Limited Agreement between Classifications of Diabetes and Prediabetes Resulting from the OGTT, Hemoglobin A1c, and Fasting Glucose Tests in 7412 U.S. Adults
Abstract
:1. Introduction
2. Materials & Methods
2.1. Sample
2.2. Methods
2.2.1. Race
2.2.2. Height and Weight
2.2.3. Oral Glucose Tolerance Test and the Fasting Glucose Test
2.2.4. Hemoglobin A1c
2.3. Diabetes Classifications
2.4. Statistical Analysis
3. Results
3.1. Comparing the OGTT and A1c
3.2. Comparing the OGTT and the Fasting Plasma Glucose Test (FPG)
4. Discussion
4.1. Comparing the OGTT and A1c
4.2. Comparing the OGTT and FPG
4.3. Sensitivity and Specificity
4.4. Studies Comparing the FPG, A1c, and OGTT
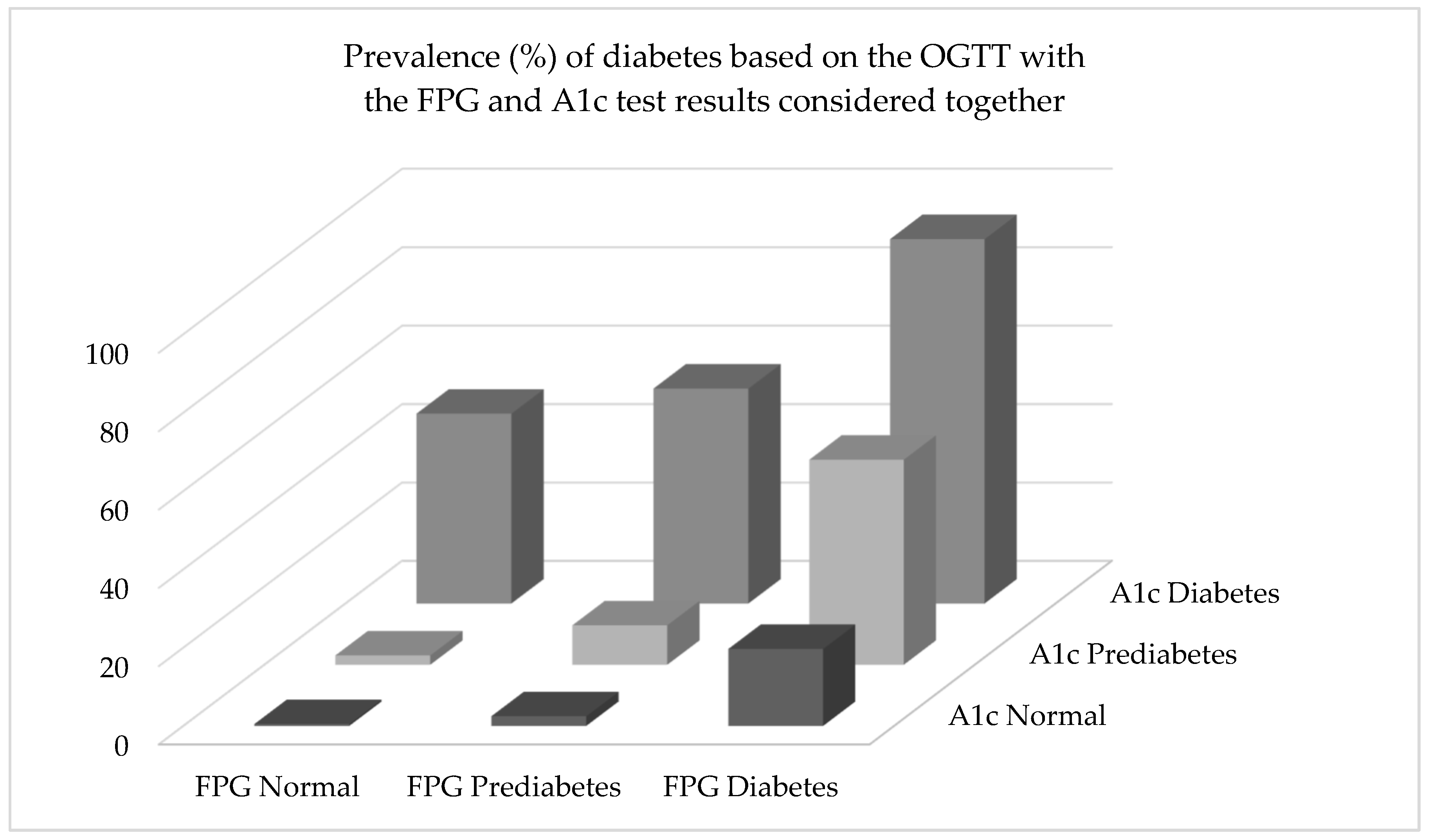
4.5. Predictive Power of the FPG and A1c Tests When Used Together
4.6. Limitations and Strengths
4.7. Future Research
5. Conclusions
Funding
Acknowledgments
Conflicts of Interest
Data Availability
Ethics Statement
References
- International Diabetes Federation. Diabetes Atlas. Available online: www.diabetesatlas.org (accessed on 13 June 2020).
- American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2019. Diabetes Care 2019, 42, S13–S28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meijnikman, A.S.; De Block, C.E.M.; Dirinck, E.; Verrijken, A.; Mertens, I.; Corthouts, B.; Van Gaal, L.F. Not performing an OGTT results in significant underdiagnosis of (pre)diabetes in a high risk adult Caucasian population. Int. J. Obes. (Lond.) 2017, 41, 1615–1620. [Google Scholar] [CrossRef] [PubMed]
- Saukkonen, T.; Cederberg, H.; Jokelainen, J.; Laakso, M.; Harkonen, P.; Keinanen-Kiukaanniemi, S.; Rajala, U. Limited overlap between intermediate hyperglycemia as defined by A1C 5.7–6.4%, impaired fasting glucose, and impaired glucose tolerance. Diabetes Care 2011, 34, 2314–2316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, F.; Moellering, D.R.; Garvey, W.T. Use of HbA1c for diagnoses of diabetes and prediabetes: Comparison with diagnoses based on fasting and 2-h glucose values and effects of gender, race, and age. Metab. Syndr. Relat. Disord. 2014, 12, 258–268. [Google Scholar] [CrossRef] [Green Version]
- Cowie, C.C.; Rust, K.F.; Byrd-Holt, D.D.; Gregg, E.W.; Ford, E.S.; Geiss, L.S.; Bainbridge, K.E.; Fradkin, J.E. Prevalence of diabetes and high risk for diabetes using A1C criteria in the U.S. population in 1988–2006. Diabetes Care 2010, 33, 562–568. [Google Scholar] [CrossRef] [Green Version]
- NCD Risk Factor Collaboration. Effects of diabetes definition on global surveillance of diabetes prevalence and diagnosis: A pooled analysis of 96 population-based studies with 331,288 participants. Lancet Diabetes Endocrinol 2015, 3, 624–637. [Google Scholar] [CrossRef] [Green Version]
- Briker, S.M.; Aduwo, J.Y.; Mugeni, R.; Horlyck-Romanovsky, M.F.; DuBose, C.W.; Mabundo, L.S.; Hormenu, T.; Chung, S.T.; Ha, J.; Sherman, A.; et al. A1C Underperforms as a Diagnostic Test in Africans Even in the Absence of Nutritional Deficiencies, Anemia and Hemoglobinopathies: Insight From the Africans in America Study. Front. Endocrinol. (Lausanne) 2019, 10, 533. [Google Scholar] [CrossRef] [Green Version]
- NHANES. Data Files: Questionnaires, Datasets, and Related Documentation. Available online: https://wwwn.cdc.gov/nchs/nhanes/Default.aspx (accessed on 20 June 2020).
- NHANES. Fasting Questionnaire: Data Documentation, Codebook, and Frequencies. Available online: https://wwwn.cdc.gov/Nchs/Nhanes/2015-2016/FASTQX_I.htm (accessed on 20 June 2020).
- NHANES. National Center of Health Statistics Research Ethics Review Board (ERB) Approval. Available online: http://www.cdc.gov/nchs/nhanes/irba98.htm (accessed on 20 June 2020).
- NHANES. Anthropometry Procedures Manual. Available online: https://wwwn.cdc.gov/nchs/data/nhanes/2015-2016/manuals/2016_Anthropometry_Procedures_Manual.pdf (accessed on 20 June 2020).
- NHANES. NHANES: Data Documentation, Codebook, and Frequencies: Two-Hour Oral Glucose Tolerance Test. Available online: https://wwwn.cdc.gov/Nchs/Nhanes/2015-2016/OGTT_I.htm (accessed on 20 June 2020).
- NHANES. MEC Laboratory Procedures Manual. Available online: https://wwwn.cdc.gov/nchs/data/nhanes/2013-2014/manuals/2013_mec_laboratory_procedures_manual.pdf (accessed on 20 June 2020).
- NHANES. NHANES: Data Documentation, Codebook, and Frequencies: Glycohemoglobin. Available online: https://wwwn.cdc.gov/Nchs/Nhanes/2013-2014/GHB_H.htm (accessed on 20 June 2020).
- Johnson, C.L.; Paulose-Ram, R.; Ogden, C.L.; Carroll, M.D.; Kruszon-Moran, D.; Dohrmann, S.M.; Curtin, L.R. National health and nutrition examination survey: Analytic guidelines, 1999–2010. Vital. Health Stat. 2013, 2, 1–24. [Google Scholar]
- Lu, J.; He, J.; Li, M.; Tang, X.; Hu, R.; Shi, L.; Su, Q.; Peng, K.; Xu, M.; Xu, Y.; et al. Predictive Value of Fasting Glucose, Postload Glucose, and Hemoglobin A1c on Risk of Diabetes and Complications in Chinese Adults. Diabetes Care 2019, 42, 1539–1548. [Google Scholar] [CrossRef]
- Qiao, Q.; Dekker, J.M.; de Vegt, F.; Nijpels, G.; Nissinen, A.; Stehouwer, C.D.; Bouter, L.M.; Heine, R.J.; Tuomilehto, J. Two prospective studies found that elevated 2-h glucose predicted male mortality independent of fasting glucose and HbA1c. J. Clin. Epidemiol. 2004, 57, 590–596. [Google Scholar] [CrossRef] [Green Version]
- Meigs, J.B.; Nathan, D.M.; D’Agostino, R.B., Sr.; Wilson, P.W.; Framingham Offspring, S. Fasting and postchallenge glycemia and cardiovascular disease risk: The Framingham Offspring Study. Diabetes Care 2002, 25, 1845–1850. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lind, M.; Tuomilehto, J.; Uusitupa, M.; Nerman, O.; Eriksson, J.; Ilanne-Parikka, P.; Keinanen-Kiukaanniemi, S.; Peltonen, M.; Pivodic, A.; Lindstrom, J. The association between HbA1c, fasting glucose, 1-hour glucose and 2-hour glucose during an oral glucose tolerance test and cardiovascular disease in individuals with elevated risk for diabetes. PLoS ONE 2014, 9, e109506. [Google Scholar] [CrossRef] [PubMed]
- Shahim, B.; De Bacquer, D.; De Backer, G.; Gyberg, V.; Kotseva, K.; Mellbin, L.; Schnell, O.; Tuomilehto, J.; Wood, D.; Ryden, L. The Prognostic Value of Fasting Plasma Glucose, Two-Hour Postload Glucose, and HbA1c in Patients With Coronary Artery Disease: A Report From EUROASPIRE IV: A Survey From the European Society of Cardiology. Diabetes Care 2017, 40, 1233–1240. [Google Scholar] [CrossRef] [Green Version]
- Phillips, P.J. Oral glucose tolerance testing. Aust. Fam. Physician 2012, 41, 391–393. [Google Scholar] [PubMed]
- Jackson, S.L.; Safo, S.E.; Staimez, L.R.; Olson, D.E.; Narayan, K.M.V.; Long, Q.; Lipscomb, J.; Rhee, M.K.; Wilson, P.W.F.; Tomolo, A.M.; et al. Glucose challenge test screening for prediabetes and early diabetes. Diabet. Med. 2017, 34, 716–724. [Google Scholar] [CrossRef] [Green Version]
- Shapiro, A.J.; Holden, E.C.; McGovern, P.G.; Alderson, D.; Morelli, S.S. Comparison of 2-Hour Oral Glucose Tolerance Test and Hemoglobin A1C in the Identification of Pre-Diabetes in Women with Infertility and Recurrent Pregnancy Loss. Clin. Med. Insights Reprod. Health 2019, 13, 1179558119831280. [Google Scholar] [CrossRef]
- Khan, S.H.; Ijaz, A.; Bokhari, S.A.; Hanif, M.S.; Azam, N. Frequency of impaired glucose tolerance and diabetes mellitus in subjects with fasting blood glucose below 6.1 mmol/L (110 mg/dL). East. Mediterr. Health J. 2013, 19, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Sehrawat, T.; Jindal, A.; Kohli, P.; Thour, A.; Kaur, J.; Sachdev, A.; Gupta, Y. Utility and Limitations of Glycated Hemoglobin (HbA1c) in Patients with Liver Cirrhosis as Compared with Oral Glucose Tolerance Test for Diagnosis of Diabetes. Diabetes Ther. 2018, 9, 243–251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersen, M.; Glintborg, D. Diagnosis and follow-up of type 2 diabetes in women with PCOS: A role for OGTT? Eur. J. Endocrinol. 2018, 179, D1–D14. [Google Scholar] [CrossRef]
- Picon, M.J.; Murri, M.; Munoz, A.; Fernandez-Garcia, J.C.; Gomez-Huelgas, R.; Tinahones, F.J. Hemoglobin A1c versus oral glucose tolerance test in postpartum diabetes screening. Diabetes Care 2012, 35, 1648–1653. [Google Scholar] [CrossRef] [Green Version]
- Rohlfing, C.L.; Wiedmeyer, H.M.; Little, R.R.; England, J.D.; Tennill, A.; Goldstein, D.E. Defining the relationship between plasma glucose and HbA(1c): Analysis of glucose profiles and HbA(1c) in the Diabetes Control and Complications Trial. Diabetes Care 2002, 25, 275–278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nathan, D.M.; Kuenen, J.; Borg, R.; Zheng, H.; Schoenfeld, D.; Heine, R.J.; A1c-Derived Average Glucose (ADAG) Study Group. Translating the A1C assay into estimated average glucose values. Diabetes Care 2008, 31, 1473–1478. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. Use of Glycated Haemoglobin (HbA1c) in the Diagnosis of Diabetes Mellitus: Abbreviated Report of a WHO Consultation; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 2009, 32, 1327–1334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gallagher, E.J.; Le Roith, D.; Bloomgarden, Z. Review of hemoglobin A(1c) in the management of diabetes. J. Diabetes 2009, 1, 9–17. [Google Scholar] [CrossRef]
- Gould, B.J.; Davie, S.J.; Yudkin, J.S. Investigation of the mechanism underlying the variability of glycated haemoglobin in non-diabetic subjects not related to glycaemia. Clin. Chim. Acta 1997, 260, 49–64. [Google Scholar] [CrossRef]
- Snieder, H.; Sawtell, P.A.; Ross, L.; Walker, J.; Spector, T.D.; Leslie, R.D. HbA(1c) levels are genetically determined even in type 1 diabetes: Evidence from healthy and diabetic twins. Diabetes 2001, 50, 2858–2863. [Google Scholar] [CrossRef] [Green Version]
- Cohen, R.M.; Snieder, H.; Lindsell, C.J.; Beyan, H.; Hawa, M.I.; Blinko, S.; Edwards, R.; Spector, T.D.; Leslie, R.D. Evidence for independent heritability of the glycation gap (glycosylation gap) fraction of HbA1c in nondiabetic twins. Diabetes Care 2006, 29, 1739–1743. [Google Scholar] [CrossRef] [Green Version]
- Cohen, R.M.; Franco, R.S.; Khera, P.K.; Smith, E.P.; Lindsell, C.J.; Ciraolo, P.J.; Palascak, M.B.; Joiner, C.H. Red cell life span heterogeneity in hematologically normal people is sufficient to alter HbA1c. Blood 2008, 112, 4284–4291. [Google Scholar] [CrossRef] [Green Version]
- Chalew, S.A.; McCarter, R.J.; Thomas, J.; Thomson, J.L.; Hempe, J.M. A comparison of the Glycosylation Gap and Hemoglobin Glycation Index in patients with diabetes. J. Diabetes Complicat. 2005, 19, 218–222. [Google Scholar] [CrossRef]
- Colagiuri, S.; Lee, C.M.; Wong, T.Y.; Balkau, B.; Shaw, J.E.; Borch-Johnsen, K.; Group, D.-C.W. Glycemic thresholds for diabetes-specific retinopathy: Implications for diagnostic criteria for diabetes. Diabetes Care 2011, 34, 145–150. [Google Scholar] [CrossRef] [Green Version]
- Mancini, G.B.J.; Maron, D.J.; Hartigan, P.M.; Spertus, J.A.; Kostuk, W.J.; Berman, D.S.; Teo, K.K.; Weintraub, W.S.; Boden, W.E.; COURAGE Trial Research Group. Lifestyle, Glycosylated Hemoglobin A1c, and Survival Among Patients With Stable Ischemic Heart Disease and Diabetes. J. Am. Coll. Cardiol. 2019, 73, 2049–2058. [Google Scholar] [CrossRef]
- Mo, Y.; Zhou, J.; Ma, X.; Zhu, W.; Zhang, L.; Li, J.; Lu, J.; Hu, C.; Bao, Y.; Jia, W. Haemoglobin A1c variability as an independent correlate of atherosclerosis and cardiovascular disease in Chinese type 2 diabetes. Diabete Vasc. Dis. Res. 2018, 15, 402–408. [Google Scholar] [CrossRef] [Green Version]
- Selvin, E.; Steffes, M.W.; Zhu, H.; Matsushita, K.; Wagenknecht, L.; Pankow, J.; Coresh, J.; Brancati, F.L. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N. Engl. J. Med. 2010, 362, 800–811. [Google Scholar] [CrossRef] [PubMed]
- Nathan, D.M.; McGee, P.; Steffes, M.W.; Lachin, J.M.; COURAGE Trial Research Group. Relationship of glycated albumin to blood glucose and HbA1c values and to retinopathy, nephropathy, and cardiovascular outcomes in the DCCT/EDIC study. Diabetes 2014, 63, 282–290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Forrest, K.Y.; Becker, D.J.; Kuller, L.H.; Wolfson, S.K.; Orchard, T.J. Are predictors of coronary heart disease and lower-extremity arterial disease in type 1 diabetes the same? A prospective study. Atherosclerosis 2000, 148, 159–169. [Google Scholar] [CrossRef]
- Pruzin, J.J.; Schneider, J.A.; Capuano, A.W.; Leurgans, S.E.; Barnes, L.L.; Ahima, R.S.; Arnold, S.E.; Bennett, D.A.; Arvanitakis, Z. Diabetes, Hemoglobin A1C, and Regional Alzheimer Disease and Infarct Pathology. Alzheimer Dis. Assoc. Disord. 2017, 31, 41–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orchard, T.J.; Olson, J.C.; Erbey, J.R.; Williams, K.; Forrest, K.Y.; Smithline Kinder, L.; Ellis, D.; Becker, D.J. Insulin resistance-related factors, but not glycemia, predict coronary artery disease in type 1 diabetes: 10-year follow-up data from the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes Care 2003, 26, 1374–1379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koivisto, V.A.; Stevens, L.K.; Mattock, M.; Ebeling, P.; Muggeo, M.; Stephenson, J.; Idzior-Walus, B. Cardiovascular disease and its risk factors in IDDM in Europe. EURODIAB IDDM Complications Study Group. Diabetes Care 1996, 19, 689–697. [Google Scholar] [CrossRef]
- Rao Kondapally Seshasai, S.; Kaptoge, S.; Thompson, A.; Di Angelantonio, E.; Gao, P.; Sarwar, N.; Whincup, P.H.; Mukamal, K.J.; Gillum, R.F.; Holme, I.; et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N. Engl. J. Med. 2011, 364, 829–841. [Google Scholar] [PubMed] [Green Version]
- Emerging Risk Factors, C.; Sarwar, N.; Gao, P.; Seshasai, S.R.; Gobin, R.; Kaptoge, S.; Di Angelantonio, E.; Ingelsson, E.; Lawlor, D.A.; Selvin, E.; et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: A collaborative meta-analysis of 102 prospective studies. Lancet 2010, 375, 2215–2222. [Google Scholar] [CrossRef] [Green Version]
- Park, C.; Guallar, E.; Linton, J.A.; Lee, D.C.; Jang, Y.; Son, D.K.; Han, E.J.; Baek, S.J.; Yun, Y.D.; Jee, S.H.; et al. Fasting glucose level and the risk of incident atherosclerotic cardiovascular diseases. Diabetes Care 2013, 36, 1988–1993. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Selvin, E.; Wang, D.; Matsushita, K.; Grams, M.E.; Coresh, J. Prognostic Implications of Single-Sample Confirmatory Testing for Undiagnosed Diabetes: A Prospective Cohort Study. Ann. Intern. Med. 2018, 169, 156–164. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2014, 37 (Suppl. 1), S81–S90. [Google Scholar]
| Variable | Percentile (±SE) | ||||
|---|---|---|---|---|---|
| 5th | 25th | 50th | 75th | 95th | |
| 2 h OGTT | |||||
| Women (mg/dL) | 68.0 ± 1.3 | 87.8 ± 0.6 | 105.1 ± 0.8 | 131.6 ± 1.2 | 203.0 ± 2.9 |
| Women (mmol/L) | 3.77 ± 0.07 | 4.87 ± 0.03 | 5.83 ± 0.04 | 7.30 ± 0.07 | 11.27 ± 0.16 |
| Men (mg/dL) | 58.6 ± 1.3 | 84.7 ± 0.7 | 103.1 ± 0.9 | 129.0 ± 1.1 | 198.0 ± 4.8 |
| Men (mmol/L) | 3.25 ± 0.07 | 4.70 ± 0.04 | 5.72 ± 0.05 | 7.16 ± 0.06 | 11.0 ± 0.27 |
| Combined (mg/dL) | 62.4 ± 1.0 | 86.1 ± 0.6 | 104.3 ± 0.6 | 130.4 ± 0.8 | 201.0 ± 2.7 |
| Combined (mmol/L) | 3.46 ± 0.06 | 4.78 ± 0.03 | 5.79 ± 0.03 | 7.24 ± 0.04 | 11.2 ± 0.15 |
| A1c | |||||
| Women (%) | 4.8 ± 0.02 | 5.1 ± 0.01 | 5.4 ± 0.01 | 5.6 ± 0.01 | 6.1 ± 0.02 |
| Women (mmol/mol) | 29 ± 0.12 | 32 ± 0.06 | 36 ± 0.07 | 38 ± 0.07 | 43 ± 0.14 |
| Men (%) | 4.7 ± 0.02 | 5.1 ± 0.01 | 5.4 ± 0.01 | 5.6 ± 0.01 | 6.1 ± 0.04 |
| Men (mmol/mol) | 28 ± 0.12 | 32 ± 0.06 | 36 ± 0.07 | 38 ± 0.07 | 43 ± 0.29 |
| Combined (%) | 4.8 ± 0.01 | 5.1 ± 0.01 | 5.4 ± 0.01 | 5.6 ± 0.01 | 6.1 ± 0.02 |
| Combined (mmol/mol) | 29 ± 0.06 | 32 ± 0.06 | 36 ± 0.07 | 38 ± 0.07 | 43 ± 0.14 |
| Fasting Plasma Glucose | |||||
| Women (mg/dL) | 81.7 ± 0.3 | 89.6 ± 0.2 | 95.4 ± 0.3 | 102.7 ± 0.4 | 118.8 ± 1.0 |
| Women (mmol/L) | 4.53 ± 0.02 | 4.97 ± 0.01 | 5.29 ± 0.02 | 5.70 ± 0.02 | 6.59 ± 0.06 |
| Men (mg/dL) | 85.6 ± 0.6 | 93.6 ± 0.3 | 99.6 ± 0.3 | 106.8 ± 0.4 | 124.0 ± 1.0 |
| Men (mmol/L) | 4.75 ± 0.03 | 5.19 ± 0.02 | 5.53 ± 0.02 | 5.93 ± 0.02 | 6.88 ± 0.06 |
| Combined (mg/dL) | 82.8 ± 0.3 | 91.4 ± 0.2 | 97.6 ± 0.2 | 104.9 ± 0.3 | 121.1 ± 0.8 |
| Combined (mmol/L) | 4.60 ± 0.02 | 5.07 ± 0.01 | 5.42 ± 0.01 | 5.82 ± 0.02 | 6.72 ± 0.04 |
| Age (years) | |||||
| Women | 21.5 ± 0.3 | 31.6 ± 0.5 | 46.1 ± 0.6 | 59.3 ± 0.4 | 77.3 ± 0.7 |
| Men | 21.3 ± 0.2 | 30.9 ± 0.4 | 43.2 ± 0.7 | 57.3 ± 0.6 | 74.2 ± 0.6 |
| Combined | 21.4 ± 0.8 | 31.2 ± 0.4 | 44.6 ± 0.6 | 58.4 ± 0.2 | 76.0 ± 0.5 |
| Body weight (kg) | |||||
| Women | 50.3 ± 0.4 | 61.7 ± 0.4 | 71.9 ± 0.5 | 86.3 ± 0.8 | 115.6 ± 1.7 |
| Men | 61.6 ± 0.5 | 74.6 ± 0.5 | 85.8 ± 0.7 | 99.5 ± 0.8 | 125.1 ± 1.6 |
| Combined | 53.4 ± 0.4 | 66.7 ± 0.3 | 79.1 ± 0.4 | 93.8 ± 0.5 | 121.7 ± 1.1 |
| OGTT Classification | A1c Classification | ||
|---|---|---|---|
| All Subjects | A1c: Normal | A1c: Prediabetes | A1c: Diabetes |
| OGTT: Normal | n = 4295 | n = 1370 | n = 13 |
| n = 5678 | row %: 80.7 | row %: 19.2 | row %: 0.1 |
| OGTT: Prediabetes | n = 581 | n = 599 | n = 41 |
| n = 1221 | row %: 51.8 | row %: 46.1 | row %: 2.1 |
| OGTT: Diabetes | n = 83 | n = 244 | n = 186 |
| n = 513 | row %: 18.6 | row %: 47.3 | row %: 34.1 |
| Column: n = 7412 | Column: n = 4959 | Column: n = 2213 | Column: n = 240 |
| Women Only | A1c: Normal | A1c: Prediabetes | A1c: Diabetes |
| OGTT: Normal | n = 2231 | n = 686 | n = 5 |
| n = 2922 | row %: 80.4 | row %: 19.5 | row %: 0.1 |
| OGTT: Prediabetes | n = 298 | n = 306 | n = 21 |
| n = 625 | row %: 51.1 | row %: 46.4 | row %: 2.5 |
| OGTT: Diabetes | n = 47 | n = 129 | n = 86 |
| n = 262 | row %: 20.9 | row %: 49.5 | row %: 29.5 |
| Column: n = 3809 | Column: n = 2576 | Column: n = 1121 | Column: n = 112 |
| Men Only | A1c: Normal | A1c: Prediabetes | A1c: Diabetes |
| OGTT: Normal | n = 2064 | n = 684 | n = 8 |
| n = 2756 | row %: 81.1 | row %: 18.8 | row %: 0.1 |
| OGTT: Prediabetes | n = 283 | n = 293 | n = 20 |
| n = 596 | row %: 52.6 | row %: 45.7 | row %: 1.7 |
| OGTT: Diabetes | n = 36 | n = 115 | n = 100 |
| n = 251 | row %: 15.6 | row %: 44.6 | row %: 39.8 |
| Column: n = 3603 | Column: n = 2383 | Column: n = 1092 | Column: n = 128 |
| OGTT Classification | A1c Classification | ||
|---|---|---|---|
| Young Adults | A1c: Normal | A1c: Prediabetes | A1c: Diabetes |
| OGTT: Normal | n = 2117 | n = 282 | n = 1 |
| n = 2400 | row %: 90.3 | row %: 9.7 | row %: 0.0 |
| OGTT: Prediabetes | n = 150 | n = 60 | n = 3 |
| n = 569 | row %: 72.9 | row %: 26.1 | row %: 1.0 |
| OGTT: Diabetes | n = 9 | n = 16 | n = 31 |
| n = 292 | row %: 19.5 | row %: 34.1 | row %: 46.4 |
| Column: n = 2669 | Column: n = 2276 | Column: n = 358 | Column: n = 35 |
| Middle-age Adults | A1c: Normal | A1c: Prediabetes | A1c: Diabetes |
| OGTT: Normal | n = 1441 | n = 566 | n = 6 |
| n = 2013 | row %: 77.8 | row %: 22.1 | row %: 0.2 |
| OGTT: Prediabetes | n = 204 | n = 220 | n = 15 |
| n = 439 | row %: 52.1 | row %: 45.9 | row %: 2.0 |
| OGTT: Diabetes | n = 30 | n = 57 | n = 78 |
| n = 165 | row %: 22.5 | row %: 35.4 | row %: 42.1 |
| Column: n = 2617 | Column: n = 1675 | Column: n = 843 | Column: n = 99 |
| Older Adults | A1c: Normal | A1c: Prediabetes | A1c: Diabetes |
| OGTT: Normal | n = 737 | n = 522 | n = 6 |
| n = 1265 | row %: 64.0 | row %: 35.9 | row %: 0.2 |
| OGTT: Prediabetes | n = 227 | n = 319 | n = 23 |
| n = 569 | row %: 41.3 | row %: 55.8 | row %: 2.8 |
| OGTT: Diabetes | n = 44 | n = 171 | n = 77 |
| n = 292 | row %: 15.5 | row %: 59.2 | row %: 25.2 |
| Column: n = 2126 | Column: n = 1008 | Column: n = 1012 | Column: n = 106 |
| OGTT Classification | Fasting Plasma Glucose Classification | ||
|---|---|---|---|
| All Subjects | FPG: Normal | FPG: Prediabetes | FPG: Diabetes |
| OGTT: Normal | n = 3595 | n = 2043 | n = 40 |
| n = 5678 | row %: 64.8 | row %: 34.7 | row %: 0.5 |
| OGTT: Prediabetes | n = 381 | n = 758 | n = 82 |
| n = 1221 | row %: 30.9 | row %: 63.4 | row %: 5.8 |
| OGTT: Diabetes | n = 37 | n = 248 | n = 228 |
| n = 513 | row %: 8.9 | row %: 46.8 | row %: 44.3 |
| Column: n = 7412 | Column: n = 4013 | Column: n = 3049 | Column: n = 350 |
| Women Only | FPG: Normal | FPG: Prediabetes | FPG: Diabetes |
| OGTT: Normal | n = 2130 | n = 781 | n = 11 |
| n = 2922 | row: 73.4% | row: 26.3% | row: 0.3% |
| OGTT: Prediabetes | n = 232 | n = 360 | n = 33 |
| n = 625 | row: 36.8% | row: 59.2% | row: 4.0% |
| OGTT: Diabetes | n = 30 | n = 143 | n = 89 |
| n = 262 | row: 13.5% | row: 52.8% | row: 33.7% |
| Column: n = 3809 | Column: n = 2392 | Column: n = 1284 | Column: n = 133 |
| Men Only | FPG: Normal | FPG: Prediabetes | FPG: Diabetes |
| OGTT: Normal | n = 1465 | n = 1262 | n = 29 |
| n = 2756 | row: 55.3% | row: 43.8% | row: 0.8% |
| OGTT: Prediabetes | n = 149 | n = 398 | n = 49 |
| n = 596 | row: 24.3% | row: 68.0% | row: 7.7% |
| OGTT: Diabetes | n = 7 | n = 105 | n = 139 |
| n = 251 | row: 3.0% | row: 39.0% | row: 57.9% |
| Column: n = 3603 | Column: n = 1621 | Column: n = 1765 | Column: n = 217 |
| OGTT Classification | Fasting Plasma Glucose Classification | ||
|---|---|---|---|
| Young Adults | FPG: Normal | FPG: Prediabetes | FPG: Diabetes |
| OGTT: Normal | n = 1760 | n = 632 | n = 8 |
| n = 2400 | row %: 73.8 | row %: 26.0 | row %: 0.2 |
| OGTT: Prediabetes | n = 93 | n = 112 | n = 8 |
| n = 213 | row %: 43.8 | row %: 52.4 | row %: 3.8 |
| OGTT: Diabetes | n = 6 | n = 16 | n = 34 |
| n = 56 | row %: 14.6 | row %: 31.4 | row %: 54.0 |
| Column: n = 2669 | Column: n = 1859 | Column: n = 760 | Column: n = 50 |
| Middle-age Adults | FPG: Normal | FPG: Prediabetes | FPG: Diabetes |
| OGTT: Normal | n = 1186 | n = 808 | n = 19 |
| n = 2013 | row %: 60.4 | row %: 38.8 | row %: 0.8 |
| OGTT: Prediabetes | n = 146 | n = 260 | n = 33 |
| n = 439 | row %: 31.3 | row %: 62.6 | row %: 6.1 |
| OGTT: Diabetes | n = 9 | n = 64 | n = 92 |
| n = 165 | row %: 8.0 | row %: 35.9 | row %: 56.1 |
| Column: n = 2617 | Column: n = 1341 | Column: n = 1132 | Column: n = 144 |
| Older Adults | FPG: Normal | FPG: Prediabetes | FPG: Diabetes |
| OGTT: Normal | n = 649 | n = 603 | n = 13 |
| n = 1265 | row %: 51.9 | row %: 47.2 | row %: 0.9 |
| OGTT: Prediabetes | n = 142 | n = 386 | n = 41 |
| n = 569 | row %: 24.2 | row %: 69.5 | row %: 6.3 |
| OGTT: Diabetes | n = 22 | n = 168 | n = 102 |
| n = 292 | row %: 8.2 | row %: 58.4 | row %: 33.5 |
| Column: n = 2126 | Column: n = 813 | Column: n = 1157 | Column: n = 156 |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tucker, L.A. Limited Agreement between Classifications of Diabetes and Prediabetes Resulting from the OGTT, Hemoglobin A1c, and Fasting Glucose Tests in 7412 U.S. Adults. J. Clin. Med. 2020, 9, 2207. https://doi.org/10.3390/jcm9072207
Tucker LA. Limited Agreement between Classifications of Diabetes and Prediabetes Resulting from the OGTT, Hemoglobin A1c, and Fasting Glucose Tests in 7412 U.S. Adults. Journal of Clinical Medicine. 2020; 9(7):2207. https://doi.org/10.3390/jcm9072207
Chicago/Turabian StyleTucker, Larry A. 2020. "Limited Agreement between Classifications of Diabetes and Prediabetes Resulting from the OGTT, Hemoglobin A1c, and Fasting Glucose Tests in 7412 U.S. Adults" Journal of Clinical Medicine 9, no. 7: 2207. https://doi.org/10.3390/jcm9072207
APA StyleTucker, L. A. (2020). Limited Agreement between Classifications of Diabetes and Prediabetes Resulting from the OGTT, Hemoglobin A1c, and Fasting Glucose Tests in 7412 U.S. Adults. Journal of Clinical Medicine, 9(7), 2207. https://doi.org/10.3390/jcm9072207





