Volume of Lateral Geniculate Nucleus in Patients with Glaucoma in 7Tesla MRI
Abstract
1. Introduction
2. Material and Methods
- -
- Open angle glaucoma diagnosed according to the criteria mentioned above,
- -
- Bilaterally the same glaucoma stage. Glaucoma staging was evaluated according to Hodapp–Parish–Anderson classification of visual field loss. Subjects with mean deviation (MD) in each eye better than −6 dB were classified as the early glaucoma group (11 patients) and subjects with MD in each eye worse than −12 dB patients were classified as the advanced glaucoma group (9 patients).
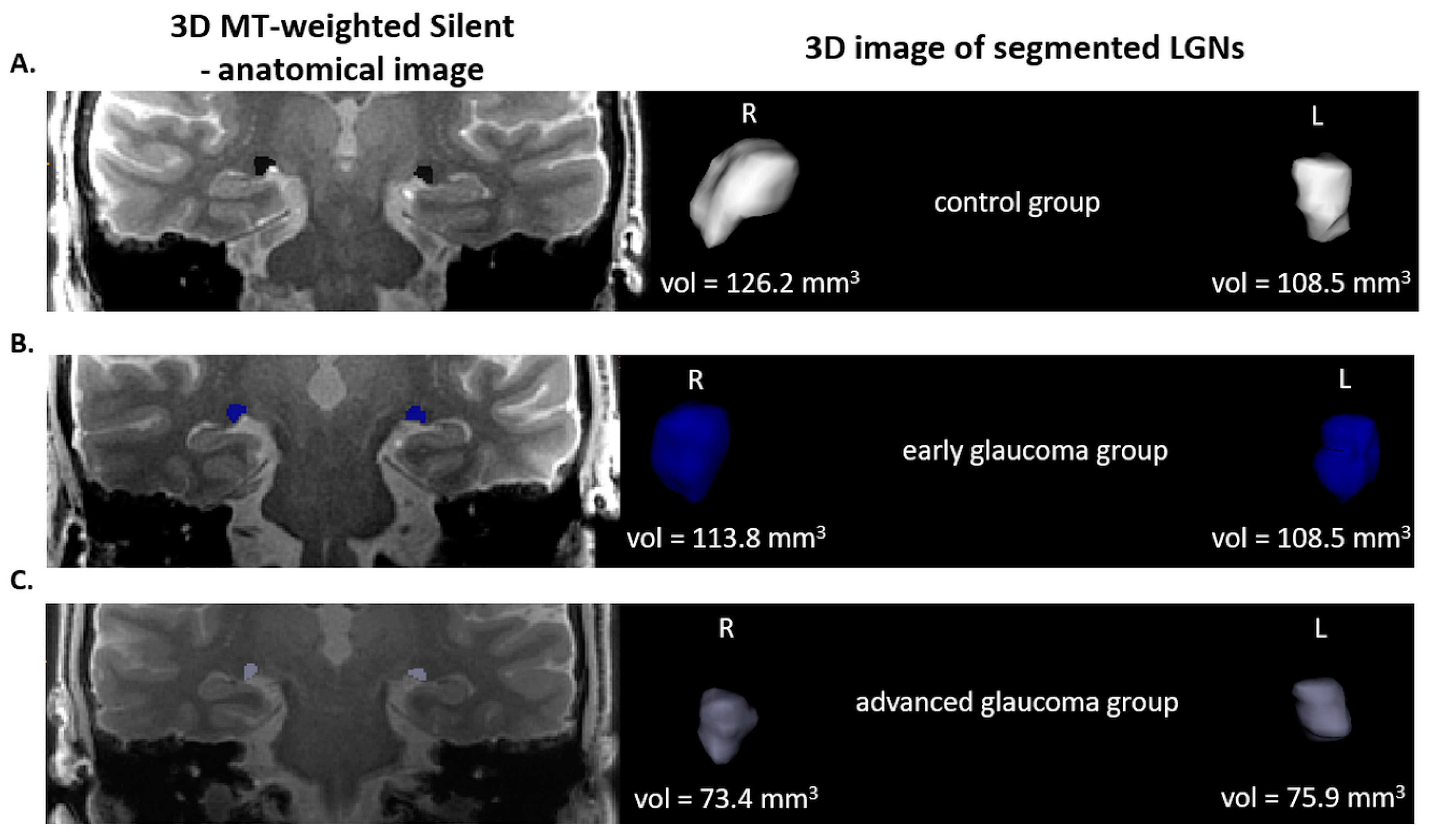
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Quigley, H.A.; Broman, A.T. The number of people with glaucoma worldwide in 2010 and 2020. Br. J. Ophthalmol. 2006, 90, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Yucel, Y.H.; Zhang, Q.; Weinreb, R.N.; Kaufman, P.L.; Gupta, N. Atrophy of relay neurons in magno- and parvocellular layers in the lateral geniculate nucleus in experimental glaucoma. Investig. Ophthalmol. Vis. Sci. 2001, 42, 3216–3222. [Google Scholar]
- Gupta, N.; Greenberg, G.; de Tilly, L.N.; Gray, B.; Polemidiotis, M.; Yucel, Y.H. Atrophy of the lateral geniculate nucleus in human glaucoma detected by magnetic resonance imaging. Br. J. Ophthalmol. 2009, 93, 56–60. [Google Scholar] [CrossRef] [PubMed]
- Ito, Y.; Shimazawa, M.; Chen, Y.N. Morphological changes in the visual pathway induced by experimental glaucoma in Japanese monkeys. Expert Eye Res. 2009, 89, 246–255. [Google Scholar] [CrossRef]
- Prins, D.; Hanekamp, S.; Cornelissen, F.W. Structural brain MRI studies in eye diseases: Are they clinically relevant? A review of current findings. Acta Ophthalmol. 2016, 94, 113–121. [Google Scholar] [CrossRef]
- Leske, M.C.; Heijl, A.; Hussein, M.; Bengtsson, B.; Hyman, L.; Komaroff, E. Factors for glaucoma progression and the effect of treatment: The early manifest glaucoma trial. Arch. Ophthalmol. 2003, 121, 48–56. [Google Scholar] [CrossRef]
- Kastner, S.; Schneider, K.A.; Wunderlich, K. Beyond a relay nucleus: Neuroimaging views on the human LGN. Prog. Brain Res. 2006, 155, 125–143. [Google Scholar]
- Kerrigan-Baumrind LA, Quigley HA, Pease ME, Kerrigan DF, Mitchell RS, Number of ganglion cells in glaucoma eyes compared with threshold visual field tests in the same persons. Investig. Ophthalmol. Vis. Sci. 2000, 41, 741–748.
- Chen, W.W.; Wang, N.; Cai, S.; Fang, Z.; Yu, M.; Wu, Q. Structural brain abnormalities in patients with primary open-angle glaucoma: A study with 3T MR imaging. Investig. Ophthalmol. Vis. Sci. 2013, 54, 545–554. [Google Scholar] [CrossRef]
- Li, C.; Cai, P.; Shi, L.; Lin, Y.; Zhang, J.; Liu, S. Voxel-based morphometry of the visual-related cortex in primary open angle glaucoma. Curr. Eye Res. 2012, 37, 794–802. [Google Scholar] [CrossRef]
- Engelhorn, T.; Michelson, G.; Waerntges, S.; Struffert, T.; Haider, S.; Doerfler, A. Diffusion tensor imaging detects rarefaction of optic radiation in glaucoma patients. Acad Radiol. 2011, 18, 764–769. [Google Scholar] [CrossRef] [PubMed]
- Li, S. Diagnostic utility of central damage determination in glaucoma by magnetic resonance imaging: An observational study. Expert Therap. Med. 2019, 17, 1891–1895. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Jeong, H.J.; Lee, J.H.; Kim, Y.J.; Kim, E.Y.; Kim, Y.Y.; Ryu, T.; Cho, Z.H.; Kim, Y.B. An investigation of lateral geniculate nucleus volume in patients with primary open-angle glaucoma using 7 tesla magnetic resonance imaging. Investig. Ophthalmol. Vis. Sci. 2014, 55, 3468–3476. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schmidt, M.A.; Knott, M.; Heidemann, R.; Michelson, G.; Kober, T.; Dörfler, A.; Engelhorn, T. Investigation of lateral geniculate nucleus volume and diffusion tensor imaging in patients with normal tension glaucoma using 7 tesla magnetic resonance imaging. PLoS ONE 2018, 13, e0198830. [Google Scholar] [CrossRef]
- Costagli, M.; Symms, M.R.; Angeli, L.; Kelley, D.A.; Biagi, L.; Farnetani, A.; Rua, C.; Donatelli, G.; Tiberi, G.; Tosetti, M.; et al. Assessment of Silent T1-weighted head imaging at 7 T. Eur. Radiol. 2016, 26, 1879–1888. [Google Scholar] [CrossRef]
- Madio, D.P.; Lowe, I.J. Ultra-Fast Imaging Using Low Flip Angles and FIDs. Magn. Reson. Med. 1995, 34, 520–525. [Google Scholar] [CrossRef]
- Yushkevich, P.; Piven, J.; Hazlett, H.C.; Gimpel Smith, R.; Ho, S.; Gee, J.C.; Gerig, G. User-guided 3D active contour segmentation of anatomical structures: Significantly improved efficiency and reliability. Neuroimage 2006, 31, 1116–1128. [Google Scholar] [CrossRef]
- Symms, M.R.; Costagli, M.; Buonincontri, G.; Wiesinger, F.; Kelley, D.A.; Tosetti, M. Zero Time of Echo imaging with an Adiabatic Fat Suppression Pulse at 7T. In Proceedings of the International Society for Magnetic Resonance in Medicine, Paris, France, 16–21 June 2018. [Google Scholar]
- Symms, M.; Jäger, H.R.; Schmierer, K.; Yousry, T.A. A review of structural magnetic resonance neuroimaging. J. Neurol. Neurosurg. Psychiatry 2004, 75, 1235–1244. [Google Scholar] [CrossRef]
- Sibon, I.; Tourdias, T.; Felix, S.; Asselineau, J.; Bracoud, L.; Dousset, V. Magnetisation transfer parameters and stroke outcome. J. Clin. Neurosci. 2015, 22, 1012–1017. [Google Scholar] [CrossRef]
- Thorpe, J.W.; Barker, G.J.; Jones, S.J.; Moseley, I.; Losseff, N.; Miller, D.H. Magnetisation transfer ratios and transverse magnetisation decay curves in optic neuritis: Correlation with clinical findings and electrophysiology. J. Neurol. Neurosurg. Psych. 1995, 59, 487–492. [Google Scholar] [CrossRef][Green Version]
- Liu, Z.; Pardini, M.; Yaldizli, O.; Sethi, V.; Muhlert, N.; Chard, D.T. Magnetization transfer ratio measures in normal-appearing white matter show periventricular gradient abnormalities in multiple sclerosis. Brain 2015, 138, 1239–1246. [Google Scholar] [CrossRef] [PubMed]
- Kolappan, M.; Henderson, A.P.; Jenkins, T.M.; Wheeler-Kingshott, C.A.; Plant, G.T.; Miller, D.H. Assessing structure and function of the afferent visual pathway in multiple sclerosis and associated optic neuritis. J. Neurol. 2009, 256, 305–319. [Google Scholar] [CrossRef] [PubMed]
- Klistorner, A.; Chaganti, J.; Garrick, R.; Moffat, K.; Yiannikas, C. Magnetisation transfer ratio in optic neuritis is associated with axonal loss, but not with demyelination. Neuroim 2011, 56, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Nucci, A.; Martucci, M.; Cesareo, M. Brain involvement in glaucoma: Advanced neuroimaging for understanding and monitoring a new target for therapy. Curr. Opin. Pharmacol. 2013, 13, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Johnson, H.; Cowey, A. Transneuronal retrograde degeneration of retinal ganglion cells following restricted lesions of striate cortex in the monkey. Exp. Brain Res. 2000, 132, 269–275. [Google Scholar] [CrossRef]
- Yucel, Y.H.; Gupta, N. Glaucoma of the brain: A disease model for the study of transsynaptic neural degeneration. Prog. Brain Res. 2008, 173, 465–478. [Google Scholar]
- Yücel, Y.H.; Zhang, Q.; Gupta, N.; Kaufman, P.L.; Weinreb, R.N. Loss of neurons in magnocellular and parvocellular layers of the lateral geniculate nucleus in glaucoma. Arch Ophthalmol. 2000, 118, 378–384. [Google Scholar] [CrossRef]
- Mancino, R.; Martucci, A.; Cesareo, M.; Giannini, C.; Corasaniti, M.T.; Bagetta, G.; Nucci, C. Glaucoma and Alzheimer Disease: One Age-Related Neurodegenerative Disease of the Brain. Curr. Neuropharmacol. 2018, 16, 971–977. [Google Scholar] [CrossRef]
- Chiasseu, M.; Cueva Vargas, J.L.; Destroismaisons, L.; Vande Velde, C.; Leclerc, N.; Di Polo, A. Tau accumulation, altered phosphorylation, and missorting promote neurodegeneration in glaucoma. J. Neurosci. 2016, 36, 5785–5798. [Google Scholar] [CrossRef]
- Bayer, A.U.; Keller, O.N.; Ferrari, F.; Maag, K.P. Association of glaucoma with neurodegenerative diseases with apoptotic cell death: Alzheimer’s disease and Parkinson’s disease. Am. J. Ophthalmol. 2002, 133, 135–137. [Google Scholar] [CrossRef]
- Saccà, S.C.; Cutolo, C.A.; Rossi, T. Visual Defects and Ageing. Subcell Biochem. 2019, 91, 393–434. [Google Scholar] [PubMed]
- Brusini, P. OCT Glaucoma Staging System: A New Method for Retinal Nerve Fiber Layer Damage Classification Using Spectral-Domain OCT. Eye 2002, 32, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Furlanetto, R.L.; Teixeira, S.H.; Barbosa Gracitelli, C.P.; Lottenberg, C.L.; Emori, F.; Michelan, M.; Amaro, E., Jr.; Paranhos, A.J. Structural and Functional Analyses of the Optic Nerve and Lateral Geniculate Nucleus in Glaucoma. PLoS ONE 2018, 13, e0194038. [Google Scholar] [CrossRef]
- Fry, L.E.; Fahy, E.; Chrysostomou, V. The coma in glaucoma: Retinal ganglion cell dysfunction and recovery. Prog. Retin Eye Res. 2018, 65, 77–92. [Google Scholar] [CrossRef]
- Malik, R.; Swanson, W.H.; Garway-Heath, D.F. Structure-function relationship’ in glaucoma: Past thinking and current concepts. Clin. Exp. Ophthalmol. 2012, 40, 369–380. [Google Scholar] [CrossRef]
- Wang, L.; Cioffi, G.A.; Cull, G. Immunohistologic evidence for retinal glial cell changes in human glaucoma. Investig. Ophthalmol. Vis. Sci. 2002, 43, 1088–1094. [Google Scholar]
- Chen, Z.; Wang, J.; Lin, F.; Dai, H.; Mu, K.; Zhang, H. Correlation between lateral geniculate nucleus atrophy and damage to the optic disc in glaucoma. J. Neuroradiol. 2013, 40, 281–287. [Google Scholar] [CrossRef]



| TR | TE | TI | ETL | Image Resolution | FOV | NEX | Matrix Size | |
|---|---|---|---|---|---|---|---|---|
| (ms) | (ms) | (ms) | (mm) | (cm) | ||||
| Ax 3D BRAVO T1 | 6.5 | 2.5 | 450 | 1 | 1 × 1 × 1 | 22 | 1 | 288 × 288 |
| Cor FSE XL T2 | 9230 | 21.3 | – | 24 | 1.4 × 1.4 | 18 | 3 | 384 × 384 |
| Sag 3D CUBE T2 | 2500 | 72.3 | – | 100 | 1 × 1 × 1 | 24 | 1 | 256 × 256 |
| Cor 3D MT-Silent | 257 | 0 | – | 1 | 0.75 × 0.75 × 0.75 | 18 | 3 | 224 × 224 |
| Control Group | Primary Glaucoma | Advanced Glaucoma | p-Level | |||
|---|---|---|---|---|---|---|
| n = 9 18 Eyes | n = 11 22 Eyes | n = 9 18 Eyes | Control vs. Early | Control vs. Advanced | Early vs. Advanced | |
| Age (y) | 70.5 ± 7.8 | 64.3 ± 8.7 | 70.7 ± 11.5 | 0.388 | 0.999 | 0.363 |
| Visual field MD right (dB) | 0.36 ± 0.70 | −4.85 ± 3.18 | −17.37 ± 4.20 | 0.049 | <0.00001 | 0.020 |
| Visual field MD left (dB) | −0.04 ± 1.08 | −4.34 ± 3.13 | −19.70 ± 7.13 | 0.076 | <0.00001 | 0.021 |
| RNFL thickness right (µm) | 92.8 ± 11.6 | 75.7 ± 13.8 | 60.2 74.7 ± 11.0 | 0.059 | 0.0005 | 0.071 |
| RNFL thickness left (µm) | 94.7 ± 11.9 | 74.7 ± 13.3 | 64.7 74.7 ± 9.4 | 0.018 | 0.0006 | 0.272 |
| VFI right (%) | 99.9 ± 0.3 | 85.6 ± 9.7 | 51.8 ± 12.9 | 0.034 | 0.00001 | 0.086 |
| VFI left (%) | 99.9 ± 0.3 | 87.4 ± 13.0 | 46.3 ± 24.5 | 0.014 | 0.00006 | 0.259 |
| Investigator 1 | Investigator 2 | Average | Concordance Assessment | ||
|---|---|---|---|---|---|
| Mean ± SD (mm3) | Mean ± SD (mm3) | Mean ± SD (mm3) | |||
| Control | |||||
| right LGN | 119.9 ± 15.9 | 124.2 ± 17.2 | 122.1 ± 14.4 | 0.70 ** | |
| left LGN | 96.1 ± 14.3 | 107.1 ± 15.6 | 101.6 ± 13.3 | 0.78 ** | |
| Early | |||||
| right LGN | 119.0 ± 30.4 | 121.4 ± 25.3 | 120.2 ± 26.5 | 0.94 *** | |
| left LGN | 101.1 ± 30.9 | 105.4 ± 28.5 | 103.2 ±28.0 | 0.84 *** | |
| Advanced | |||||
| right LGN | 78.5 ± 22.0 | 81.9 ± 15.2 | 80.2 ± 17.7 | 0.69 ** | |
| left LGN | 68.3 ± 18.5 | 75.3 ± 13.0 | 71.8 ± 14.2 | 0.82 ** | |
| Control Group | Early Glaucoma | Advanced Glaucoma | Group Comparison (p-Level) | Right vs. Left (p-Level) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Control vs. Early | Control vs. Advanced | Early vs. Advanced | Control | Early | Advanced | ||||
| Mean right LGN volume (mm3) | 122.1 ± 14.4 | 120.2 ± 26.5 | 80.2 ± 17.7 | 0.998 0.998 | 0.003 0.009 | 0.006 0.012 | 0.009 0.027 | 0.180 0.360 | 0.289 0.289 |
| Mean left LGN volume (mm3) | 101.6 ± 13.3 | 103.2 ±28.0 | 71.8 ± 14.2 | 0.986 0.986 | 0.018 0.036 | 0.012 0.036 | |||
| Mean right thalamus volume (mm3) | 5326 ± 366 | 5842 ± 674 | 5792 ± 505 | 0.143 0.286 | 0.120 0.360 | 0.980 0.980 | 0.320 0.960 | 0.667 1.000 | 0.721 0.721 |
| Mean left thalamus volume (mm3) | 5152 ± 325 | 5697 ± 653 | 5696 ± 563 | 0.120 0.240 | 0.120 0.240 | 0.999 0.999 | |||
| Control Group | Early Glaucoma | Advanced Glaucoma | Glaucoma (Early and Advanced) | |||||
|---|---|---|---|---|---|---|---|---|
| Pearson’s r | Spearman’s R | Pearson’s r | Spearman’s R | Pearson’s r | Spearman’s R | Pearson’s r | Spearman’s R | |
| LGN volume vs. Age | ||||||||
| R | 0.07 | 0.07 | –0.21 | –0.20 | –0.07 | –0.17 | –0.30 | –0.44 |
| L | –0.41 | –0.55 | –0.11 | –0.14 | –0.13 | –0.17 | –0.25 | –0.42 |
| LGN volume vs. MD | ||||||||
| MD–LGN (R & L) corresponding eye | – | – | −0.21 | −0.25 | −0.14 | −0.13 | −0.56 ** | −0.58 *** |
| MD–LGN (R & L) opposite eye | – | – | −0.31 | −0.32 | −0.13 | −0.13 | −0.58 *** | −0.61 *** |
| LGN volume vs. mean RNFL | ||||||||
| RNFL–LGN (R & L) corresponding eye | 0.51 | 0.41 | 0.57 ** | 0.53 * | 0.18 | 0.10 | 0.62 *** | 0.52 ** |
| RNFL–LGN (R & L) opposite eye | 0.58 * | 0.58 * | 0.58 ** | 0.53 * | 0.30 | 0.17 | 0.64 *** | 0.56 *** |
| LGN volume vs. VFI | ||||||||
| VFI- LGN (R & L) corresponding eye | –0.25 | –0.24 | 0.11 | 0.04 | 0.38 | 0.45 | 0.56 ** | 0.53 ** |
| VFI- LGN (R & L) opposite eye | –0.25 | –0.24 | 0.19 | 0.16 | 0.29 | 0.35 | 0.56 ** | 0.58 ** |
| LGN volume vs. quadrant RNFL | ||||||||
| LGN–Inferior (R & L) corresponding eye | 0.43 | 0.23 | 0.47 * | 0.44 | –0.22 | –0.31 | 0.53 ** | 0.40 * |
| LGN–Inferior (R & L) opposite eye | 0.49 | 0.44 | 0.55 * | 0.51 * | –0.15 | –0.31 | 0.58 *** | 0.47 ** |
| LGN–Superior (R & L) corresponding eye | 0.23 | 0.31 | 0.50 * | 0.50 * | 0.51 * | 0.33 | 0.62 *** | 0.61 *** |
| LGN–Superior (R & L) opposite eye | 0.50 | 0.45 | 0.47 * | 0.37 | 0.62 * | 0.37 | 0.63 *** | 0.63 *** |
| LGN–Nasal (R & L) corresponding eye | 0.33 | 0.40 | 0.01 | –0.07 | –0.06 | –0.08 | 0.15 | 0.13 |
| LGN–Nasal (R & L) opposite eye | 0.24 | 0.28 | –0.08 | –0.13 | –0.01 | –0.17 | 0.12 | 0.12 |
| LGN–Temporal (R & L) corresponding eye | 0.59 * | 0.50 | 0.66 ** | 0.63 ** | 0.06 | 0.14 | 0.42 * | 0.51 ** |
| LGN–Temporal (R & L) opposite eye | 0.48 | 0.62 * | 0.68 ** | 0.65 ** | 0.17 | 0.26 | 0.46 * | 0.54 *** |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kosior-Jarecka, E.; Pankowska, A.; Polit, P.; Stępniewski, A.; Symms, M.R.; Kozioł, P.; Żarnowski, T.; Pietura, R. Volume of Lateral Geniculate Nucleus in Patients with Glaucoma in 7Tesla MRI. J. Clin. Med. 2020, 9, 2382. https://doi.org/10.3390/jcm9082382
Kosior-Jarecka E, Pankowska A, Polit P, Stępniewski A, Symms MR, Kozioł P, Żarnowski T, Pietura R. Volume of Lateral Geniculate Nucleus in Patients with Glaucoma in 7Tesla MRI. Journal of Clinical Medicine. 2020; 9(8):2382. https://doi.org/10.3390/jcm9082382
Chicago/Turabian StyleKosior-Jarecka, Ewa, Anna Pankowska, Piotr Polit, Andrzej Stępniewski, Mark Roger Symms, Paulina Kozioł, Tomasz Żarnowski, and Radosław Pietura. 2020. "Volume of Lateral Geniculate Nucleus in Patients with Glaucoma in 7Tesla MRI" Journal of Clinical Medicine 9, no. 8: 2382. https://doi.org/10.3390/jcm9082382
APA StyleKosior-Jarecka, E., Pankowska, A., Polit, P., Stępniewski, A., Symms, M. R., Kozioł, P., Żarnowski, T., & Pietura, R. (2020). Volume of Lateral Geniculate Nucleus in Patients with Glaucoma in 7Tesla MRI. Journal of Clinical Medicine, 9(8), 2382. https://doi.org/10.3390/jcm9082382






