The Use of Bovine Xenogeneic Bone Graft for Dega Pelvic Osteotomy in Children with Hip Dysplasia: A Retrospective Study of 147 Treated Hips
Abstract
:1. Introduction
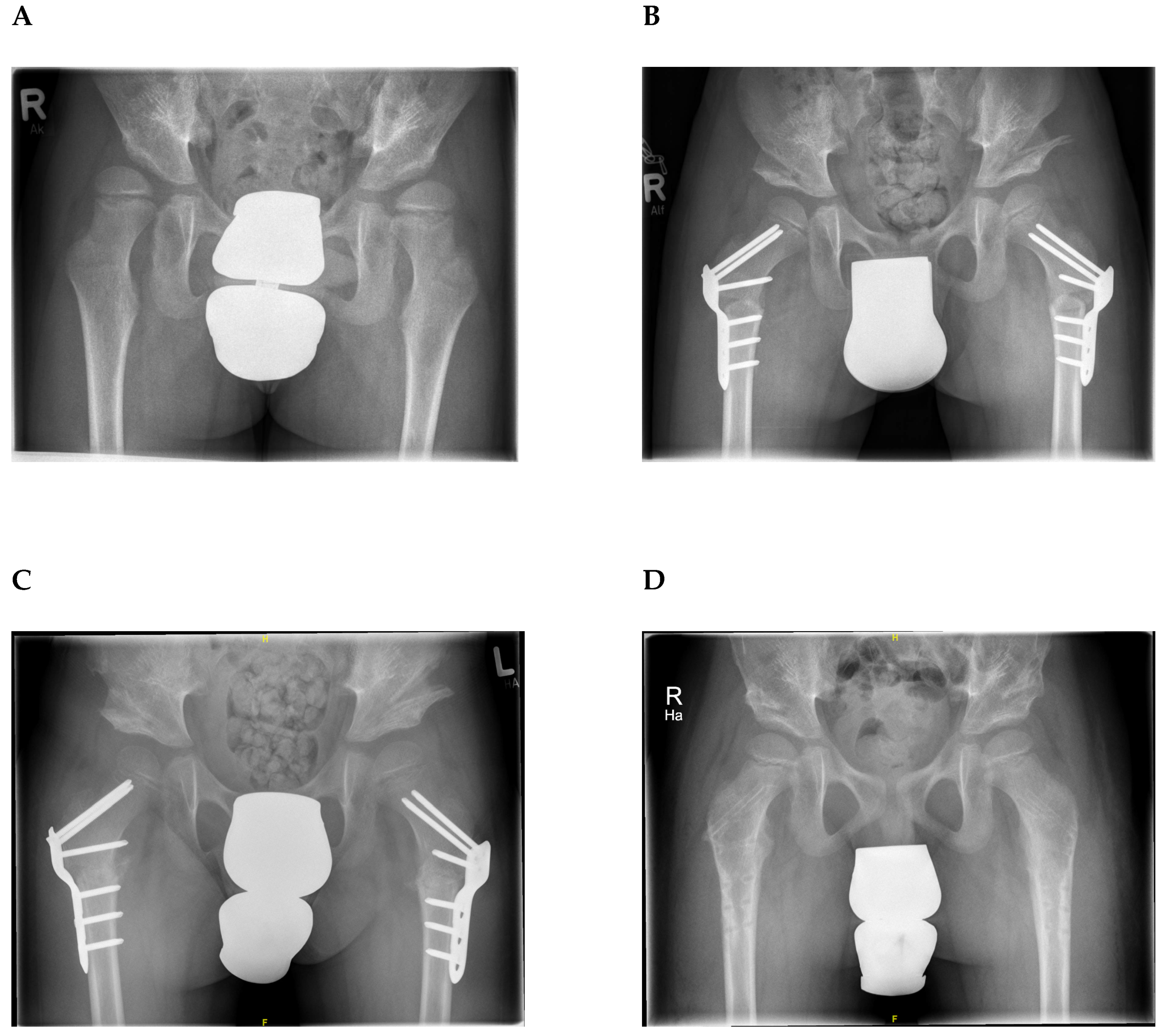
2. Materials and Methods
2.1. Bovine Xenogeneic Bone Graft
2.2. Patients
2.3. Surgical Procedure and Perioperative Care
2.4. Radiological Assessment
2.5. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Ethics Approval
References
- Thomas, S.R. A review of long-term outcomes for late presenting developmental hip dysplasia. Bone Jt. J. 2015, 97, 729–733. [Google Scholar] [CrossRef] [PubMed]
- Gala, L.; Clohisy, J.C.; Beaule, P.E. Hip dysplasia in the young adult. J. Bone Jt. Surg. Am. Vol. 2016, 98, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Czubak, J.; Kowalik, K.; Kawalec, A.; Kwiatkowska, M. Dega pelvic osteotomy: Indications, results and complications. J. Child. Orthop. 2018, 12, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Wade, W.J.; Alhussainan, T.S.; Al Zayed, Z.; Hamdi, N.; Bubshait, D. Contoured iliac crest allograft interposition for pericapsular acetabuloplasty in developmental dislocation of the hip: Technique and short-term results. J. Child. Orthop. 2010, 4, 429–438. [Google Scholar] [CrossRef] [Green Version]
- Moon, S.Y.; Kwon, S.S.; Cho, B.C.; Chung, C.Y.; Lee, K.M.; Sung, K.H.; Chung, M.K.; Zulkarnain, A.; Kim, Y.S.; Park, M.S. Osteopenic features of the hip joint in patients with cerebral palsy: A hospital-based study. Dev. Med. Child Neurol. 2016, 58, 1153–1158. [Google Scholar] [CrossRef] [Green Version]
- Rossillon, R.; Desmette, D.; Rombouts, J.J. Growth disturbance of the ilium after splitting the iliac apophysis and iliac crest bone harvesting in children: A retrospective study at the end of growth following unilateral salter innominate osteotomy in 21 children. Acta Orthop. Belg. 1999, 65, 295–301. [Google Scholar] [PubMed]
- Goulet, J.A.; Senunas, L.E.; DeSilva, G.L.; Greenfield, M.L. Autogenous iliac crest bone graft. Complications and functional assessment. Clin. Orthop. Relat. Res. 1997, 339, 76–81. [Google Scholar] [CrossRef] [Green Version]
- Silber, J.S.; Anderson, D.G.; Daffner, S.D.; Brislin, B.T.; Leland, J.M.; Hilibrand, A.S.; Vaccaro, A.R.; Albert, T.J. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine 2003, 28, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Murata, Y.; Takahashi, K.; Yamagata, M.; Sameda, H.; Moriya, H. Injury to the lateral femoral cutaneous nerve during harvest of iliac bone graft, with reference to the size of the graft. J. Bone Jt. Surg. Br. Vol. 2002, 84, 798–801. [Google Scholar] [CrossRef]
- Velchuru, V.R.; Satish, S.G.; Petri, G.J.; Sturzaker, H.G. Hernia through an iliac crest bone graft site: Report of a case and review of the literature. Bulletin 2006, 63, 166–168. [Google Scholar]
- Ibrahim, M.M.; El-Lakkany, M.R.; Wahba, M.M.; El-Ganainy, A.A.; Aly, A.M. Combined open reduction and dega transiliac osteotomy for developmental dysplasia of the hip in walking children. Acta Orthop. Belg. 2019, 85, 545–553. [Google Scholar] [PubMed]
- Stangenberg, L.; Schaefer, D.J.; Buettner, O.; Ohnolz, J.; Mobest, D.; Horch, R.E.; Stark, G.B.; Kneser, U. Differentiation of osteoblasts in three-dimensional culture in processed cancellous bone matrix: Quantitative analysis of gene expression based on real-time reverse transcription-polymerase chain reaction. Tissue Eng. 2005, 11, 855–864. [Google Scholar] [CrossRef] [PubMed]
- Meyer, S.; Floerkemeier, T.; Windhagen, H. Histological osseointegration of tutobone: First results in human. Arch. Orthop. Trauma Surg. 2008, 128, 539–544. [Google Scholar] [CrossRef] [PubMed]
- Merckaert, S.R.; Pierzchala, K.; Bregou, A.; Zambelli, P.Y. Residual hip dysplasia in children: Osseous and cartilaginous acetabular angles to guide further treatment-a pilot study. J. Orthop. Surg. Res. 2019, 14, 379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tonnis, D.; Brunken, D. Differentiation of normal and pathological acetabular roof angle in the diagnosis of hip dysplasia. Evaluation of 2294 acetabular roof angles of hip joints in children. Arch. Orthop. Unf. Chir. 1968, 64, 197–228. [Google Scholar]
- Tönnis, D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin. Orthop. Relat. Res. 1976, 119, 39–47. [Google Scholar]
- Wiberg, G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. With special reference to the complication of osteo-arthritis. Acta Chir. Scand. 1939, 83, 1–135. [Google Scholar]
- Omeroglu, H.; Bicimoglu, A.; Agus, H.; Tumer, Y. Measurement of center-edge angle in developmental dysplasia of the hip: A comparison of two methods in patients under 20 years of age. Skelet. Radiol. 2002, 31, 25–29. [Google Scholar] [CrossRef]
- Goldberg, V.M.; Powell, A.; Shaffer, J.W.; Zika, J.; Bos, G.D.; Heiple, K.G. Bone grafting: Role of histocompatibility in transplantation. J. Orthop. Res. 1985, 3, 389–404. [Google Scholar] [CrossRef] [PubMed]
- Sung, K.H.; Kwon, S.S.; Chung, C.Y.; Lee, K.M.; Kim, J.; Park, M.S. Use of iliac crest allograft for dega pelvic osteotomy in patients with cerebral palsy. BMC Musculoskelet. Disord. 2018, 19, 375. [Google Scholar] [CrossRef]
- Patil, S.; Auyeung, J.; Gower, A. Outcome of subtalar fusion using bovine cancellous bone graft: A retrospective case series. J. Foot Ankle Surg. 2011, 50, 388–390. [Google Scholar] [CrossRef] [PubMed]
- Makridis, K.G.; Ahmad, M.A.; Kanakaris, N.K.; Fragkakis, E.M.; Giannoudis, P.V. Reconstruction of iliac crest with bovine cancellous allograft after bone graft harvest for symphysis pubis arthrodesis. Int. Orthop. 2012, 36, 1701–1707. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bauer, T.W.; Muschler, G.F. Bone graft materials. An overview of the basic science. Clin. Orthop. Relat. Res. 2000, 371, 10–27. [Google Scholar] [CrossRef]
- Cypher, T.J.; Grossman, J.P. Biological principles of bone graft healing. J. Foot Ankle Surg. 1996, 35, 413–417. [Google Scholar] [CrossRef]
- El-Sayed, M.M.; Hegazy, M.; Abdelatif, N.M.; ElGebeily, M.A.; ElSobky, T.; Nader, S. Dega osteotomy for the management of developmental dysplasia of the hip in children aged 2–8 years: Results of 58 consecutive osteotomies after 13–25 years of follow-up. J. Child. Orthop. 2015, 9, 191–198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Houlihan, C.M.; Stevenson, R.D. Bone density in cerebral palsy. Phys. Med. Rehabil. Clin. N. Am. 2009, 20, 493–508. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| 1. Graft appearance | |
| Resorbed | 0 |
| Mostly resorbed | 1 |
| Largely intact | 2 |
| Reorganizing | 3 |
| 2. Bony union (proximal) | |
| Non-union | 0 |
| Possible union | 1 |
| Radiographic union | 2 |
| 3. Bony union (distal) | |
| Non-union | 0 |
| Possible union | 1 |
| Radiographic union | 2 |
| Acetabular Angle | Lateral Centre-Edge-Angle | ||||||
|---|---|---|---|---|---|---|---|
| Right | Left | Both | Right | Left | Both | ||
| Preoperative | Mean ± SD | 27.2 ± 5.4 | 28.9 ± 7.6 | 28.1 ± 6.7 | 11.2 ± 6.8 | 8.6 ± 6.4 | 9.9 ± 6.7 |
| Postoperative (1 week) | Mean ± SD | 14.0 ± 5.3 | 15.4 ± 4.9 | 14.7 ± 5.1 | 22.9 ± 7.0 | 20.4 ± 6.4 | 21.8 ± 6.8 |
| Postoperative (6 weeks) | Mean ± SD | 14.5 ± 5.5 | 15.4 ± 4.9 | 14.9 ± 5.2 | 22.2 ± 6.6 | 21.3 ± 6.2 | 21.8 ± 6.4 |
| Postoperative (1 year) | Mean ± SD | 14.8 ± 5.9 | 15.6 ± 5.6 | 15.2 ± 5.8 | 21.1 ± 6.7 | 20.5 ± 7.3 | 20.8 ± 6.9 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stiel, N.; Moritz, M.; Babin, K.; Suling, A.; Rupprecht, M.; Beil, F.T.; Stuecker, R.; Spiro, A.S. The Use of Bovine Xenogeneic Bone Graft for Dega Pelvic Osteotomy in Children with Hip Dysplasia: A Retrospective Study of 147 Treated Hips. J. Clin. Med. 2020, 9, 2241. https://doi.org/10.3390/jcm9072241
Stiel N, Moritz M, Babin K, Suling A, Rupprecht M, Beil FT, Stuecker R, Spiro AS. The Use of Bovine Xenogeneic Bone Graft for Dega Pelvic Osteotomy in Children with Hip Dysplasia: A Retrospective Study of 147 Treated Hips. Journal of Clinical Medicine. 2020; 9(7):2241. https://doi.org/10.3390/jcm9072241
Chicago/Turabian StyleStiel, Norbert, Menard Moritz, Kornelia Babin, Anna Suling, Martin Rupprecht, Frank T. Beil, Ralf Stuecker, and Alexander S. Spiro. 2020. "The Use of Bovine Xenogeneic Bone Graft for Dega Pelvic Osteotomy in Children with Hip Dysplasia: A Retrospective Study of 147 Treated Hips" Journal of Clinical Medicine 9, no. 7: 2241. https://doi.org/10.3390/jcm9072241




