A Multimethod Approach for Healthcare Information Sharing Systems: Text Analysis and Empirical Data
Abstract
:1. Introduction
1.1. Healthcare Spending and Financial Pressures
1.2. Adoption of Electronic Health Records (EHR) and Healthcare
1.3. Adoption Challenges and Disparities in EHR Implementation
1.4. Assessing EHR Implementation
2. Theoretical Foundation
2.1. Resource Advantage Theory and Competitive Advantage
2.2. Research Limitations and Gaps in Understanding Successful EHR Adoption
2.3. Complexity of EHR Implementation
2.4. For-Profit and Not-for-Profit Classification and EHR Implementation
2.5. Joint-Venture Hospitals and EHR Implementation
2.6. Hospital Monitoring and EHR Implementation
3. Methodology
Sample, Data, Variables
4. Results
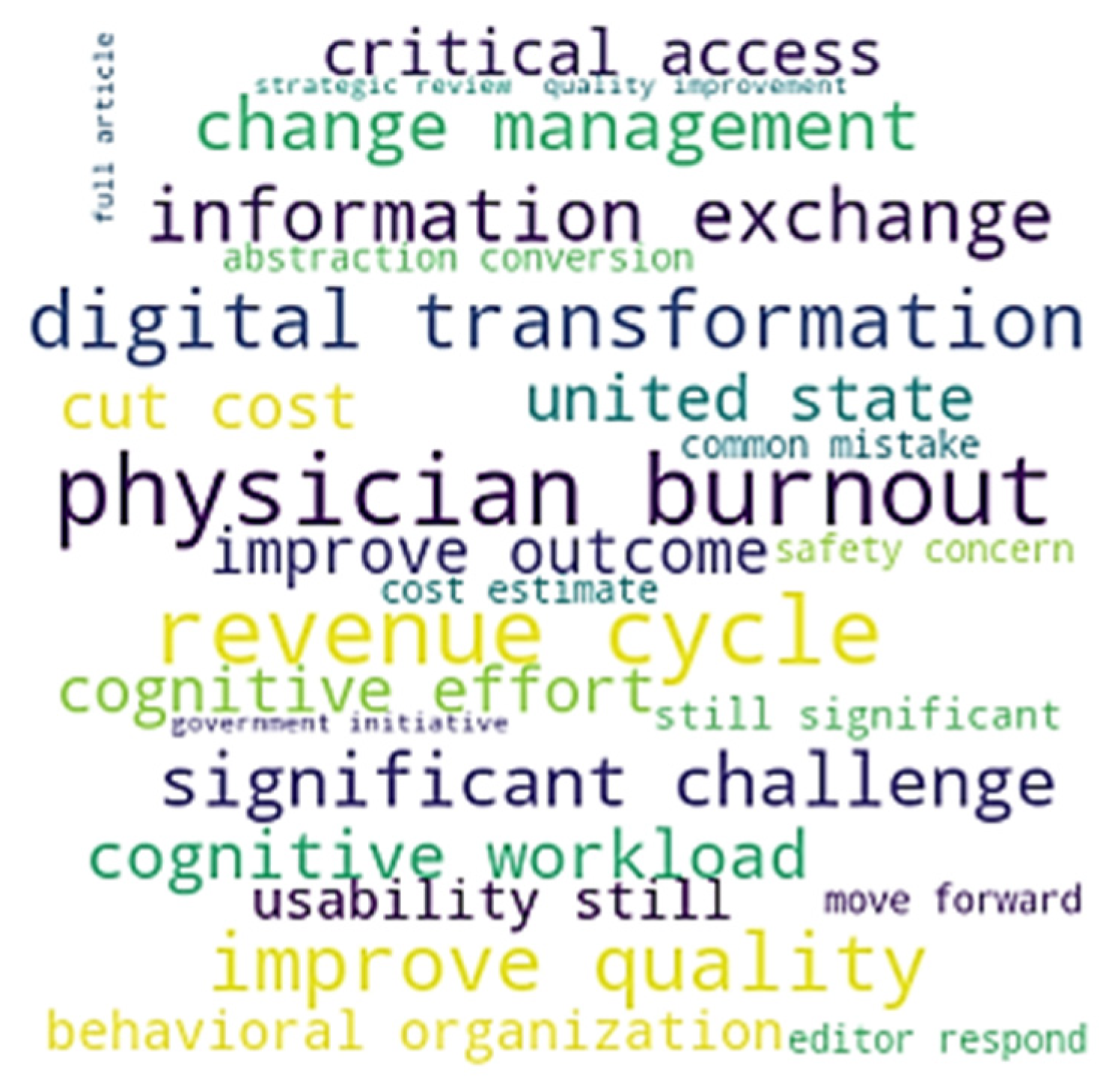
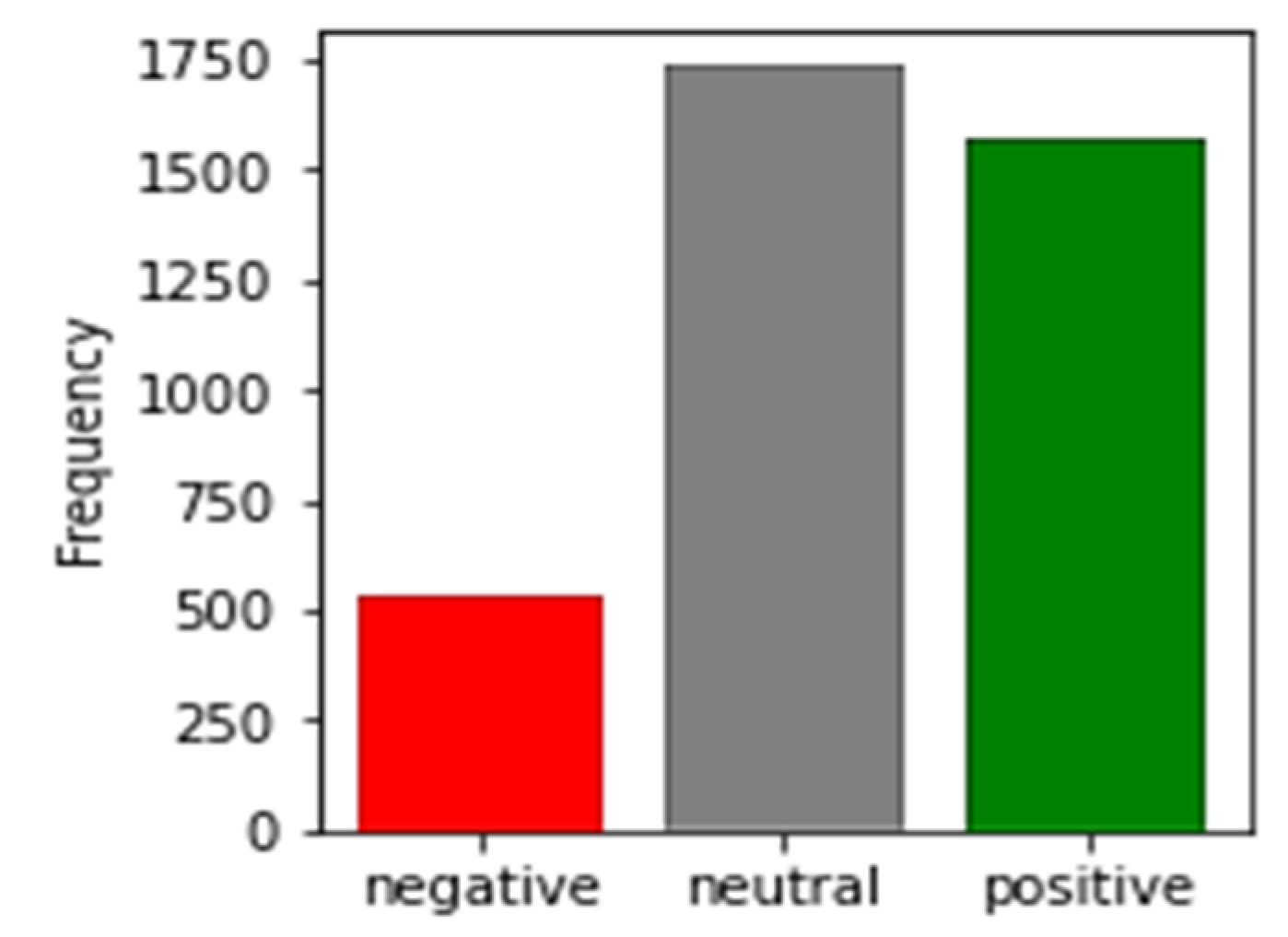
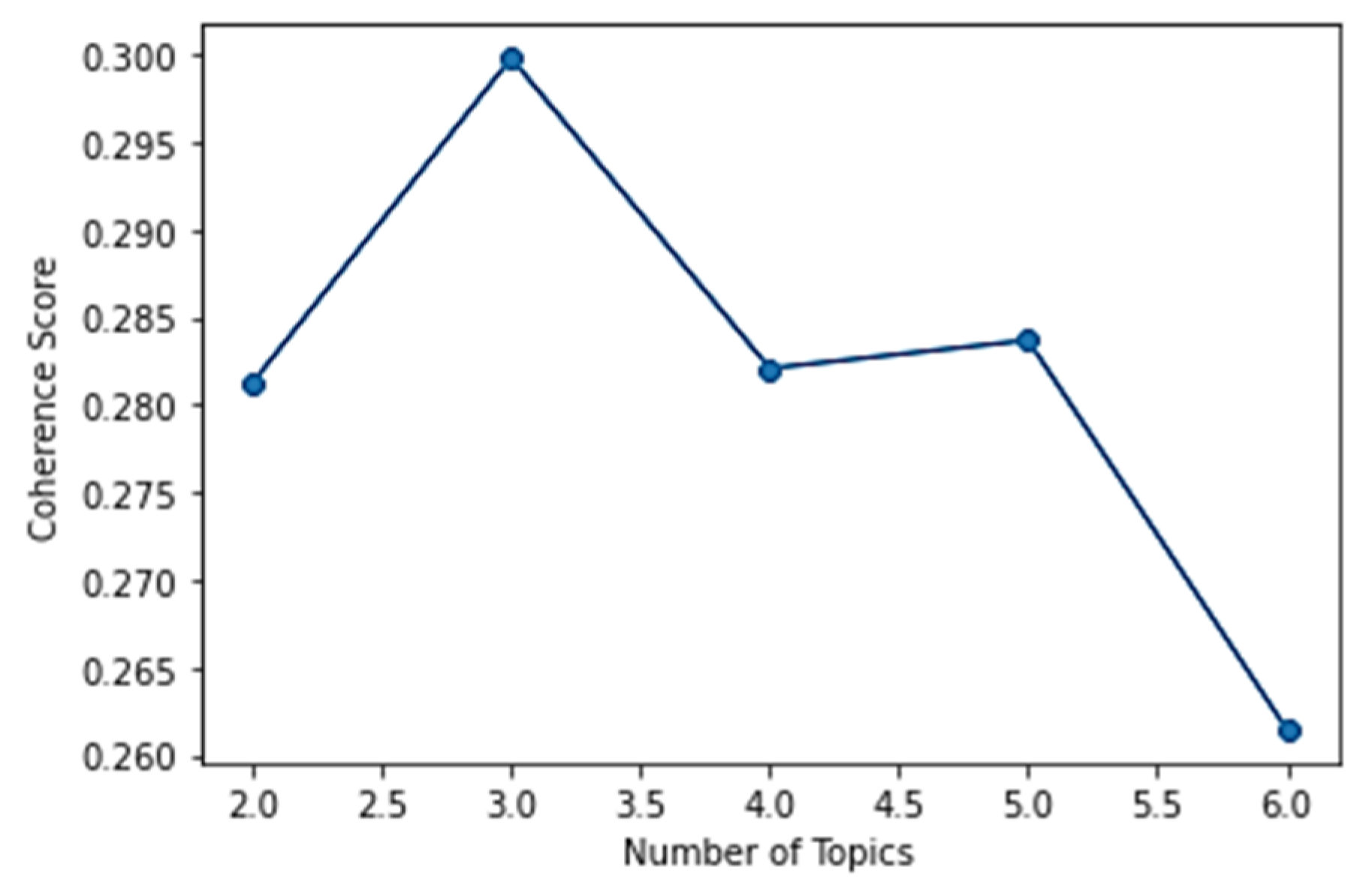
Text Analysis: Study 2
5. Discussion
Limitations and Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hynes, W.; Trump, B.; Love, P.; Linkov, I. Bouncing Forward: A Resilience Approach to Dealing with COVID-19 and Future Systemic Shocks. Environ. Syst. Decis. 2020, 40, 174–184. [Google Scholar] [CrossRef]
- Malhan, A.S.; Sadeghi-R, K.; Pavur, R.; Pelton, L. Healthcare Information Management and Operational Cost Performance: Empirical Evidence. Eur. J. Health Econ. 2023, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Dean, B.B.; Lam, J.; Natoli, J.L.; Butler, Q.; Aguilar, D.; Nordyke, R.J. Use of Electronic Medical Records for Health Outcomes Research: A Literature Review. Med. Care Res. Rev. 2009, 66, 611–638. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi, K.; Abadi, M.Q.H. Sustainable Supply Chain Resilience for Logistics Problems: Empirical Validation Using Robust and Computational Intelligence Methods. J. Clean. Prod. 2024, 437, 140267. [Google Scholar] [CrossRef]
- Tiwari, P.; Sadeghi, J.K.; Eseonu, C. A Sustainable Lean Production Framework with a Case Implementation: Practice-Based View Theory. J. Clean. Prod. 2020, 277, 123078. [Google Scholar] [CrossRef]
- Statista. Statistica Health Expenditures in the U.S.—Statistics & Facts; Statista Research Department: New York, NY, USA, 2022. [Google Scholar]
- Kaufman, B.G.; Thomas, S.R.; Randolph, R.K.; Perry, J.R.; Thompson, K.W.; Holmes, G.M.; Pink, G.H. The Rising Rate of Rural Hospital Closures. J. Rural Health 2016, 32, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.L.; Jervis, K.J.; Younis, M.Z.; Forgione, D.A. Hospital Financial Distress, Recovery and Closure: Managerial Incentives and Political Costs. J. Public Budg. Account. Financ. Manag. 2011, 23, 31–68. [Google Scholar] [CrossRef]
- Gapenski, L.C.; Pink, G.H. Understanding Healthcare Financial Management; Health Administration Press: Chicago, IL, USA, 2007. [Google Scholar]
- Esmaeilzadeh, P. How Does IT Identity Affect Individuals’ Use Behaviors Associated with Personal Health Devices (PHDs)? An Empirical Study. Inf. Manag. 2021, 58, 103313. [Google Scholar] [CrossRef]
- Cocosila, M.; Archer, N. Practitioner Pre-Adoption Perceptions of Electronic Medical Record Systems. Behav. Inf. Technol. 2017, 36, 827–838. [Google Scholar] [CrossRef]
- Sadeghi-R, J.K.; Prybutok, V.R.; Sauser, B. Theoretical and Practical Applications of Blockchain in Healthcare Information Management. Inf. Manag. 2022, 59, 103649. [Google Scholar] [CrossRef]
- Tan, H.; Yan, M. Physician-User Interaction and Users’ Perceived Service Quality: Evidence from Chinese Mobile Healthcare Consultation. Inf. Technol. People 2020, 33, 1403–1426. [Google Scholar] [CrossRef]
- Razmak, J.; Belanger, C. Using the Technology Acceptance Model to Predict Patient Attitude toward Personal Health Records in Regional Communities. Inf. Technol. People 2018, 31, 306–326. [Google Scholar] [CrossRef]
- Sadoughi, F.; Nasiri, S.; Ahmadi, H. The Impact of Health Information Exchange on Healthcare Quality and Cost-Effectiveness: A Systematic Literature Review. Comput. Methods Programs Biomed. 2018, 161, 209–232. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi, J.K.; Struckell, E.; Ojha, D.; Nowicki, D. Absorptive Capacity and Disaster Immunity: The Mediating Role of Information Quality and Change Management Capability. J. Knowl. Manag. 2021, 25, 714–742. [Google Scholar] [CrossRef]
- Kohli, R.; Tan, S.S.-L. Electronic Health Records. Mis Q. 2016, 40, 553–574. [Google Scholar] [CrossRef]
- Bakker, A. Access to EHR and Access Control at a Moment in the Past: A Discussion of the Need and an Exploration of the Consequences. Int. J. Med. Inform. 2004, 73, 267–270. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, M.N.; Haleem, A.; Javaid, M. Scope of Health Care System in Rural Areas under Medical 4.0 Environment. Intell. Pharm. 2023, 1, 217–223. [Google Scholar] [CrossRef]
- Alzghaibi, H.; Alharbi, A.H.; Mughal, Y.H.; Alwheeb, M.H.; Alhlayl, A.S. Assessing Primary Health Care Readiness for Large-Scale Electronic Health Record System Implementation: Project Team Perspective. Health Inform. J. 2023, 29, 14604582231152790. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.-C.; Veeranki, S.P.; Serag, H.; Eschbach, K.; Smith, K.D. Improving the Collection of Race, Ethnicity, and Language Data to Reduce Healthcare Disparities: A Case Study from an Academic Medical Center. Perspect. Health Inf. Manag. 2016, 13, 1–11. [Google Scholar]
- Heath, M.; Porter, T.H.; Dunegan, K. Obstacles to Continued Use of Personal Health Records. Behav. Inf. Technol. 2022, 41, 574–587. [Google Scholar] [CrossRef]
- Chui, K.T.; Liu, R.W.; Lytras, M.D.; Zhao, M. Big Data and IoT Solution for Patient Behaviour Monitoring. Behav. Inf. Technol. 2019, 38, 940–949. [Google Scholar] [CrossRef]
- Carayon, P.; Smith, P.; Hundt, A.; Kuruchittham, V.; Li, Q. Implementation of an electronic health records system in a small clinic: The viewpoint of clinic staff. Behav. Inf. Technol. 2009, 28, 5–20. [Google Scholar] [CrossRef]
- Ahmadi, H.; Nilashi, M.; Shahmoradi, L.; Ibrahim, O. Hospital Information System Adoption: Expert Perspectives on an Adoption Framework for Malaysian Public Hospitals. Comput. Hum. Behav. 2017, 67, 161–189. [Google Scholar] [CrossRef]
- Sadeghi R, J.K.; Azadegan, A.; Ojha, D.; Ogden, J.A. Benefiting from Supplier Business Continuity: The Role of Supplier Monitoring and Buyer Power. Ind. Mark. Manag. 2022, 106, 432–443. [Google Scholar] [CrossRef]
- Varadarajan, R. Resource Advantage Theory, Resource Based Theory, and Theory of Multimarket Competition: Does Multimarket Rivalry Restrain Firms from Leveraging Resource Advantages? J. Bus. Res. 2023, 160, 113713. [Google Scholar] [CrossRef]
- Hunt, S.D.; Morgan, R.M. The Comparative Advantage Theory of Competition. J. Mark. 1995, 59, 1–15. [Google Scholar] [CrossRef]
- Hunt, S.D.; Morgan, R.M. The Resource-Advantage Theory of Competition: Dynamics, Path Dependencies, and Evolutionary Dimensions. J. Mark. 1996, 60, 107–114. [Google Scholar] [CrossRef]
- Hunt, S.D.; Davis, D.F. Grounding Supply Chain Management in Resource-advantage Theory. J. Supply Chain Manag. 2008, 44, 10–21. [Google Scholar] [CrossRef]
- Crespo, C.F.; Griffith, D.A.; Lages, L.F. The Performance Effects of Vertical and Horizontal Subsidiary Knowledge Outflows in Multinational Corporations. Int. Bus. Rev. 2014, 23, 993–1007. [Google Scholar] [CrossRef]
- Dheensa, S.; Carrieri, D.; Kelly, S.; Clarke, A.; Doheny, S.; Turnpenny, P.; Lucassen, A. A ‘joint Venture’ model of Recontacting in Clinical Genomics: Challenges for Responsible Implementation. Eur. J. Med. Genet. 2017, 60, 403–409. [Google Scholar] [CrossRef]
- Freedman, S.; Lin, H. Hospital Ownership Type and Innovation: The Case of Electronic Medical Records Adoption. Nonprofit Volunt. Sect. Q. 2018, 47, 537–561. [Google Scholar] [CrossRef]
- Hu, X.; Qu, H.; Houser, S.H.; Chen, H.; Zhou, J.; Yu, M. Hospital Characteristics Associated with Certified EHR Adoption among US Psychiatric Hospitals. Risk Manag. Healthc. Policy 2020, 13, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Hajian, A.; Prybutok, V.R.; Chang, H.-C. An Empirical Study for Blockchain-Based Information Sharing Systems in Electronic Health Records: A Mediation Perspective. Comput. Hum. Behav. 2023, 138, 107471. [Google Scholar] [CrossRef]
- Masterson, L. Hospital Operating Margins Dropped 39% over 3 Years; Healthcare Dive: Washington, DC, USA, 2018. [Google Scholar]
- Sloan, F.A.; Valdmanis, V.G. Relative Productivity of For-Profit Hospitals: A Big or a Little Deal? Med. Care Res. Rev. 2023, 80, 355–371. [Google Scholar] [CrossRef] [PubMed]
- Adler-Milstein, J.; Holmgren, A.J.; Kralovec, P.; Worzala, C.; Searcy, T.; Patel, V. Electronic Health Record Adoption in US Hospitals: The Emergence of a Digital “Advanced Use” Divide. J. Am. Med. Inform. Assoc. 2017, 24, 1142–1148. [Google Scholar] [CrossRef] [PubMed]
- Pai, D.R.; Rajan, B.; Chakraborty, S. Do EHR and HIE Deliver on Their Promise? Analysis of Pennsylvania Acute Care Hospitals. Int. J. Prod. Econ. 2022, 245, 108398. [Google Scholar] [CrossRef]
- Song, M. Market Competition and Regulatory Compliance in Public, Non-Profit, and for-Profit Organizations. Public Manag. Rev. 2023, 25, 1982–2002. [Google Scholar] [CrossRef]
- Zajac, E.J.; Golden, B.R.; Shortell, S.M. New Organizational Forms for Enhancing Innovation: The Case of Internal Corporate Joint Ventures. Manag. Sci. 1991, 37, 170–184. [Google Scholar] [CrossRef]
- Al-Mazroei, A.A. Factors Affecting the Implementation of Joint Ventures: A Study of Outsourcing in Healthcare Services in Low and Middle-Income Countries; University of Salford: Salford, UK, 2015; ISBN 9798597003993. [Google Scholar]
- Pelfrey, S.; Theisen, B.A. Joint Ventures in Health Care. JONA J. Nurs. Adm. 1989, 19, 39. [Google Scholar] [CrossRef]
- Harrison, J.P. The Impact of Joint Ventures on US Hospitals. J. Health Care Financ. 2006, 32, 28–38. [Google Scholar]
- Solheim-Kile, E.; Wald, A. Public–Private Joint Ventures in the Healthcare Sector: Enlarging the Shadow of the Future through Social and Economic Incentives. Int. J. Public Sect. Manag. 2020, 33, 647–662. [Google Scholar] [CrossRef]
- Bahri Korbi, F.; Geraudel, M.; Nakara, W.A. Toward an Understanding of the Implementation of Management Innovation in International Joint Ventures: A Multilevel Perspective. Eur. Manag. Rev. 2023, 20, 425–442. [Google Scholar] [CrossRef]
- Cherbib, J.; Bahri, F.; Berraies, S.; Chebbi, H. Towards the Co-Evolution of Multinationals’ and Local Firms’ Global Strategies in an Uncertain Environment: Insights from International Joint Ventures. J. Int. Manag. 2023, 29, 101089. [Google Scholar] [CrossRef]
- Karamyar, F.; Sadeghi, J.; Yazdi, M.M. A Benders Decomposition for the Location-Allocation and Scheduling Model in a Healthcare System Regarding Robust Optimization. Neural Comput. Appl. 2018, 29, 873–886. [Google Scholar] [CrossRef]
- Coddington, D.C.; Palmquist, L.E.; Trollinger, W.V. Strategies for Survival in the Hospital Industry. Harv. Bus. Rev. 1985, 3, 129–138. [Google Scholar]
- Lin, M.; Lekhawipat, W. Key Influencing Factors for the Success of External Innovation Strategies in the Biotechnology Industry. J. Bus. Ind. Mark. 2023, 38, 2745–2759. [Google Scholar] [CrossRef]
- Chen, C.; Pao, L.-S.; Lei, H. The Examination of Job Separation Tendency of Nursing Staff in the First Public–Private Joint-Venture Hospital in Taiwan: A Multiple Mediation Model of Job Satisfaction and Job Performance. Humanit. Soc. Sci. Commun. 2022, 9, 425. [Google Scholar] [CrossRef]
- Narayanan, S.; Vickery, S.K.; Nicolae, M.L.; Castel, M.J.; McLeod, M.K. The Effects of Lean Implementation on Hospital Financial Performance. Decis. Sci. 2022, 53, 557–577. [Google Scholar] [CrossRef]
- Viswanadham, N. Ecosystem Model for Healthcare Platform. Sādhanā 2021, 46, 188. [Google Scholar] [CrossRef]
- Smith, P.C. An Examination of the Financial Structure of Not-for-Profit Hospitals Engaging in Joint Ventures: Is Tax-Exempt Status in Jeopardy? Res. Healthc. Financ. Manag. 2005, 10, 43. [Google Scholar]
- Amarasingham, R.; Plantinga, L.; Diener-West, M.; Gaskin, D.J.; Powe, N.R. Clinical information technologies and inpatient outcomes: A multiple hospital study. Arch. Intern. Med. 2009, 169, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Parente, S.T.; McCullough, J.S. Health Information Technology and Patient Safety: Evidence from Panel Data. Health Aff. 2009, 28, 357–360. [Google Scholar] [CrossRef] [PubMed]
- Featherly, K.; Garets, D.; Davis, M.; Wise, P.; Becker, P. Sharpening the case for returns on investment from clinical information systems. Healthc. Q. 2007, 10, 101–110. [Google Scholar] [PubMed]
- Menachemi, N.; Saunders, C.; Chukmaitov, A.; Matthews, M.C.; Brooks, R.G. Hospital Adoption of Information Technologies and Improved Patient Safety: A Study of 98 Hospitals in Florida. J. Healthc. Manag. 2007, 52, 398–410. [Google Scholar] [CrossRef]
- Ergai, A.; Spiva, L.; Thurman, S.; Hatfield, M.; McCollum, M.; Holmes, M. The Effectiveness of Remote Video Monitoring on Fall Prevention and Nurses’ Acceptance. J. Nurs. Care Qual. 2024, 39, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Burnett, J.R.; Lisk, T.C. The Future of Employee Engagement: Real-Time Monitoring and Digital Tools for Engaging a Workforce. In International Perspectives on Employee Engagement; Routledge: London, UK, 2021; pp. 117–128. [Google Scholar]
- Hong Mershon, B.; Vannucci, A.; Bryson, T.; Lin, F.; Greilich, P.E.; Dear, G.; Guffey, P.; Agarwala, A. A Collaborative Partnership between the Multicenter Handoff Collaborative and an Electronic Health Record Vendor. Appl. Clin. Inf. 2021, 12, 647–654. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, A.; Anderson, M.; Albala, S.; Casadei, B.; Franklin, B.D.; Richards, M.; Taylor, D.; Tibble, H.; Mossialos, E. Health Information Technology and Digital Innovation for National Learning Health and Care Systems. Lancet Digit. Health 2021, 3, e383–e396. [Google Scholar] [CrossRef] [PubMed]
- Hajian, A.; Prybutok, V.R.; Chang, H.-C. How Do Morning and Friendly Ads Influence Mobile Advertising? A Mediation Perspective Using Appraisal Theory. J. Mark. Commun. 2023, 29, 510–532. [Google Scholar] [CrossRef]
- Sadeghi, K.; Azadegan, A.; Ojha, D. A Path to Build Supply Chain Cyber-Resilience through Absorptive Capacity and Visibility: Two Empirical Studies. Ind. Mark. Manag. 2023, 111, 202–215. [Google Scholar] [CrossRef]
- Hahs-Vaughn, D.L. Applied Multivariate Statistical Concepts; Routledge Taylor & Francis Group: New York, NY, USA, 2016; ISBN 1-317-81137-2. [Google Scholar]
- Mousavi, S.M.; Sadeghi R, K.; Lee, L.S. An Interactive Analytics Approach for Sustainable and Resilient Case Studies: A Machine Learning Perspective. J. Bus. Anal. 2023, 6, 276–293. [Google Scholar] [CrossRef]
- Sadeghi, R.; Hajian, A.; Rabiee, M. Blockchain and Machine Learning Framework for Financial Performance in Pharmaceutical Supply Chains. In Advancement in Business Analytics Tools for Higher Financial Performance; IGI Global: Hershey, PA, USA, 2023; pp. 112–128. [Google Scholar]
- Kolliakou, A.; Ball, M.; Derczynski, L.; Chandran, D.; Gkotsis, G.; Deluca, P.; Jackson, R.; Shetty, H.; Stewart, R. Novel Psychoactive Substances: An Investigation of Temporal Trends in Social Media and Electronic Health Records. Eur. Psychiatry 2016, 38, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Denecke, K.; Reichenpfader, D. Sentiment Analysis of Clinical Narratives: A Scoping Review. J. Biomed. Inform. 2023, 140, 104336. [Google Scholar] [CrossRef]
- Santillana, M.; Nguyen, A.T.; Louie, T.; Zink, A.; Gray, J.; Sung, I.; Brownstein, J.S. Cloud-Based Electronic Health Records for Real-Time, Region-Specific Influenza Surveillance. Sci. Rep. 2016, 6, 25732. [Google Scholar] [CrossRef] [PubMed]
- Grover, P.; Kar, A.K.; Davies, G. “Technology Enabled Health”–Insights from Twitter Analytics with a Socio-Technical Perspective. Int. J. Inf. Manag. 2018, 43, 85–97. [Google Scholar] [CrossRef]
- Guidry, J.P.; Jin, Y.; Orr, C.A.; Messner, M.; Meganck, S. Ebola on Instagram and Twitter: How Health Organizations Address the Health Crisis in Their Social Media Engagement. Public Relat. Rev. 2017, 43, 477–486. [Google Scholar] [CrossRef]
- Galavi, Z.; Montazeri, M.; Ahmadian, L. Barriers and Challenges of Using Health Information Technology in Home Care: A Systematic Review. Int. J. Health Plan. Manag. 2022, 37, 2542–2568. [Google Scholar] [CrossRef]
- Hajian, A.; Sadeghi, R.; Prybutok, V.R.; Koh, C.E. Increasing Trust and Value of Mobile Advertising in Retailing: A Survey Design, Machine Learning Approach, and Blockchain in the Trust Path. J. Retail. Consum. Serv. 2024, 79, 103794. [Google Scholar] [CrossRef]
- Garvey, M.D.; Samuel, J.; Pelaez, A. Would You Please like My Tweet?! An Artificially Intelligent, Generative Probabilistic, and Econometric Based System Design for Popularity-Driven Tweet Content Generation. Decis. Support Syst. 2021, 144, 113497. [Google Scholar] [CrossRef]
- Sadeghi, K.; Ojha, D.; Kaur, P.; Mahto, R.V.; Dhir, A. Explainable Artificial Intelligence and Agile Decision-Making in Supply Chain Cyber Resilience. Decis. Support Syst. 2024, 180, 114194. [Google Scholar] [CrossRef]
- Shmerling, R.H. Is Our Healthcare System Broken? Available online: https://www.health.harvard.edu/blog/is-our-healthcare-system-broken-202107132542 (accessed on 8 May 2024).
- Ding, X. Benchmark and Performance Progression: Examining the Roles of Market Competition and Focus. J. Oper. Manag. 2024, 70, 381–410. [Google Scholar] [CrossRef]
- Ding, X.; Peng, X.; Heim, G.R.; Jordan, V.S. Service Mix, Market Competition, and Cost Efficiency: A Longitudinal Study of US Hospitals. J. Oper. Manag. 2020, 66, 176–198. [Google Scholar] [CrossRef]
- Lee, C.K.H. How Guest-Host Interactions Affect Consumer Experiences in the Sharing Economy: New Evidence from a Configurational Analysis Based on Consumer Reviews. Decis. Support Syst. 2022, 152, 113634. [Google Scholar] [CrossRef]
- Stöckli, D.R.; Khobzi, H. Recommendation Systems and Convergence of Online Reviews: The Type of Product Network Matters! Decis. Support Syst. 2021, 142, 113475. [Google Scholar] [CrossRef]
- Ghosh, S.; Chakraborty, S.; Gupta, N.; Basu, S. What Ails Physician Review Websites? A Study of Information Needs of Patients. Decis. Support Syst. 2023, 166, 113897. [Google Scholar] [CrossRef]
- Hunt, S.D.; Lambe, C.J. Marketing’s Contribution to Business Strategy: Market Orientation, Relationship Marketing and Resource-advantage Theory. Int. J. Manag. Rev. 2000, 2, 17–43. [Google Scholar] [CrossRef]
- Southwick, R. There Were More Hospital Mergers in 2023, and Financial Distress Is Driving More Deals. Available online: https://www.chiefhealthcareexecutive.com/view/there-were-more-hospital-mergers-in-2023-and-financial-distress-is-driving-more-deals (accessed on 8 May 2024).
- Hajian, A.; Daneshgar, S.; Sadeghi R, K.; Ojha, D.; Katiyar, G. From Theory to Practice: Empirical Perspectives on the Metaverse’s Potential. Technol. Forecast. Soc. Change 2024, 201, 123224. [Google Scholar] [CrossRef]




| EHR | Ownership | Joint Venture | Monitoring | Number of Beds | |
|---|---|---|---|---|---|
| EHR | 1 | −0.353 ** | 0.382 ** | 0.157 * | 0.232 ** |
| Ownership | −0.353 ** | 1 | −0.280 ** | −0.060 | −0.272 ** |
| Joint venture | 0.382 ** | −0.280 ** | 1 | 0.226 ** | 0.254 ** |
| Monitoring | 0.157 * | −0.060 | 0.226 ** | 1 | 0.194 ** |
| Number of beds | 0.232 ** | −0.272 ** | 0.254 ** | 0.194 ** | 1 |
| Model | B | Error | β | t | p | |
|---|---|---|---|---|---|---|
| 1 | (Constant) | 0.396 | 0.046 | - | 8.534 | <0.001 |
| Number of beds | 0.001 | 0.000 | 0.232 | 3.352 | 0.001 | |
| 2 | (Constant) | 0.582 | 0.076 | - | 7.627 | <0.001 |
| Number of beds | 0.000 | 0.000 | 0.091 | 1.361 | 0.175 | |
| Ownership | −0.272 | 0.074 | −0.247 | −3.659 | <0.001 | |
| Joint venture | 0.370 | 0.085 | 0.290 | 4.330 | <0.001 | |
| 3 | (Constant) | 0.583 | 0.084 | - | 6.964 | <0.001 |
| Number of beds | 0.000 | 0.000 | 0.086 | 1.288 | 0.199 | |
| Ownership | −0.276 | 0.073 | −0.251 | −3.774 | <0.001 | |
| Joint venture | −0.129 | 0.207 | −0.101 | −0.623 | 0.534 | |
| Monitoring | 0.008 | 0.071 | 0.008 | 0.117 | 0.907 | |
| Monitoring × Joint venture | 0.572 | 0.223 | 0.424 | 2.566 | 0.011 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malhan, A.; Pavur, R.; Pelton, L.E.; Hajian, A. A Multimethod Approach for Healthcare Information Sharing Systems: Text Analysis and Empirical Data. Information 2024, 15, 319. https://doi.org/10.3390/info15060319
Malhan A, Pavur R, Pelton LE, Hajian A. A Multimethod Approach for Healthcare Information Sharing Systems: Text Analysis and Empirical Data. Information. 2024; 15(6):319. https://doi.org/10.3390/info15060319
Chicago/Turabian StyleMalhan, Amit, Robert Pavur, Lou E. Pelton, and Ava Hajian. 2024. "A Multimethod Approach for Healthcare Information Sharing Systems: Text Analysis and Empirical Data" Information 15, no. 6: 319. https://doi.org/10.3390/info15060319





