demographic characteristics at T1 | |||
| Age (years) | 40.0 ± 7.9 | 43.7 ± 8.7 | t = −1.83 |
| Gender (male) | 73.9% (17) | 85.3% (58) | χ2 = 1.54 |
| Marital status (married or in a relationship) | 26.1% (6) | 39.7% (27) | χ2 = 1.38 |
| Alcohol use disorder severity at T1 (AUDIT total score) | 27.0 ± 7.3 | 28.0 ± 7.9 | t = −0.56 |
| PTSD severity at T1 (PCL-5 total score) | 43.8 ± 8.8 | 47.3 ± 11.4 | t = 1.34 |
| Lifetime exposure to a traumatic event (LEC-5) | |||
| Natural disaster or/and accident (at least one) | 91.3% (21) | 86.8% (59) | χ2 = 0.33 |
| Physical or/and sexual aggression (at least one) | 78.3% (18) | 83.8% (57) | χ2 = 0.37 |
| War-related trauma (at least one) | 8.6% (2) | 5.9% (4) | χ2 = 0.22 |
| Illness, injury, or death experience (at least one) | 39.1% (9) | 29.4% (20) | χ2 = 0.75 |
| Any other traumatic event (at least one) | 78.3% (18) | 75% (51) | χ2 = 0.10 |
| Childhood trauma (CTQ sub-scores) | |||
| CTQ physical abuse score * | 10.7 ± 6.5 | 7.5 ± 3.8 | t = 2.22 |
| CTQ emotional abuse score * | 15.1 ± 6.2 | 12.1 ± 5.6 | t = 2.16 |
| CTQ sexual abuse score | 8.4 ± 6.1 | 6.2 ± 2.7 | t = 1.64 |
| CTQ physical negligence score | 10.3 ± 3.8 | 8.4 ± 3.2 | t = 1.75 |
| CTQ emotional negligence score | 13.7 ± 6.1 | 12.5 ± 4.6 | t = 0.99 |
| Non-Remitted PTSD | Remitted PTSD | Chi-Squared | p-value | Odds-Ratio | CI 95% | |
|---|---|---|---|---|---|---|
| at T2 (n = 23) | at T2 (n = 68) | |||||
| Socio-demographic characteristics | ||||||
| Gender (male) | 73.9% (17) | 85.3% (58) | 2.05 | 0.15 | 0.42 | 0.13–1.38 |
| Marital status (married or in a relationship) | 26.1% (6) | 39.7% (27) | 1.57 | 0.21 | 0.5 | 0.17–1.47 |
| Alcohol use disorder severity at T1 (AUDIT total score) | 27.0 ± 7.3 | 28.0 ± 7.9 | 0.46 | 0.5 | 1.02 | 0.96–1.09 |
| PTSD severity at T1 (PCL-5 total score) | 43.8 ± 8.8 | 47.3 ± 11.4 | 1.94 | 0.16 | 1.03 | 0.99–1.08 |
| Life events (LEC-5) | ||||||
| Natural disaster or/and accident (at least one) | 91.3% (21) | 86.8% (59) | 0.27 | 0.61 | 0.1.54 | 0.30–7.92 |
| Physical or/and sexual aggression (at least one) | 78.3% (18) | 83.8% (57) | 0.49 | 0.49 | 0.65 | 0.19–2.18 |
| War-related trauma | 8.6% (2) | 5.9% (4) | 1.2 | 0.27 | 2.98 | 0.42–20.99 |
| Illness, injury, or death experience | 39.1% (9) | 29.4% (20) | 1.77 | 0.18 | 2.05 | 0.71–5.91 |
| Any other traumatic event | 78.3% (18) | 75% (51) | 0.13 | 0.72 | 1.24 | 0.23–3.02 |
| Childhood trauma (CTQ sub-scores) | ||||||
| CTQ physical abuse * | 10.7 ± 6.5 | 7.5 ± 3.8 | 7.4 | <0.001 * | 0.8741 | 0.79–0.96 |
| CTQ emotional abuse * | 15.1 ± 6.2 | 12.1 ± 5.6 | 4.8 | 0.03 * | 0.91 | 0.84–0.99 |
| CTQ sexual abuse * | 8.4 ± 6.1 | 6.2 ± 2.7 | 4.8 | 0.03 * | 0.88 | 0.78–0.99 |
| CTQ physical negligence * | 10.3 ± 3.8 | 8.4 ± 3.2 | 4.05 | 0.05 * | 0.88 | 0.78–0.99 |
| CTQ emotional negligence | 13.7 ± 6.1 | 12.5 ± 4.6 | 1.98 | 0.16 | 0.93 | 0.39–3.90 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brunault, P.; Lebigre, K.; Idbrik, F.; Maugé, D.; Adam, P.; Barrault, S.; Baudin, G.; Courtois, R.; El Ayoubi, H.; Grall-Bronnec, M.; et al. Childhood Trauma Predicts Less Remission from PTSD among Patients with Co-Occurring Alcohol Use Disorder and PTSD. J. Clin. Med. 2020, 9, 2054. https://doi.org/10.3390/jcm9072054
Brunault P, Lebigre K, Idbrik F, Maugé D, Adam P, Barrault S, Baudin G, Courtois R, El Ayoubi H, Grall-Bronnec M, et al. Childhood Trauma Predicts Less Remission from PTSD among Patients with Co-Occurring Alcohol Use Disorder and PTSD. Journal of Clinical Medicine. 2020; 9(7):2054. https://doi.org/10.3390/jcm9072054
Chicago/Turabian StyleBrunault, Paul, Kevin Lebigre, Fatima Idbrik, Damien Maugé, Philippe Adam, Servane Barrault, Grégoire Baudin, Robert Courtois, Hussein El Ayoubi, Marie Grall-Bronnec, and et al. 2020. "Childhood Trauma Predicts Less Remission from PTSD among Patients with Co-Occurring Alcohol Use Disorder and PTSD" Journal of Clinical Medicine 9, no. 7: 2054. https://doi.org/10.3390/jcm9072054
APA StyleBrunault, P., Lebigre, K., Idbrik, F., Maugé, D., Adam, P., Barrault, S., Baudin, G., Courtois, R., El Ayoubi, H., Grall-Bronnec, M., Hingray, C., Ballon, N., & El-Hage, W. (2020). Childhood Trauma Predicts Less Remission from PTSD among Patients with Co-Occurring Alcohol Use Disorder and PTSD. Journal of Clinical Medicine, 9(7), 2054. https://doi.org/10.3390/jcm9072054








