The Role of Religious Behavior in Health Self-Management: A Community-Based Participatory Research Study
Abstract
1. Introduction
1.1. Community-Based Participatory Research (CBPR)
1.2. Geographical Factors Affecting Health Behavior
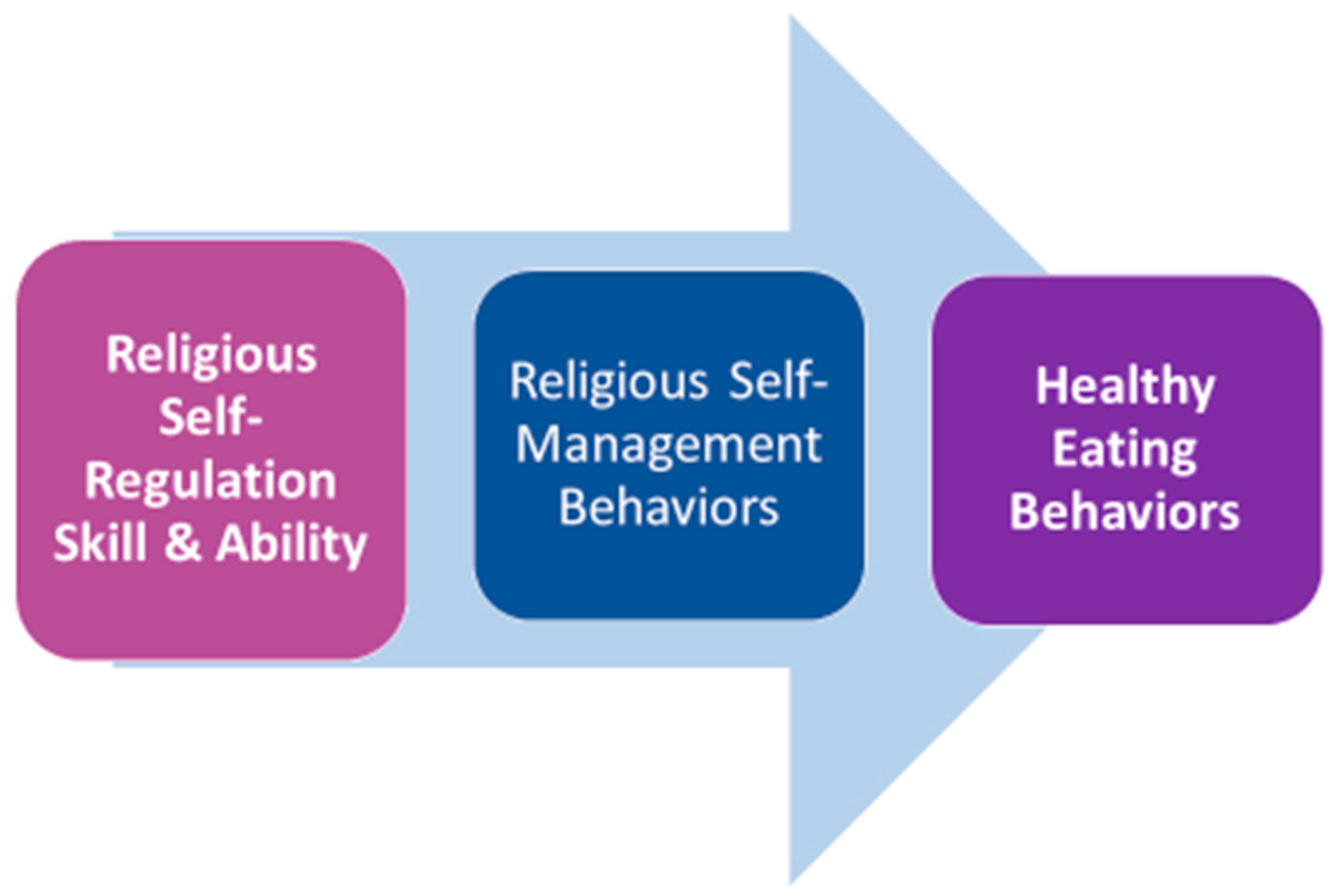
1.3. Religious Self-Regulation
1.4. Religious Behavior
1.5. Fast Food Intake
2. Results
3. Discussion
4. Methods and Materials
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Abernethy, Alexis D., H. Theresa Chang, Larry Seidlitz, James S. Evinger, and Paul R. Duberstein. 2002. Religious coping and depression among spouses of people with lung cancer. Psychosomatics 43: 456–63. [Google Scholar] [CrossRef] [PubMed]
- Agboola, Fayomi, R. Patti Herring, Mark Ghamsary, Daniel Handysides, Naomi Modeste, and Keiji Oda. 2017. Enhancing culture of health in food deserts: Reports of a community supported agriculture study in San Bernardino, CA. International Journal of Food Research 4: 1–11. [Google Scholar]
- Allport, Gordon W., and J. Michael Ross. 1967. Personal religious orientation and prejudice. Journal of Personality and Social Psychology 5: 432–43. [Google Scholar] [CrossRef] [PubMed]
- Andrade, Chittaranjan, and Rajiv Radhakrishnan. 2009. Prayer and healing: A medical and scientific perspective on randomized controlled trials. Indian Journal of Psychiatry 51: 247. [Google Scholar] [CrossRef] [PubMed]
- Ansari, Serene, Erica G. Soltero, Elizabeth Lorenzo, and Rebecca E. Lee. 2017. The impact of religiosity on dietary habits and physical activity in minority women participating in the Health is Power (HIP) study. Preventive Medicine Reports 5: 210–13. [Google Scholar] [CrossRef] [PubMed]
- Arredondo, Elva M., John P. Elder, Guadalupe X. Ayala, and Nadia R. Campbell. 2005. Is church attendance associated with Latinas’ health practices and self-reported health? American Journal of Health Behavior 29: 502–11. [Google Scholar] [CrossRef] [PubMed]
- Ayton, Darshini, Lenore Manderson, and Ben J. Smith. 2017. Barriers and challenges affecting the contemporary church’s engagement in health promotion. Health Promotion Journal of Autrailia 28: 52–58. [Google Scholar] [CrossRef] [PubMed]
- Balbuena, Lloyd, Marilyn Baetz, and Rudy Bowen. 2013. Religious attendance, spirituality, and major depression in Canada: A 14-year follow-up study. The Canadian Journal of Psychiatry 58: 225–32. [Google Scholar] [CrossRef] [PubMed]
- Beezhold, Bonnie L., Carol S. Johnston, and Deanna R. Daigle. 2010. Vegetarian diets are associated with healthy mood states: A cross-sectional study in seventh day adventist adults. Nutrition Journal 9: 26. [Google Scholar] [CrossRef] [PubMed]
- Behere, Prakash B., Anweshak Das, Richa Yadav, and Aniruddh P. Behere. 2013. Religion and mental health. Indian Journal of Psychiatry 55 Suppl. 2: S187. [Google Scholar] [CrossRef] [PubMed]
- Bomback, Andrew S., Vimal K. Derebail, David A. Shoham, Cheryl A. Anderson, Lyn M. Steffen, Wayne D. Rosamond, and Abhijit V. Kshirsagar. 2010. Sugar-sweetened soda consumption, hyperuricemia, and kidney disease. Kidney International 77: 609–16. [Google Scholar] [CrossRef] [PubMed]
- Bryan, Valerie, Willette Brye, Kenneth Hudson, Leevones Dubose, Shantisha Hansberry, and Martha Arrieta. 2014. Investigating health disparities through community-based participatory research: Lessons learned from a process evaluation. Social Work in Public Health 29: 318–34. [Google Scholar] [CrossRef] [PubMed]
- Cacari-Stone, Lisa, Nina Wallerstein, Analilia P. Garcia, and Meredith Minkler. 2014. The promise of community-based participatory research for health equity: A conceptual model for bridging evidence with policy. American Journal of Public Health 104: 1615–23. [Google Scholar] [CrossRef] [PubMed]
- Cargo, Margaret, and Shawna L. Mercer. 2008. The Value and Challenges of Participatory Research: Strengthening Its Practice. Annual Review of Public Health 29: 325–50. [Google Scholar] [CrossRef] [PubMed]
- Clark, Eddie M., Jin Huang, David L. Roth, Emily Schulz, Beverly R. Williams, and Cheryl L. Holt. 2018. The relationship between religious beliefs and behaviors and changes in spiritual health locus of control over time in a national sample of African Americans. Mental Health, Religion & Culture 20: 449–63. [Google Scholar] [CrossRef]
- Clements, Andrea D., Tifani R. Fletcher, Natalie A. Cyphers, Anna V. Ermakova, and Beth Bailey. 2015. RSAS-3: Validation of a Very Brief Measure of Religious Commitment for Use in Health Research. Journal of Religion & Health 54: 134–52. [Google Scholar] [CrossRef]
- Çoruh, Başak, Hana Ayele, Meredith Pugh, and Thomas Mulligan. 2005. Does religious activity improve health outcomes? A critical review of the recent literature. Explore: The Journal of Science and Healing 1: 186–91. [Google Scholar] [CrossRef] [PubMed]
- Cummings, Jeremy P., and Kenneth I. Pargament. 2010. Medicine for the spirit: Religious coping in individuals with medical conditions. Religions 1: 28–53. [Google Scholar] [CrossRef]
- De Las Nueces, Denise, Karen Hacker, Ann DiGirolamo, and LeRoi S. Hicks. 2012. A systematic review of community-based participatory research to enhance clinical trials in racial and ethnic minority groups. Health Services Research 47: 1363–86. [Google Scholar] [CrossRef] [PubMed]
- Fincham, Frank D., Gregory S. Seibert, Ross W. May, Colwick M. Wilson, and Zephon D. Lister. 2018. Religious coping and glycemic control in couples with type 2 diabetes. Journal of Marital and Family Therapy 44: 138–49. [Google Scholar] [CrossRef] [PubMed]
- George, Linda K., Christopher G. Ellison, and David B. Larson. 2002. Explaining the relationships between religious involvement and health. Psychological Inquiry 13: 190–200. [Google Scholar] [CrossRef]
- Gillum, R. Frank, and Deborah D. Ingram. 2006. Frequency of attendance at religious services, hypertension, and blood pressure: The Third National Health and Nutrition Examination Survey. Psychosomatic Medicine 68: 382–85. [Google Scholar] [CrossRef] [PubMed]
- Gillum, Frank, and Carla Williams. 2009. Associations between breast cancer risk factors and religiousness in American women in a national health survey. Journal of Religion and Health 48: 178–88. [Google Scholar] [CrossRef] [PubMed]
- Gunderson, Gary. 1997. Deeply Woven Roots: Improving the Quality of Life in Your Community. Minneapolis: Fortress Press. [Google Scholar] [CrossRef]
- Hafizi, Sina, Harold Koenig, and Doaa Ahmed Khalifa. 2015. Psychometric properties of the Farsi version of Hoge Intrinsic Religiosity Scale in muslims: A brief report. Pastoral Psychology 64: 839–45. [Google Scholar] [CrossRef]
- Hall, Daniel E., Keith G. Meador, and Harold Koenig. 2008. Measuring religiousness in health research: Review and critique. Journal of Religion & Health 2008: 134–63. [Google Scholar] [CrossRef]
- Helm, Hughes M., Judith C. Hays, Elizabeth P. Flint, Harold G. Koenig, and Dan G. Blazer. 2000. Does private religious activity prolong survival? A six-year follow-up study of 3,851 older adults. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 55: M400–5. [Google Scholar] [CrossRef]
- Higgs, Suzanne, and Jason Thomas. 2016. Social influences on eating. Current Opinion in Behavioral Sciences 9: 1–6. [Google Scholar] [CrossRef]
- Hill, Peter C., and Kenneth I. Pargament. 2008. Advances in the conceptualization and measurement of religion and spirituality: Implications for physical and mental health research. The American Psychologist 58: 64–74. [Google Scholar] [CrossRef]
- Hilmers, Angela, David C. Hilmers, and Jayna Dave. 2012. Neighborhood disparities in access to healthy foods and their effects on environmental justice. American Journal of Public Health 102: 1644–54. [Google Scholar] [CrossRef] [PubMed]
- Hoge, Dean R. 1972. A validated intrinsic religious motivation scale. Journal for the Scientific Study of Religion 11: 369–76. [Google Scholar] [CrossRef]
- Holkup, Patricia A., Toni Tripp-Reimer, Emily Matt Salois, and Clairann Weinert. 2004. Community-based participatory research: An approach to intervention research within an American Indian community. Advances in Nursing Science 27: 162–75. [Google Scholar] [CrossRef] [PubMed]
- Holt, Cheryl L., Eddie M. Clark, Matthew W. Kreuter, and Doris M. Rubio. 2003. Spiritual health locus of control and breast cancer beliefs among urban African American women. Health Psychology 22: 294–99. [Google Scholar] [CrossRef] [PubMed]
- Holt, Cheryl L., David L. Roth, Jin Huang, and Eddie M. Clark. 2015. Gender differences in the roles of religion and locus of control on alcohol use and smoking among African Americans. Journal of Studies on Alcohol and Drugs 76: 482–92. [Google Scholar] [CrossRef] [PubMed]
- Hvidt, Niels Christian, Dorte Hvidtjørn, Kaare Christensen, Jesper Bo Nielsen, and Jens Søndergaard. 2017. Faith moves mountains-mountains move faith: Two opposite epidemiological forces in research on religion and health. Journal of Religion & Health 56: 294–304. [Google Scholar] [CrossRef]
- Israel, Barbara A., Amy J. Schulz, Edith A. Parker, and Adam B. Becker. 2001. Community-based participatory research: Policy recommendations for promoting a partnership approach in health research. Education for Health 14: 182–97. [Google Scholar] [CrossRef] [PubMed]
- Israel, Barbara A., Chris M. Coombe, Rebecca R. Cheezum, Amy J. Schulz, Robert J. McGranaghan, Richard Lichtenstein, Angela G Reyes, Jaye Clement, and Akosua Burris. 2010. Community-based participatory research: A capacity-building approach for policy advocacy aimed at eliminating health disparities. American Journal of Public Health 100: 2094–102. [Google Scholar] [CrossRef] [PubMed]
- Jagosh, Justin, Paula L. Bush, Jon Salsberg, Ann C. Macaulay, Trish Greenhalgh, Geoff Wong, Margaret Cargo, Lawrence W. Green, Carol P. Herbert, and Pierre Pluye. 2015. A realist evaluation of community-based participatory research: Partnership synergy, trust building and related ripple effects. BMC Public Health 15: 725. [Google Scholar] [CrossRef] [PubMed]
- Koenig, Harold G. 1993. Religion and aging. Reviews in Clinical Gerontology 3: 195–203. [Google Scholar] [CrossRef]
- Koenig, Harold G. 2004. Religion, spirituality, and medicine: Research findings and implications for clinical practice. The Southern Medical Journal 97: 1194–200. [Google Scholar] [CrossRef] [PubMed]
- Koenig, Harold G., and Arndt Büssing. 2010. The Duke University Religion Index (DUREL): A five-item measure for use in epidemological studies. Religions 1: 78–85. [Google Scholar] [CrossRef]
- Koenig, Harold, George R. Parkerson, Jr., and Keith G. Meador. 1997. Religion index for psychiatric research. The American Journal of Psychiatry 154: 885–86. [Google Scholar] [CrossRef] [PubMed]
- Koenig, Harold G., Kenneth I. Pargament, and Julie Nielsen. 1998. Religious coping and health status in medically ill hospitalized older adults. The Journal of Nervous and Mental Disease 186: 513–21. [Google Scholar] [CrossRef] [PubMed]
- Koenig, Harold, Harold George Koenig, Dana King, and Verna B. Carson. 2012. Handbook of Religion and Health. New York: Oxford University Press. [Google Scholar]
- Krause, Neal, Gail Ironson, and Kenneth I. Pargament. 2016. Spiritual struggles and resting pulse rates: Does strong distress tolerance promote more effective coping? Personality and Individual Differences 98: 261–65. [Google Scholar] [CrossRef]
- Larson, Nicole I., Mary T. Story, and Melissa C. Nelson. 2009. Neighborhood environments: Disparities in access to healthy foods in the US. American Journal of Preventive Medicine 36: 74–81. [Google Scholar] [CrossRef] [PubMed]
- Levin, Jeff. 2013. Engaging the faith community for public health advocacy: An agenda for the Surgeon General. Journal of Religion & Health 52: 368–85. [Google Scholar] [CrossRef]
- Malik, Vasanti S., and Frank B. Hu. 2015. Fructose and cardiometabolic health: What the evidence from sugar-sweetened beverages tells us. Journal of the American College of Cardiology 66: 1615–24. [Google Scholar] [CrossRef] [PubMed]
- Maselko, Joanna, Stephen E. Gilman, and S. Buka. 2009. Religious service attendance and spiritual well-being are differentially associated with risk of major depression. Psychological Medicine 39: 1009–17. [Google Scholar] [CrossRef] [PubMed]
- McCullough, Michael E., and Brian L. B. Willoughby. 2009. Religion, self-regulation, and self-control: Associations, explanations, and implications. Psychological Bulletin 135: 69. [Google Scholar] [CrossRef] [PubMed]
- Mekonnen, Tekeshe A., Michelle C. Odden, Pamela G. Coxson, David Guzman, James Lightwood, Y. Claire Wang, and Kirsten Bibbins-Domingo. 2013. Health benefits of reducing sugar-sweetened beverage intake in high risk populations of California: Results from the cardiovascular disease (CVD) policy model. PLoS ONE 8: e81723. [Google Scholar] [CrossRef] [PubMed]
- Morland, Kimberly B., and Kelly R. Evenson. 2009. Obesity prevalence and the local food environment. Health & Place 15: 491–95. [Google Scholar] [CrossRef]
- Mosqueiro, Bruno Paz, Neusa Sica de Rocha, and Marcelo Pio de Almeida Fleck. 2015. Intrinsic Religiosity, Resilience, Quality of Life, and Suicide Risk in Depressed Inpatients. Journal of Affective Disorders 179: 128–33. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, Dariush. 2016. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: A comprehensive review. Circulation 133: 187–225. [Google Scholar] [CrossRef] [PubMed]
- Mpofu, Elias. 2018. How religion frames health norms: A structural theory approach. Religions 9: 119. [Google Scholar] [CrossRef]
- Nam, Sanggon. 2013. The effects of religious attendance and obesity on health by race/ethnicity. Osong Public Health and Research Perspectives 4: 81–88. [Google Scholar] [CrossRef] [PubMed]
- Norton, Maria C., Archana Singh, Ingmar Skoog, Christopher Corcoran, JoAnn T. Tschanz, Peter P. Zandi, John C. S. Breitner, Kathleen A. Welsh-Bohmer, and David C. Steffens. 2008. Church attendance and new episodes of major depression in a community study of older adults: The Cache County Study. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 63: P129–37. [Google Scholar] [CrossRef]
- O’Brien, Matthew J., and Robert C. Whitaker. 2011. The role of community-based participatory research to inform local health policy: A case study. Journal of General Internal Medicine 26: 1498–501. [Google Scholar] [CrossRef] [PubMed]
- Oexmann, Mary J., Rhoda Ascanio, and Brent M. Egan. 2001. Efficacy of a Church-Based Intervention on Cardiovascular risk Reduction. Ethnicity & Disease 11: 817–22. [Google Scholar]
- Olson, Michael M., Dorothy B. Trevino, Jenenne A. Geske, and Harold Vanderpool. 2012. Religious coping and mental health outcomes: An exploratory study of socioeconomically disadvantaged patients. Explore: The Journal of Science and Healing 8: 172–76. [Google Scholar] [CrossRef] [PubMed]
- Orlich, Michael J., Pramil N. Singh, Joan Sabaté, Jing Fan, Lars Sveen, Hannelore Bennett, Synnove F. Knutsen, W. Lawrence Beeson, Karen Jaceldo-Siegl, and Terry L. Butler. 2015. Vegetarian dietary patterns and the risk of colorectal cancers. JAMA Internal Medicine 175: 767–76. [Google Scholar] [CrossRef] [PubMed]
- Pargament, Kenneth I., Joseph Kennell, William Hathaway, Nancy Grevengoed, Jon Newman, and Wendy Jones. 1988. Religion and the problem-solving process: Three styles of coping. Journal for the Scientific Study of Religion, 90–104. [Google Scholar] [CrossRef]
- Pargament, Kenneth, Margaret Feuille, and Donna Burdzy. 2011. The Brief RCOPE: Current psychometric status of a short measure of religious coping. Religions 2: 51–76. [Google Scholar] [CrossRef]
- Persynaki, Angeliki, Spyridon Karras, and Claude Pichard. 2017. Unraveling the metabolic health benefits of fasting related to religious beliefs: A narrative review. Nutrition 35: 14–20. [Google Scholar] [CrossRef] [PubMed]
- Pirutinsky, Steven, David H. Rosmarin, and Cheryl L. Holt. 2012. Religious coping moderates the relationship between emotional functioning and obesity. Health Psychology 31: 394. [Google Scholar] [CrossRef] [PubMed]
- Plunkett, Robyn, Barbara Leipert, and Joanne Olson. 2016. Exploring the influence of social determinants, social capital, and health expertise on health and the rural church. Journal of Holistic Nursing 34: 236–43. [Google Scholar] [CrossRef] [PubMed]
- Rosinger, Asher, Kirsten Herrick, Jaime Gahche, and Sohyun Park. 2017. Sugar-Sweetened Beverage Consumption among US Youth, 2011–2014. NCHS Data Brief. Number 271. National Center for Health Statistics. Available online: https://www.cdc.gov/nchs/data/databriefs/db271.pdf (accessed on 13 April 2018).
- Ryan, Polly. 2009. Integrated theory of health behavior change: Background and intervention development. Clinical Nurse Specialist 23: 161. [Google Scholar] [CrossRef] [PubMed]
- Saint Onge, Jarron M., and Patrick M. Krueger. 2017. Health lifestyle behaviors among US adults. SSM-Population Health 3: 89–98. [Google Scholar] [CrossRef] [PubMed]
- San Bernardino County Board of Supervisors. 2015. Community Indicators Report 2015. Edited by San Bernardino Board of Supervisors. San Bernardino, California. Available online: http://cms.sbcounty.gov/portals/21/resources%20documents/cir_2015_report.pdf (accessed on 20 April 2018).
- San Bernardino County Board of Supervisors. 2016. Commnity Indicators Report 2016. Edited by San Bernardino Board of Supervisors. San Bernardino, California. Available online: http://cms.sbcounty.gov/Portals/21/Resources%20Documents/SB_2016_REPORT.ONLINE%20bookmarked.pdf?ver=2017-05-11-102049-407 (accessed on 20 April 2018).
- Schuster, Mark A., Bradley D. Stein, Lisa H. Jaycox, Rebecca L. Collins, Grant N. Marshall, Marc N. Elliott, Annie J. Zhou, David E. Kanouse, Janina L. Morrison, and Sandra H. Berry. 2001. A national survey of stress reactions after the September 11, 2001, terrorist attacks. New England Journal of Medicine 345: 1507–12. [Google Scholar] [CrossRef] [PubMed]
- Short, Susan E., and Stefanie Mollborn. 2015. Social determinants and health behaviors: Conceptual frames and empirical advances. Current Opinion in Psychology 5: 78–84. [Google Scholar] [CrossRef] [PubMed]
- Steffen, Patrick R., Alan L. Hinderliter, James A. Blumenthal, and Andrew Sherwood. 2001. Religious coping, ethnicity, and ambulatory blood pressure. Psychosomatic Medicine 63: 523–30. [Google Scholar] [CrossRef] [PubMed]
- Strawbridge, William J., Sarah J. Shema, Richard D. Cohen, and George A. Kaplan. 2001. Religious attendance increases survival by improving and maintaining good health behaviors, mental health, and social relationships. Annals of Behavioral Medicine 23: 68–74. [Google Scholar] [CrossRef] [PubMed]
- Tan, Min-Min, Carina K. Y. Chan, and Daniel D. Reidpath. 2013. Religiosity and spirituality and the intake of fruit, vegetable, and fat: A systematic review. Evidence-Based Complementary and Alternative Medicine 2013. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, Marie-Claude, Debbie H. Martin, Alex M. McComber, Amelia McGregor, and Ann C. Macaulay. 2018. Understanding Community-Based Participatory Research through a Social Movement Framework: A Case Study of the Kahnawake Schools Diabetes Prevention Project. BMC Public Health 18: 487. [Google Scholar] [CrossRef] [PubMed]
- Trevino, Kelly M., and Timothy R. McConnell. 2014. Religiosity and Religious Coping in Patients with Cardiovascular Disease: Change over Time and Associations with Illness Adjustment. Journal of Religion and Health 53: 1907–17. [Google Scholar] [CrossRef] [PubMed]
- United States Census Bureau. 2014. San Bernardino County, California. Available online: https://www.census.gov/quickfacts/fact/table/sanbernardinocountycalifornia/AFN120212 (accessed on 28 April 2018).
- Van Dyke, Cydney J., David S. Glenwick, John J. Cecero, and Se-Kang Kim. 2009. The relationship of religious coping and spirituality to adjustment and psychological distress in urban early adolescents. Mental Health, Religion and Culture 12: 369–83. [Google Scholar] [CrossRef]
- Zenk, Shannon N., Lisa M. Powell, Leah Rimkus, Zeynep Isgor, Dianne C. Barker, Punam Ohri-Vachaspati, and Frank Chaloupka. 2014. Relative and absolute availability of healthier food and beverage alternatives across communities in the United States. American Journal of Public Health 104: 2170–78. [Google Scholar] [CrossRef] [PubMed]
| 1 | The Prosperity Gospel is the doctrine that God wants people to be prosperous, especially financially; adherents to the Prosperity Gospel believe that wealth is a sign of God’s blessing and the poor are poor due to a lack of faith. Koch, Bradley. Journal of Ideology Volume 36, 2014. |

| Demographic Data (N = 261) | N | % |
|---|---|---|
| Gender–Female | 191 | 74.3 |
| Age—30–49 years | 119 | 46.5 |
| Religious preference | ||
| Christian | 110 | 42.1 |
| Seventh Day Adventist | 48 | 18.3 |
| Catholic | 45 | 17.2 |
| Ethnicity | ||
| Non-Hispanic | 138 | 55.2 |
| Hispanic | 112 | 44.8 |
| Annual income | ||
| <$30,000 | 128 | 56.6 |
| $30,000–<$50,000 | 38 | 16.8 |
| $50,000 | 29 | 12.8 |
| Prefer not to answer | 31 | 11.7 |
| Education | ||
| High school degree, GED, or less | 115 | 44.6 |
| Some college, associate, or bachelor’s degree | 128 | 48.1 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pfeiffer, J.; Li, H.; Martez, M.; Gillespie, T. The Role of Religious Behavior in Health Self-Management: A Community-Based Participatory Research Study. Religions 2018, 9, 357. https://doi.org/10.3390/rel9110357
Pfeiffer J, Li H, Martez M, Gillespie T. The Role of Religious Behavior in Health Self-Management: A Community-Based Participatory Research Study. Religions. 2018; 9(11):357. https://doi.org/10.3390/rel9110357
Chicago/Turabian StylePfeiffer, Jane, Hong Li, Maybelline Martez, and Tim Gillespie. 2018. "The Role of Religious Behavior in Health Self-Management: A Community-Based Participatory Research Study" Religions 9, no. 11: 357. https://doi.org/10.3390/rel9110357
APA StylePfeiffer, J., Li, H., Martez, M., & Gillespie, T. (2018). The Role of Religious Behavior in Health Self-Management: A Community-Based Participatory Research Study. Religions, 9(11), 357. https://doi.org/10.3390/rel9110357




