Could Evening Dietary Protein Intake Play a Role in Nocturnal Polyuria?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Renal Function Profiling
2.3. Protein Intake Estimation
2.4. Statistical Analysis
3. Results
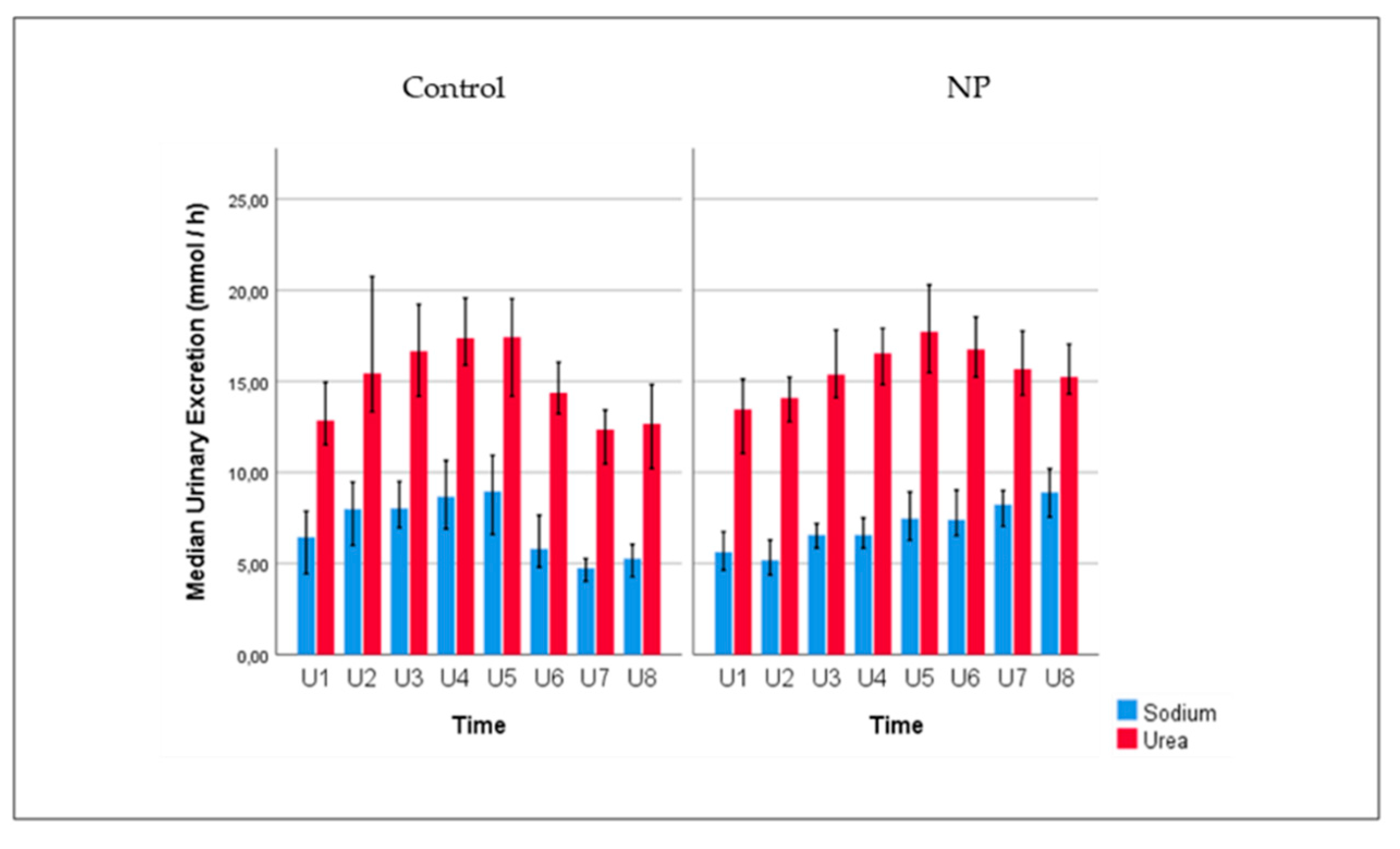
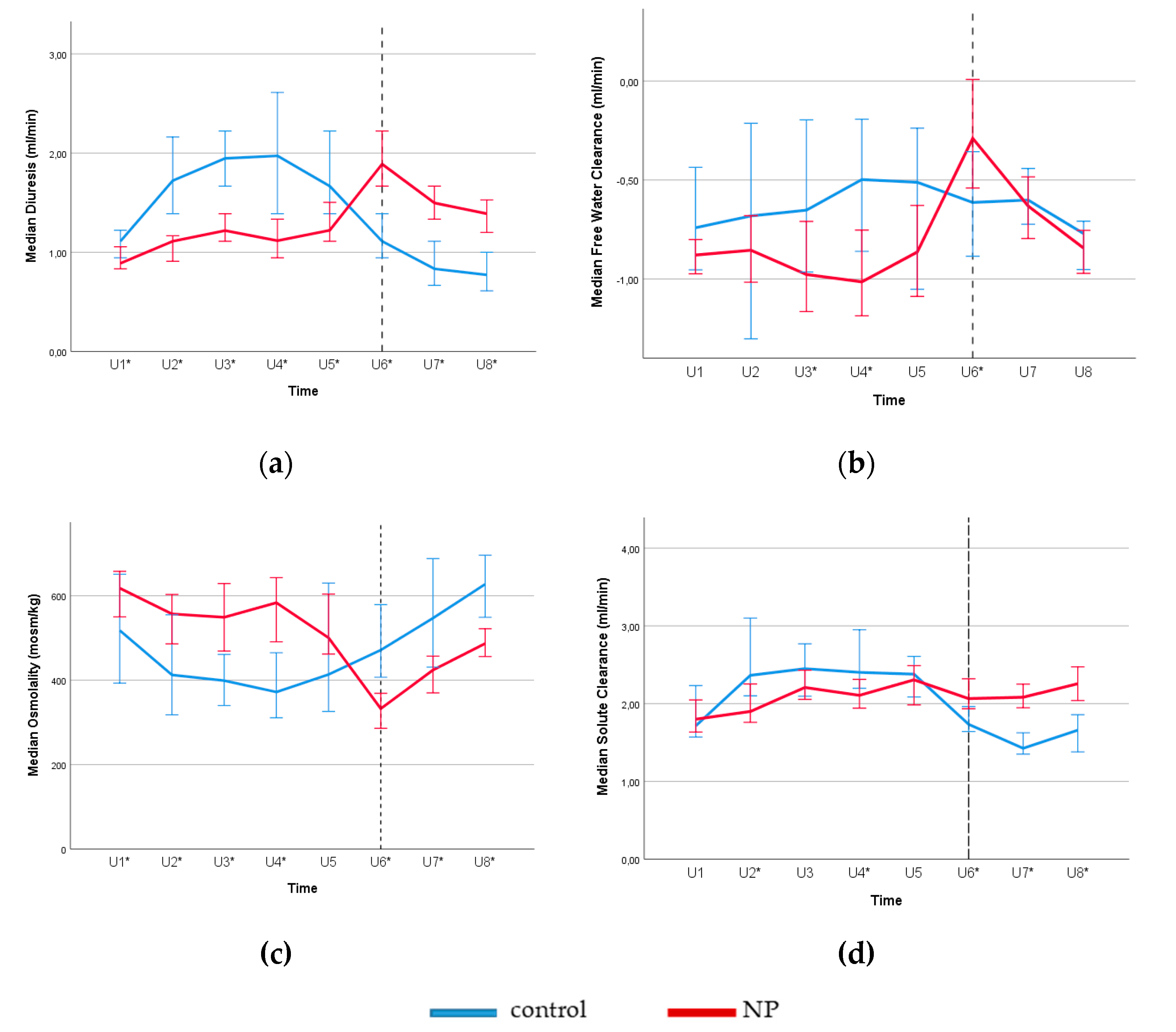
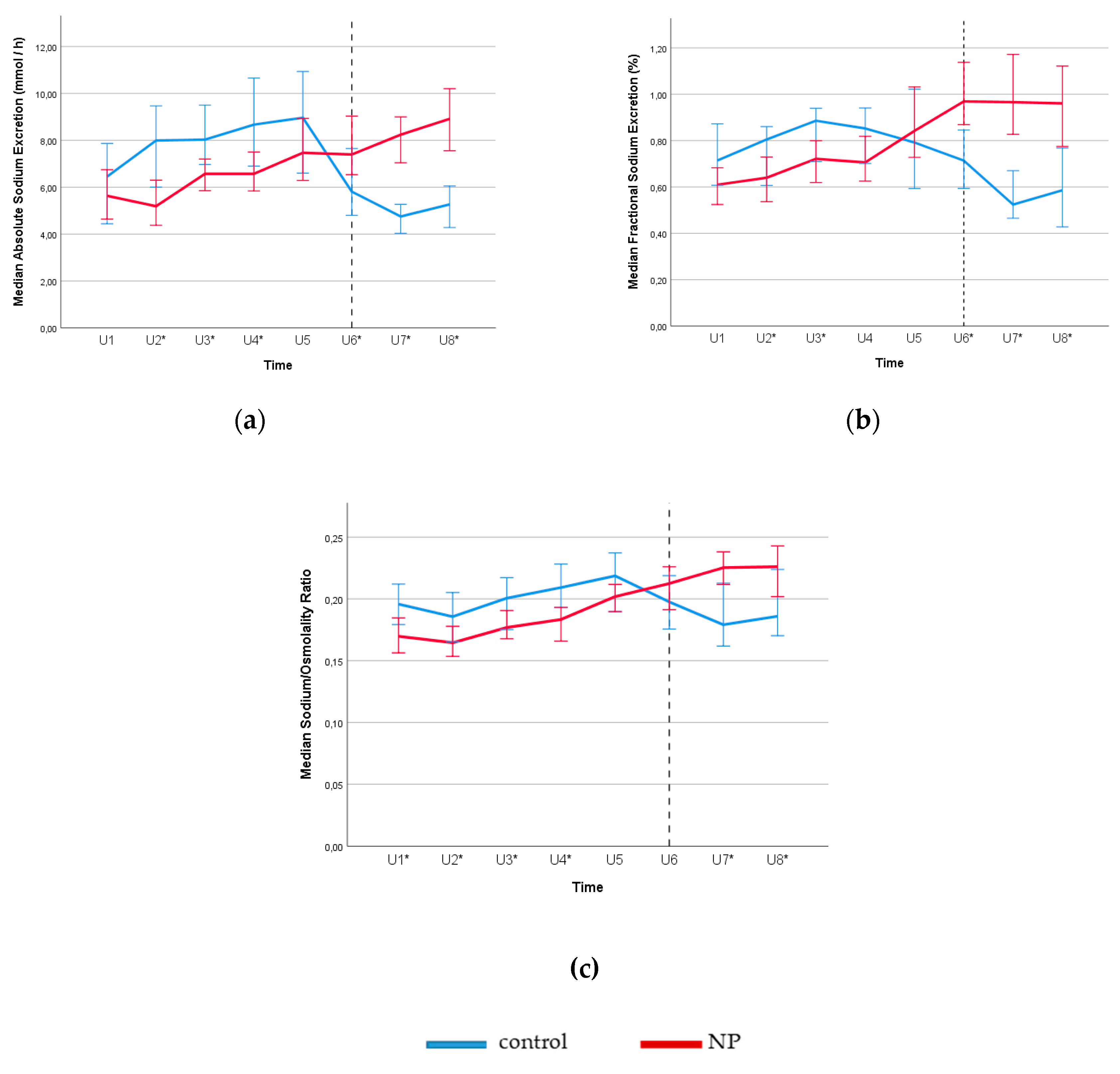
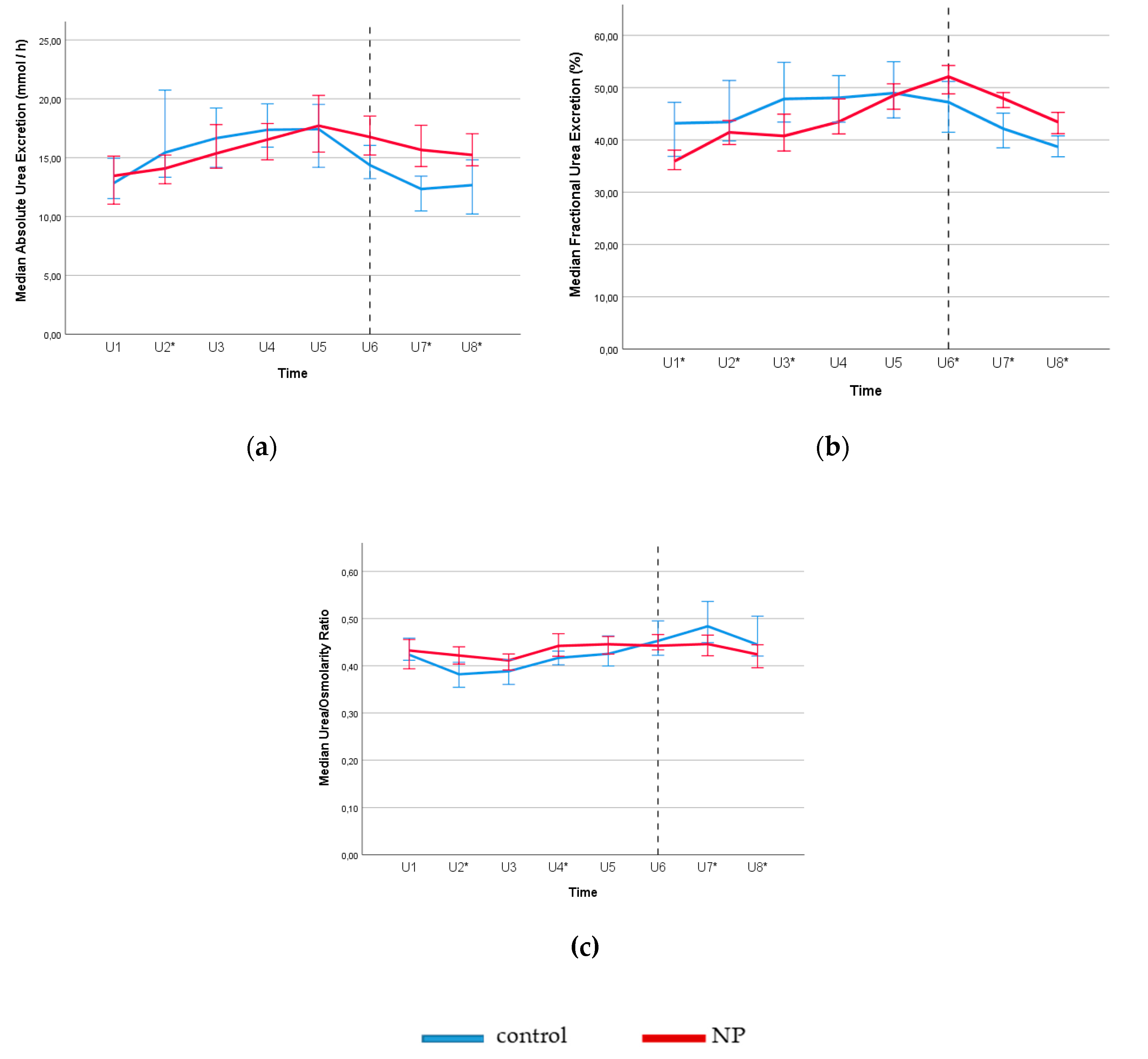
3.1. Renal Function Profiles and Estimated Protein Intake
3.2. Circadian Rhythms of Water and Osmotic Diuresis
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hashim, H.; Wen, J.G.; Wein, A.; Drake, M.J.; Djurhuus, J.C.; Meijlink, J.; Blanker, M.H.; Morris, V.; Petros, P. International Continence Society (ICS) report on the terminology for nocturia and nocturnal lower urinary tract function. Neurourol. Urodyn. 2019, 38, 499–508. [Google Scholar] [CrossRef]
- Everaert, K.; Hervé, F.; Bower, W.; Djurhuus, J.C.; Dmochowski, R.; Fine, N.; Wein, A.; Wyndaele, M.; Weiss, J. How can we develop a more clinically useful and robust algorithm for diagnosing and treating nocturia? ICI-RS 2017. Neurourol. Urodyn. 2018, 37, S46–S59. [Google Scholar] [CrossRef] [PubMed]
- Weiss, J.P.; Van Kerrebroeck, P.E.V.; Klein, B.M.; Nørgaard, J.P. Excessive nocturnal urine production is a major contributing factor to the etiology of nocturia. J. Urol. 2011, 186, 1358–1363. [Google Scholar] [CrossRef] [PubMed]
- Hofmeester, I.; Kollen, B.J.; Steffens, M.G.; Bosch, J.R.; Drake, M.J.; Weiss, J.P.; Blanker, M.H. The association between nocturia and nocturnal polyuria in clinical and epidemiological studies: A systematic review and meta-analyses. J. Urol. 2014, 191, 1028–1033. [Google Scholar] [CrossRef] [PubMed]
- Goessaert, A.S.; Krott, L.; Hoebeke, P.; Vande Walle, J.; Everaert, K. Diagnosing the pathophysiologic mechanisms of nocturnal polyuria. Eur. Urol. 2015, 67, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Monaghan, T.F.; Bliwise, D.L.; Denys, M.A.; Goessaert, A.S.; Decalf, V.; Kumps, C.; Vande Walle, J.; Weiss, J.P.; Epstein, M.R.; Weedon, J.; et al. Phenotyping nocturnal polyuria: Circadian and age-related variations in diuresis rate, free water clearance and sodium clearance. Age Ageing 2020, 49, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Dossche, L.; Vande Walle, J.; Van Herzeele, C. The pathophysiology of monosymptomatic nocturnal enuresis with special emphasis on the circadian rhythm of renal physiology. Eur. J. Pediatr. 2016, 7175, 47–54. [Google Scholar] [CrossRef]
- Everaert, K.; Hervé, F.; Bosch, R.; Dmochowski, R.; Drake, M.; Hashim, H.; Chapple, C.; Van Kerrebroeck, P.; Mourad, S.; Abrams, P.; et al. International continence society consensus on the diagnosis and treatment of nocturia. Neurourol. Urodyn. 2019, 38, 478–498. [Google Scholar] [CrossRef]
- Gasthuys, E.; Dossche, L.; Michelet, R.; Nørgaard, J.P.; Devreese, M.; Croubels, S.; Vermeulen, A.; Van Bocxlaer, J.; Walle, J.V. Pediatric pharmacology of desmopressin in children with enuresis: A comprehensive review. Pediatr. Drugs 2020, 22, 369–383. [Google Scholar] [CrossRef]
- Okumura, Y.; Asai, K.; Kobayashi, T.; Miyata, H.; Tanaka, Y.; Okada, Y.; Sakai, K.; Kamba, T.; Tsuji, H.; Shide, K.; et al. Dietary sodium restriction reduces nocturnal urine volume and nocturnal polyuria index in renal allograft recipients with nocturnal polyuria. Urology 2017, 106, 60–64. [Google Scholar] [CrossRef]
- Matsuo, T.; Miyata, Y.; Sakai, H. Effect of salt intake reduction on nocturia in patients with excessive salt intake. Neurourol. Urodyn. 2019, 38, 927–933. [Google Scholar] [CrossRef] [PubMed]
- Monaghan, T.F.; Michelson, K.P.; Wu, Z.D.; Gong, F.; Agudelo, C.W.; George, C.D.; Alwis, U.S.; Epstein, M.R.; Mekki, P.; Flores, V.X.; et al. Sodium restriction improves nocturia in patients at a cardiology clinic. J. Clin. Hypertens 2020, 22, 633–638. [Google Scholar] [CrossRef] [PubMed]
- Bankir, L.; Bouby, N.; Ritz, E. Vasopressin: A novel target for the prevention and retardation of kidney disease? Nat. Rev. Nephrol. 2013, 9, 223–239. [Google Scholar] [CrossRef] [PubMed]
- Fouillet, H.; Juillet, B.; Bos, C.; Mariotti, F.; Gaudichon, C.; Benamouzig, R.; Tomé, D. Urea-nitrogen production and salvage are modulated by protein intake in fed humans: Results of an oral stable-isotope-tracer protocol and compartmental modeling. Am. J. Clin. Nutr. 2008, 87, 1702–1714. [Google Scholar] [CrossRef] [PubMed]
- Weiner, I.D.; Mitch, W.E.; Sands, J.M. Urea and ammonia metabolism and the control of renal nitrogen excretion. Clin. J. Am. Soc. Nephrol. 2015, 10, 1444–1458. [Google Scholar] [CrossRef]
- Bankir, L.; Roussel, R.; Bouby, N. Protein-and diabetes-induced glomerular hyperfiltration: Role of glucagon, vasopressin, and urea. Am. J. Physiol.-Ren. Physiol. 2015, 309, F2–F23. [Google Scholar] [CrossRef]
- EFSA Panel on Dietetic Products, Nutrition, and Allergies (NDA). Scientific opinion on dietary reference values for protein. EFSA J. 2012, 10, 1–66. [Google Scholar]
- Higgins, C. Urea and the Clinical Value of Measuring Blood Urea Concentration. 2016. Available online: acutecaretesting.org/en/articles/urea-and-the-clinicalvalue-of-measuring-blood-urea-concentration (accessed on 7 May 2020).
- Goldstein, M.; Lenz, P.; Levitt, M. Effect of urine flow rate on urea reabsorption in man: Urea as a tubular marker. J. Appl. Physiol. 1969, 26, 594–599. [Google Scholar] [CrossRef]
- Krishna, G.G.; Newell, G.; Miller, E.; Heeger, P.; Smith, R.; Polansky, M.; Kapoor, S.; Hoeldtke, R. Protein-induced glomerular hyperfiltration: Role of hormonal factors. Kidney Int. 1988, 33, 578–583. [Google Scholar] [CrossRef]
- Hostetter, T.H. Human renal response to a meat meal. Am. J. Physiol.-Ren. Fluid Electrolyte Physiol. 1986, 250, F613–F618. [Google Scholar] [CrossRef]
- Stevens, L.A.; Shastri, S.; Levey, A. Assessment of Renal Function. In Comprehensive Clinical Nephrology; Floege, J., Ed.; Elsevier: St. Louis, MO, USA, 2010; pp. 31–38. [Google Scholar]
- Elorza, M.A.; Garcia, A.; Fuster, A.; Muller, A. Evaluation of the “Auto-Stat 6010” automatic osmometer and its comparison with the “Digimatic-Advanced 3DII” manual osmometer. Eur. J. Clin. Chem. Clin. Biochem. 1993, 31, 245–249. [Google Scholar] [PubMed]
- Wuyts, B.; Bernard, D.; Van Den Noortgate, N.; Van De Walle, J.; Van Vlem, B.; De Smet, R.; De Geeter, F.; Vanholder, R.; Delanghe, J.R. Re-evaluation of formulas for predicting creatinine clearance in adults and children, using compensated creatinine methods. Clin. Chem. 2003, 49, 1011–1014. [Google Scholar] [CrossRef]
- Sampson, E.J.; Baird, M.A. Chemical inhibition used in a kinetic urease/glutamate dehydrogenase method for urea in serum. Clin. Chem. 1979, 25, 1721–1729. [Google Scholar] [CrossRef] [PubMed]
- von Eckardstein, A.; Roth, H.J.; Jones, G.; Preston, S.; Szekeres, T.; Imdahl, R.; Conti, M.; Blanckaert, N.; Jose, D.; Thiery, J.; et al. Cobas 8000 modular analyzer series evaluated under routine-like conditions at 14 sites in Australia, Europe, and the United States. J. Lab. Autom. 2013, 18, 306–327. [Google Scholar] [CrossRef] [PubMed]
- Teunissen-Beekman, K.F.; Dopheide, J.; Geleijnse, J.M.; Bakker, S.J.; Brink, E.J.; de Leeuw, P.W.; van Baak, M.A. Effect of increased protein intake on renal acid load and renal hemodynamic responses. Physiol. Rep. 2016, 4, e12687. [Google Scholar] [CrossRef]
- De Ridder, K. Proteins. In Food Consumption Survey 2014–2015. Report 4; Bel, S., Tafforeau, J., Eds.; WIV-ISP: Brussels, Belgium, 2016. [Google Scholar]
- De Ridder, K.; Teppers, E. Sodium. In Food Consumption Survey 2014–2015. Report 4; Bel, S., Tafforeau, J., Eds.; WIV-ISP: Brussels, Belgium, 2016. [Google Scholar]
- Kanno, H.; Kanda, E.; Sato, A.; Sakamoto, K. Estimation of daily protein intake based on spot urine urea nitrogen concentration in chronic kidney disease patients. Clin. Exp. Nephrol. 2016, 20, 258–264. [Google Scholar] [CrossRef]
- Kida, Y.; Ueda, H.; Tanaka, H.; Ichinose, M. Estimation of protein intake using urinary urea nitrogen in patients with early-stage liver cirrhosis. Hepatol. Int. 2007, 1, 382–386. [Google Scholar] [CrossRef][Green Version]
- Chin, H.J.; Kim, D.K.; Park, J.H.; Shin, S.J.; Lee, S.H.; Choi, B.S.; Kim, S.; Lim, C.S. Effect of urine urea nitrogen and protein intake adjusted by using the estimated urine creatinine excretion rate on the antiproteinuric effect of angiotensin II type I receptor blockers. Nutrition 2015, 31, 1333–1338. [Google Scholar] [CrossRef]
- Miller, M. Nocturnal polyuria in older people: Pathophysiology and clinical implications. J. Am. Geriatr. Soc. 2000, 48, 1321–1329. [Google Scholar] [CrossRef]
- Musch, W.; Verfaillie, L.; Decaux, G. Age-related increase in plasma urea level and decrease in fractional urea excretion: Clinical application in the syndrome of inappropriate secretion of antidiuretic hormone. Clin. J. Am. Soc. Nephrol. 2006, 1, 909–914. [Google Scholar] [CrossRef]
- Perucca, J.; Bouby, N.; Valeix, P.; Bankir, L. Sex difference in urine concentration across differing ages, sodium intake, and level of kidney disease. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2007, 292, R700–R705. [Google Scholar] [CrossRef] [PubMed]
- Johnston, J.D.; Ordovás, J.M.; Scheer, F.A.; Turek, F.W. Circadian rhythms, metabolism, and chrononutrition in rodents and humans. Adv. Nutr. 2016, 7, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Kessler, K.; Pivovarova-Ramich, O. Meal timing, aging, and metabolic health. Int. J. Mol. Sci. 2019, 20, 1911. [Google Scholar] [CrossRef]
- EFSA Panel on Dietetic Products, Nutrition, and Allergies (NDA). Scientific Opinion on Dietary reference values for water. EFSA J. 2010, 8, 1459. [Google Scholar]
| Control (n = 52) | NP (n = 118) | p–Value | |
|---|---|---|---|
| Age (years) | 51 (37–66) | 67 (58–73) | <0.001 * |
| Sex (F // M) | 40 // 12 | 65 // 53 | 0.007 * |
| BMI (kg/m2) | 24 (22–26) | 25 (22–28) | 0.172 |
| NUP (ml/h) | 56 (44–84) | 100 (71–126) | <0.001 * |
| Daytime osmolality (mOsm/kg) | 435(318–577) | 537 (442–684) | 0.001 * |
| Nighttime osmolality (mOsm/kg) | 547 (402–680) | 411 (337–534) | 0.001 * |
| 24-h osmolality (mOsm/kg) | 470 (382–622) | 505 (412–628) | 0.404 |
| Daytime sodium excretion (mmol) | 144 (101–175) | 108 (69–137) | <0.001 * |
| Nighttime sodium excretion (mmol) | 53 (36–73) | 80 (61–102) | <0.001 * |
| 24-h sodium excretion (mmol) | 199 (147–259) | 188 (140–247) | 0.361 |
| Daytime urea excretion (mmol) | 306 (233–371) | 260 (198–324) | 0.009 * |
| Nighttime urea excretion (mmol) | 132 (106–152) | 156 (129–197) | <0.001 * |
| 24-h urea excretion (mmol) | 442 (372–558) | 413 (358–538) | 0.351 |
| Daytime protein intake (g/kg body weight) | 0.9 (0.8–1.1) | 0.8 (0.6–0.9) | <0.001 * |
| Evening protein intake (g/kg body weight) | 0.5 (0.4–0.6) | 0.6 (0.5–0.6) | 0.005 * |
| 24-h protein intake (g/kg body weight) | 1.3 (1.1–1.6) | 1.2 (1.0–1.4) | 0.063 |
| Control | NP | |||
|---|---|---|---|---|
| β | p−Value | β | p−Value | |
| Age (years) | 0.120 | 0.070 | 0.117 | 0.001 * |
| Gender | −0.039 | 0.491 | −0.015 | 0.629 |
| BMI (kg/m2) | 0.028 | 0.596 | 0.021 | 0.466 |
| Nighttime free water clearance (mL/min) | 1.1016 | <0.001 * | 0.971 | <0.001 * |
| Nighttime sodium excretion (mmol) | 0.595 | <0.001 * | 0.509 | <0.001 * |
| Nighttime urea excretion (mmol) | 0.461 | <0.001 * | 0.497 | <0.001 * |
| Nighttime creatinine clearance (mL/min) | 0.217 | 0.006 * | 0.213 | <0.001 * |
| Food | Protein (gram) 1 | Sodium (milligram) 1 | Effect on Urinary Osmolality (mOsm) 2 |
|---|---|---|---|
| Meat products | |||
| Bacon, smoked, salted | 22.7 | 1532 | 263 |
| Beef, smoked, fillet | 22.9 | 3100 | 265 |
| Chicken ham | 20.0 | 787 | 148 |
| Salami | 19.8 | 1370 | 173 |
| Sausage, poultry, raw | 18.9 | 310 | 121 |
| Spread, meat salad | 8.0 | 761 | 79 |
| Milk products | |||
| Cheese spread, full fat | 11.0 | 702 | 92 |
| Cheese, Cheddar | 25.5 | 700 | 173 |
| Cheese, Cottage | 11.7 | 370 | 81 |
| Cheese, Emmentaler | 28.0 | 300 | 170 |
| Cheese, Mozzarella | 19.5 | 200 | 118 |
| Cheese processed, slices light | 17.5 | 1253 | 152 |
| Cereal products | |||
| Baguette, white | 8.5 | 486 | 74 |
| Bread, French roll | 12.5 | 518 | 101 |
| Bread, white | 8.4 | 484 | 74 |
| Croissant | 9.2 | 426 | 76 |
| Crackers | 11.3 | 795 | 105 |
| Corn flakes, enriched | 8.0 | 613 | 77 |
| Muesli, crunchy, enriched | 7.5 | 320 | 61 |
| Granola, crunchy, original | 8.6 | 98 | 58 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alwis, U.S.; Delanghe, J.; Dossche, L.; Walle, J.V.; Van Camp, J.; Monaghan, T.F.; Roggeman, S.; Everaert, K. Could Evening Dietary Protein Intake Play a Role in Nocturnal Polyuria? J. Clin. Med. 2020, 9, 2532. https://doi.org/10.3390/jcm9082532
Alwis US, Delanghe J, Dossche L, Walle JV, Van Camp J, Monaghan TF, Roggeman S, Everaert K. Could Evening Dietary Protein Intake Play a Role in Nocturnal Polyuria? Journal of Clinical Medicine. 2020; 9(8):2532. https://doi.org/10.3390/jcm9082532
Chicago/Turabian StyleAlwis, Upeksha S., Joris Delanghe, Lien Dossche, Johan Vande Walle, John Van Camp, Thomas F. Monaghan, Saskia Roggeman, and Karel Everaert. 2020. "Could Evening Dietary Protein Intake Play a Role in Nocturnal Polyuria?" Journal of Clinical Medicine 9, no. 8: 2532. https://doi.org/10.3390/jcm9082532
APA StyleAlwis, U. S., Delanghe, J., Dossche, L., Walle, J. V., Van Camp, J., Monaghan, T. F., Roggeman, S., & Everaert, K. (2020). Could Evening Dietary Protein Intake Play a Role in Nocturnal Polyuria? Journal of Clinical Medicine, 9(8), 2532. https://doi.org/10.3390/jcm9082532






