Enhancing Online Patient Support through Health-Care Knowledge in Online Health Communities: A Descriptive Study
Abstract
:1. Introduction
- How do existing OHCs influence information availability for online patients?
- How do existing OHCs facilitate social services for online patient support?
- How does domain knowledge in health-care enhance existing OHCs?
2. Materials and Methods
2.1. Criteria for Selecting OHCs
- (1)
- The OHC must be built upon a social platform that supports interaction among online patients.
- (2)
- The OHC must present a brief introduction of biomedical and health-care knowledge relevant to patients’ conditions, treatments and symptoms.
- (3)
- The OHC must utilize recommendation mechanisms for similar patients and posts.
- (4)
- The OHC must provide an open subscription network that aids online users to explore other online patients with similar conditions.
- (5)
- The OHC must allow online patients to find information on other patients and doctors.
- (6)
- The OHC’s health services must include publication of health-related announcement, news, warnings and reports.
- (7)
- The OHC must assist online patients in decision making regarding their treatment and enhancement of health lifestyle.
- (8)
- The OHC must show patients’ charts and journals.
- (9)
- The OHC must provide the summarized data of patient-reported outcomes for similar patients’ reference.
- (1)
- Sites that merely introduce a health-related product for specific companies.
- (2)
- Sites with content that is irrelevant to humans.
- (3)
- Sites that do not allow users to interact with health service providers or other users.
- (4)
- Sites run by specific governments and other non-profit organizations that only publish information resources.
- (5)
- Sites that show excessive commercial advertising and pricing.
- (6)
- Sites resembling libraries for mere educational purposes.
- (7)
- Sites that do not provide a user account or only offer a subscription panel.
2.2. Evaluation Instruments
2.2.1. Evaluation of Information Availability of Websites
2.2.2. Evaluation of the User Availability of Websites
2.2.3. Evaluation of Knowledge Usability of Websites
2.3. Review Process
3. Results
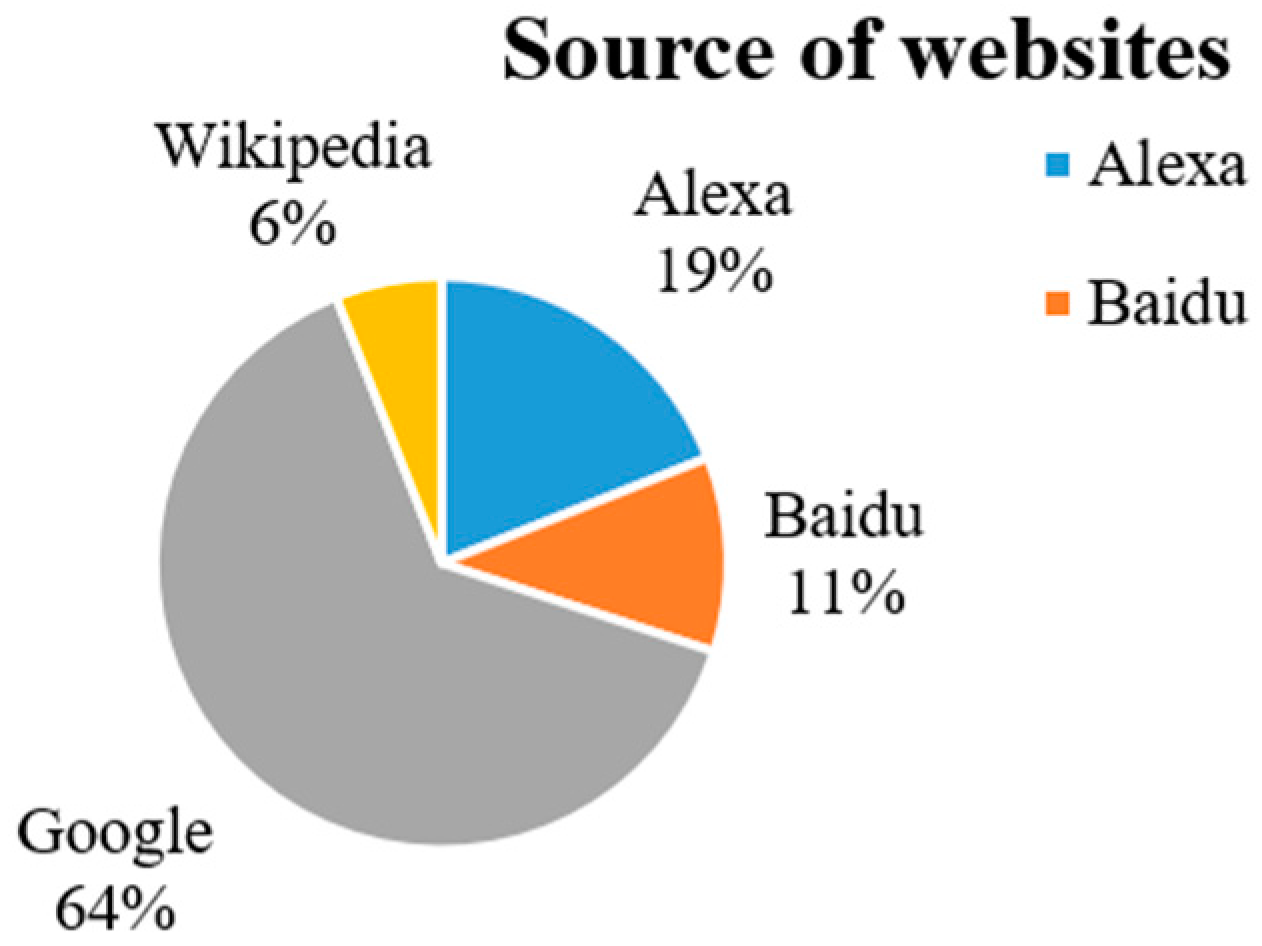
3.1. Overview of Existing OHCs
3.2. Measurement for Effective OHCs
3.3. Information Availability
3.4. User Availability
3.5. Knowledge Usability
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Gray, C.S.; Miller, D.; Kuluski, K.; Cott, C. Trying eHealth tools to patient needs: Exploring the use of eHealth for community-dwelling patients with complex chronic disease and disability. JMIR Res. Protoc. 2014, 3, e67. [Google Scholar] [CrossRef] [PubMed]
- Willis, E.; Royne, M.B. Online health communities and chronic disease self-management. Health Commun. 2016, 32, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Cameron, J.; Rhodes, K.L.; Ski, C.F.; Thompson, D.R. Careers’ views on patient self-care in chronic heart failure. J. Nurs. 2016, 25, 144–152. [Google Scholar]
- Allen, C.; Vassilev, I.; Kennedy, A.; Rogers, A. Long-term condition self-management support in online communities: A meta-synthesis of qualitative papers. J. Med. Internet Res. 2016, 18, e61. [Google Scholar] [CrossRef] [PubMed]
- Dobkin, P.L.; Boothroyd, L.J. Organizing health services for patients with chronic pain: When there is a will there is a way. Pain Med. 2008, 9, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Wicks, P.; Massagli, M.; Frost, J.; Brownstein, C.; Okun, S.; Vaughan, T.; Bradley, R.; Heywood, J. Sharing health data for better outcomes on PatientsLikeMe. J. Med. Internet Res. 2017, 12, e19. [Google Scholar] [CrossRef] [PubMed]
- James, D.C.; Harville, C. eHealth Literacy, Online help-seeking behavior, and willingness to participate in mHealth chronic disease research among African Americans, Florida, 2014–2015. Prev. Chron. Dis. 2016, 13, E156. [Google Scholar] [CrossRef] [PubMed]
- Mccloud, R.F.; Okechukwu, C.A.; Sorensen, G.; Viswanath, K. Beyond access: Barriers to internet health information seeking among the urban poor. J. Am. Med. Inf. Assoc. 2016, 23, 1053–1059. [Google Scholar] [CrossRef] [PubMed]
- Kazmer, M.M.; Lustria, M.L.A.; Cortese, J.; Burnett, G.; Kim, J.H. Distributed knowledge in an online patient support community: Authority and discovery. J. Am. Infom. Sci. Technol. 2014, 65, 1319–1334. [Google Scholar] [CrossRef] [Green Version]
- Huh, J.; Kwon, B.C.; Kim, S.H.; Lee, S.; Choo, J.; Kim, J.; Choi, M.J.; Yi, J.S. Personas in online health communities. J. Biomed. Inf. 2016, 63, 212–225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xiang, J.; Stanley, S.J. From online to offline: Exploring the role of e-health consumption, patient involvement, and patient-centered communication on perceptions of health care quality. Comput. Hum. Behav. 2017, 70, 446–452. [Google Scholar] [CrossRef]
- Juth, V.; Smyth, J.M.; Santuzzi, A.M. How do you feel? self-esteem predicts affect, stress, social interaction, and symptom severity during daily life in patients with chronic illness. J. Health Psychol. 2008, 13, 884–894. [Google Scholar] [CrossRef] [PubMed]
- Rzeszutek, M.; Oniszczenko, W.; Schier, K.; BiernatKaluza, E.; Gasik, R. Temperament traits, social support, and trauma symptoms among HIV/AIDS and chronic pain patients. Int. J. Clin. Health Psychol. 2016, 16, 137–146. [Google Scholar] [CrossRef]
- Morrison, E.J.; Flynn, J.M.; Jones, J.; Byrd, J.C.; Andersen, B.L. Individual differences in physical symptom burden and psychological responses in individuals with chronic lymphocytic leukemia. Ann. Hematol. 2016, 95, 1989–1997. [Google Scholar] [CrossRef] [PubMed]
- Möller-Leimkühler, A.M.; Wiesheu, A. Caregiver burden in chronic mental illness: The role of patient and caregiver characteristics. Eur. Arch. Psychiatry Clin. Neurosci. 2012, 262, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Diviani, N.; Van, D.; Meppelink, C.S.; Weert, J.C. Exploring the role of health literacy in the evaluation of online health information: Insights from a mixed-methods study. Patient Educ. Couns. 2016, 99, 1017–1025. [Google Scholar] [CrossRef] [PubMed]
- Zisook, S.; Tal, I.; Weingart, K.; Hicks, P.; Davis, L.L.; Chen, P.; Yoon, J.; Johnson, G.R.; Vertrees, J.E.; et al. Characteristics of US veteran patients with major depressive disorder who require “next-step” treatments: A VAST-D report. J. Affect. Disord. 2016, 206, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Joensen, L.E.; Almdal, T.P.; Willaing, I. Associations between patient characteristics, social relations, diabetes management, quality of life, glycaemic control and emotional burden in Type 1 diabetes. Primary Care Diabetes 2015, 10, 41–50. [Google Scholar]
- Gordon, K.; Smith, F.; Dhillon, S. Effective chronic disease management: Patients’ perspectives on medication-related problems. Patient Educ. Counsel. 2007, 65, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Allen, M.; Iezzoni, L.I.; Huang, A.; Huang, L.; Leveille, S.G. Improving patient-clinician communication about chronic conditions: Description of an internet-based nurse E-coach intervention. Nurs. Res. 2008, 57, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Gaikwad, M.; Vanlint, S.; Moseley, G.L.; Mittinty, M.N.; Stocks, N. Understanding patient perspectives on management of their chronic pain—Online survey protocol. J. Pain Res. 2016, 10, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Diviani, N.; Putte, B.; Giani, S.; Weert, J. Low health literacy and evaluation of online health information: A systematic review of the literature. J. Med. Internet Res. 2015, 17, e112. [Google Scholar] [CrossRef] [PubMed]
- Theresa, D.; Jordan, B.; Harris, L.M.; Wu, H.; Williams, H.S. Making quality health websites a national public health priority: Toward quality standards. J. Med. Internet Res. 2016, 18, e211. [Google Scholar]
- Yan, Z.; Wang, T.; Chen, Y.; Zhang, H. Knowledge sharing in online health communities: A social exchange theory perspective. Inform. Manag. 2016, 53, 643–653. [Google Scholar] [CrossRef]
- Mohammad, H.; Woensel, W.V.; Abidi, R.S.; Abidi, S.S. Semantics-based plausible reasoning to extend the knowledge coverage of medical knowledge bases for improved clinical decision support. Biodata Min. 2017, 10, 7. [Google Scholar]
- Wicks, P.; Vaughan, T.E.; Massagli, M.P.; Heywood, J. Accelerated clinical discovery using self-reported patient data collected online and a patient-matching algorithm. Nat. Biotechnol. 2011, 29, 411–414. [Google Scholar] [CrossRef] [PubMed]
- Wiering, B.; De, B.D.; Dlnoij, D. Patient involvement in the development of patient-reported outcome measures: A scoping review. Health Expect. 2017, 20, 11–23. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Xie, B. Health literacy in the eHealth era: A systematic review of the literature. Patient Educ. Counsel. 2017, 100, 1073–1082. [Google Scholar] [CrossRef] [PubMed]
- Protheroe, J.; Whittle, R.; Bartlam, B.; Estacio, E.V.; Clark, L.; Kurth, J. Health literacy, associated lifestyle and demographic factors in adult population of an English city: A cross-sectional survey. Health Expect. 2017, 20, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Quinn, S.; Bond, R.; Nugent, C. Quantifying health literacy and eHealth literacy using existing instruments and browser-based software for tracking online health information seeking behavior. Comput. Hum. Behav. 2017, 69, 256–267. [Google Scholar] [CrossRef]
- Gutierrez, N.; Kindratt, T.B.; Pagels, P.; Foster, P.; Gimpel, N.E. Health literacy, health information seeking behaviors and internet use among patients attending a private and public clinic in the same geographic area. J. Commun. Health 2014, 39, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.; Yu, G.; Mcnichol, K.; Marczewski, K.; Closs, S.J. The effects of patient–professional partnerships on the self-management and health outcomes for patients with chronic back pain: A quasi-experimental study. Int. J. Nurs. Stud. 2016, 59, 197. [Google Scholar] [CrossRef] [PubMed]
- Tommasetti, A.; Troisi, O.; Cosimato, S. Patient empowerment and health online community: Two ways to give the new viability doctor-patient relationship. J. Mol. Struct. 2014, 193, 295–300. [Google Scholar]
- Van der Eijk, M.; Faber, M.J.; Aarts, J.W.; Kremer, J.A.; Munneke, M.; Bloem, B.R. Using online health communities to deliver patient-centered care to people with chronic conditions. J. Med. Internet Res. 2013, 15, e115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Online Health Communities. Available online: https://en.wikipedia.org/wiki/Online_health_communities (accessed on 21 July 2018).
- Yan, L.L.; Peng, J.; Tan, Y. Network dynamics: How can we find patients like us? Inf. Syst. Res. 2015, 26, 496–512. [Google Scholar] [CrossRef]
- Amann, J.; Zanini, C.; Rubinelli, S. What online user innovation communities can teach us about capturing the experiences of patients living with chronic health conditions: A scoping review. PLoS ONE 2016, 11, e0156175. [Google Scholar] [CrossRef] [PubMed]
- Rozenblum, R.; Bates, D.W. Patient-centred healthcare, social media and the internet: the perfect storm? BMJ Qual. Saf. 2013, 22, 183. [Google Scholar] [CrossRef] [PubMed]
- Meppelink, C.S.; Smit, E.G.; Diviani, N.; Weert, J. Health literacy and online health information processing: Uinraveling the underlying mechanisms. J. Health Commun. 2017, 21, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Koekkoek, B.; Van, M.B.; Schene, A.; Hutschemaekers, G. A Delphi study of problems in providing community care to patients with nonpsychotic chronic mental illness. Psychiatr. Serv. 2009, 60, 694–697. [Google Scholar] [CrossRef] [PubMed]
- Magnezi, R.; Bergman, D.; Grosberg, D. Online activity and participation in treatment affects the perceived efficacy of social health networks among patients with chronic illness. J. Med. Internet Res. 2014, 16, e12. [Google Scholar] [CrossRef] [PubMed]
- Centola, D.; Van, D.R.A. Choosing your network: Social preferences in an online health community. Soc. Sci. Med. 2015, 125, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Naujoks, C.; Olson, M.; Simsek, D.; Vulpillieres, F.; Vo, P.; Kendall, K.R.; Cerrato, D. How do Migraines Impact Patient Day-To-Day life? An Exploratory Analysis of Patient Reported Data From The Patientslikeme Community. Val. Health 2016, 19, A438–A439. [Google Scholar] [CrossRef]
- Ammerlaan, J.W.; Van, O.H.; De, B.N.; Scholtus, L.; Kruize, A.A.; Bijlsma, J.W.; Geenen, R. Preferences and needs of patients with a rheumatic disease regarding the structure and content of online self-management support. Patient Educ. Couns. 2017, 100, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Spiers, H.; Amin, N.; Lakhani, R.; Martin, A.J.; Patel, P.M. Assessing Readability and Reliability of Online Patient Information Regarding Vestibular Schwannoma. Otol. Neurotol. 2017, 38, e470–e475. [Google Scholar] [CrossRef] [PubMed]
- Bosslet, G.T.; Torke, A.M.; Hickman, S.E.; Terry, C.L.; Helft, P.R. The patient-doctor relationship and online social networks: Results of a national survey. J. Gen. Intern. Med. 2012, 27, 404. [Google Scholar] [CrossRef] [PubMed]
- Alex Top 500 Global Sites. Available online: https://www.alexa.com/topsites (accessed on 28 July 2018).
- Lewis, J.R. The System Usability Scale: Past, Present, and Future. Int. J. Hum.-Comput. Interact. 2018, 3, 577–590. [Google Scholar] [CrossRef]






| OHC | In Functional Module | In Subscription Network | In User Profile | In User Interaction |
|---|---|---|---|---|
| PatientsLikeMe | Diseases Conditions Treatments Symptom categories Quality of life | Conditions Symptoms Treatments Interests | Conditions Symptoms Treatments | / |
| HealthBoards | Types of anxiety Treatments A–Z drugs Disease categories | / | Diagnosis illnesses Medications and dosages | / |
| WebMed | Common conditions Drugs First aid Living healthy Parent guide Family and pregnancy Diet and food and fitness Beauty and balance Living well | / | / | Symptoms checker Message boards Answers Food and fitness planner Vaccine Lupus action plan Blood glucose Medicine |
| MedHelp | Disease categories Conditions | Conditions | Types of disorder Food diet Body weight Shape Diabetes | Disease trackers Baby growth Basal metabolic rate Body mass index Burned calories Diabetes risks Nutrition search Ovulations Pregnancy due |
| DailyStrength | Disease categories | Disease categories | / | / |
| HealthUnlocked | Actions of treatments | Disease information | / | / |
| OHC | Main Modules It Has | What Patients Can Do |
|---|---|---|
| PatientsLikeMe | Patient/condition/treatment/symptom, search module, Research participation module | Update patients’ own profile (hospitalization, laboratory tests, mood maps, charts, journals, conditions, symptoms, treatments, quality of life and weight); browse other patients’ journal and charts; review; find clinical trials; activity trackers; doctor visit sheet; care teams and patients |
| HealthBoards | Health centres (only anxiety), Message boards, Drug talks, Blogs | Update profile, browse types of anxiety, new post, find a board, search drug talks, search blogs |
| MedHelp | Communities/conditions, search modules, Heath tools | Update profile, mobile applications for tracker, health charts, overview of communities and forums relevant to specific diseases, posts and articles on specific diseases |
| DailyStrength | Support groups, Help/FAQ, Critical resources, ShareCare | New post, search blogs, browse members, browse most popular/recommended/trending groups |
| WebMed | Health A–Z, Drugs and supplements, Living healthy, Family and pregnancy, News and experts | Search topics relevant to health A–Z; check symptoms; find a doctor; find lowest drug prices; search drugs and medicines A–Z, as well as browse latest drug news; recipe finders, foot calorie counters, fitness calorie counters, calcium counters, food and fitness planners and portion size plates |
| HealthUnlocked | Drug-, condition- and wellness-related community search | Find communities relevant to your conditions; browse posts, polls, followers and basic introduction of specific communities; browse health topics in common drugs, condition communities, and wellness communities; share experiences and follow patients like you |
| Criterion | N | Count | Percent (%) |
|---|---|---|---|
| Terms of use | 100 | 98 | 98 |
| Privacy | 100 | 92 | 92 |
| Contents related to health-care | 100 | 89 | 89 |
| Information recommendation | 100 | 88 | 88 |
| Social functions | 100 | 84 | 84 |
| Mission to improve health literacy | 100 | 70 | 70 |
| Mission or purpose | 100 | 66 | 66 |
| Contents by doctors or patients | 100 | 66 | 66 |
| Open subscription network | 100 | 59 | 59 |
| Commercial purpose | 100 | 58 | 58 |
| Feedback (form) | 100 | 49 | 49 |
| Knowledge directory | 100 | 42 | 42 |
| Heath-related decision making | 100 | 33 | 33 |
| Comprehensive websites | 100 | 32 | 32 |
| Disease-specific websites | 100 | 29 | 29 |
| Commercial introduction | 100 | 24 | 24 |
| Social websites | 100 | 11 | 11 |
| Patients’ charts and journals | 100 | 3 | 3 |
| Statistical results of patient-reported outcomes | 100 | 1 | 1 |
| Criterion | Average Percent (%) | Average Score |
|---|---|---|
| 1. Provide clear feedback signals for actions | 98.50 | 3.925 |
| 2. Make clickable elements evident | 99.30 | 3.870 |
| 3. Use conventional interaction elements | 99.30 | 3.795 |
| 4. Minimize vertical scrolling | 93.00 | 3.740 |
| 5. Offer a functional home page | 85.30 | 3.680 |
| 6. Provide clear feedback signals for actions | 73.30 | 3.230 |
| 7. Ensure that the back button behaves predictably | 69.00 | 3.050 |
| 8. Ensure site is accessible for users with disabilities and uses elements of 508 compliance | 56.00 | 2.620 |
| 9. Incorporate multimedia | 37.00 | 2.090 |
| Criterion | Average Percent (%) | Average Score |
|---|---|---|
| 10. Ensure texts and background colours contrast | 100.00 | 3.945 |
| 11. Present a clear visual hierarchy | 98.50 | 3.858 |
| 12. Visually group-related topics | 95.70 | 3.820 |
| 13. Make elements on the page easy to read | 99.30 | 3.790 |
| 14. Make pages easy to skim or scan | 95.00 | 3.780 |
| 15. Clearly label content categories | 94.00 | 3.765 |
| 16. Provide easy search functionality | 54.00 | 2.568 |
| Criterion | Average Percent (%) | Average Score |
|---|---|---|
| 17. Use users’ language; minimize jargon and technical terms | 59.00 | 3.290 |
| 18. Allow for interaction with the content | 82.00 | 3.260 |
| 19. Focus the writing on audience and purpose | 81.50 | 3.193 |
| Criterion | Percentage |
|---|---|
| It has a health-related news list | 76% |
| It has a sharing function to help share their web pages | 71% |
| It has relevant topics in the home page | 50% |
| It has basic social functions like posting and commenting | 49% |
| Knowledge categories have subcategories | 41% |
| Finding information is convenient for patients | 39% |
| The main goal of the site is to provide social services | 35% |
| It provides details of specific biomedical terms and topics | 31% |
| It has an open subscription network | 28% |
| It has the function of “find doctors” or “find experts” | 25% |
| It has certain knowledge graphs connecting different concepts | 23% |
| It has health evaluation tools | 15% |
| It has a research support function | 14% |
| It has hyperlinks to external health-related websites | 12% |
| It has a patient searching function | 10% |
| It has certain charts to show the changes of health conditions | 10% |
| It provides summarized results on the basis of patient-reported data | 7% |
| It uses codes of terminology from health-care domain knowledge | 1% |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, D.; Zhang, R.; Liu, K.; Hou, L. Enhancing Online Patient Support through Health-Care Knowledge in Online Health Communities: A Descriptive Study. Information 2018, 9, 199. https://doi.org/10.3390/info9080199
Chen D, Zhang R, Liu K, Hou L. Enhancing Online Patient Support through Health-Care Knowledge in Online Health Communities: A Descriptive Study. Information. 2018; 9(8):199. https://doi.org/10.3390/info9080199
Chicago/Turabian StyleChen, Donghua, Runtong Zhang, Kecheng Liu, and Lei Hou. 2018. "Enhancing Online Patient Support through Health-Care Knowledge in Online Health Communities: A Descriptive Study" Information 9, no. 8: 199. https://doi.org/10.3390/info9080199
APA StyleChen, D., Zhang, R., Liu, K., & Hou, L. (2018). Enhancing Online Patient Support through Health-Care Knowledge in Online Health Communities: A Descriptive Study. Information, 9(8), 199. https://doi.org/10.3390/info9080199





