A Review on 3D-Printed Templates for Precontouring Fixation Plates in Orthopedic Surgery
Abstract
:1. Introduction
- −
- RQ1: What is the reported use of 3D-printed models for precontouring plates in orthopedic surgery? → Obj1. Presents a state of the art reference document through performing a systematic review.
- −
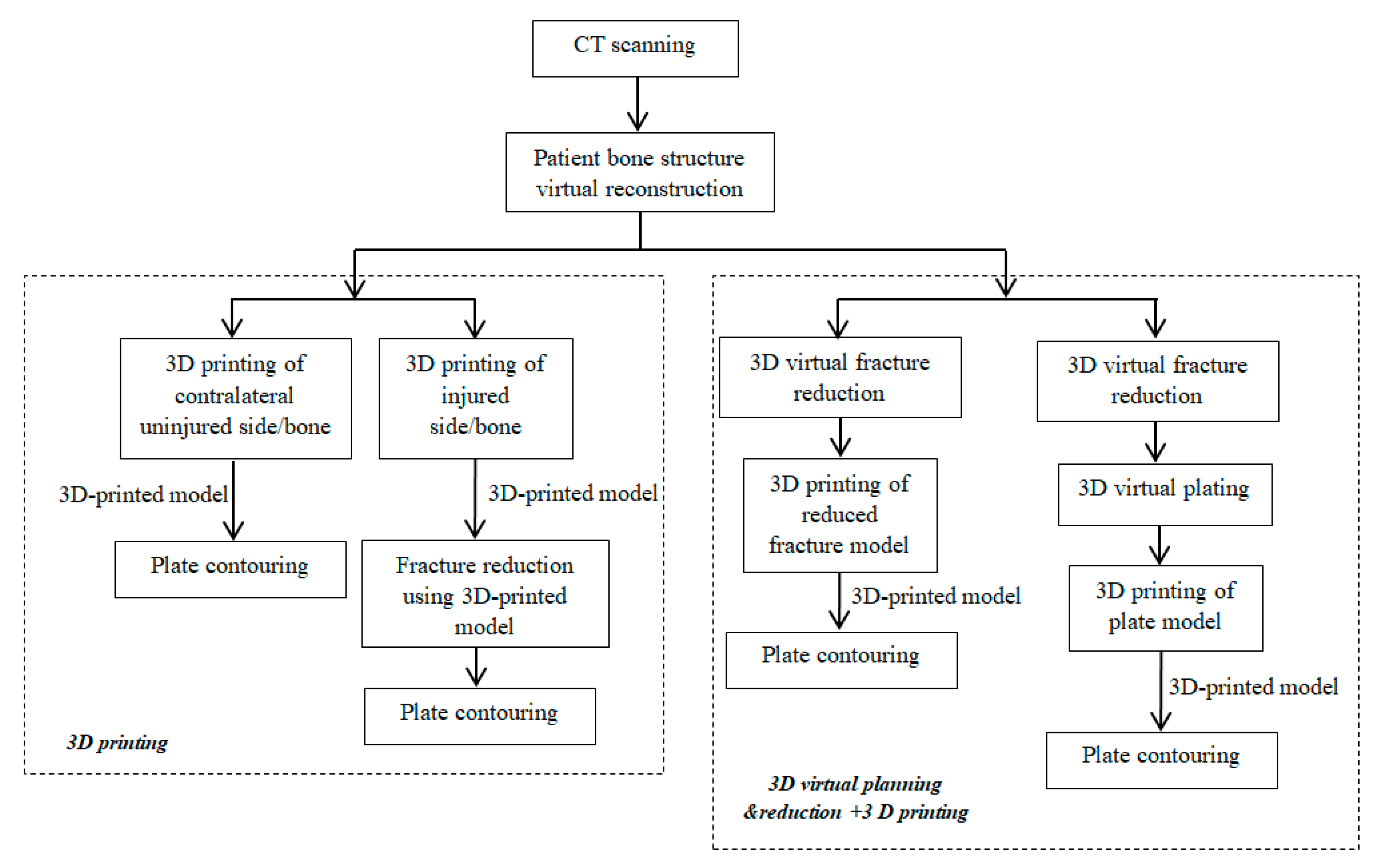
- RQ2: What are the approaches in developing and using 3D-printed models for precontouring plates? → Obj2. Identify the typical workflows currently used in this field.
- −
- RQ3: What are the reported advantages and challenges? → Obj3. Discuss the review results, reported benefits and shortcomings, and preferred anatomical zones for this type of application.
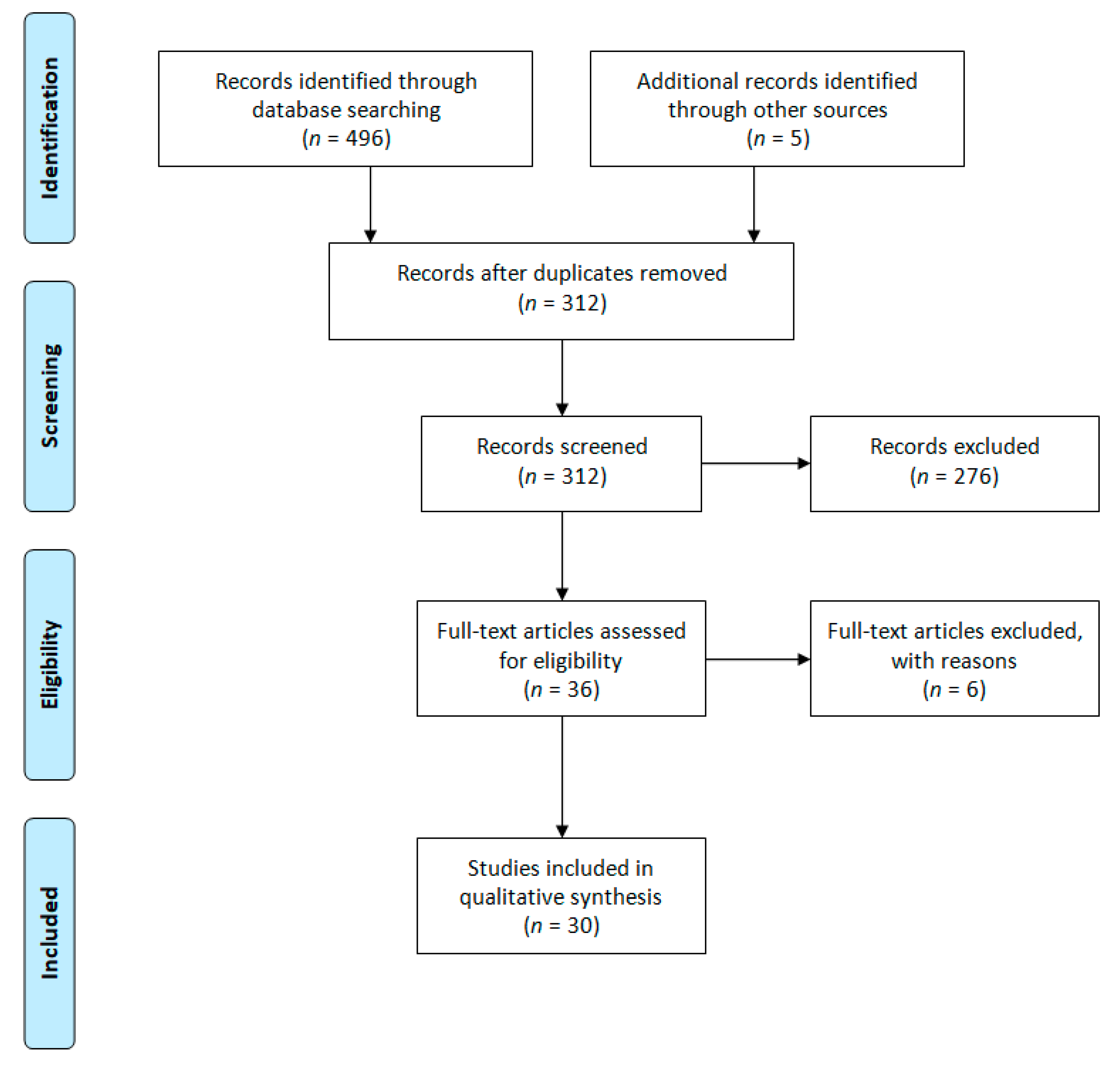
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Data Extraction
2.4. Data Analysis
3. Results
3.1. Studies Design
3.2. Studies Quality
3.3. Anatomical Locations of Reported Cases
3.4. Data on Reported Advantages
3.5. 3D Printing Based Approaches
3.6. Reviewed Studies Timeline
4. Discussions
4.1. 3DP Templating for Acetabular Zone
4.2. 3DP Templating for Clavicle Zone
4.3. 3DP Templating for Calcaneus Fractures
4.4. 3DP Templating for Chest Zone
4.5. 3DP Templating for Humeral Zone
4.6. 3DP Templating for Scaphoid Zone
4.7. 3D Printing Process Related Aspects: Manufacturing Time and Costs, Advantages and Disadvantages
5. Conclusions and Future Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Jin, Y.; Li, X.; Campbell, I.R.; Ji, S. Visualizing the hotspots and emerging trends of 3D printing through scientometrics. Rapid Prototyp. J. 2018, 24, 801–812. [Google Scholar] [CrossRef] [Green Version]
- Ramola, M.; Yadav, V.; Jain, R. On the adoption of additive manufacturing in healthcare: A literature review. J. Manuf. Technol. Manag. 2019, 30, 48–69. [Google Scholar] [CrossRef]
- Pereira, T.; Kennedy, J.V.; Potgieter, J. A comparison of traditional manufacturing vs. additive manufacturing, the best method for the job. Procedia Manuf. 2019, 30, 11–18. [Google Scholar] [CrossRef]
- Martelli, N.; Serrano, C.; van den Brink, H.; Pineau, J.; Prognon, P.; Borget, I.; El Batti, S. Advantages and disadvantages of 3-dimensional printing in surgery: A systematic review. Surgery 2016, 159, 1485–1500. [Google Scholar] [CrossRef] [PubMed]
- Vaishya, R.; Patralekh, M.K.; Vaish, A.; Agarwal, A.K.; Vijaya, V. Publication trends and knowledge mapping in 3D printing in Orthopaedics. J. Clin. Orthop. Trauma 2018, 9, 194–201. [Google Scholar] [CrossRef] [PubMed]
- Lal, H.; Patralekh, M.K. 3D printing and its applications in orthopaedic trauma: A technological marvel. J. Clin. Orthop. Trauma 2018, 9, 260–268. [Google Scholar] [CrossRef]
- Chang, D.; Tummala, S.; Sotero, D.; Tong, E.; Mustafa, L.; Mustafa, M.; Browne, W.F.; Winokur, R.S. Three-Dimensional Printing for Procedure Rehearsal/Simulation/Planning. Tech. Vasc. Interv. Radiol. 2019, 22, 14–20. [Google Scholar] [CrossRef] [Green Version]
- Langridge, B.; Momin, S.; Coumbe, B.; Woin, E.; Griffin, M.; Butler, P. Systematic Review of the Use of 3-Dimensional Printing in Surgical Teaching and Assessment. J. Surg. Educ. 2018, 75, 209–221. [Google Scholar] [CrossRef]
- Gao, C.; Wang, C.; Jin, H.; Wang, Z.; Li, Z.; Shi, C.; Leng, Y.; Yang, F.; Liu, H.; Wang, J. Additive manufacturing technique-designed metallic porous implants for clinical application in orthopaedics. RSC Adv. 2018, 8, 25210–25227. [Google Scholar] [CrossRef] [Green Version]
- Popescu, D.; Laptoiu, D. Rapid prototyping for patient-specific surgical orthopaedics guides: A systematic literature review. Proc. Inst. Mech. Eng. 2016, 230, 495–515. [Google Scholar] [CrossRef]
- Diment, L.E.; Thompson, M.S.; Bergmann, J.H.M. Clinical efficacy and effectiveness of 3D printing: A systematic review. BMJ Open 2017, 7, e016891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Courvoisier, A.; Boudissa, M.; Chabanas, M.; Tonetti, J. Computer assisted surgery in preoperative planning of acetabular fracture surgery: State of the art. Expert Rev. Med. Devices 2017, 15, 81–89. [Google Scholar]
- Bagaria, V.; Deshpande, S.; Rasalkar, D.D.; Kuthe, A.; Paunipagar, B.K. Use of rapid prototyping and three-dimensional reconstruction modeling in the management of complex fractures. Eur. J. Radiol. 2011, 80, 814–820. [Google Scholar] [CrossRef] [PubMed]
- Battiato, C.; Basiglini, L.; Giovannini, F. Traumatological Application of 3D Model in Complex Acetabular Fractures. Trauma Cases Rev. 2017, 3, 1–4. [Google Scholar]
- Belien, H.; Biesmans, H.; Steenwerckx, A.; Bijnens, E.; Dierickx, C. Prebending of osteosynthesis plate using 3D printed models to treat symptomatic os acromiale and acromial fracture. J. Exp. Orthop. 2017, 4, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Brown, G.A.; Milner, B.; Firoozbakhsh, K. Application of computer-generated stereolithography and interpositioning template in acetabular fractures: A report of eight cases. J. Orthop. Trauma 2002, 16, 347–352. [Google Scholar] [CrossRef]
- Chana-Rodríguez, F.; Mañanes, R.P.; Rojo-Manaute, J.; Gil, P.; Martínez-Gómiz, J.M.; Vaquero-Martín, J. 3D surgical printing and pre contoured plates for acetabular fractures. Injury 2016, 47, 2507–2511. [Google Scholar] [CrossRef]
- Chana-Rodríguez, F.; Pérez Mananes, R.; Narbona Cárceles, F.J.; Gil Martínez, P. 3D printing utility for surgical treatment of acetabular fractures. Rev. Esp. Cir. Ortop. Traumatol. 2018, 62, 231–239. [Google Scholar] [CrossRef]
- Chen, Y.Y.; Lin, K.H.; Huang, H.K.; Chang, H.; Lee, S.C.; Huang, T.W. The beneficial application of preoperative 3D printing for surgical stabilization of rib fractures. PLoS ONE 2018, 13, e0204652. [Google Scholar] [CrossRef]
- Chen, K.; Yang, F.; Yao, S.; Xiong, Z.; Sun, T.; Zhu, F.; Teemacque, D.; Drpaul, D.; Ren, Z.; Guo, X. Application of computer-assisted virtual surgical procedures and three-dimensional printing of patient-specific pre-contoured plates in bicolumnar acetabular fracture fixation. Orthop. Traumatol. Surg. Res. 2019, 105, 877–884. [Google Scholar] [CrossRef]
- Chung, K.J.; Hong, D.Y.; Kim, Y.T.; Yang, I.; Park, Y.W.; Kim, H.N. Preshaping Plates for Minimally Invasive Fixation of Calcaneal Fractures Using a Real-Size 3D-Printed Model as a Preoperative and Intraoperative Tool. Foot Ankle Int. 2014, 35, 1231–1236. [Google Scholar] [CrossRef] [PubMed]
- Hao, S.; Wang, F.; Liu, Z.; Liu, Y.; Liu, J.; Wang, Y.; Bai, L. 3D printing mirror model to assist MIPPO technology in the treatment of displaced midshaft clavicle fracture: A case report. Int. J. Clin. Exp. Med. 2019, 11, 2717–2720. [Google Scholar]
- Hsu, C.L.; Chou, Y.C.; Li, Y.T.; Chen, J.E.; Hung, C.C.; Wu, C.C.; Shen, H.C.; Yehv, T.T. Pre-operative virtual simulation and three-dimensional printing techniques for the surgical management of acetabular fractures. Int. Orthop. 2019, 43, 1969–1976. [Google Scholar] [CrossRef] [PubMed]
- Hung, C.C.; Li, Y.T.; Chou, Y.C.; Chen, J.E.; Wu, C.C.; Shen, H.C.; Yeh, T.T. Conventional plate fixation method versus pre-operative virtual simulation and three-dimensional printing-assisted contoured plate fixation method in the treatment of anterior pelvic ring fracture. Int. Orthop. 2016, 3, 425–431. [Google Scholar] [CrossRef]
- Jeong, H.S.; Park, K.J.; Kil, K.M.; Chong, S.; Eun, H.J.; Lee, T.S.; Lee, J.P. Minimally invasive plate osteosynthesis using 3D printing for shaft fractures of clavicles: Technical note. Arch. Orthop. Trauma Surg. 2014, 134, 1551–1555. [Google Scholar] [CrossRef]
- Kataoka, T.; Oka, K.; Miyake, J.; Omori, S.; Tanaka, H.; Murase, T. 3-Dimensional Prebent Plate Fixation in Corrective Osteotomy of Malunited Upper Extremity Fractures Using a Real-Sized Plastic Bone Model Prepared by Preoperative Computer Simulation. J. Hand Surg. Am. 2013, 38, 909–919. [Google Scholar] [CrossRef]
- Kim, H.N.; Xiao, N.L.; Noh, K.C. Use of a real-size 3d-printed model as a preoperative and intra-operative tool for minimally invasive plating of comminuted midshaft clavicle fractures. J. Orthop. Surg. Res. 2015, 10, 91–96. [Google Scholar] [CrossRef] [Green Version]
- Li, L.; Gao, J.; Bi, L.; Yuan, Z.; Pei, G. Comparison of three-dimensional printing and conventional imaging in surgical treatment of Tile C pelvic fractures: A long-term follow-up study. Int. J. Clin. Exp. Med. 2017, 10, 12433–12439. [Google Scholar]
- Li, Y.T.; Hung, C.C.; Chou, Y.C.; Chen, J.E.; Wu, C.C.; Shen, H.C.; Yeh, T.T. Surgical Treatment for Posterior Dislocation of Hip Combined with Acetabular Fractures Using Preoperative Virtual Simulation and Three-Dimensional Printing Model-Assisted Precontoured Plate Fixation Techniques. Biomed Res. Int. 2019, 2019, 3971571. [Google Scholar] [CrossRef] [Green Version]
- Maini, L.; Sharma, A.; Jha, S.; Sharma, A.; Tiwari, A. Three dimensional printing and patient-specific pre-contoured plate: Future of acetabulum fracture fixation? Eur. J. Trauma Emerg. Surg. 2018, 44, 215–224. [Google Scholar] [CrossRef]
- Maini, L.; Verma, T.; Sharma, A.; Sharma, A.; Mishra, A.; Jha, S. Evaluation of accuracy of virtual surgical planning for patient specific pre-contoured plate in acetabular fracture fixation. Arch. Orthop. Trauma Surg. 2018, 138, 495–504. [Google Scholar] [CrossRef] [PubMed]
- Nie, W.B.; Ye, F.G.; Ma, J.L.; Yu, J.P.; Wang, M.X.; Zhang, Z.H.; Sun, F.J. Three-dimensional (3D) Printing Technology Assisted by Minimally Invasive Surgery for Pubic Rami Fractures. Curr. Med. Sci. 2018, 38, 827–833. [Google Scholar] [CrossRef] [PubMed]
- Shon, H.C.; Choi, S.; Yang, J.Y. Three-dimensional printing-assisted surgical technique with limited operative exposure for both-column acetabular fractures. Ulus Travma Acil Cerrahi Derg 2018, 24, 369–375. [Google Scholar] [PubMed]
- Smith, J.A.; Ho, V.P.; Towe, C.W. Using 3-Dimensional Modeling to Customize Titanium Plates for Repair of Chest Wall Trauma. Surg. Innov. 2018, 25, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Ten Berg, P.W.L.; Dobbe, J.G.G.; Streekstra, G.J. Three-dimensional printed anatomical models in scaphoid surgery. J. Hand Surg. (Eur. Vol.) 2018, 43, 101–102. [Google Scholar] [CrossRef] [PubMed]
- Upex, P.; Jouffroy, P.; Riouallon, G. Application of 3D printing for treating fractures of both columns of the acetabulum: Benefit of pre-contouring plates on the mirrored healthy pelvis. Orthop. Traumatol. Surg. Res. 2017, 103, 331–334. [Google Scholar] [CrossRef]
- Van Doremalen, R.F.M.; Kootstra, J.J.; Hekman, E.E.G.; van Helden, S.H. Use of rapid prototyping in a midschaft clavicular pseudarthrosis repair. J. Shoulder Elbow Surg. 2016, 25, e21–e24. [Google Scholar] [CrossRef]
- Wang, Q.; Hu, J.; Guan, J.; Chen, Y.; Wang, L. Proximal third humeral shaft fractures fixed with long helical PHILOS plates in elderly patients: Benefit of pre-contouring plates on a 3D-printed model-A retrospective study. J. Orthop. Surg. Res. 2018, 13, 203. [Google Scholar] [CrossRef] [Green Version]
- Yao, L.F.; Wang, H.Q.; Zhang, F.; Wang, L.P.; Dong, J.H. Minimally invasive treatment of calcaneal fractures via the sinus tarsi approach based on a 3D printing technique. Math. Biosci. Eng. 2019, 16, 1597–1610. [Google Scholar] [CrossRef]
- Yu, A.W.; Duncan, J.M.; Daurka, J.S.; Lewis, A.; Cobb, J. A Feasibility Study into the Use of Three-Dimensional Printer Modelling in Acetabular Fracture Surgery. Adv. Orthop. 2015, 2015, 617046. [Google Scholar] [CrossRef]
- Zeng, C.; Xing, W.; Wu, Z.; Huang, H.; Huang, W. A combination of three-dimensional printing and computer-assisted virtual surgical procedure for preoperative planning of acetabular fracture reduction. Injury 2016, 47, 2223–2227. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, Y.; Cao, S.; Lin, Y.; Li, R.; Wang, G.; Wang, Y. Minimally invasive plate osteosynthesis of acetabular anterior column fractures using the two-incision minimally invasive approach and a preshaped three dimension plate. Int. Orthop. 2016, 40, 2157–2162. [Google Scholar] [CrossRef] [PubMed]
- Prabhu, S.P. From CT and MR images to 3D printed models-Software Basics for the Surgeon in 3D. 3D Print. Orthop. Surg. 2019, 31–40. [Google Scholar] [CrossRef]
- Biomet Microfixation. Warnings and Precautions for the Use of Biomet Microfixation RibFix Blu Thoracic Fixation System. Available online: http://www.biomet.com/wps/wcm/connect/internet/07e48ba6-e374-4f01-8363-7a4a956d1875/01-50-1605+RevB+English.pdf?MOD=AJPERES (accessed on 5 April 2019).
- Lubovsky, O.; Peleg, E.; Joskowicz, L. Acetabular orientation variability and symmetry based on CT scans of adults. Int. J. Comp. Ass. Rad. 2010, 5, 449–454. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Ji, Y.; Wang, X.; Liu, J.; Li, D. Can the recovery of lower limb fractures be achieved by use of 3D printing mirror model? Injury 2017, 48, 2485–2495. [Google Scholar] [CrossRef]
- Tile, M. Fractures of the acetabulum. In The Rationale of Operative Fracture Care, 3rd ed.; Schatzker, J., Tile, M., Eds.; Springer: Berlin/Heidelberg, Germany, 2005; pp. 291–340. [Google Scholar]
- Matta, J.M. Indications for anterior fixation of pelvic fractures. Clin. Orthop. Relat. Res. 1996, 329, 88–96. [Google Scholar] [CrossRef]
- Wu, X.B.; Wang, J.Q.; Zhao, C.P.; Sun, X.; Shi, Y.; Zhang, Z.A.; Li, Y.N.; Wang, M.Y. Printed three-dimensional anatomic templates for virtual preoperative planning before reconstruction of old pelvic injuries: Initial results. Chin. Med. J. 2015, 128, 477–482. [Google Scholar] [CrossRef] [PubMed]
- McKee, R.C.; Whelan, D.B.; Schemitsch, E.H.; McKee, M.D. Operative versus nonoperative care of displaced midshaft clavicular fractures: A meta-analysis of randomized clinical trials. J. Bone Joint Surg. Am. 2012, 94, 675–684. [Google Scholar] [CrossRef]
- Jiang, H.; Qu, W. Operative treatment of clavicle midshaft fractures using a locking compression plate: Comparison between mini-invasive plate osteosynthesis (MIPPO) technique and conventional open reduction. Orthop. Traumatol. Surg. Res. 2012, 98, 666–671. [Google Scholar] [CrossRef] [Green Version]
- Cunningham, B.P.; McLaren, A.; Richardson, M.; McLemore, R. Clavicular length: The assumption of symmetry. Orthopedics 2013, 36, e343–e347. [Google Scholar] [CrossRef] [Green Version]
- Epstein, N.; Chandran, S.; Chou, L. Current concepts review: Intra-articular fractures of the calcaneus. Foot Ankle Int. 2012, 33, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Harvey, E.J.; Grujic, L.; Early, J.S.; Benirschke, S.K.; Sangeorzan, B.J. Morbidity associated with ORIF of intra-articular calcaneus fractures using a lateral approach. Foot Ankle Int. 2001, 22, 868–873. [Google Scholar] [CrossRef] [PubMed]
- Kasotakis, G.; Hasenboehler, E.A.; Streib, E.W.; Patel, N.; Patel, M.B.; Alarcon, L.; Bosarge, P.L.; Love, J.; Haut, E.R.; Como, J.J. Operative fixation of rib fractures after blunt trauma: A practice management guideline from the Eastern Association for the Surgery of Trauma. J. Trauma Acute Care Surg. 2017, 82, 618–626. [Google Scholar] [CrossRef] [PubMed]
- El-Din, W.A.; Ali, M.H. A morphometric study of the patterns and variations of the acromion and glenoid cavity of the scapulae in Egyptian population. J. Clin. Diagn. Res. 2015, 9, AC08–AC11. [Google Scholar] [CrossRef] [PubMed]
- Adey, L.; Souer, J.S.; Lozano-Calderon, S.; Palmer, W.; Lee, S.G.; Ring, D. Computed tomography of suspected scaphoid fractures. J. Hand Surg. 2007, 32, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Msallem, B.; Sharma, N.; Cao, S.; Halbeisen, F.S.; Zeilhofer, H.-F.; Thieringer, F.M. Evaluation of the Dimensional Accuracy of 3D-Printed Anatomical Mandibular Models Using FFF, SLA, SLS, MJ, and BJ Printing Technology. J. Clin. Med. 2020, 9, 817. [Google Scholar] [CrossRef] [Green Version]
- Popescu, D.; Laptoiu, D.; Marinescu, R.; Botezatu, I. Design and 3D printing customized guides for orthopaedic surgery-lessons learned. Rapid Prototyp. J. 2018, 24, 901–913. [Google Scholar] [CrossRef]
- Salmi, M.; Kaija-Stiina Paloheimo, K.S.; Tuomia, J.; Wolff, J.; Mäkitiead, A. Accuracy of medical models made by additive manufacturing (rapid manufacturing). J. Craniomaxillofac. Surg. 2013, 41, 603–609. [Google Scholar] [CrossRef]
- Mallepree, T.; Bergers, D. Accuracy of medical RP models. Rapid Prototyp. J. 2019, 15, 325–332. [Google Scholar] [CrossRef]
- George, E.; Liacouras, P.; Rybicki, F.J.; Mitsouras, D. Measuring and Establishing the Accuracy and Reproducibility of 3D Printed Medical Models. Radiographics 2017, 37, 1424–1450. [Google Scholar] [CrossRef]

| Reference | Type of Intervention | No. of Patients Treated Using 3D Prints | Design Study, Level of Evidence | Approach | Software for 3D Model | 3D Printing (Printer, Material, Time, Cost) |
|---|---|---|---|---|---|---|
| Bagaria et al. [13] Year: 2011 Country: India, China | Acetabular fracture, femoral condyle fracture, calcaneal fracture | 4 | Case series LOE-IV | 3DP model of fractured acetabulum (with indelible ink marked zones of fracture) used as template for precontouring the plate | Mimics (Materialise, Leuven, Belgium) | FDM process, ABS 19 euros |
| Battiato et al. [14] Year: 2017 Country: Italy | Both acetabular fractures | 1 | Case report LOE-V | 3DP of entire pelvis used for fractures reduction and then for precontouring the plates | Mimics (Materialise, Leuven, Belgium) | SLS process, Polyamide PA2200, 46 h the entire development process |
| Belien et al. [15] Year: 2017 Country: Belgium | Os acromiale, acromial fracture | 5 | Case series LOE-IV | 3DP model of fractured bone after fracture reduction used as template for precontouring the plate | in Vesalius (CTI, SP, Brazil), Rhinoceros 5 (Robert McNeel & Associates, Seattle, USA), Meshmixer (Autodesk, San Rafael, USA), Netfabb Pro (Autodesk, San Rafael, USA) | Makerbot Replicator 2, FDM process |
| Brown et al. [16] Year: 2002 Country: USA | Acetabular fracture | 8 | Case series LOE-IV | 3DP model of the mirrored model of uninjured acetabulum for precontouring the plate | Mimics (Materialise, Leuven, Belgium) | Actua 2100, SLA, Wax, then mould methyl methacrylate |
| Chana-Rodriquez et al. [17] Year: 2016 Country: Spain | Acetabular fracture | 1 | Case report LOE-V | 3DP model of the mirrored model of uninjured acetabulum used as template for precontouring the plate | OsiriX (Pixmeo, Geneva, Switzerland), Meshlab V1.3.3 (Visual Computing Lab, Pisa, Italy), Meshmixer 2.4 (Autodesk, San Rafael, USA | Da Vinci 3D printer, FDM process, ABS, 11 h, 12 euros |
| Chana- Rodriquez et al. [18] Year: 2018 Country: Spain | Acetabular fractures | 20 | Prospective case series LOE-IV | 3DP model of the mirrored model of uninjured acetabulum used as template for precontouring the plate | OsiriX (Pixmeo, Geneva, Switzerland), Meshmixer (Autodesk, San Rafael, USA) Mean of 10.7 min for medical modeling | Da Vinci 3D printer, FDM process, ABS Mean of 385 min for 3D prints manufacturing 12 euros |
| Chen YY et al. [19] Year: 2018 Country: China | Rib fractures | 16 | Retrospective review 48 patients LOE-IV | 3DP model of fractured ribs/rib (with indelible ink marked zones of fractures) used as template for precontouring the plate | - | UP-BOX 3D Printer, FDM process, ABS 5–6 h for 3DP printing |
| Chen K et al. [20] Year 2019 Country: China | Bicolumnar acetabular fracture | 28 | Retrospective analysis, 52 patients, LOE-III | Virtual fracture reduction + 3DP reduced fracture model for precontouring the plate | Mimics 16.0 (Materialise, Leuven, Belgium) | PLA, 36 h total time (including sterilization, bending), 65 euro |
| Chung et al. [21] Year: 2014 Country: S. Korea | Calcaneal fracture | 1 | Case report LOE-V | 3DP model of contralateral uninjured calcaneus used as template for precontouring the plate | Mimics (Materialise, Leuven, Belgium), 30 min modeling | Probably FDM process 3 h printing |
| Hao et al. [22] Year: 2019 Country: China | Midshaft clavicle fracture | 1 | Case report LOE-V | 3DP model of contralateral uninjured clavicle used as template for precontouring plate | Mimics 17.0 (Materialise, Leuven, Belgium) | DLP process |
| Hsu et al. [23] Year: 2019 Country: China | Acetabular fracture | 12 | Retrospective study with control group LOE-III Total of 29 patients | Virtual reduction of fracture + 3DP model of reduced fracture used as template for precontouring plate | Mimics 19.0 (Materialise, Leuven, Belgium) | Up Box+, FDM process |
| Hung et al. [24] Year: 2019 Country: China | Pelvic ring fractures | 16 | Retrospective study, non-randomized with control group LOE-III Total of 30 patients | Virtual reduction of fracture + 3DP model of reduced fracture used as template for precontouring the plate | Mimics 19.0 (Materialise, Leuven, Belgium) Up to 90 min virtual reduction for complex cases | UP BOX+ 3D printer, FDM process Less than 24 h the entire process, 20 euros |
| Jeong et al. [25] Year: 2014 Country: S. Korea | Clavicle shaft fracture | 1 | Case report LOE-V | 3DP of contralateral clavicle used as template for precontouring the plate | - | $20, 3 h for 3DP, 3 h for plate bending and sterilization |
| Kataoka et al. [26] Year: 2013 Country: Japan | 4 cubitus varus, 1 cubitus valgus, 4 diaphyseal malunions of the forearm | 9 | Series of cases, LOE-Therapeutic IV | Virtual planning and simulation using contralateral normal bone as template + 3DP of repositioned bone models as template for precontouring the plate | Bone Simulator (Orthree, Osaka, Japan) | Eden 250, Objet, Medical grade resin |
| Kim et al. [27] Year: 2015 Country: S. Korea, China | Midshaft clavicle fracture | 7 | Series of cases (technical note) LOE-IV | 3DP model of contralateral uninjured clavicle used as template for precontouring the plate | Mimics (Materialise, Leuven, Belgium) | Project x60 series, $100, 2–3 days the whole process CT to solid model |
| Li L et al. [28] Year: 2017 Country: China | Pelvic fracture | 28 | Retrospective review (long-term follow up study with control group), Total of 64 patients LOE-III | 3DP model of pelvis used for simulating operation and then for precontouring the plates | Mimics 14.0 (Materialise, Leuven, Belgium) | Yinhua Rapid Prototyping 3D printer, probably FDM process |
| Li YT et al. [29] Year: 2019 Country: China | Hip dislocation combined with acetabular fracture | 7 | Retrospective review control group Total of 16 patients LOE-III | Virtual reduction by mirroring contralateral, uninjured side + 3DP model of reduced model used as template for precontouring the plate | Mimics 19.0 (Materialise, Leuven, Belgium), 11 min for modeling | Up Box+ 3D printer, FDM process, 10 h for 3D printing |
| Maini et al. [30] Year: 2018 Country: India | Acetabular fracture | 10 | Prospective randomized case control study Total of 21 patients LOE-II | 3DP model of fractured acetabulum followed by its reduction and its use as template for precontouring the plate | Mimics 8.13 (Materialise, Leuven, Belgium) | Eosint P380, SLS, nylon polyamide, $15–20 |
| Maini et al. [31] Year: 2018 Country: India | Acetabular fracture | 12 | Randomized case control study 25 patients LOE-II | Virtual planning and simulation for reducing fracture followed by virtual modeling the plate (virtual plating) + 3D-printed plate model as template for precontouring the metal plate | Mimics and 3-Matic (Materialise, Leuven, Belgium), Average time: 4.3 h | FDM, PLA, $4 |
| Nie et al. [32] Year: 2018 Country: China | Pubic rami fractures | 30 | Consecutive case series LOE-IV | Virtual planning and reduction of fracture + 3DP model of reduced fracture used as template for precontouring plate | Mimics 10.01 (Materialise, Leuven, Belgium) | FDM process, ABS material probably |
| Shon et al. [33] Year: 2018 Country: S. Korea | Both-column acetabular fractures | 5 | Series of cases LOE-IV | 3DP model of fractured acetabulum (with indelible ink marked fracture line) followed by reduction and fixation with glue, thus reduced model being used as template for precontouring the plate | - | Edison 3D printer, FDM process, PLA, 3 h total development time for the 3D print, $30 |
| Smith et al. [34] Year: 2018 Country: USA | Rib fractures | 1 | Case report LOE-V | Virtual reduction using mirroring of contralateral uninjured side + 3DP model with reduced fractured and marked fracture lines used as template for precontouring plates | D2P (3D Systems, Rock Hill, USA), Geomagic Freeform Plus (3D Systems, Rock Hill, USA) | ProX 800 3D printer, SLA, ClearView polycarbonate-like resin |
| ten Berg et al. [35] Year: 2017 Country: The Netherlands | Nonunion of scaphoid fracture | 8 | Series of cases (short report letter) LOE-V | 3DP model of uninjured contralateral bone for plate bending | Custom software (C++(Visual Studio 2005, Microsoft, Redmond, USA), Visualization ToolKit (VTK 5.0.4, Kitware, Inc., NY, USA), Insightt ToolKit (ITK 3.6.0, Kitware, Inc., NY, USA) | Blue printer M2, Selective Heat Sintering, Thermoplastic powder |
| Upex et al. [36] Year: 2017 Country: France | Acetabular fracture | 1 | Case report (technical note) LOE-V | 3DP model of the healthy hemipelvis used as template for precontouring plate | OsiriX (Pixmeo, Geneva, Switzerland), Meshmixer (Autodesk, San Rafael, USA) | Ultimaker, FDM process, PLA, 6 euros |
| Van Doremalen et al. [37] Year: 2016 Country: The Netherlands | Midshaft clavicle fracture | 1 | Case report LOE-V | 3DP model of contralateral intact clavicle for plate bending | Matlab(MathWorks, Natick, USA), Meshlab (Visual Computing Lab, Pisa, Italy | BQ Witbox, FDM process, PLA, 4 h total time for the whole process (modeling, 3DP, bending) |
| Wang et al. [38] Year: 2018 Country: China | Humeral shaft fracture | 21 | Retrospective review, 46 patients, comparison 3DP model with Synbone model LOE-IV | 3DP model of intact bone used as template for precontouring the plate | Mimics 16.0 (Materialise, Leuven, Belgium) 3 h modeling time | Lite, RS6000, DLP process, ultraviolet curable resin |
| Yao et al. [39] Year: 2019 Country: China, Australia | Calcaneal fractures | 25 | Case series LOE-IV | 3DP model of uninjured calcaneus used as template for precontouring plate | Mimics 15.0 (Materialise, Leuven, Belgium) | Makerbot Replicator 3D printer |
| Yu et al. [40] Year: 2015 Country: UK | Both column acetabulum fractures | 2 | Cases report LOE-V | 3DP model of contralateral uninjured side used as template for precontouring the plate | - | Objet Eden 250 3D printer, SLS process, MED610 polymer |
| Zeng et al. [41] Year: 2016 Country: China | Acetabular fracture | 10 | Series of cases LOE-IV | Virtual fracture reduction + 3DP reduced fracture model for precontouring the plate | Mimics 14.0 (Materialise, Leuven, Belgium) | Makerbot Replicator 2, FDM process |
| Zhuang et al. [42] Year: 2016 Country: China | Acetabular fractures (7 fractures anterior column, 4 anterior column with posterior hemitransverse, 1 anterior column with the pubic symphysis) | 12 | Case series LOE-IV | 3D printed model on uninjured hemipelvis with marked fracture lines used as template for precontouring the plate | - | Mira ProJet 3510 3D printer, MJ process, ultraviolet curable resin |
| Studies Design | Case Reports | Series of Cases | Non-Randomized Clinical Studies | Randomized-Clinical Studies |
|---|---|---|---|---|
| Representing % from the total No. of papers | 36.67% | 33.33% | 23.33% | 6.67% |
| No. of patients in 3DP group | 10 | 143 | 128 | 22 |
| No. of patients in control group | - | - | 233 | 24 |
| Anatomical Location | Total No. of Patients Using 3D Prints | Total No. of Studies Per Anatomical Location | Total No. of Patients in Studies |
|---|---|---|---|
| Acetabulum | 206 | 18 (60%) | 415 (206 3DP + 209 control) |
| Clavicle | 15 | 5 (17%) | 15 |
| Rib | 17 | 2 (6.8%) | 65 (17 3DP + 48 control) |
| Humerus | 21 | 1 | 21 |
| Cubitus | 9 | 1 | 9 |
| Scaphoid | 8 | 1 | 8 |
| Calcaneus | 27 | 2 | 27 |
| Study | Mean Blood Loss (mL) | Mean Surgical Time (min)/Instrumentation Time (Min) | Quality of Reduction | ||
|---|---|---|---|---|---|
| 3DP Group | Conventional Group | 3DP Group | Conventional Group | ||
| Chen YY et al. [19] | - | - | 125 ± 33.44 | 175.24 ± 60.58 | - |
| Chen K et al. [20] | 696.0 7 ± 66.54 | 833.75 ± 227.44 | 157.5 ± 20.48 | 187.08 ± 35.81 | Similar |
| Hsu et al. [23] | 433.33 ± 317.28 | 958.33 ± 427.10 | 199.00 ± 50.29 | 274.17 ± 80.95 | Similar |
| Hung et al. [24] | 275.00 ± 196.64 | 549.29 ± 404.43 | 206.13 ± 70.32/ 45.63 ± 15.26 | 276.21 ± 89.53/ 102.86 ± 25.85 | Similar |
| Li L et al. [28] | 481.4 ± 103.2 | 771.1 ± 114.4 | 128.9 ± 59.2 | 191.4 ± 85.1 | Better in 3DP group (Matta score) |
| Li YT et al. [29] | 735.71 ± 614.22 | 742.22 ± 228.68 | 211.71 ± 52.23/ 38.43 ± 10.81 | 254.44 ± 34.46/ 71.78 ± 9.69 | Similar |
| Maini et al. [30] | 620 ± 246.9 | 720 ± 286.2 | 120 ± 37.7 | 132 ± 41.0 | Better in 3DP group (Matta score) |
| Maini et al. [31] | 467 | 525 | 111 | 119 | Better in 3DP group |
| Wang et al. [38] | 105.19 ± 14.67 | 120.80 ± 10.61 | 42.62 ± 7.61 | 60.36 ± 10.20 | Similar |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marinescu, R.; Popescu, D.; Laptoiu, D. A Review on 3D-Printed Templates for Precontouring Fixation Plates in Orthopedic Surgery. J. Clin. Med. 2020, 9, 2908. https://doi.org/10.3390/jcm9092908
Marinescu R, Popescu D, Laptoiu D. A Review on 3D-Printed Templates for Precontouring Fixation Plates in Orthopedic Surgery. Journal of Clinical Medicine. 2020; 9(9):2908. https://doi.org/10.3390/jcm9092908
Chicago/Turabian StyleMarinescu, Rodica, Diana Popescu, and Dan Laptoiu. 2020. "A Review on 3D-Printed Templates for Precontouring Fixation Plates in Orthopedic Surgery" Journal of Clinical Medicine 9, no. 9: 2908. https://doi.org/10.3390/jcm9092908
APA StyleMarinescu, R., Popescu, D., & Laptoiu, D. (2020). A Review on 3D-Printed Templates for Precontouring Fixation Plates in Orthopedic Surgery. Journal of Clinical Medicine, 9(9), 2908. https://doi.org/10.3390/jcm9092908






