Children’s Dental Anxiety during the COVID-19 Pandemic: Polish Experience
Abstract
:1. Introduction
2. Experimental Section
2.1. Study Design
- To limit the direct time of the visit, medical history was taken via phone or online call.
- Children’s caregivers were informed about new safety regulations and measures employed by the dental clinic, and about additional safety measures.
- Before the appointment, all caregivers were advised to explain the safety measures to children and show them a picture of dental staff in PPE to make them more familiar with the situation.
- The body temperature of each child and caregiver was measured at the entrance to the waiting room.
- Each child and caregiver was instructed to disinfect hands in the waiting room.
- Only one adult caregiver was allowed to accompany a child during the visit to the dental office.
- In the case of all appointments, two professionals (a dentist and assistant) were maximally present in the dental office.
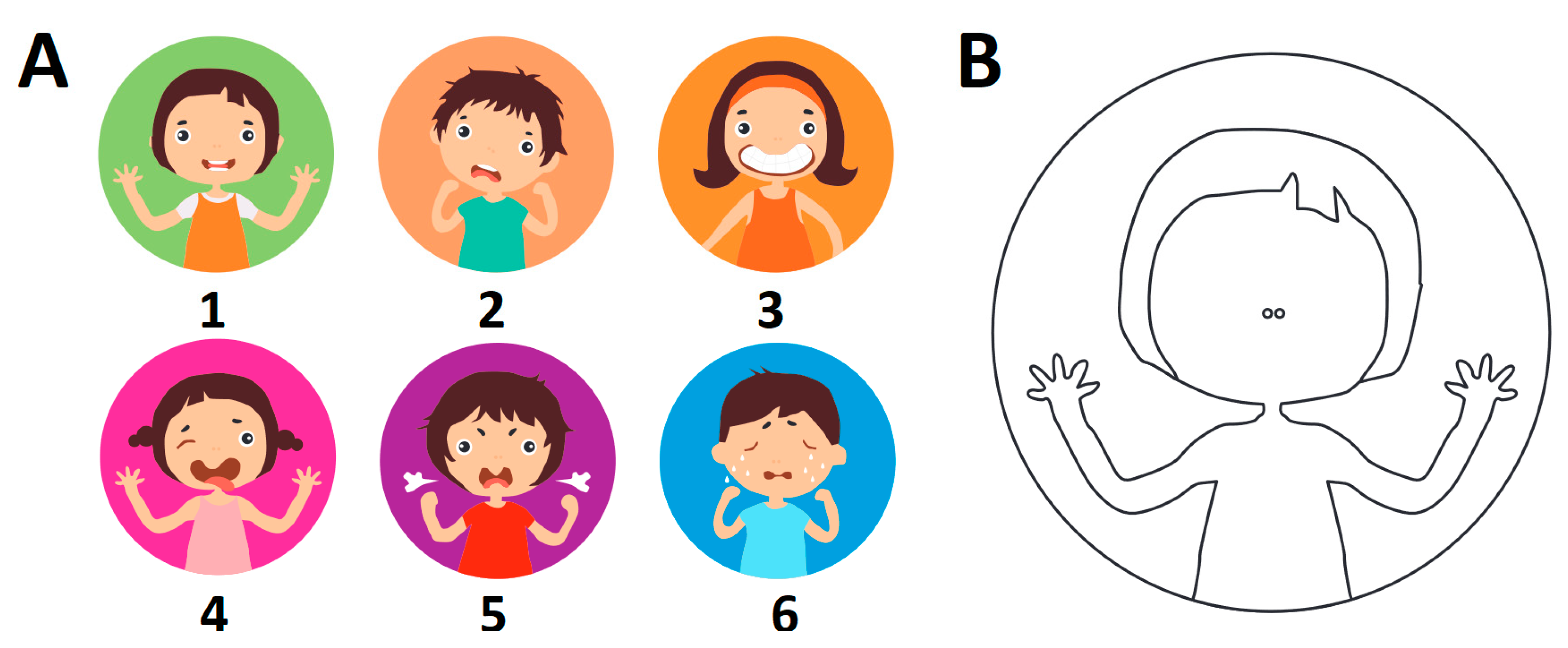
2.2. Emotional State Evaluation
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Bio-Med. Atenei Parm. 2020, 91, 157–160. [Google Scholar] [CrossRef]
- Bogoch, I.I.; Watts, A.; Thomas-Bachli, A.; Huber, C.; Kraemer, M.U.G.; Khan, K. Pneumonia of unknown aetiology in Wuhan, China: Potential for international spread via commercial air travel. J. Travel Med. 2020, 27. [Google Scholar] [CrossRef]
- Magro, F.; Perazzo, P.; Bottinelli, E.; Possenti, F.; Banfi, G. Managing a Tertiary Orthopedic Hospital during the COVID-19 Epidemic, Main Challenges and Solutions Adopted. Int. J. Environ. Res. Public Health 2020, 17, 4818. [Google Scholar] [CrossRef]
- Wang, N.C.; Jain, S.K.; Estes, N.A.M., III; Barrington, W.W.; Bazaz, R.; Bhonsale, A.; Kancharla, K.; Shalaby, A.A.; Voigt, A.H.; Saba, S. Priority plan for invasive cardiac electrophysiology procedures during the coronavirus disease 2019 (COVID-19) pandemic. J. Cardiovasc. Electrophysiol. 2020, 31, 1255–1258. [Google Scholar] [CrossRef]
- Pinheiro, R.N.; Coimbra, F.J.F.; Costa, W.L.D., Jr.; Ribeiro, H.S.D.C.; Ribeiro, R.; Wainstein, A.J.A.; Laporte, G.A.; Coelho, M.J.P., Jr.; Fernandes, P.H.D.S.; Cordeiro, E.Z.; et al. Surgical cancer care in the COVID-19 era: Front line views and consensus. Rev. Colégio Bras. Cir. 2020, 47. [Google Scholar] [CrossRef]
- Coulthard, P. Dentistry and coronavirus (COVID-19)—Moral decision-making. Br. Dent. J. 2020, 228, 503–505. [Google Scholar] [CrossRef]
- Bizzoca, M.E.; Campisi, G.; Lo Muzio, L. Covid-19 Pandemic: What Changes for Dentists and Oral Medicine Experts? A Narrative Review and Novel Approaches to Infection Containment. Int. J. Environ. Res. Public Health 2020, 17, 3793. [Google Scholar] [CrossRef]
- Rzymski, P.; Nowicki, M. COVID-19-related prejudice toward Asian medical students: A consequence of SARS-CoV-2 fears in Poland. J. Infect. Public Health 2020, 13, 873–876. [Google Scholar] [CrossRef]
- Shimizu, K. 2019-nCoV, fake news, and racism. Lancet 2020, 395, 685–686. [Google Scholar] [CrossRef]
- Orso, D.; Federici, N.; Copetti, R.; Vetrugno, L.; Bove, T. Infodemic and the spread of fake news in the COVID-19-era. Eur. J. Emerg. Med. 2020. [Google Scholar] [CrossRef]
- Sidor, A.; Rzymski, P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Fontanesi, L.; Marchetti, D.; Mazza, C.; Di Giandomenico, S.; Roma, P.; Verrocchio, M.C. The effect of the COVID-19 lockdown on parents: A call to adopt urgent measures. Psychol. Trauma Theory Res. Pract. Policy 2020. [Google Scholar] [CrossRef]
- Thakur, K.; Kumar, N.; Sharma, N. Effect of the Pandemic and Lockdown on Mental Health of Children. Indian J. Pediatr. 2020, 87, 552. [Google Scholar] [CrossRef]
- Clemens, V.; Deschamps, P.; Fegert, J.M.; Anagnostopoulos, D.; Bailey, S.; Doyle, M.; Eliez, S.; Hansen, A.S.; Hebebrand, J.; Hillegers, M.; et al. Potential effects of “social” distancing measures and school lockdown on child and adolescent mental health. Eur. Child Adolesc. Psychiatry 2020, 29, 739–742. [Google Scholar] [CrossRef]
- Fegert, J.M.; Vitiello, B.; Plener, P.L.; Clemens, V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child. Adolesc. Psychiatry Ment. Health 2020, 14, 20. [Google Scholar] [CrossRef]
- Peloso, R.M.; Pini, N.I.P.; Sunfeld Neto, D.; Mori, A.A.; Oliveira, R.C.G.d.; Valarelli, F.P.; Freitas, K.M.S. How does the quarantine resulting from COVID-19 impact dental appointments and patient anxiety levels? Braz. Oral Res. 2020, 34. [Google Scholar] [CrossRef]
- Pisano, L.; Galimi, D.; Cerniglia, L. A qualitative report on exploratory data on the possible emotional/behavioral correlates of Covid-19 lockdown in 4-10 years children in Italy. Psyarxiv 2020. [Google Scholar] [CrossRef]
- Dalton, L.; Rapa, E.; Ziebland, S.; Rochat, T.; Kelly, B.; Hanington, L.; Bland, R.; Yousafzai, A.; Stein, A. Communication with children and adolescents about the diagnosis of a life-threatening condition in their parent. Lancet 2019, 393, 1164–1176. [Google Scholar] [CrossRef]
- Dalton, L.; Rapa, E.; Stein, A. Protecting the psychological health of children through effective communication about COVID-19. Lancet Child. Adolesc. Health 2020, 4, 346–347. [Google Scholar] [CrossRef]
- Spinelli, M.; Lionetti, F.; Pastore, M.; Fasolo, M. Parents’ Stress and Children’s Psychological Problems in Families Facing the COVID-19 Outbreak in Italy. Front. Psychol. 2020, 11. [Google Scholar] [CrossRef]
- Dahlander, A.; Soares, F.; Grindefjord, M.; Dahllöf, G. Factors Associated with Dental Fear and Anxiety in Children Aged 7 to 9 Years. Dent. J. 2019, 7, 68. [Google Scholar] [CrossRef] [Green Version]
- Wong, M.L.W.; Lai, S.H.F.; Wong, H.M.; Yang, Y.X.; Yiu, C.K.Y. Dental anxiety in Hong Kong preschool children: Prevalence and associated factors. Adv. Pediatric Res. 2017, 4, 1. [Google Scholar] [CrossRef] [Green Version]
- Siegel, K.; Schrimshaw, E.W.; Kunzel, C.; Wolfson, N.H.; Moon-Howard, J.; Moats, H.L.; Mitchell, D.A. Types of dental fear as barriers to dental care among African American adults with oral health symptoms in Harlem. J. Health Care Poor Underserved 2012, 23, 1294–1309. [Google Scholar] [CrossRef] [Green Version]
- Armfield, J.M.; Heaton, L.J. Management of fear and anxiety in the dental clinic: A review. Aust. Dent. J. 2013, 58, 390–407. [Google Scholar] [CrossRef]
- Appukuttan, D.P. Strategies to manage patients with dental anxiety and dental phobia: Literature review. Clin. Cosmet. Investig. Dent. 2016, 8, 35–50. [Google Scholar] [CrossRef] [Green Version]
- Dou, L.; Vanschaayk, M.M.; Zhang, Y.; Fu, X.; Ji, P.; Yang, D. The prevalence of dental anxiety and its association with pain and other variables among adult patients with irreversible pulpitis. BMC Oral Health 2018, 18, 101. [Google Scholar] [CrossRef]
- Townsend, J.A.; Wells, M.H. 24—Behavior Guidance of the Pediatric Dental Patient. In Pediatric Dentistry, 6th ed.; Nowak, A.J., Christensen, J.R., Mabry, T.R., Townsend, J.A., Wells, M.H., Eds.; Content Repository: Philadelphia, PA, USA, 2019; pp. 352–370. [Google Scholar] [CrossRef]
- Ahmed, M.A.; Jouhar, R.; Ahmed, N.; Adnan, S.; Aftab, M.; Zafar, M.S.; Khurshid, Z. Fear and Practice Modifications among Dentists to Combat Novel Coronavirus Disease (COVID-19) Outbreak. Int. J. Environ. Res. Public Health 2020, 17, 2821. [Google Scholar] [CrossRef]
- Mahendran, K.; Patel, S.; Sproat, C. Psychosocial effects of the COVID-19 pandemic on staff in a dental teaching hospital. Br. Dent. J. 2020, 229, 127–132. [Google Scholar] [CrossRef]
- Ekman, P.; Friesen, W.V. Facial Action Coding System: A Technique for the Measurement of Facial Movement; Consulting Psychologists Press: Palo Alto, CA, USA, 1978; Volume 3. [Google Scholar]
- Sattler, J.M. Assessment of Children: Behavioral and Clinical Applications, 4th ed.; Jerome M. Sattler: La Mesa, CA, USA, 2002; p. 620. [Google Scholar]
- Goodenough, B.; Piira, T.; Baeyer, C.L.V.; Chua, K.S.G.; Trieu, J.; Champion, G.D. Comparing six self-report measures of pain intensity in children. Suff. Child. 2005, 8, 1–25. [Google Scholar]
- Keck, J.F.; Gerkensmeyer, J.E.; Joyce, B.A.; Schade, J.G. Reliability and validity of the faces and word descriptor scales to measure procedural pain. J. Pediatric Nurs. 1996, 11, 368–374. [Google Scholar] [CrossRef]
- Ryan, R.; O’Farrelly, C.; Ramchandani, P. Parenting and child mental health. Lond. J. Prim. Care 2017, 9, 86–94. [Google Scholar] [CrossRef] [Green Version]
- Power, T.G. Stress and Coping in Childhood: The Parents’ Role. Parenting 2004, 4, 271–317. [Google Scholar] [CrossRef]
- Von Baeyer, C.L.; Forsyth, S.J.; Stanford, E.A.; Watson, M.; Chambers, C.T. Response biases in preschool children’s ratings of pain in hypothetical situations. Eur. J. Pain 2009, 13, 209–213. [Google Scholar] [CrossRef]
- Von Baeyer, C.L. Children’s self-report of pain intensity: What we know, where we are headed. Pain Res. Manag. 2009, 14, 39–45. [Google Scholar] [CrossRef]
- Boutelle, K.; Eisenberg, M.E.; Gregory, M.L.; Neumark-Sztainer, D. The reciprocal relationship between parent–child connectedness and adolescent emotional functioning over 5 years. J. Psychosom. Res. 2009, 66, 309–316. [Google Scholar] [CrossRef]
- Wu, L.; Gao, X. Children’s dental fear and anxiety: Exploring family related factors. BMC Oral Health 2018, 18, 100. [Google Scholar] [CrossRef] [Green Version]
- D’Alessandro, G.; Alkhamis, N.; Mattarozzi, K.; Mazzetti, M.; Piana, G. Fear of dental pain in Italian children: Child personality traits and parental dental fear. J. Public Health Dent. 2016, 76, 179–183. [Google Scholar] [CrossRef]
- Raj, S.; Agarwal, M.; Aradhya, K.; Konde, S.; Nagakishore, V. Evaluation of Dental Fear in Children during Dental Visit using Children’s Fear Survey Schedule-Dental Subscale. Int. J. Clin. Pediatr. Dent. 2013, 6, 12–15. [Google Scholar] [CrossRef]
- Carter, A.S.; Godoy, L.; Wagmiller, R.L.; Veliz, P.; Marakovitz, S.; Briggs-Gowan, M.J. Internalizing Trajectories in Young Boys and Girls: The Whole is Not a Simple Sum of its Parts. J. Abnorm. Child. Psychol. 2010, 38, 19–31. [Google Scholar] [CrossRef]
- Bleses, D.; Vach, W.; Slott, M.; Wehberg, S.; Thomsen, P.I.A.; Madsen, T.O.; BasbØLl, H. The Danish Communicative Developmental Inventories: Validity and main developmental trends. J. Child. Lang. 2008, 35, 651–669. [Google Scholar] [CrossRef]
- Huttenlocher, J.; Haight, W.; Bryk, A.; Seltzer, M.; Lyons, T. Early vocabulary growth: Relation to language input and gender. Dev. Psychol. 1991, 27, 236–248. [Google Scholar] [CrossRef]
- Maccoby, E.E. The Development of Sex. Differences; Stanford University Press: Palo Alto, CA, USA, 1966. [Google Scholar]
- Ramer, A.L.H. Syntactic styles in emerging language. J. Child. Lang. 2008, 3, 49–62. [Google Scholar] [CrossRef]
- Bowers, J.M.; Perez-Pouchoulen, M.; Edwards, N.S.; McCarthy, M.M. Foxp2 mediates sex differences in ultrasonic vocalization by rat pups and directs order of maternal retrieval. J. Neurosci. 2013, 33, 3276–3283. [Google Scholar] [CrossRef] [Green Version]
- Wheaton, M.G.; Abramowitz, J.S.; Berman, N.C.; Fabricant, L.E.; Olatunji, B.O. Psychological Predictors of Anxiety in Response to the H1N1 (Swine Flu) Pandemic. Cogn. Ther. Res. 2012, 36, 210–218. [Google Scholar] [CrossRef]
- Bults, M.; Beaujean, D.J.M.A.; de Zwart, O.; Kok, G.; van Empelen, P.; van Steenbergen, J.E.; Richardus, J.H.; Voeten, H.A.C.M. Perceived risk, anxiety, and behavioural responses of the general public during the early phase of the Influenza A (H1N1) pandemic in the Netherlands: Results of three consecutive online surveys. BMC Public Health 2011, 11, 2. [Google Scholar] [CrossRef] [Green Version]
- Everts, J. Announcing Swine Flu and the Interpretation of Pandemic Anxiety. Antipode 2013, 45, 809–825. [Google Scholar] [CrossRef]
- Fu, W.; Wang, C.; Zou, L.; Guo, Y.; Lu, Z.; Yan, S.; Mao, J. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Transl. Psychiatry 2020, 10, 225. [Google Scholar] [CrossRef]
- Petzold, M.B.; Bendau, A.; Plag, J.; Pyrkosch, L.; Mascarell Maricic, L.; Betzler, F.; Rogoll, J.; Große, J.; Ströhle, A. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain Behav. 2020, e01745. [Google Scholar] [CrossRef]
- Gualano, M.R.; Lo Moro, G.; Voglino, G.; Bert, F.; Siliquini, R. Effects of Covid-19 Lockdown on Mental Health and Sleep Disturbances in Italy. Int. J. Environ. Res. Public Health 2020, 17, 4779. [Google Scholar] [CrossRef]
- Majstorovic, M.; Morse, D.; Do, D.; Lim, L.; Herman, N.; Moursi, A. Indicators of Dental Anxiety in Children Just Prior to Treatment. J. Clin. Pediatric Dent. 2014, 39, 12–17. [Google Scholar] [CrossRef]
- Boynes, S.G.; Abdulwahab, M.; Kershner, E.; Mickens, F.; Riley, A. Analysis of parental factors and parent-child communication with pediatric patients referred for nitrous oxide administration in a rural community health center setting. Oral Biol. Dent. 2014, 2. [Google Scholar] [CrossRef]
- Themessl-Huber, M.; Freeman, R.; Humphris, G.; Macgillivray, S.; Terzi, N. Empirical evidence of the relationship between parental and child dental fear: A structured review and meta-analysis. Int. J. Paediatr. Dent. 2010, 20, 83–101. [Google Scholar] [CrossRef]
- Townend, E.; Dimigen, G.; Fung, D. A clinical study of child dental anxiety. Behav. Res. Ther. 2000, 38, 31–46. [Google Scholar] [CrossRef]
- Eli, I.; Uziel, N.; Baht, R.; Kleinhauz, M. Antecedents of dental anxiety: Learned responses versus personality traits. Community Dent. Oral Epidemiol. 1997, 25, 233–237. [Google Scholar] [CrossRef]
- Saheer, P.A.; Marriette, T.M.; Alappat, A.T.; Majid, S.A.; Hafiz, H.; Jamal, F.; Badar, N. Association of dental anxiety with personality traits among Al Azhar arts students in Thodupuzha, Kerala. J. Glob. Oral Health 2019, 1. [Google Scholar] [CrossRef]


| Group | Caregiver Evaluation | Children Evaluation | |
|---|---|---|---|
| Dentist evaluation | pre-pandemic | 0.88 | 0.59 |
| pandemic | 0.86 | 0.75 | |
| Caregivers evaluation | pre-pandemic | - | 0.79 |
| pandemic | - | 0.82 |
| Medical indication | Pandemic Group (n = 25) | Pre-pandemic Group (n = 20) |
|---|---|---|
| Tooth extraction (n/%) | 14/56 | 10/50 |
| Abscess treatment (n/%) | 5/20 | 1/5 |
| Mucosal lesion (n/%) | 1/4 | 2/10 |
| Pulp treatment (n/%) | 2/8 | 5/25 |
| Dental trauma (n/%) | 3/12 | 2/10 |
| Evaluation | Score | Boys | Girls | ||
|---|---|---|---|---|---|
| Pre-Pandemic (n = 10) | Pandemic (n = 15) | Pre-Pandemic (n = 10) | Pandemic (n = 10) | ||
| Dentist (%) | Lowest | 20.0 | 6.7 | 40.0 | 30.0 |
| Highest | 10.0 | 13.3 | 10.0 | 10.0 | |
| Caregiver (%) | Lowest | 10.0 | 6.7 | 20.0 | 20.0 |
| Highest | 10.0 | 20.0 | 10.0 | 10.0 | |
| Children (%) | Lowest | 40.0 | 13.3 | 40.0 | 40.0 |
| Highest | 10.0 | 13.3 | 10.0 | 10.0 | |
| Group | Dentist Evaluation | Caregiver Evaluation | Children Evaluation | |
|---|---|---|---|---|
| Age | Pandemic boys (n = 15) girls (n = 10) | −0.67 * −0.84 * −0.34 ns | −0.63 * −0.69 * 0.57 ns | −0.44 * −0.57 * −0.39 ns |
| Pre-pandemic boys (n = 10) girls (n = 10) | −0.25 ns −0.08 ns −0.38 ns | −0.40 ns −0.14 ns −0.69 * | −0.36 ns −0.32 ns −0.52 ns |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Olszewska, A.; Rzymski, P. Children’s Dental Anxiety during the COVID-19 Pandemic: Polish Experience. J. Clin. Med. 2020, 9, 2751. https://doi.org/10.3390/jcm9092751
Olszewska A, Rzymski P. Children’s Dental Anxiety during the COVID-19 Pandemic: Polish Experience. Journal of Clinical Medicine. 2020; 9(9):2751. https://doi.org/10.3390/jcm9092751
Chicago/Turabian StyleOlszewska, Aneta, and Piotr Rzymski. 2020. "Children’s Dental Anxiety during the COVID-19 Pandemic: Polish Experience" Journal of Clinical Medicine 9, no. 9: 2751. https://doi.org/10.3390/jcm9092751
APA StyleOlszewska, A., & Rzymski, P. (2020). Children’s Dental Anxiety during the COVID-19 Pandemic: Polish Experience. Journal of Clinical Medicine, 9(9), 2751. https://doi.org/10.3390/jcm9092751






