Evaluation of the Reliability, Reproducibility and Validity of Digital Orthodontic Measurements Based on Various Digital Models among Young Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients Inclusion Criteria and Group Classification
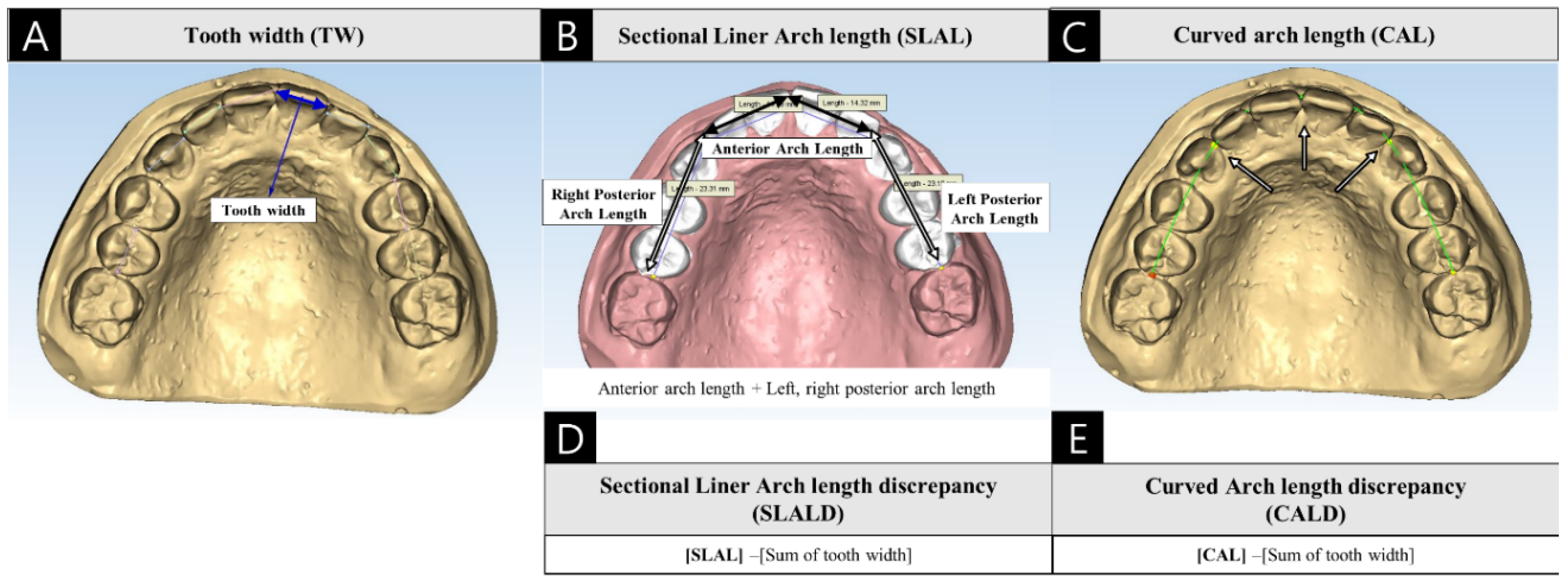
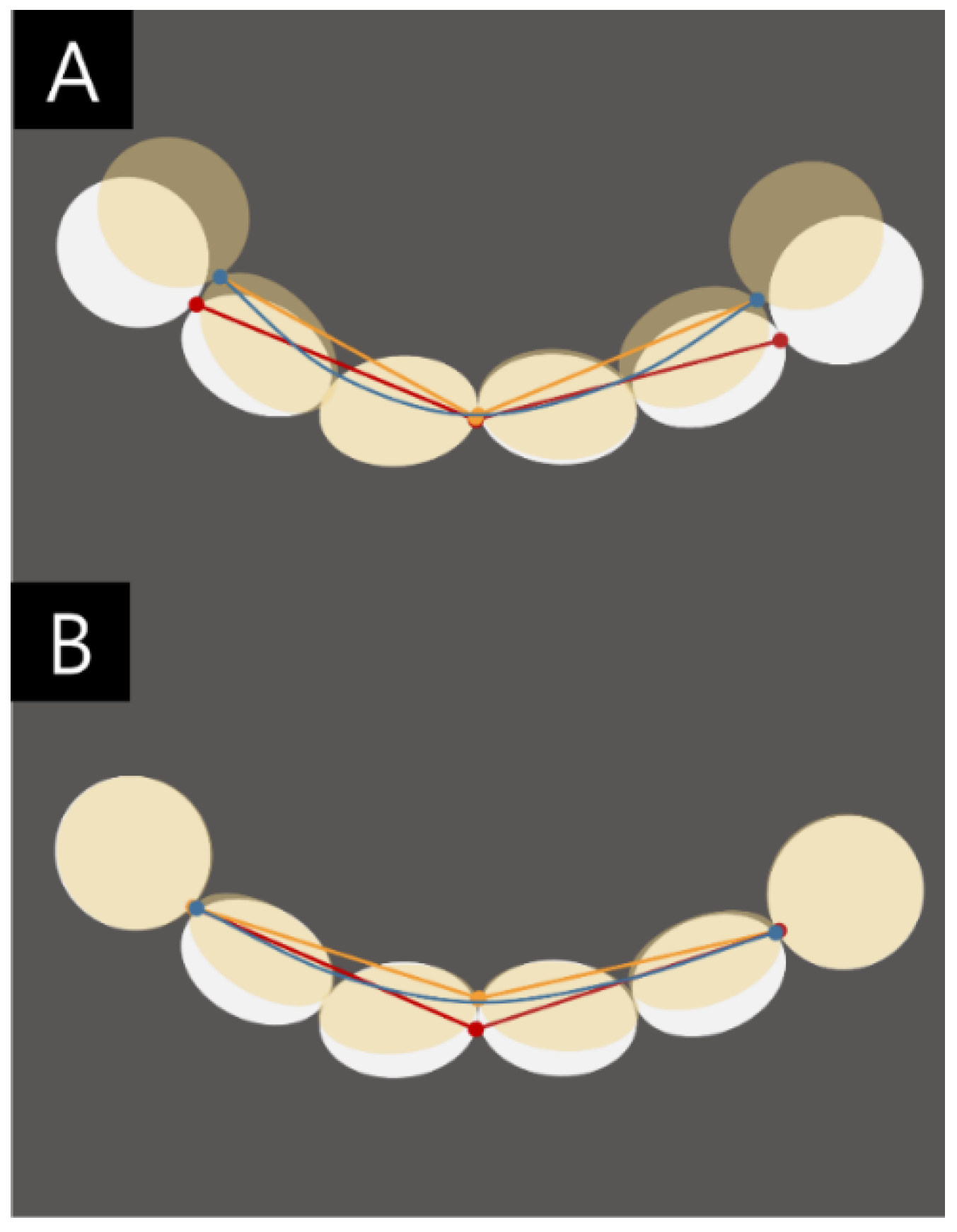
2.2. Orthodontic Measurements
2.3. Statistical Methods
3. Results
3.1. Reliability
3.2. Reproducibility
3.3. Validity
3.4. Validity of the Space Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Richter, A.E.; Arruda, A.O.; Peters, M.C.; Sohn, W. Incidence of caries lesions among patients treated with comprehensive orthodontics. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Crosby, D.R.; Alexander, C.G. The occurrence of tooth size discrepancies among different malocclusion groups. Am. J. Orthod. Dentofac. Orthop. 1989, 95, 457–461. [Google Scholar] [CrossRef]
- Schirmer, U.R.; Wiltshire, W.A. Manual and computer-aided space analysis: A comparative study. Am. J. Orthod. Dentofac. Orthop. 1997, 112, 676–680. [Google Scholar] [CrossRef]
- Motohashi, N.; Kuroda, T. A 3D computer-aided design system applied to diagnosis and treatment planning in orthodontics and orthognathic surgery. Eur. J. Orthod. 1999, 21, 263–274. [Google Scholar] [CrossRef] [PubMed]
- Zilberman, O.; Huggare, J.A.; Parikakis, K.A. Evaluation of the validity of tooth size and arch width measurements using conventional and three-dimensional virtual orthodontic models. Angle Orthod. 2003, 73, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Fleming, P.S.; Marinho, V.; Johal, A. Orthodontic measurements on digital study models compared with plaster models: A systematic review. Orthod. Craniofac. Res. 2011, 14, 1–16. [Google Scholar] [CrossRef]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Diagnostic accuracy and measurement sensitivity of digital models for orthodontic purposes: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 161–170. [Google Scholar] [CrossRef]
- Santoro, M.; Galkin, S.; Teredesai, M.; Nicolay, O.F.; Cangialosi, T.J. Comparison of measurements made on digital and plaster models. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 101–105. [Google Scholar] [CrossRef]
- Stevens, D.R.; Flores-Mir, C.; Nebbe, B.; Raboud, D.W.; Heo, G.; Major, P.W. Validity, reliability, and reproducibility of plaster vs digital study models: Comparison of peer assessment rating and Bolton analysis and their constituent measurements. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 794–803. [Google Scholar] [CrossRef]
- Tomassetti, J.J.; Taloumis, L.J.; Denny, J.M.; Fischer, J.R., Jr. A comparison of 3 computerized Bolton tooth-size analyses with a commonly used method. Angle Orthod. 2001, 71, 351–357. [Google Scholar] [CrossRef]
- Mullen, S.R.; Martin, C.A.; Ngan, P.; Gladwin, M. Accuracy of space analysis with emodels and plaster models. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Jeong, I.D.; Lee, J.J.; Jeon, J.H.; Kim, J.H.; Kim, H.Y.; Kim, W.C. Accuracy of complete-arch model using an intraoral video scanner: An in vitro study. J. Prosthet. Dent. 2016, 115, 755–759. [Google Scholar] [CrossRef] [PubMed]
- Malik, J.; Rodriguez, J.; Weisbloom, M.; Petridis, H. Comparison of Accuracy between a Conventional and Two Digital Intraoral Impression Techniques. Int. J. Prosthodont. 2018, 31, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Kihara, H.; Hatakeyama, W.; Komine, F.; Takafuji, K.; Takahashi, T.; Yokota, J.; Oriso, K.; Kondo, H. Accuracy and practicality of intraoral scanner in dentistry: A literature review. J. Prosthodont. Res. 2019. [Google Scholar] [CrossRef] [PubMed]
- An, X.; Yang, H.W.; Choi, B.H. Digital Workflow for Computer-Guided Implant Surgery in Edentulous Patients with an Intraoral Scanner and Old Complete Denture. J. Prosthodont. 2019, 28, 715–718. [Google Scholar] [CrossRef]
- Resnick, C.M.; Doyle, M.; Calabrese, C.E.; Sanchez, K.; Padwa, B.L. Is It Cost Effective to Add an Intraoral Scanner to an Oral and Maxillofacial Surgery Practice? J. Oral Maxillofac. Surg. 2019, 77, 1687–1694. [Google Scholar] [CrossRef]
- Grunheid, T.; McCarthy, S.D.; Larson, B.E. Clinical use of a direct chairside oral scanner: An assessment of accuracy, time, and patient acceptance. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 673–682. [Google Scholar] [CrossRef]
- Goracci, C.; Franchi, L.; Vichi, A.; Ferrari, M. Accuracy, reliability, and efficiency of intraoral scanners for full-arch impressions: A systematic review of the clinical evidence. Eur. J. Orthod. 2016, 38, 422–428. [Google Scholar] [CrossRef]
- Camardella, L.T.; Breuning, H.; de Vasconcellos Vilella, O. Accuracy and reproducibility of measurements on plaster models and digital models created using an intraoral scanner. J. Orofac. Orthop. 2017, 78, 211–220. [Google Scholar] [CrossRef]
- Sfondrini, M.F.; Gandini, P.; Malfatto, M.; Di Corato, F.; Trovati, F.; Scribante, A. Computerized Casts for Orthodontic Purpose Using Powder-Free Intraoral Scanners: Accuracy, Execution Time, and Patient Feedback. Biomed. Res. Int. 2018, 2018, 4103232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomita, Y.; Uechi, J.; Konno, M.; Sasamoto, S.; Iijima, M.; Mizoguchi, I. Accuracy of digital models generated by conventional impression/plaster-model methods and intraoral scanning. Dent. Mater. J. 2018, 37, 628–633. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ender, A.; Attin, T.; Mehl, A. In vivo precision of conventional and digital methods of obtaining complete-arch dental impressions. J. Prosthet. Dent. 2016, 115, 313–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, F.; Suh, K.J.; Lee, K.M. Validity of Intraoral Scans Compared with Plaster Models: An In-Vivo Comparison of Dental Measurements and 3D Surface Analysis. PLoS ONE 2016, 11, e0157713. [Google Scholar] [CrossRef] [PubMed]
- Nedelcu, R.; Olsson, P.; Nystrom, I.; Ryden, J.; Thor, A. Accuracy and precision of 3 intraoral scanners and accuracy of conventional impressions: A novel in vivo analysis method. J. Dent. 2018, 69, 110–118. [Google Scholar] [CrossRef]
- Sun, L.; Lee, J.S.; Choo, H.H.; Hwang, H.S.; Lee, K.M. Reproducibility of an intraoral scanner: A comparison between in-vivo and ex-vivo scans. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 305–310. [Google Scholar] [CrossRef] [Green Version]
- Jimenez-Gayosso, S.I.; Lara-Carrillo, E.; Lopez-Gonzalez, S.; Medina-Solis, C.E.; Scougall-Vilchis, R.J.; Hernandez-Martinez, C.T.; Colome-Ruiz, G.E.; Escoffie-Ramirez, M. Difference between manual and digital measurements of dental arches of orthodontic patients. Medicine 2018, 97, e10887. [Google Scholar] [CrossRef]
- Burhardt, L.; Livas, C.; Kerdijk, W.; van der Meer, W.J.; Ren, Y. Treatment comfort, time perception, and preference for conventional and digital impression techniques: A comparative study in young patients. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 261–267. [Google Scholar] [CrossRef]
- Mangano, A.; Beretta, M.; Luongo, G.; Mangano, C.; Mangano, F. Conventional Vs Digital Impressions: Acceptability, Treatment Comfort and Stress Among Young Orthodontic Patients. Open Dent. J. 2018, 12, 118–124. [Google Scholar] [CrossRef] [Green Version]
- Ting-Shu, S.; Jian, S. Intraoral Digital Impression Technique: A Review. J. Prosthodont. 2015, 24, 313–321. [Google Scholar] [CrossRef]
- Kim, E.-J.; Hwang, H.-S. Reproducibility and accuracy of tooth size measurements obtained by the use of computer. Korean J. Orthod. 1998, 29, 563–573. [Google Scholar]
- Flugge, T.V.; Schlager, S.; Nelson, K.; Nahles, S.; Metzger, M.C. Precision of intraoral digital dental impressions with iTero and extraoral digitization with the iTero and a model scanner. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Gul Amuk, N.; Karsli, E.; Kurt, G. Comparison of dental measurements between conventional plaster models, digital models obtained by impression scanning and plaster model scanning. Int. Orthod. 2019, 17, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Muallah, J.; Wesemann, C.; Nowak, R.; Robben, J.; Mah, J.; Pospiech, P.; Bumann, A. Accuracy of full-arch scans using intraoral and extraoral scanners: An in vitro study using a new method of evaluation. Int. J. Comput. Dent. 2017, 20, 151–164. [Google Scholar] [PubMed]
- Muller, P.; Ender, A.; Joda, T.; Katsoulis, J. Impact of digital intraoral scan strategies on the impression accuracy using the TRIOS Pod scanner. Quintessence Int. 2016, 47, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Shahen, S.; Carrino, G.; Carrino, R.; Abdelsalam, R.; Flores-Mir, C.; Perillo, L. Palatal volume and area assessment on digital casts generated from cone-beam computed tomography scans. Angle Orthod. 2018, 88, 397–402. [Google Scholar] [CrossRef] [Green Version]


| Verification | p-MSD | P-ISD | Verification | P-MSD | P-ISD | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | p Value | Mean | SD | p Value | Mean | SD | p Value | Mean | SD | p Value | ||
| #15 | −0.088 | 0.223 | 0.000 *** | −0.096 | 0.297 | 0.001 ** | #35 | −0.061 | 0.251 | 0.009 ** | −0.017 | 0.312 | 0.542 |
| #14 | −0.123 | 0.250 | 0.000 *** | −0.105 | 0.296 | 0.000 *** | #34 | 0.001 | 0.218 | 0.947 | 0.020 | 0.264 | 0.418 |
| #13 | −0.075 | 0.222 | 0.000 *** | 0.078 | 0.293 | 0.004 ** | #33 | 0.001 | 0.265 | 0.959 | 0.035 | 0.319 | 0.227 |
| #12 | −0.042 | 0.216 | 0.037 * | −0.007 | 0.231 | 0.747 | #32 | −0.034 | 0.196 | 0.056 | −0.033 | 0.197 | 0.070 |
| #11 | −0.023 | 0.197 | 0.207 | 0.028 | 0.317 | 0.340 | #31 | −0.061 | 0.200 | 0.001 *** | −0.008 | 0.268 | 0.731 |
| #21 | −0.033 | 0.226 | 0.116 | −0.011 | 0.254 | 0.358 | #41 | −0.063 | 0.202 | 0.001 *** | −0.026 | 0.222 | 0.201 |
| #22 | −0.034 | 0.258 | 0.150 | 0.002 | 0.282 | 0.954 | #42 | −0.039 | 0.242 | 0.082 | −0.008 | 0.264 | 0.751 |
| #23 | −0.040 | 0.239 | 0.068 | −0.056 | 0.270 | 0.024 * | #43 | −0.070 | 0.278 | 0.007 ** | −0.032 | 0.342 | 0.310 |
| #24 | −0.107 | 0.226 | 0.000 *** | −0.106 | 0.251 | 0.000 *** | #44 | −0.062 | 0.225 | 0.003 ** | −0.056 | 0.280 | 0.032 * |
| #25 | −0.086 | 0.255 | 0.000 *** | 0.060 | 0.271 | 0.008 ** | #45 | −0.070 | 0.260 | 0.004 ** | −0.029 | 0.275 | 0.259 |
| Maxilla | Mandible | ||||||||||||
| AAL | 0.013 | 1.244 | 0.908 | 0.389 | 1.497 | 0.005 ** | AAL | 0.060 | 1.055 | 0.535 | 0.270 | 1.046 | 0.006 ** |
| LAL | −0.204 | 0.882 | 0.013 * | 0.076 | 1.094 | 0.451 | LAL | −0.136 | 0.832 | 0.015 * | 0.133 | 1.178 | 0.219 |
| RAL | −0.209 | 1.119 | 0.043 * | 0.045 | 1.085 | 0.146 | RAL | −0.160 | 0.730 | 0.018 * | 0.120 | 0.844 | 0.121 |
| P-MSD | P-ISD | P-MSD | P-ISD | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | p Value | Mean | SD | p Value | Mean | SD | p Value | Mean | SD | p Value | ||
| Maxilla | Mandible | ||||||||||||
| SLAL | −0.399 | 2.328 | 0.063 | 0.519 | 2.695 | 0.000 * | SLAL | −0.236 | 1.641 | 0.118 | 0.523 | 2.070 | 0.007 * |
| CAL | −0.755 | 2.113 | 0.000 * | 0.022 | 1.695 | 0.059 | CAL | −0.649 | 2.013 | 0.000 * | −0.173 | 1.887 | 0.067 |
| RS | −0.649 | 1.120 | 0.000 * | −0.233 | 1.234 | 0.197 | RS | −0.456 | 1.191 | 0.000 * | −0.153 | 1.351 | 0.216 |
| SLALD | 0.250 | 2.410 | 0.257 | 0.752 | 3.084 | 0.009 * | SLALD | 0.221 | 1.789 | 0.179 | 0.676 | 2.390 | 0.002 * |
| CALD | −0.106 | 2.998 | 0.321 | 0.255 | 2.929 | 0.117 | CALD | 0.193 | 2.410 | 0.257 | −0.040 | 1.084 | 0.718 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, S.-H.; Byun, S.-H.; Oh, S.-H.; Lee, H.-L.; Kim, J.-W.; Yang, B.-E.; Park, I.-Y. Evaluation of the Reliability, Reproducibility and Validity of Digital Orthodontic Measurements Based on Various Digital Models among Young Patients. J. Clin. Med. 2020, 9, 2728. https://doi.org/10.3390/jcm9092728
Park S-H, Byun S-H, Oh S-H, Lee H-L, Kim J-W, Yang B-E, Park I-Y. Evaluation of the Reliability, Reproducibility and Validity of Digital Orthodontic Measurements Based on Various Digital Models among Young Patients. Journal of Clinical Medicine. 2020; 9(9):2728. https://doi.org/10.3390/jcm9092728
Chicago/Turabian StylePark, Seo-Hyun, Soo-Hwan Byun, So-Hee Oh, Hye-Lim Lee, Ju-Won Kim, Byoung-Eun Yang, and In-Young Park. 2020. "Evaluation of the Reliability, Reproducibility and Validity of Digital Orthodontic Measurements Based on Various Digital Models among Young Patients" Journal of Clinical Medicine 9, no. 9: 2728. https://doi.org/10.3390/jcm9092728





