Macular Perfusion Impairment in Von Hippel-Lindau Disease Suggests a Generalized Retinal Vessel Alteration
Abstract
:1. Introduction
2. Experimental Section
2.1. Participants
2.2. OCT and OCT Angiography
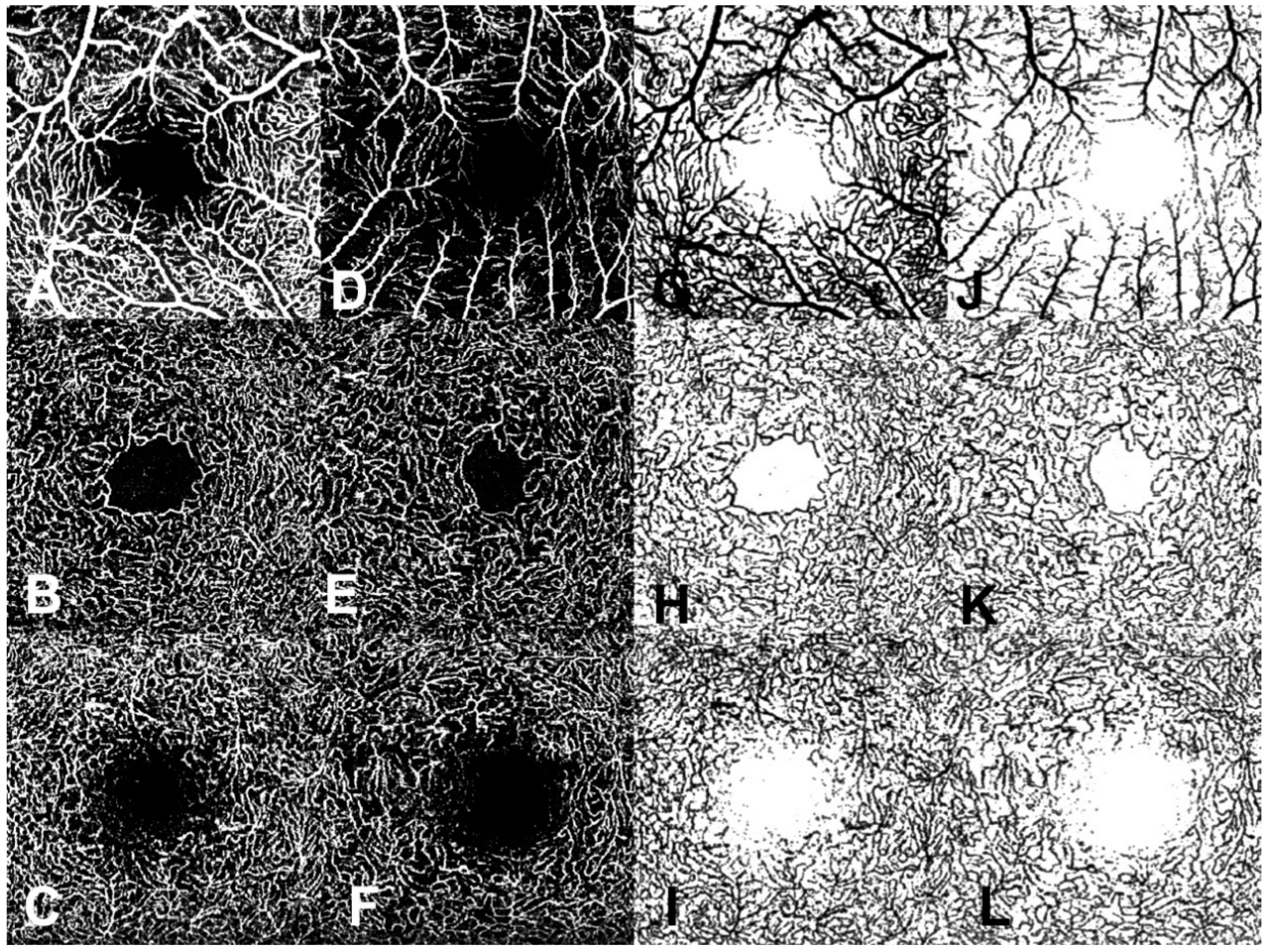
2.3. OCTA en Face Image Analysis
2.4. Statistical Evaluation
3. Results
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Aronow, M.; Wiley, H.; Gaudric, A.; Krivosic, V.; Gorin, M.B.; Shields, C.; Shields, J.A.; Jonasch, E.W.; Singh, A.D.; Chew, E.Y. Von Hippel-Lindau Disease: Update on Pathogenesis and Systemic Aspects. Retina 2019, 39, 2243–2253. [Google Scholar] [CrossRef] [PubMed]
- Von Hippel, E. Die anatomische Grundlage der von mir beschriebenen “sehr seltenen Erkrankung der Netzhaut”. Arch. Opthalmol. 1911, 79, 350–377. [Google Scholar] [CrossRef]
- Lindau, A. Zur Frage der Angiomatosis Retinae und ihrer Hirnkomplikationen. Acta Ophthalmol. Scand. 1927, 4, 193–226. [Google Scholar] [CrossRef]
- Hajjaj, A.; van Overdam, K.A.; Oldengurg, R.A.; Koopmans, A.E.; van den Ouweland, A.M.; de Klein, A.; Kiliç, E. Retinal haemangioblastomas in von Hippel-Lindau germline mutation carriers: Progression, complications and treatment outcome. Acta Ophthalmol. 2020, 98, 464–471. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dalvin, L.A.; Yu, M.D.; Ancona-Lezama, D.A.; Pulido, J.S.; Olsen, T.W.; Shields, C.L. Retinal haemangioblastoma associated with peripheral non-perfusion: Widefield fluoresceina angiography analysis of 41 cases. Br. J. Ophthalmol. 2020, 104, 167–172. [Google Scholar] [CrossRef]
- Spaide, R.F.; Klancnik, J.M., Jr.; Cooney, M.J. Retinal vascular layers imaged by fluorescein angiography and optical coherence tomography angiography. JAMA Ophthalmol. 2015, 133, 45–50. [Google Scholar] [CrossRef]
- Campbell, J.P.; Zhang, M.; Hwang, T.S.; Bailey, S.T.; Wilson, D.J.; Jia, Y.; Huang, D. Detailed Vascular Anatomy of the Human Retina by Projection-Resolved Optical Coherence Tomography Angiography. Sci. Rep. 2017, 7, 42201. [Google Scholar] [CrossRef] [Green Version]
- Lim, H.B.; Kim, Y.W.; Kim, J.M.; Jo, Y.J.; Kim, J.Y. The Importance of Signal Strenght in Quantitative Assessment of Retinal Vessel Density Using Optical Coherence Tomography Angiography. Sci. Rep. 2018, 8, 12897. [Google Scholar] [CrossRef]
- Huang, Y.; Gangaputra, S.; Lee, K.E.; Narkar, A.R.; Klein, R.; Klein, B.E.; Meuer, S.M.; Danis, R.P. Signal Quality Assessment of Retinal Optical CoherenceTomography Images. Investig. Ophthalmol. Vis. Sci. 2012, 53, 2133–2141. [Google Scholar] [CrossRef]
- Parrozzani, R.; Frizziero, L.; Londei, D.; Trainiti, S.; Modugno, R.L.; Leonardi, F.; Pulze, S.; Miglionico, G.; Pilotto, E.; Midena, E. Peripapillary vascular changes in radiation optic neuropathy: An optical coherence tomography angiography grading. Br. J. Ophthalmol. 2018, 102, 1238–1243. [Google Scholar] [CrossRef]
- Kim, A.Y.; Chu, Z.; Shahidzadeh, A.; Wang, R.K.; Puliafito, C.A.; Kashani, A.H. Quantifying microvascular density and morphology in diabetic retinopathy using spectral-domain optical coherence tomography angiography. Investig. Ophthalmol. Vis. Sci. 2016, 57, 362–370. [Google Scholar] [CrossRef]
- Pulido, J.S.; Dalvin, L.A.; Olsen, T.W.; Mano, F.; Yu, M.; Shields, C.L. Peripheral retinal nonperfusion using widefield imaging with von Hippel-Lindau disease. Int. J. Retin. Vitr. 2018, 4, 36–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurihara, T.; Kubota, Y.; Ozawa, Y.; Takubo, K.; Noda, K.; Simon, M.C.; Johnson, R.S.; Suematsu, M.; Tsubota, K.; Ishida, S.; et al. Von Hippel-Lindau protein regulates transition from fetal to adult circulatory system in retina. Development 2010, 137, 1563–1571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arreola, A.; Payne, L.B.; Julian, M.H.; de Cubas, A.A.; Daniels, A.B.; Taylor, S.; Zhao, H.; Darden, J.; Bautch, V.L.; Rathmell, W.K.; et al. Von Hippel-Lindau mutations disrupt vascular patterning and maturation via Notch. JCI Insight 2018, 3, e92193. [Google Scholar] [CrossRef] [PubMed]
- Bonnin, S.; Mané, V.; Couturier, A.; Julien, M.; Pasques, M.; Tadayoni, R.; Gaudric, A. New insight into the macular deep vascular plexus imaged by optical coherence tomography angiography. Retina 2015, 35, 2347–2352. [Google Scholar] [CrossRef] [PubMed]
- Garrity, S.T.; Pasques, M.; Gaudric, A.; Freund, K.B.; Sarraf, D. Considerations in the understanding of venous outflow in the retinal capillary plexus. Retina 2017, 37, 1809–1812. [Google Scholar] [CrossRef] [PubMed]
- Provis, J.M. Development of the primate retinal vasculature. Prog. Retin. Eye Res. 2001, 20, 799–821. [Google Scholar] [CrossRef]
- Pellegrini, M.; Vagge, A.; Ferro Desideri, L.; Bernabei, F.; Triolo, G.; Mastropasqua, R.; Del Noce, C.; Borrelli, E.; Sacconi, R.; Iovino, C.; et al. Optical Coherence Tomography Angiography in Neurodegenerative Disorders. J. Clin. Med. 2020, 9, 1706. [Google Scholar] [CrossRef]
- Huaa, D.; Xua, Y.; Zengb, X.; Yanga, N.; Jianga, M.; Zhanga, X.; Yanga, J.; Hea, T.; Xinga, Y. Use of optical coherence tomography angiography for assessment of microvascular changes in the macula and optic nerve head in hypertensive patients without hypertensive retinopathy. Microvasc. Res. 2020, 129, 103969. [Google Scholar] [CrossRef]
- Yarmohammadi, A.; Zangwill, L.M.; Diniz-Filiho, A.; Diniz-Filho, A.; Suh, M.H.; Yousefi, S.; Saunders, L.J.; Belghith, A.; Manalastas, P.I.C.; Medeiros, F.A.; et al. Relationship between optical coherence tomography angiography vessel density and severity of visual field loss in glaucoma. Ophthalmology 2016, 123, 2498–2508. [Google Scholar] [CrossRef]
- Lee, G.; Park, K.; Oh, S.Y.; Kong, D. Analysis of optic chiasmal compression caused by brain tumors using optical coherence tomography angiography. Sci. Rep. 2020, 10, 2088. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sagar, P.; Rajesh, R.; Shanmugam, M.; Konana, V.K.; Mishra, D. Comparison of optical coherence tomography angiography and fundus fluorescein angiography features of retinal capillary hemangioblastoma. Indian J. Ophthalmol. 2018, 66, 872–876. [Google Scholar] [PubMed]
- Lang, S.J.; Cakir, B.; Evers, C.; Ludwig, F.; Lange, C.A.K.; Agostini, H.T. Value of Optical Coherence Tomography angiography imaging in diagnosis and treatment of hemangioblastomas in von Hippel-Lindau disease. Ophthalmic Surg. Lasers Imaging 2016, 47, 935–946. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Wang, J.C.; Zeng, R.; Nagata, T.; Katz, R.; Mukai, S.; Miller, J.B. Detection of retinal microvascular changes in von Hippel-Lindau disease using optical coherence tomography angiography. PLoS ONE 2020, 15, e0229213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mao, J.; Lao, J.; Liu, C.; Zhang, C.; Chen, Y.; Tao, J.; Shen, L. A study analyzing macular microvasculature features after vitrectomy using OCT angiography in patients with idiopathic macular epiretinal membrane. BMC Ophthlamol. 2020, 20, 165. [Google Scholar] [CrossRef]
- Dollfus, H.; Massin, P.; Taupin, P.; Nemeth, C.; Amara, S.; Giraud, S.; Béroud, C.; Dureau, P.; Gaudric, A.; Landais, P.; et al. Retinal hemangioblastomas in von Hippel-Lindau disease: A clinical and molecular study. Investig. Ophthalmol. Vis. Sci. 2002, 43, 3067–3074. [Google Scholar]
| VHL Patients | Controls | p Value | |
|---|---|---|---|
| Subjects, (number) | 63 | 28 | |
| Mean age (years: mean, SD) | 40.5, 14.4 | 40.0, 11.8 | 0.8824 |
| Female:Male (number, %) | 36:27, 57.1:42.9 | 17:11, 60.7:39.3 | 0.7498 |
| BCVA (letters: mean, SD) | 84.4, 8.4 | 87.8, 3.7 | 0.0003 |
| Peripheral RH (number, %) | |||
| Present | 36, 57 | - | - |
| Absent | 27, 43 | - | - |
| Subjects | VHL Patients | Controls | p Value |
|---|---|---|---|
| (number, %) | (63, 69.2) | (28, 30.7) | |
| CRT (mm: mean ± SD) | 273.9 ±17.5 | 272.7 ±18.0 | 0.8194 |
| FAZ (mm2: mean ± SD) | 0.30 ± 0.11 | 0.32 ± 0.09 | 0.3637 |
| VAD (mean ± SD) | |||
| SVP | 0.3476 ± 0.07 | 0.3685 ± 0.06 | 0.0368 |
| ICP | 0.1517 ± 0.03 | 0.1653 ± 0.03 | 0.1536 |
| DCP | 0.1905 ± 0.04 | 0.2067 ± 0.05 | 0.0942 |
| VLF (mean ± SD) | |||
| SVP | 0.0789 ± 0.01 | 0.0815 ± 0.01 | 0.2476 |
| ICP | 0.0497 ± 0.01 | 0.0528 ± 0.01 | 0.1824 |
| DCP | 0.0589 ± 0.01 | 0.0622 ± 0.01 | 0.1462 |
| VDI (mean ± SD) | |||
| SVP | 4.4038 ± 0.23 | 4.5237 ± 0.24 | 0.0012 |
| ICP | 3.0218 ± 0.16 | 3.1087 ± 0.14 | 0.0159 |
| DCP | 3.2056 ± 0.17 | 3.2931 ± 0.16 | 0.0153 |
| FDbin (mean ± SD) | |||
| SVP | 1.7470 ± 0.07 | 1.7655 ± 0.05 | 0.1659 |
| ICP | 1.5546 ± 0.08 | 1.5761 ± 0.07 | 0.1160 |
| DCP | 1.6190 ± 0.07 | 1.6367 ± 0.08 | 0.1819 |
| FDsk (mean ± SD) | |||
| SVP | 1.5052 ± 0.07 | 1.5174 ± 0.05 | 0.2985 |
| ICP | 1.3795 ± 0.07 | 1.3957 ± 0.07 | 0.1883 |
| DCP | 1.4353 ± 0.06 | 1.4481 ± 0.07 | 0.2781 |
| VHL Eyes | With RHs | w/Out RHs | p Value |
|---|---|---|---|
| (number, %) | (42, 37.1) | (71, 62.8) | |
| BCVA (letters: mean ± SD) | 85.29 ± 2.08 | 85.01 ± 2.60 | 0.1809 |
| CRT (m: mean ± SD) | 273.8 ± 18.5 | 273.9 ± 17.0 | 0.3011 |
| FAZ (mm2: mean ± SD) | 0.31 ± 0.12 | 0.29 ± 0.10 | 0.1302 |
| VAD (mean ± SD) | |||
| SVP | 0.3486 ± 0.06 | 0.3470 ± 0.08 | 0.9510 |
| ICP | 0.1503 ± 0.03 | 0.1526 ± 0.03 | 0.6872 |
| DCP | 0.1838 ± 0.04 | 0.1945 ± 0.04 | 0.1661 |
| VLF (mean ± SD) | |||
| SVP | 0.0789 ± 0.01 | 0.0789 ± 0.01 | 0.9245 |
| ICP | 0.0492 ± 0.01 | 0.0501 ± 0.01 | 0.7261 |
| DCP | 0.0570 ± 0.01 | 0.0600 ± 0.01 | 0.1626 |
| VDI (mean ± SD) | |||
| SVP | 4.4188 ± 0.27 | 4.3948 ± 0.21 | 0.7534 |
| ICP | 3.0259 ± 0.17 | 3.0194 ± 0.16 | 0.8362 |
| DCP | 3.1962 ± 0.17 | 3.2113 ± 0.16 | 0.3958 |
| FDbin (mean ± SD) | |||
| SVP | 1.7520 ± 0.05 | 1.7440 ± 0.08 | 0.7727 |
| ICP | 1.5527 ± 0.07 | 1.5558 ± 0.08 | 0.4647 |
| DCP | 1.6109 ± 0.06 | 1.6239 ± 0.08 | 0.1018 |
| FDsk (mean ± SD) | |||
| SVP | 1.5096 ± 0.05 | 1.5026 ± 0.08 | 0.7254 |
| ICP | 1.3774 ± 0.06 | 1.3807 ± 0.07 | 0.5236 |
| DCP | 1.4277 ± 0.05 | 1.4399 ± 0.07 | 0.1346 |
| VHL Patients | Eyes with RHs | Fellow Eyes | p Value |
|---|---|---|---|
| (16 cases) | |||
| BCVA (letters: mean ± SD) | 85.31 ± 1.74 | 85.75 ± 2.70 | 0.2760 |
| CRT (m: mean ± SD) | 275.1 ± 17.7 | 277.0 ± 19.4 | 0.3669 |
| FAZ (mm2: mean ± SD) | 0.31 ± 0.14 | 0.32 ± 0.13 | 0.3313 |
| VAD (mean ± SD) | |||
| SVP | 0.3193 ± 0.07 | 0.3378 ± 0.06 | 0.0770 |
| ICP | 0.1375 ± 0.04 | 0.1423 ± 0.03 | 0.6418 |
| DCP | 0.1858 ± 0.06 | 0.1819 ± 0.05 | 0.7066 |
| VLF (mean ± SD) | |||
| SVP | 0.0726 ± 0.01 | 0.0768 ± 0.01 | 0.1212 |
| ICP | 0.0456 ± 0.01 | 0.0469 ± 0.01 | 0.6249 |
| DCP | 0.0577 ± 0.01 | 0.0566 ± 0.01 | 0.6756 |
| VDI (mean ± SD) | |||
| SVP | 4.4038 ± 0.24 | 4.4056 ± 0.22 | 0.9734 |
| ICP | 2.9578 ± 0.21 | 2.9974 ± 0.19 | 0.4550 |
| DCP | 3.1718 ± 0.21 | 3.1811 ± 0.17 | 0.8612 |
| FDbin (mean ± SD) | |||
| SVP | 1.7207 ± 0.07 | 1.7420 ± 0.05 | 0.1678 |
| ICP | 1.5170 ± 0.11 | 1.5340 ± 0.08 | 0.2715 |
| DCP | 1.6082 ± 0.08 | 1.6037 ± 0.08 | 0.7724 |
| FDsk (mean ± SD) | |||
| SVP | 1.4787 ± 0.07 | 1.4993 ± 0.05 | 0.1626 |
| ICP | 1.3467 ± 0.09 | 1.3599 ± 0.07 | 0.3695 |
| DCP | 1.4266 ± 0.07 | 1.4210 ± 0.07 | 0.7002 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pilotto, E.; Nacci, E.B.; Ferrara, A.M.; De Mojà, G.; Zovato, S.; Midena, E. Macular Perfusion Impairment in Von Hippel-Lindau Disease Suggests a Generalized Retinal Vessel Alteration. J. Clin. Med. 2020, 9, 2677. https://doi.org/10.3390/jcm9082677
Pilotto E, Nacci EB, Ferrara AM, De Mojà G, Zovato S, Midena E. Macular Perfusion Impairment in Von Hippel-Lindau Disease Suggests a Generalized Retinal Vessel Alteration. Journal of Clinical Medicine. 2020; 9(8):2677. https://doi.org/10.3390/jcm9082677
Chicago/Turabian StylePilotto, Elisabetta, Elisabetta Beatrice Nacci, Alfonso Massimiliano Ferrara, Gilda De Mojà, Stefania Zovato, and Edoardo Midena. 2020. "Macular Perfusion Impairment in Von Hippel-Lindau Disease Suggests a Generalized Retinal Vessel Alteration" Journal of Clinical Medicine 9, no. 8: 2677. https://doi.org/10.3390/jcm9082677




