Can Dissociation Mediate the Relationship between Emotional Dysregulation and Intelligence? An Empirical Study Involving Adolescents with and without Complex Trauma Histories
Abstract
:1. Introduction
1.1. Complex Trauma
1.1.1. Attachment
1.1.2. Biology
1.1.3. Affect Regulation
1.1.4. Dissociation
1.1.5. Behavioral Control
1.1.6. Cognition
1.1.7. Self-Concept
1.2. Aims of the Study
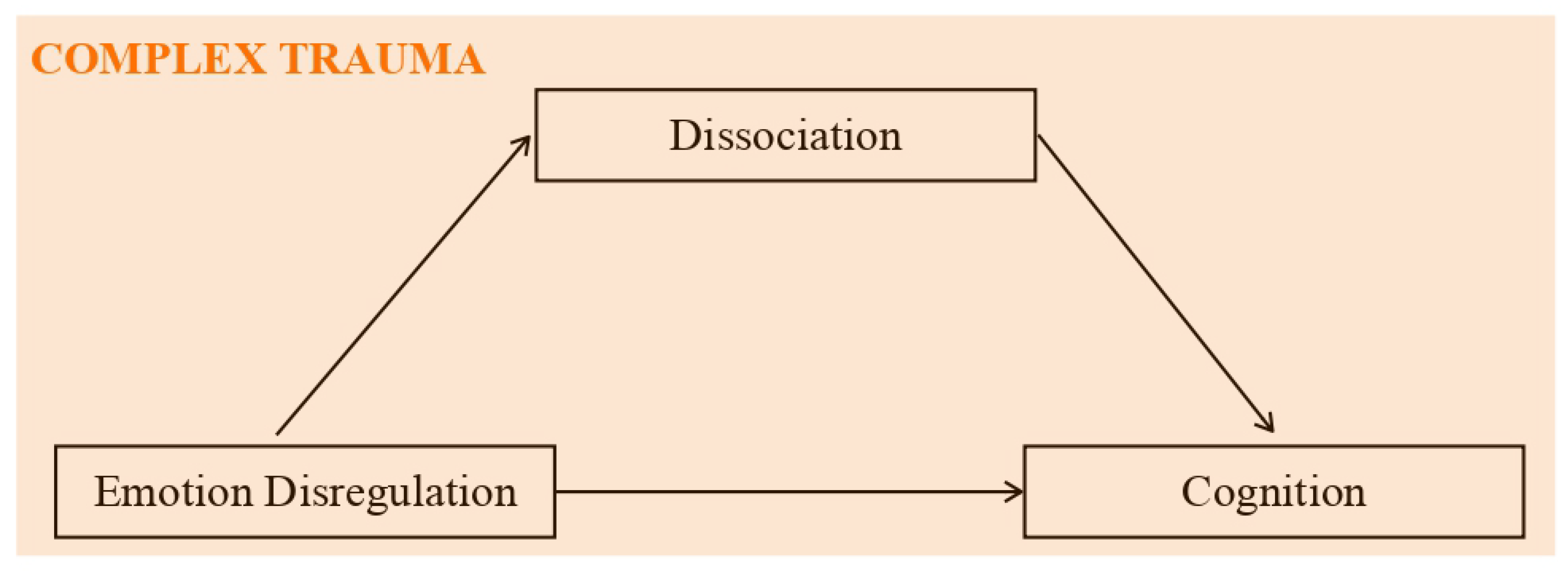
1.3. Mediation Model: Theoretical Bases
2. Materials and Methods
2.1. Goals
2.2. Sample
2.3. Instruments
2.4. Procedure
2.5. Statistical Analysis
3. Results
- Model 1. The first significant model (p value = 0.04) featured the total DERS scores as the independent variable (IV), the dissociation scale of TSCC (TSCC_Dissociation) as the mediator, and the processing speed index (PSI) as the dependent variable (DV) (Figure 4);
- Model 2. The second model that almost reached the threshold for significance (p value = 0.06) adopted the non-acceptance sub-scale of DERS as the independent variable (IV), TSCC_Dissociation as the mediator, and the processing speed index (PSI) as the dependent variable (DV) (Figure 5);
- Model 3. The third significant model (p value = 0.03) took the non-acceptance DERS sub-scales as independent variables (IV), TSCC_Dissociation as the mediator, and the PSI as the dependent variable (DV) (Figure 6);
- Model 4. The fourth model, which reaches the significance threshold (p value = 0.05), adopted the awareness sub-scale of DERS as the independent variable (IV), the A-DES scale as the mediator, and PSI as the dependent variable (DV) (Figure 7);
- Model 5. The fifth model was close to the significance threshold (p value = 0.06) and featured the clarity sub-scale of DERS as the independent variable (IV), A-DES as the mediator, and PSI as the dependent variable (DV) (Figure 8);
- Model 6. The sixth significant model (p value = 0.05) featured the clarity sub-scale of DERS as an independent variable (IV), A-DES as the mediator, and the intelligence quotient (IQ) as the dependent variable (DV) (Figure 9).
Moderated Mediation Model Controlled for Gender
4. Discussion
4.1. Analysis of Variance (ANOVA)
4.2. Moderated Mediation Model
4.3. Further Considerations about the Sample
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Marks, J.S. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. Am. J. Prev. Med. 1998, 14, 245–258. [Google Scholar] [CrossRef] [PubMed]
- Van Der Kolk, B. Il Corpo Accusa il Colpo: Mente, Corpo e Cervello Nell’elaborazione delle Memorie Traumatiche; Raffaello Cortina Editore: Milano, Italy, 2015. [Google Scholar]
- Fairbank, J.A.; Fairbank, D.W. Epidemiology of child traumatic stress. Curr. Psychiatry Rep. 2009, 11, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Castelli, B.; Festa, F.; Di Sanzo, M.A.; Guala, A.; Pellai, A. Prevalence of child sexual abuse: A comparison among 4 Italian epidemiological studies. Pediatr. Medica Chir. 2015, 37, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Cook, A.; Spinazzola, J.; Ford, J.; Lanktree, C.; Blaustein, M.; Cloitre, M.; Van der Kolk, B. Complex trauma. Psychiatr. Ann. 2005, 35, 390–398. [Google Scholar] [CrossRef] [Green Version]
- Lanius, R.; Vermetten, E.; Pain, C. L’impatto del Trauma Infantile Sulla Salute e Sulla Malattia. L’epidemia Nascosta; Giovanni Fioritti Editore: Roma, Italy, 2012. [Google Scholar]
- Siegel, D. The Developing Mind: How Relationships and the Brain Interact to Shape Who We Are, 2nd ed.; Raffaello Cortina Editore: Milano, Italy, 2012. [Google Scholar]
- Lis, A.; Mazzeschi, C.; Salcuni, S. Modelli di Intervento Nella Relazione Familiare; Carocci: Roma, Italy, 2005. [Google Scholar]
- Ricciutello, C.; Cheli, M.; Montenegro, M.E.; Campieri, M.; Fini, A.; Pincanelli, F. Violenza intrafamiliare e salute mentale in adolescenza: Il trauma complesso come disturbo dello sviluppo. Riv. Psichiatr. 2012, 47, 413–423. [Google Scholar]
- LeDoux, J. Synaptic Self: How Our Brains Become Who We Are; Penguin: London, UK, 2002. [Google Scholar]
- McEwen, B.S. Stress, adaptation, and disease: Allostasis and allostatic load. Ann. N. Y. Acad. Sci. 1998, 840, 33–44. [Google Scholar] [CrossRef]
- Van der Kolk, B.A. The neurobiology of childhood trauma and abuse. Child Adolesc. Psychiatr. Clin. 2003, 12, 293–317. [Google Scholar] [CrossRef]
- Kim, J.; Cicchetti, D. Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. J. Child Psychol. Psychiatry 2010, 51, 706–716. [Google Scholar] [CrossRef] [Green Version]
- Putnam, F.W. Dissociation in Children and Adolescents: A Developmental Perspective; Guilford Press: Guilford, CA, USA, 1997. [Google Scholar]
- Allen, J.G. Traumatic Relationships and Serious Mental Disorders; John Wiley & Sons Ltd.: Hoboken, NJ, USA, 2001. [Google Scholar]
- Crittenden, P.M.; DiLalla, D.L. Compulsive compliance: The development of an inhibitory coping strategy in infancy. J. Abnorm. Child Psychol. 1988, 16, 585–599. [Google Scholar] [CrossRef]
- Koenen, K.C.; Moffitt, T.E.; Caspi, A.; Taylor, A.; Purcell, S. Domestic violence is associated with environmental suppression of IQ in young children. Dev. Psychopathol. 2003, 15, 297–311. [Google Scholar] [CrossRef] [Green Version]
- Jiménez, E.; Solé, B.; Arias, B.; Mitjans, M.; Varo, C.; Reinares, M.; Bonnín, C.d.M.; Ruíz, V.; Saiz, P.A.; García-Portilla, M.P.; et al. Impact of childhood trauma on cognitive profile in bipolar disorder. Bipolar Disord. 2017, 19, 363–374. [Google Scholar] [CrossRef] [PubMed]
- Beers, S.R.; De Bellis, M.D. Neuropsychological function in children with maltreatment-related posttraumatic stress disorder. Am. J. Psychiatry 2002, 159, 483–486. [Google Scholar] [CrossRef] [PubMed]
- Livesley, W.J.; Dimaggio, G.; Clarkin, J.F. Integrated Treatment for Personality Disorder: A Modular Approach; Guilford Publications: Guilford, CA, USA, 2016. [Google Scholar]
- Cavicchioli, M.; Scalabrini, A.; Northoff, G.; Mucci, C.; Ogliari, A.; Maffei, C. Dissociation and emotion regulation strategies: A meta-analytic review. J. Psychiatr. Res. 2021, 143, 370–387. [Google Scholar] [CrossRef] [PubMed]
- Blair, C. School readiness: Integrating cognition and emotion in a neurobiological conceptualization of children’s functioning at school entry. Am. Psychol. 2002, 57, 111. [Google Scholar] [CrossRef]
- Gross, J.J. Emotion regulation: Affective, cognitive, and social consequences. Psychophysiology 2002, 39, 281–291. [Google Scholar] [CrossRef] [Green Version]
- Viau-Quesnel, C.; Savary, M.; Blanchette, I. Reasoning and concurrent timing: A study of the mechanisms underlying the effetct of emotion on reasoning. Cogn. Emot. 2019, 33, 1020–1030. [Google Scholar] [CrossRef]
- Slovic, P.; Finucane, M.L.; Peters, E.; MacGregor, D.G. Risk as analysis and risk as feelings: Some thoughts about affect, reason, risk and rationality. In The Feeling of Risk; Routledge: London, UK, 2013; pp. 21–36. [Google Scholar]
- Shalev, A.Y.; Rogel-Fuchs, Y. Psychophysiology of the posttraumatic stress disorder: From sulfur fumes to behavioral genetics. Psychosom. Med. 1993, 55, 413–423. [Google Scholar] [CrossRef]
- Navarro-Haro, M.V.; Wessman, I.; Botella, C.; García-Palacios, A. The role of emotion regulation strategies and dissociation in non-suicidal self-injury for women with borderline personality disorder and comorbid eating disorder. Compr. Psychiatry 2015, 63, 123–130. [Google Scholar] [CrossRef] [Green Version]
- Briere, J.; Hodges, M.; Godbout, N. Traumatic stress, affect dysregulation, and dysfunctional avoidance: A structural equation model. J. Trauma. Stress 2010, 23, 767–774. [Google Scholar] [CrossRef]
- Baumeister, R.F.; Dale, K.; Sommer, K.L. Freudian defense mechanisms and empirical findings in modern social psychology: Reaction formation, projection, displacement, undoing, isolation, sublimation, and denial. J. Personal. 1998, 66, 1081–1124. [Google Scholar] [CrossRef]
- Mohiyeddini, C.; Semple, S. Displacement behaviour regulates the experience of stress in men. Stress 2013, 16, 163–171. [Google Scholar] [CrossRef] [PubMed]
- McWilliams, N. Psychoanalytic Diagnosis: Understanding Personality Structure in the Clinical Process; Guilford Press: Guilford, CA, USA, 2011. [Google Scholar]
- Hébert, M.; Langevin, R.; Oussaïd, E. Cumulative childhood trauma, emotion regulation, dissociation, and behavior problems in school-aged sexual abuse victims. J. Affect. Disord. 2018, 225, 306–312. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henschel, S.; Doba, K.; Nandrino, J.L. Emotion Regulation Processes and Psychoform and Somatoform Dissociation in Adolescents and Young Adults with Cumulative Maltreatment. J. Trauma Dissociation 2019, 20, 197–211. [Google Scholar] [CrossRef] [PubMed]
- Kaplow, J.B.; Hall, E.; Koenen, K.C.; Dodge, K.A.; Amaya-Jackson, L. Dissociation predicts later attention problems in sexually abused children. Child Abus. Negl. 2008, 32, 261–275. [Google Scholar] [CrossRef] [Green Version]
- De Bellis, M.D.; Woolley, D.P.; Hooper, S.R. Neuropsychological findings in pediatric maltreatment: Relationship of PTSD, dissociative symptoms, and abuse/neglect indices to neurocognitive outcomes. Child Maltreat. 2013, 18, 171–183. [Google Scholar] [CrossRef] [Green Version]
- Haaland, V.; Landrø, N. Pathological dissociation and neuropsychological functioning in borderline personality disorder. Acta Psychiatr. Scand. 2009, 119, 383–392. [Google Scholar] [CrossRef]
- Brewin, C.R.; Ma, B.Y.; Colson, J. Effects of experimentally induced dissociation on attention and memory. Conscious. Cogn. 2013, 22, 315–323. [Google Scholar] [CrossRef]
- DePrince, A.P.; Weinzierl, K.M.; Combs, M.D. Executive function performance and trauma exposure in a community sample of children. Child Abus. Negl. 2009, 33, 353–361. [Google Scholar] [CrossRef]
- Freyd, J.J.; Martorello, S.R.; Alvarado, J.S.; Hayes, A.E.; Christman, J.C. Cognitive environments and dissociative tendencies: Performance on the standard Stroop task for high versus low dissociators. Appl. Cogn. Psychol. Off. J. Soc. Appl. Res. Mem. Cogn. 1998, 12, S91–S103. [Google Scholar] [CrossRef]
- Guralnik, O.; Giesbrecht, T.; Knutelska, M.; Sirroff, B.; Simeon, D. Cognitive functioning in depersonalization disorder. J. Nerv. Ment. Dis. 2007, 195, 983–988. [Google Scholar] [CrossRef]
- Simeon, D.; Guralnik, O.; Hazlett, E.A.; Spiegel-Cohen, J.; Hollander, E.; Buchsbaum, M.S. Feeling unreal: A PET study of depersonalization disorder. Am. J. Psychiatry 2000, 157, 1782–1788. [Google Scholar] [CrossRef] [PubMed]
- Černis, E.; Evans, R.; Ehlers, A.; Freeman, D. Dissociation in relation to other mental health conditions: An exploration using network analysis. J. Psychiatr. Res. 2021, 136, 460–467. [Google Scholar] [CrossRef] [PubMed]
- Sighinolfi, C.; Pala, A.N.; Chiri, L.R.; Marchetti, I.; Sica, C. Difficulties in emotion regulation scale (DERS): Traduzione e adattamento italiano. Psicoter. Cogn. E Comport. 2010, 16, 141–170. [Google Scholar]
- Luciano, G.; F, A.; Gaia, D.C.; Alessandro, Z.; Claudia, P. Developing age and gender adjusted normative reference values for the Difficulties in Emotion Regulation Scale (DERS). J. Psychopathol. Behav. Assess. 2017, 39, 705–714. [Google Scholar]
- Fossati, A.; Feeney, J.; Maffei, C.; Borroni, S. Thinking about feelings: Affective state mentalization, attachment styles, and borderline personality disorder features among Italian nonclinical adolescents. Psychoanal. Psychol. 2014, 31, 41. [Google Scholar] [CrossRef]
- Fossati, A.; Gratz, K.L.; Maffei, C.; Borroni, S. Impulsivity dimensions, emotion dysregulation, and borderline personality disorder features among Italian nonclinical adolescents. Borderline Personal. Disord. Emot. Dysregulation 2014, 1, 5. [Google Scholar] [CrossRef] [Green Version]
- Pace, C.S.; Guiducci, V.; Cavanna, D. Attachment in eating-disordered outpatients with and without borderline personality disorder. J. Health Psychol. 2017, 22, 1808–1818. [Google Scholar] [CrossRef]
- De Ruiter, M.B.; Phaf, R.H.; Elzinga, B.M.; van Dyck, R. Dissociative style and individual differences in verbal working memory span. Conscious. Cogn. 2004, 13, 821–828. [Google Scholar] [CrossRef]
- Scroppo, J.C.; Drob, S.L.; Weinberger, J.L.; Eagle, P. Identifying dissociative identity disorder: A self-report and projective study. J. Abnorm. Psychol. 1998, 107, 272. [Google Scholar] [CrossRef]
- Sundermann, J.M.; Chu, A.T.; DePrince, A.P. Cumulative violence exposure, emotional nonacceptance, and mental health symptoms in a community sample of women. J. Trauma Dissociation 2013, 14, 69–83. [Google Scholar] [CrossRef] [Green Version]
- Bonanno, G.A.; Keltner, D.; Holen, A.; Horowitz, M.J. When avoiding unpleasant emotions might not be such a bad thing: Verbal-autonomic response dissociation and midlife conjugal bereavement. J. Personal. Soc. Psychol. 1995, 69, 975. [Google Scholar] [CrossRef]
- Khawaja, N.G.; Stallman, H.M. Understanding the coping strategies of international students: A qualitative approach. J. Psychol. Couns. Sch. 2011, 21, 203–224. [Google Scholar] [CrossRef] [Green Version]
- Majohr, K.L.; Leenen, K.; Grabe, H.J.; Jenewein, J.; Nuñez, D.G.; Rufer, M. Alexithymia and its relationship to dissociation in patients with panic disorder. J. Nerv. Ment. Dis. 2011, 199, 773–777. [Google Scholar] [CrossRef] [PubMed]
- Modestin, J.; Lötscher, K.; Erni, T. Dissociative experiences and their correlates in young non-patients. Psychol. Psychother. Theory Res. Pract. 2002, 75, 53–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Craparo, G. Addiction, dissociazione e inconscio non rimosso. Un contributo teorico secondo la prospettiva evolutivo-relazionale. Ric. Psicoanal. 2013, 2, 73–84. [Google Scholar] [CrossRef]









| IV = Group | Control Group | Clinical Group | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| DV | R2 | df | F | p | N | M | SD | N | M | SD |
| IQ | 0.49 | 1.60 | 56.62 | <0.001 | 33 | 108.67 | 11.77 | 29 | 79.76 | 18.17 |
| VCI | 0.51 | 1.62 | 64.08 | <0.001 | 33 | 110.24 | 13.28 | 31 | 81.39 | 15.53 |
| VSI | 0.30 | 1.62 | 26.08 | <0.001 | 33 | 111.33 | 13.55 | 31 | 87.97 | 22.26 |
| WMI | 0.20 | 1.62 | 15.76 | <0.001 | 33 | 98.33 | 11.69 | 31 | 82.13 | 20.12 |
| PSI | 0.47 | 1.62 | 54.02 | <0.001 | 33 | 103.09 | 11.94 | 31 | 76.97 | 16.29 |
| IV = Group | |||
|---|---|---|---|
| DV | df | F | p |
| DERS_Total Score | 1.62 | 0.47 | 0.50 |
| non-acceptance | 1.62 | 0.03 | 0.87 |
| goals | 1.62 | 0.58 | 0.45 |
| impulse | 1.62 | 0.28 | 0.60 |
| awareness | 1.62 | 2.83 | 0.10 |
| strategies | 1.62 | 2.77 | 0.10 |
| clarity | 1.62 | 2.21 | 0.14 |
| A-DES | 1.62 | 2.14 | 0.15 |
| TSCC_Dissociation | 1.62 | 0.98 | 0.33 |
| Moderator Level = Control Group | |||
|---|---|---|---|
| Model | Effect | Beta | p |
| Model 1 | DERS_TOT ⇒ TSCC_DIS ⇒ PSI | 0.12 | 0.06 |
| DERS_TOT ⇒ TSCC_DIS | 0.47 | 0.02 | |
| TSCC_DIS ⇒ PSI | 0.26 | 0.003 | |
| Model 2 | NONACC ⇒ TSCC_DIS ⇒ PSI | 0.10 | 0.07 |
| NONACC ⇒ TSCC_DIS | 0.43 | 0.01 | |
| TSCC_DIS ⇒ PSI | 0.23 | 0.01 | |
| Model 3 | STRAT ⇒ TSCC_DIS ⇒ PSI | 0.10 | 0.11 |
| STRAT ⇒ TSCC_DIS | 0.40 | 0.06 | |
| TSCC_DIS ⇒ PSI | 0.25 | 0.005 | |
| Model 4 | AWAR ⇒ A-DES ⇒PSI | 0.10 | 0.10 |
| AWAR ⇒ A-DES | 0.50 | 0.01 | |
| A-DES ⇒ PSI | 0.20 | 0.02 | |
| Model 5 | CLARITY ⇒ A-DES ⇒ PSI | 0.12 | 0.09 |
| CLARITY ⇒ A-DES | 0.63 | 0.002 | |
| A-DES ⇒ PSI | 0.19 | 0.04 | |
| Model 6 | CLARITY ⇒ A-DES ⇒ IQ | 0.11 | 0.11 |
| CLARITY ⇒ A-DES | 0.63 | 0.002 | |
| A-DES ⇒ IQ | 0.18 | 0.06 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cristofanelli, S.; Baccini, G.; Centonze, E.; Colombesi, A.; Cariello, M.; Ferro, L. Can Dissociation Mediate the Relationship between Emotional Dysregulation and Intelligence? An Empirical Study Involving Adolescents with and without Complex Trauma Histories. Int. J. Environ. Res. Public Health 2023, 20, 1729. https://doi.org/10.3390/ijerph20031729
Cristofanelli S, Baccini G, Centonze E, Colombesi A, Cariello M, Ferro L. Can Dissociation Mediate the Relationship between Emotional Dysregulation and Intelligence? An Empirical Study Involving Adolescents with and without Complex Trauma Histories. International Journal of Environmental Research and Public Health. 2023; 20(3):1729. https://doi.org/10.3390/ijerph20031729
Chicago/Turabian StyleCristofanelli, Stefania, Giorgia Baccini, Eleonora Centonze, Alessandra Colombesi, Marina Cariello, and Laura Ferro. 2023. "Can Dissociation Mediate the Relationship between Emotional Dysregulation and Intelligence? An Empirical Study Involving Adolescents with and without Complex Trauma Histories" International Journal of Environmental Research and Public Health 20, no. 3: 1729. https://doi.org/10.3390/ijerph20031729





