Effect of Raja Yoga Meditation on the Distress and Anxiety Levels of Women with Breast Cancer
Abstract
:1. Introduction
2. Method
Design
3. Ethical Aspects
3.1. Participants and Sample
3.2. Randomization, Allocation, and Blinding
3.3. Intervention Protocol
3.4. Measuring Instruments
3.5. Data Analysis
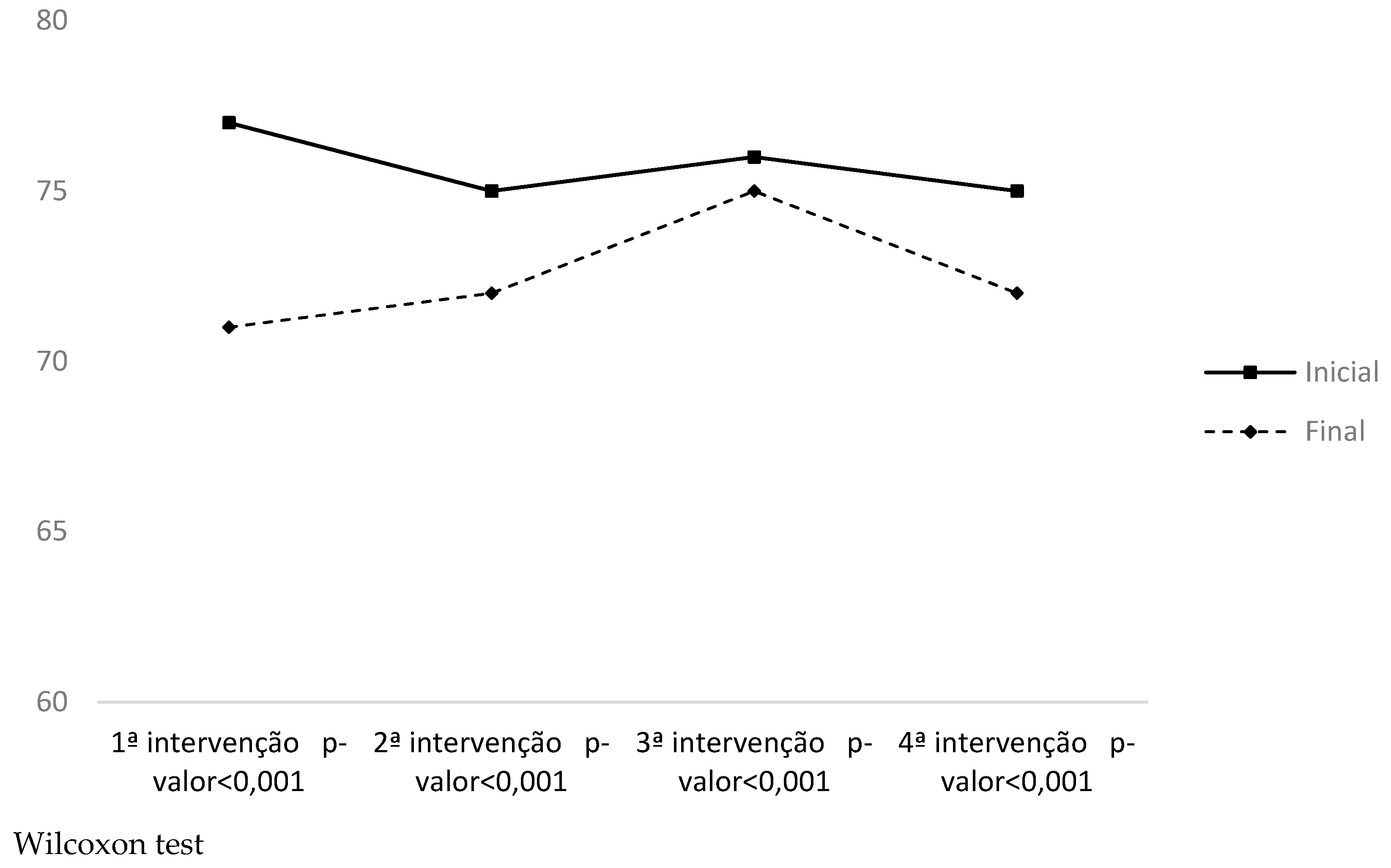
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Abrahão, Camila Aparecida, Emilia Bomfim, Luiz Carlos Lopes-Júnior, and Gabriela Pereira-da-Silva. 2019. Complementary Therapies as a Strategy to Reduce Stress and Stimulate Immunity of Women with Breast Cancer. Journal of Evidence-Based Integrative Medicine 24: 1–7. [Google Scholar] [CrossRef] [Green Version]
- Agarwal, Kanishtha, Luana Fortune, Jennifer C. Heintzman, and Lisa L. Kelly. 2020. Spiritual Experiences of Long-Term Meditation Practitioners Diagnosed with Breast Cancer: An Interpretative Phenomenological Analysis Pilot Study. Journal of Religion and Health 59: 2364–80. [Google Scholar] [CrossRef]
- Amorim, Mary Anne Pasta, and Keila Zaniboni Siqueira. 2017. Relationship Between The Experience of Stressor Factors and the Emergence of Breast Cancer. Psicologia Argumento 32: 2364–80. [Google Scholar] [CrossRef]
- Andersen, Signe R., Hanne Würtzen, Marianne Steding-Jessen, Jane Christensen, Klaus K. Andersen, Henrik Flyger, Cathy Mitchelmore, Christoffer Johansen, and Susanne O. Dalton. 2013. Effect of mindfulness-based stress reduction on sleep quality: Results of a randomized trial among Danish breast cancer patients. Acta Oncologica 52: 336–44. [Google Scholar] [CrossRef] [Green Version]
- Araújo, Raquel Vilanova, Ana Fátima Carvalho Fernandes, Inez Sampaio Nery, Elaine Maria Leite Rangel Andrade, Lídya Tolstenko Nogueira, and Francisco Honeidy Carvalho Azevedo. 2019. Meditation Effect on Psychological Stress Level in Women with Breast Cancer: A Systematic Review. Revista da Escola de Enfermagem da USP 53: e03529. [Google Scholar] [CrossRef]
- Bahri, Narjes, Tahereh Fathi Najafi, Fatemeh Homaei Shandiz, Hamid Reza Tohidinik, and Abdoljavad Khajavi. 2019. The Relation Between Stressful Life Events and Breast Cancer: A Systematic Review and Meta-Analysis of Cohort Studies. Breast Cancer Research and Treatment 176: 53–61. [Google Scholar] [CrossRef]
- Bharshankar, Jyotsana R., Archana D. Mandape, Mrunal S. Phatak, and Rajay N. Bharshankar. 2015. Autonomic Functions in Raja-Yoga Meditators. Indian Journal of Physiology and Pharmacology 59: 396–401. Available online: https://pubmed.ncbi.nlm.nih.gov/27530006/ (accessed on 14 July 2021).
- Bhopal, Jaswant S., Kamyar Dahi, Rajesh Sharma, Larry Frisch, and Ming Yang. 2018. The Immediate Effect of Raja-Yoga Group Therapy on the Well-Being of Psychiatric Outpatients—An Exploratory Single-Center Retrospective Study. Journal of Psychiatry and Behaviour Therapy 1: 13–17. [Google Scholar] [CrossRef] [Green Version]
- Botega, Neury J., Márcia R. Bio, Maria Adriana Zomignani, Celso Garcia Jr., and Walter A. B. Pereira. 1995. Transtornos do Humor em Enfermaria de Clínica Médica e Validação de Escala de Medida (HAD) de Ansiedade e Depressão. Revista de Saúde Pública 29: 555–63. [Google Scholar] [CrossRef] [Green Version]
- Bower, Julienne E., Alexandra D. Crosswell, Annette L. Stanton, Catherine M. Crespi, Diana Winston, Jesusa Arevalo, Jeffrey Ma, Steve W. Cole, and Patricia A. Ganz. 2015. Mindfulness Meditation for Younger Breast Cancer Survivors: A Randomized Controlled Trial. Cancer 121: 1231–40. [Google Scholar] [CrossRef]
- Boyle, Chloe C., Annette L. Stanton, Patricia A. Ganz, Catherine M. Crespi, and Julienne E. Bower. 2017. Improvements in emotion regulation following mindfulness meditation: Effects on depressive symptoms and perceived stress in younger breast cancer survivors. Journal of Consulting and Clinical Psychology 85: 397–402. [Google Scholar] [CrossRef]
- Brasil. 2018a. Portaria n° 702, de 21 de Março de 2018, Altera a Portaria de Consolidação nº 2/GM/MS, de 28 de Setembro de 2017, para Incluir Novas Práticas na Política Nacional de Práticas Integrativas e Complementares—PNPIC; Brasil: Ministério da Saúde.
- Brasil. 2018b. Portaria nº 04 de 23 de Janeiro de 2018. Aprova as Diretrizes Diagnósticas e Terapêuticas do Carcinoma de Mama; Brasil: Ministério da Saúde.
- Bultz, Barry D. 2016. Patient Care and Outcomes: Why Cancer Care Should Screen for Distress, the 6th Vital Sign. Asia-Pacific Journal of Oncology Nursing 3: 21–24. [Google Scholar] [CrossRef]
- Carlson, Linda E., Rie Tamagawa, Joanne Stephen, Elaine Drysdale, Lihong Zhong, and Michael Speca. 2016. Randomized-Controlled Trial of Mindfulness-Based Cancer Recovery Versus Supportive Expressive Group Therapy Among Distressed Breast Cancer Survivors (MINDSET): Long-term Follow-up Results. Psycho-Oncology 25: 750–59. [Google Scholar] [CrossRef] [Green Version]
- Cavalcante, Marcia Luiza Ferreira, Fernanda Chaves, and Arlene Laurenti Monterrosa Ayala. 2016. Câncer de mama: Sentimentos e percepções das mulheres mastectomizadas. Revista de Atenção à Saúde 14: 41–52. [Google Scholar] [CrossRef]
- Charlson, Mary E., Joseph Loizzo, Alyson Moadel, Miles Neale, Chayim Newman, Erin Olivo, Emily Wolf, and Janey C. Peterson. 2014. Contemplative self healing in women breast cancer survivors: A pilot study in underserved minority women shows improvement in quality of life and reduced stress. BMC Complementary Medicine and Therapies 14: 349. [Google Scholar] [CrossRef] [Green Version]
- Chawla, Tara G., Mrunal S. Phatak, and Rajendra G. Bhagchandani. 2020. Positive Effect of Raja Yoga Meditation on Cardiopulmonary Parameters in Type II Diabetes Mellitus. National Journal of Physiology, Pharmacy and Pharmacology 10: 1–5. [Google Scholar] [CrossRef]
- da Mata, Luciana Regina Ferreira, Giannina Marcela Chávez, Beatriz Simões Faria, Ana Cláudia Castro Antunes, Marcela Ribeiro da Silva, and Patrícia Peres de Oliveira. 2016. Self-esteem and Distress in Patients Undergoing Cancer Surgery: A Correlational Study. Online Brazilian Journal of Nursing 15: 664–74. [Google Scholar]
- Decat, Cristiane Sant’Anna, Jacob Arie Laros, and Tereza Cristina Cavalcanti Ferreira de Araujo. 2009. Distress Thermometer: Validation of a Brief Screening Instrument to Detect Distress in Oncology Patients. Psico-USF 14: 253–60. [Google Scholar] [CrossRef] [Green Version]
- Espino-Polanco, Aydé Concepción, and Mercedes García-Cardona. 2018. Cáncer de Mama y su Relación Con el Manejo de las Emociones y el Estrés. Revista de Enfermería del Instituto Mexicano del Seguro Social 26: 145–55. Available online: https://www.medigraphic.com/pdfs/enfermeriaimss/eim-2018/eim182l.pdf (accessed on 14 June 2021).
- Ferreira, Juliana Carvalho, and Cecilia Maria Patino. 2016. Randomization: Beyond Tossing a Coin. Jornal Brasileiro de Pneumologia 42: 310–10. [Google Scholar] [CrossRef] [Green Version]
- Friston, Karl. 2012. Ten ironic rules for non-statistical reviewers. NeuroImage 61: 1300–10. [Google Scholar] [CrossRef]
- Goyal, Atul Kumar, Jaimanti Bakshi, Sushma Rani, Bk Anita Didi, and Akshay Anand. 2018. Is Rajyoga Helpful in Maintaining Patient’s Biochemical and Hematological Profile during Breast Cancer Treatment? Journal of Complementary & Integrative Medicine 16: 1–7. [Google Scholar] [CrossRef]
- Gurgel, Isabela Oliva, Paola Miranda de Sá, Paula Elaine Diniz dos Reis, Mariângela Leal Cherchiglia, Ilka Afonso Reis, Ana Lúcia de Mattia, and Giovana Paula Rezende Simino. 2019. Prevalence of Integrative and Complementary Practices in Patients Undergoing Antineoplastic Chemotherapy. Cogitare Enfermagem 24: e64450. [Google Scholar] [CrossRef]
- Hashemi, Seyed-Mehdi, Hosein Rafiemanesh, Tayebe Aghamohammadi, Mahin Badakhsh, Mehrbanoo Amirshahi, Mahdieh Sari, Niaz Behnamfar, and Kamran Roudini. 2020. Prevalence of Anxiety among Breast Cancer Patients: A Systematic Review and Meta-Analysis. Breast Cancer 27: 166–78. [Google Scholar] [CrossRef]
- Hoffman, Caroline J., Steven J. Ersser, Jane B. Hopkinson, Peter G. Nicholls, Julia E. Harrington, and Peter W. Thomas. 2012. Effectiveness of mindfulness-based stress reduction in mood, breast- and endocrine-related quality of life, and well-being in stage 0 to III breast cancer: A randomized, controlled trial. Journal of Clinical Oncology 30: 1335–42. [Google Scholar] [CrossRef]
- Hulley, Stephen B., Steven R. Cummings, Warren S. Browner, Deborah G. Grady, and Thomas B. Newman. 2019. Delineando a Pesquisa Clinica, 4th ed. Porto Alegre: Artmed. [Google Scholar]
- Instituto Nacional de Câncer. 2019. A situação do câncer de mama no Brasil: Síntese de dados dos sistemas de informação. Rio de Janeiro: INCA, p. 85. [Google Scholar]
- Johns, Shelley A., Linda F. Brown, Kathleen Beck-Coon, Tasneem L. Talib, Patrick O. Monahan, R. Brian Giesler, Yan Tong, Laura Wilhelm, Janet S. Carpenter, Diane Von Ah, and et al. 2016. Randomized Controlled Pilot Trial Of Mindfulness-Based Stress Reduction Compared to Psychoeducational Support for Persistently Fatigued Breast and Colorectal Cancer Survivors. Supportive Care in Cancer 24: 4085–96. [Google Scholar] [CrossRef]
- Kiran, Kiran, Suruchi Ladha, Neeti Makhija, Poonam Malhotra Kapoor, Minati Choudhury, Sambhunath Das, Parag Gharde, Vishwas Malik, and Balram Airan. 2017. The Role of Rajyoga Meditation for Modulation of Anxiety and Serum Cortisol in Patients Undergoing Coronary Artery Bypass Surgery: A Prospective Randomized Control Study. Annals of Cardiac Anaesthesia 20: 158–62. [Google Scholar] [CrossRef]
- Lengacher, Cecile A., Kevin E. Kip, Michelle Barta, Janice Post-White, Paul B. Jacobsen, Maureen Groer, Brandy Lehman, Manolete S. Moscoso, Rajendra Kadel, Nancy Le, and et al. 2012. A pilot study evaluating the effect of mindfulness-based stress reduction on psychological status, physical status, salivary cortisol, and interleukin-6 among advanced-stage cancer patients and their caregivers. Journal of Holistic Nursing 30: 170–85. [Google Scholar] [CrossRef]
- Lengacher, Cecile A., Richard R. Reich, Kevin E. Kip, Michelle Barta, Sophia Ramesar, Carly L. Paterson, Manolete S Moscoso, Irina Carranza, Pinky H Budhrani, Seung Joon Kim, and et al. 2014. Influence of mindfulness-based stress reduction (MBSR) on telomerase activity in women with breast cancer (BC). Biological Research for Nursing 16: 438–47. [Google Scholar] [CrossRef] [Green Version]
- Li, Hongjin, Anna L. Marsland, Yvette P. Conley, Susan M. Sereika, and Catherine M. Bender. 2020. Genes Involved in the HPA Axis and the Symptom Cluster of Fatigue, Depressive Symptoms, and Anxiety in Women with Breast Cancer During 18 Months of Adjuvant Therapy. Biological Research for Nursing 22: 277–86. [Google Scholar] [CrossRef]
- Maass, S. W. M. C., M. Boerman, P. F. M. Verhaak, J. Du, G. H. de Bock, and A. J. Berendsen. 2019. Long-Term Psychological Distress in Breast Cancer Survivors and Their Matched Controls: A Cross-Sectional Study. Maturitas 130: 6–12. [Google Scholar] [CrossRef]
- Mallik, Debesh, Sarah Bowen, Yang Yang, Richard Perkins, and Emily K. Sandoz. 2019. Raja yoga meditation and medication-assisted treatment for relapse prevention: A pilot study. Journal of Substance Abuse Treatment 96: 58–64. [Google Scholar] [CrossRef]
- Marcolino, José Álvaro Marques, Fernando Mikio Suzuki, Luís Augusto Cunha Alli, Judymara Lauzi Gozzani, and Ligia Andrade da Silva Telles Mathias. 2007. Measurement of Anxiety and Depression in Preoperative Patients. Comparative Study. Revista Brasileira de Anestesiologia 57: 157–66. [Google Scholar] [CrossRef]
- Martins, Helga, Tiago Dias Domingues, and Sílvia Caldeira. 2020. Spiritual Well-Being in Cancer Patients Undergoing Chemotherapy in an Outpatient Setting: A Cross-Sectional Study. Journal of Holistic Nursing 38: 68–77. [Google Scholar] [CrossRef]
- Matchim, Yaowarat Matchim, Jane M. Armer, and Bob R. Stewart. 2011. Effects of mindfulness-based stress reduction (MBSR) on health among breast cancer survivors. Western Journal of Nursing Research 33: 996–1016. [Google Scholar] [CrossRef]
- Melo, Saulo Maia d’Avila, Marília Ferraz de Oliveira Macedo, and Juliana Silva Santana Pereira. 2020. Agreement Among four Portable Wireless Pulse Oximeters and In-Office Evaluation of Peripheral Oxygen Saturation. Jornal Brasileiro de Pneumologia 47: e20200251. [Google Scholar] [CrossRef]
- Miranda, Talita Prado Simão, Sílvia Caldeira, Harley Francisco de Oliveira, Denise Hollanda Iunes, Denismar Alves Nogueira, Erika de Cássia Lopes Chaves, and Emília Campos de Carvalho. 2020. Intercessory Prayer on Spiritual Distress, Spiritual Coping, Anxiety, Depression and Salivary Amylase in Breast Cancer Patients During Radiotherapy: Randomized Clinical Trial. Journal of Religion and Health 59: 365–80. [Google Scholar] [CrossRef]
- Nidich, Sanford I., Jeremy Z. Fields, Maxwell V. Rainforth, Rhoda Pomerantz, David Cella, Jean Kristeller, John W. Salerno, and Robert H. Schneider. 2009. A randomized controlled trial of the effects of transcendental meditation on quality of life in older breast cancer patients. Integrative Cancer Therapies 8: 228–34. [Google Scholar] [CrossRef]
- Offidani, Emanuela, Janey C. Peterson, Joseph Loizzo, Anne Moore, and Mary E. Charlson. 2017. Stress and Response to Treatment: Insights from a Pilot Study Using a 4-week Contemplative Self-Healing Meditation Intervention for Posttraumatic Stress in Breast Cancer. Journal of Evidence-Based Complementary & Alternative Medicine 22: 715–20. [Google Scholar] [CrossRef] [Green Version]
- Oliveira, Magda A., Carla Sousa, André Ferreira, and Andreia Cruz. 2017. Screening for Distress, the Sixth Vital Sign in Oncology: Preliminary Data of Newly Diagnosed Cancer Outpatients of Oporto Hospital CUF. Gazeta Médica 4: 1–7. [Google Scholar] [CrossRef] [Green Version]
- Ownby, Kristin K. 2019. Use of the Distress Thermometer in Clinical Practice. Journal of the Advanced Practitioner in Oncology 10: 175–79. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6750919/ (accessed on 14 June 2021).
- Pandya, Samta P. 2019. Meditation for Meaning in Life and Happiness of Older Adults: A Multi-City Experiment of the Brahma Kumaris’ Raja Yoga Practice. Journal of Religion, Spirituality & Aging 31: 282–304. [Google Scholar] [CrossRef]
- Pereira, Graziele Batista, Alice Madalena Silva Martins Gomes, and Riza Rute de Oliveira. 2017. Impact of Breast Cancer Treatment on the Self-Image and Affective Relationships of Matectomized Women. Life Style 4: 99–119. [Google Scholar] [CrossRef]
- Phatak, Mrunal S., Tara G. Chawla, and Pallavi S. Phatak. 2017. Effect of Raja Yoga Meditation on Glycaemic Status in Type 2 Diabetes Mellitus. International Journal of Research in Medical Sciences 5: 4385–88. [Google Scholar] [CrossRef] [Green Version]
- Pillai, Radhakrishna R., Anil Kumar G., and Krishnadas Nanath. 2015. Role of Self-managing Leadership in Crisis Management: An Empirical Study on the Effectiveness of Rajayoga. IIM Kozhikode Society & Management Review 4: 15–37. [Google Scholar] [CrossRef]
- Polo, Larissa Helena Vitoriano, and Marcia Wanderley de Moraes. 2009. The Zubrod Performance Status and the Karnofsky Index in Quality of Life Evaluation of Children with Cancer. Einstein 7: 314–21. Available online: http://apps.einstein.br/revista/arquivos/PDF/1241-Einstein%20v7n3p314-21_1.pdf (accessed on 14 June 2021).
- Portella, Caio Fábio Schlechta, Isabel Cristina Espósito Sorpreso, Alanda Silva Menezes de Assis, Luiz Carlos de Abreu, José Maria Soares Junior, Edmund Chada Baracat, Sandra Dircinha Teixeira de Araujo Moraes, and Ana Cristina D’Andretta Tanaka. 2020. Meditation as an Approach to Lessen Menopausal Symptoms and Insomnia in Working Women Undergoing the Menopausal Transition Period: A Randomized Controlled Trial. Advances in Integrative Medicine 26: 1–26. [Google Scholar] [CrossRef]
- Rajoria, Kshipra, and Sarvesh Kumar Singh. 2017. Therapeutic Benefits of Raj Yoga—A Review. Indian Journal of Traditional Knowledge 16: 88–95. Available online: http://nopr.niscair.res.in/bitstream/123456789/42275/1/IJTK%2016%28Suppl%29%2088-95.pdf (accessed on 14 June 2021).
- Regino, Patrícia Afonso, Thaís Cristina Elias, Caroline Freitas Silveira, Cristina Wide Pissetti, Gilberto de Araújo Pereira, and Sueli Riul da Silva. 2018. Anxiety, Depression and Quality of Life of Patients with Breast and Gynecological Cancer in Face of the Effects of Antineoplastic Chemotherapy. Ciência, Cuidado e Saúde 17: 1–6. [Google Scholar] [CrossRef] [Green Version]
- Saha, Felix J., Alexander Brüning, Cyrus Barcelona, Arndt Büssing, Jost Langhorst, Gustav Dobos, Romy Lauche, and Holger Cramer. 2016. Integrative Medicine for Chronic Pain: A Cohort Study Using a Process-Outcome Design in the Context of a Department for Internal and Integrative Medicine. Medicine 95: 41–52. [Google Scholar] [CrossRef] [PubMed]
- Santiago, Lucas, Pedro Reggiani Anzuatégui, José Paulo Agner Ribeiro, Maurício Carrilho Filon, Glauco José Pauka Mello, and Ana Valéria Brunetti Rigolino. 2019. Assessing psychosocial Distress in bone metastases treated with endoprosthesis. Acta Ortopedica Brasileira 27: 257–60. [Google Scholar] [CrossRef] [Green Version]
- Santo, Helena Espirito, and Fernanda Daniel. 2017. Calculating and Reporting Effect Sizes on Scientific Papers (1): P < 0.05 Limitations in the Analysis of Mean Differences of two Groups. Revista Portuguesa de Investigação Comportamental e Social 1: 3–16. [Google Scholar] [CrossRef]
- Sarenmalm, Elisabeth Kenne, Lena B. Mårtensson, Bengt A. Andersson, Per Karlsson, and Ingrid Bergh. 2017. Mindfulness and its Efficacy for Psychological and Biological Responses in Women with Breast Cancer. Cancer Medicine 6: 1108–22. [Google Scholar] [CrossRef]
- Schell, Lisa K., Ina Monsef, Achim Wöckel, and Nicole Skoetz. 2019. Mindfulness-based Stress Reduction for Women Diagnosed with Breast Cancer. Cochrane Database of Systematic Reviews 3: CD011518. [Google Scholar] [CrossRef] [PubMed]
- Sharma, Kanishka, Peter Achermann, Bhawna Panwar, Shrikant Sahoo, Ramakrishnan Angarai, Roberto D. Pascual-Marqui, and Pascal Faber. 2020. Brain-electric Activity During Eyes Open Brahma Kumaris Rajayoga Meditation. MindRxiv. [Google Scholar] [CrossRef]
- Shim, Eun-Jung, Donghee Jeong, Hyeong-Gon Moon, Dong-Young Noh, So-Youn Jung, Eunsook Lee, Zisun Kim, Hyun Jo Youn, Jihyoung Cho, and Jung Eun Lee. 2020. Profiles of Depressive Symptoms and the Association with Anxiety and Quality of Life in Breast Cancer Survivors: A Latent Profile Analysis. Quality of Life Research 29: 421–29. [Google Scholar] [CrossRef] [PubMed]
- Silva, Araceli Vicente da, Eliana Zandonade, and Maria Helena Costa Amorim. 2017. Anxiety and coping in women with breast cancer in chemotherapy. Revista Latino-Americana de Enfermagem 25: e2891. [Google Scholar] [CrossRef] [Green Version]
- Sociedade Brasileira de Cardiologia (SBC). 2016. III Diretrizes Da Sociedade Brasileira de Cardiologia sobre análise e emissão de laudos Eletrocardiográficos. Arquivos Brasileiros de Cardiologia 106: 1–38. [Google Scholar] [CrossRef]
- Sociedade Brasileira de Cardiologia (SBC). 2019. 7th Brazilian Guideline of Arterial Hypertension: Chapter 2—Diagnosis and Classification. Arquivos Brasileiros de Cardiologia 107: 1–104. [Google Scholar] [CrossRef]
- Soo, Mary Scott, Jennifer A. Jarosz, Anava A. Wren, Adrianne E. Soo, Yvonne M. Mowery, Karen S. Johnson, Sora C. Yoon, Connie Kim, E. Shelley Hwang, Francis J. Keefe, and et al. 2016. Support Care cancer imaging-guided core-needle breast biopsy: Impact of meditation and music interventions on patient anxiety, pain, and fatigue. Journal of the American College of Radiology 13: 526–34. [Google Scholar] [CrossRef]
- Toutain, Thaise Graziele L. O., Raphael Rosário, Carlos Maurício Cardeal Mendes, and Eduardo Pondé de Sena. 2019. Alfa no estado alterado de consciência: Meditação raja yoga. Revista de Ciencias Medicas e Biologicas 18: 38–43. [Google Scholar] [CrossRef]
- Veronese, Felipe, and Marcelo Nonaka Frade. 2021. Prevalência de ansiedade e depressão em pacientes submetidos à quimioterapia e/ou radioterapia. Fag Journal of Health (FJH) 3: 38–43. [Google Scholar] [CrossRef]
- Villar, Raquel Rey, Salvador Pita Fernández, Carmen Cereijo Garea, Maria Teresa Seoane Pillado, Vanesa Balboa Barreiro, and Cristina González Martín. 2017. Quality of life and anxiety in women with breast cancer before and after treatment. Revista Latino-Americana de Enfermagem 25: e2958. [Google Scholar] [CrossRef]
- Vivekananda, Swami. 2009. Raja Yoga—O Caminho Real. Available online: https://docplayer.com.br/19729837-Raja-yoga-o-caminho-real.html (accessed on 14 July 2021).
- Yee, Melissa K., Susan M. Sereika, Catherine M. Bender, Adam M. Brufsky, Mary C. Connolly, and Margaret Q. Rosenzweig. 2017. Symptom incidence, distress, cancer-related distress, and adherence to chemotherapy among African American women with breast cancer. Cancer 123: 2061–69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zerati, Antonio Eduardo, Nelson Wolosker, Nelson de Luccia, and Pedro Puech-Leão. 2017. Totally Implantable Venous Catheters: History, Implantation Technique and Complications. Jornal Vascular Brasileiro 16: 128–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]








| Variables | Total n = 50 | Group | p-Value | |
|---|---|---|---|---|
| Intervention n = 25 | Control n = 25 | |||
| Median (P25–P75) | Median (P25–P75) | Median (P25–P75) | ||
| Age (years) | 47 (40.8–56) | 46 (38.5–56) | 47 (43.5–55.5) | 0.4311 1 |
| n (%) | n (%) | n (%) | ||
| Ethnicity | 0.2082 2 | |||
| White | 36 (72.0) | 16 (64.0) | 20 (80.0) | |
| Non-white | 14 (28.0) | 9 (36.0) | 5 (20.0) | |
| Marital status | 0.7772 2 | |||
| Living with a partner | 27 (54.0) | 14 (56.0) | 13 (52.0) | |
| Living without a partner | 23 (46.0) | 11 (44.0) | 12 (48.0) | |
| Educational level | 1.0002 2 | |||
| Low | 12 (24.0) | 6 (24.0) | 6 (24.0) | |
| High * | 38 (76.0) | 19 (76.0) | 19 (76.0) | |
| Occupation | 0.2392 3 | |||
| Unpaid | 18 (36.0) | 11 (44.0) | 7 (28.0) | |
| Paid | 32 (64.0) | 14 (56.0) | 18 (72.0) | |
| Family income | 0.7652 3 | |||
| Up to 1 minimum wage | 33 (66.0) | 17 (68.0) | 16 (64.0) | |
| >1 minimum wage | 17 (34.0) | 8 (32.0) | 9 (36.0) | |
| Religion | 0.5292 2 | |||
| Catholic | 36 (72.0) | 17 (68.0) | 19 (76.0) | |
| Protestant | 14 (28.0) | 8 (32.0) | 6 (24.0) | |
| Variables | Total n = 50 | Group | p-Value | |
|---|---|---|---|---|
| Intervention n = 25 | Control n = 25 | |||
| Median (P25-P75) | Median (P25-P75) | Median (P25-P75) | ||
| Age at menarche | 13 (12.5–15) | 14 (13–14) | 13 (12–15) | 0.8621 |
| Age at menopause | 46 (44.8–49.3) | 46 (45–50.0) | 45 (39–49) | 0.2751 1 |
| n (%) | n (%) | n (%) | ||
| Ever having had children | 1.000 2 | |||
| Yes | 38 (76.0) | 19 (76.0) | 19 (76.0) | |
| No | 12 (24.0) | 6 (24.0) | 6 (24.0) | |
| First pregnancy after 30 years | 0.699 3 | |||
| Yes | 7 (15.7) | 3 (13.0%) | 4 (18.2%) | |
| No | 38 (84.4) | 20 (87.0%) | 18 (81.8%) | |
| Ever having breastfed | 0.488 3 | |||
| Yes | 38 (95.0) | 19 (90.5) | 19 (100.0) | |
| No | 2 (5.0) | 2 (9.5) | 0 (0.0) | |
| Use of oral contraceptives | 0.564 2 | |||
| Yes | 20 (40.0) | 11 (44.0) | 9 (36.0) | |
| No | 30 (60.0) | 14 (56.0) | 16 (64.0) | |
| Physical activity | 0.508 2 | |||
| Yes | 12 (24.0) | 5 (20.0) | 7 (28.0) | |
| No | 38 (76.0) | 20 (80.0) | 18 (72.0) | |
| BMI | 0.447 2 | |||
| Adequate | 14 (28.0) | 5 (20.0) | 9 (36.0) | |
| Overweight | 22 (44.0) | 12 (48.0) | 10 (40.0) | |
| Obesity | 14 (28.0) | 8 (32.0) | 6 (24.0) | |
| Habits | 0.429 3 | |||
| Smoking | 4 (57.1) | 2 (100.0) | 2 (40.0) | |
| Alcohol drinking | 3 (42.9) | 0 (0.0) | 3 (60.0) | |
| Having a relative with breast cancer | 0.306 2 | |||
| Yes | 11 (22.0) | 7 (28.0) | 4 (16.0) | |
| No | 39 (78.0) | 18 (72.0) | 21 (84.0) | |
| Variables | Total n (%) | Group | p-Value | |
|---|---|---|---|---|
| Intervention n (%) | Control n (%) | |||
| Having breast surgery | ||||
| Yes | 7 (14.0) | 3 (12.0) | 4 (16.0) | 1.00 |
| No | 43 (86.0) | 22 (88.0) | 21 (84.0) | |
| Affected breast | ||||
| Right | 26 (52.0) | 13 (52.0) | 13 (52.0) | 1.00 |
| Left | 24 (48.0) | 12 (48.0) | 12 (48.0) | |
| Surgery information | ||||
| Total mastectomy | 2 (4.0) | 1 (4.0) | 1 (4.0) | 1.00 |
| Quadrandectomy | 1 (2.0) | 0 (0.0) | 1 (4.0) | |
| Sectorectomy | 3 (6.0) | 2 (8.0) | 1 (4.0) | |
| Lymphaticectomy | 5 (10.0) | 3 (12.0) | 2 () 8.0 | |
| Breast reconstruction | 1 (2.0) | 1 (4.0) | 0 (0.0) | |
| Current treatment | ||||
| Chemotherapy | 48 (96.0) | 23 (92.0) | 25 (100.0) | 1.00 |
| Radiotherapy | 4 (8.0) | 2 (8.0) | 2 (8.0) | |
| Surgery | 5 (10.0) | 2 (8.0) | 3 (12.0) | |
| Hormone therapy | 4 (8.0) | 3 (12.0) | 1 (4.0) | |
| Immunotherapy | 4 (8.0) | 1 (4.0) | 3 (12.0) | |
| Port-cath implantation | ||||
| Yes | 21 (42.0) | 10 (40.0) | 11 (44.0) | |
| No | 29 (59.0) | 15 (60.0) | 14 (56.0) | |
| Metastasis | ||||
| Yes | 7 (14.0) | 4 (16.0) | 3 (12.0) | 1.00 |
| No | 43 (86.0) | 21 (84.0) | 22 (88.0) | |
| Purpose of chemotherapy | ||||
| Neoadjuvant | 37 (74.0) | 18 (72.0) | 19 (76.0) | 1.00 |
| Adjuvant | 6 (12.0) | 3 (12.0) | 3 (12.0) | |
| Palliative | 7 (14.0) | 4 (16.0) | 3 (12.0) | |
| TNM staging | ||||
| IA—T1 N0 M0 | 1 (2.0) | 0 (0.0) | 1 (4.0) | 1.00 |
| IIA—T1 N1 M0 | 1 (2.0) | 0 (0.0) | 1 (4.0) | |
| IIA—T2 N0 M0 | 11 (22.0) | 5 (20.0) | 6 (24.0) | |
| IIB—T2 N1 M0 | 8 (16.0) | 2 (8.0) | 6 (24.0) | |
| IIB—T3 N0 M0 | 5 (10.0) | 1 (4.0) | 4 (16.0) | |
| IIIA—T2 N2 M0 | 2 (4.0) | 0 (0.0) | 2 (8.0) | |
| IIIA—T3 N1 M0 | 7 (14.0) | 6 (24.0) | 1 (4.0) | |
| IIIA—T3 N2 M | 1 (2.0) | 1 (4.0) | 0 (0.0) | |
| IIIB—T4N0 | 1 (2.0) | 1 (4.0) | 0 (0.0) | |
| IIIB—T4N1 | 3 (6.0) | 3 (12.0) | 0 (0.0) | |
| IIIB—T4N2 | 2 (4.0) | 2 (8.0) | 0 (0.0) | |
| IV—TX NX M1 | 8 (16.0) | 4 (16.0) | 4 (16.0) | |
| Assessment of Distress Level | Intervention Group | Control Group | ||||||
|---|---|---|---|---|---|---|---|---|
| Total n (%) | Presence of Distress after | Absence of Distress after | p-Value * | Total n (%) | Presence of Distress after | Absence of Distress after | p-Value * | |
| Presence of distress before | 23 (100) | 13 (56.5) | 10 (43.5) | 0.002 | 21 (100) | 21 (100.0) | 0 (4.0) | 1.000 |
| Absence of distress before | 2 (100) | 0 (0.0) | 2 (100.0) | 4 (100) | 0 (0.0) | 4 (100.0) | ||
| Anxiety | Intervention Group | Control Group | ||||||
|---|---|---|---|---|---|---|---|---|
| Total n (%) | Presence of Anxiety after n (%) | Absence of Anxiety after n (%) | p-Value * | Total n (%) | Presence of Anxiety after n (%) | Absence of Anxiety after n (%) | p-Value * | |
| Presence of anxiety before | 9 (100) | 1 (11.1) | 8 (88.9) | 0.008 | 8 (100.0) | 7 (87.5) | 1 (12.5) | 1.000 |
| Absence of anxiety before | 16 (100) | 0 (0.0) | 16 (100.0) | 17 (100.0) | 1 (5.9) | 16 (94.1) | ||
| Variables | Intervention Group | Control Group | Cohen’s d | Effect Size | |
|---|---|---|---|---|---|
| Distress thermometer | 1st moment | 6.52 (± 2.23) | 6.70 (± 2.49) | −0.079 | −0.03 |
| 2nd moment | 3.72 (± 1.54) | 6.75 (± 2.41) | −1.49 | −0.59 | |
| Anxiety | 1st moment | 6.32 (± 4.62) | 6.24 (± 4.69) | 0.017 | 0.008 |
| 2nd moment | 3.12 (± 2.55) | 6.20 (± 4.70) | −0.814 | −0.37 | |
| Depression | 1st moment | 5.48 (± 4.32) | 5.16 (± 4.20) | 0.075 | 0.03 |
| 2nd moment | 3.16 (± 2.62) | 5.76 (± 4.17) | −0.746 | −0.34 | |
| Systolic blood pessure | 1st moment | 121.64 (± 19.28) | 132.40 (± 19.85) | −0.549 | −0.26 |
| 2nd moment | 117.8 (± 15.53) | 132.24 (± 11.68) | −1.05 | −0.46 | |
| Diastolic blood pressure | 1st moment | 70.08 (± 19.98) | 78.12 (± 17.01) | −0.433 | −0.21 |
| 2nd moment | 72.28 (± 9.57) | 85.20 (± 7.57) | −1.497 | −0.59 | |
| HR | 1st moment | 82.92 (±12.43) | 79.62 (±10.80) | 0.283 | 0.14 |
| 2nd moment | 79.08 (±9.52) | 85.50 (±9.78) | −0.66 | −0.31 | |
| SPO2 | 1st moment | 97.72 (±1.02) | 97.12 (±2.17) | 0.353 | 0.17 |
| 2nd moment | 97.80 (±0.70) | 97.25 (±0.94) | 0.663 | 0.31 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Araújo, R.V.; Fernandes, A.F.C.; Campelo, R.C.V.; Silva, R.A.; Nery, I.S. Effect of Raja Yoga Meditation on the Distress and Anxiety Levels of Women with Breast Cancer. Religions 2021, 12, 590. https://doi.org/10.3390/rel12080590
Araújo RV, Fernandes AFC, Campelo RCV, Silva RA, Nery IS. Effect of Raja Yoga Meditation on the Distress and Anxiety Levels of Women with Breast Cancer. Religions. 2021; 12(8):590. https://doi.org/10.3390/rel12080590
Chicago/Turabian StyleAraújo, Raquel Vilanova, Ana Fátima Carvalho Fernandes, Regina Célia Vilanova Campelo, Renan Alves Silva, and Inez Sampaio Nery. 2021. "Effect of Raja Yoga Meditation on the Distress and Anxiety Levels of Women with Breast Cancer" Religions 12, no. 8: 590. https://doi.org/10.3390/rel12080590
APA StyleAraújo, R. V., Fernandes, A. F. C., Campelo, R. C. V., Silva, R. A., & Nery, I. S. (2021). Effect of Raja Yoga Meditation on the Distress and Anxiety Levels of Women with Breast Cancer. Religions, 12(8), 590. https://doi.org/10.3390/rel12080590






