Titanium Lattice Structures Produced via Additive Manufacturing for a Bone Scaffold: A Review
Abstract
:1. Introduction
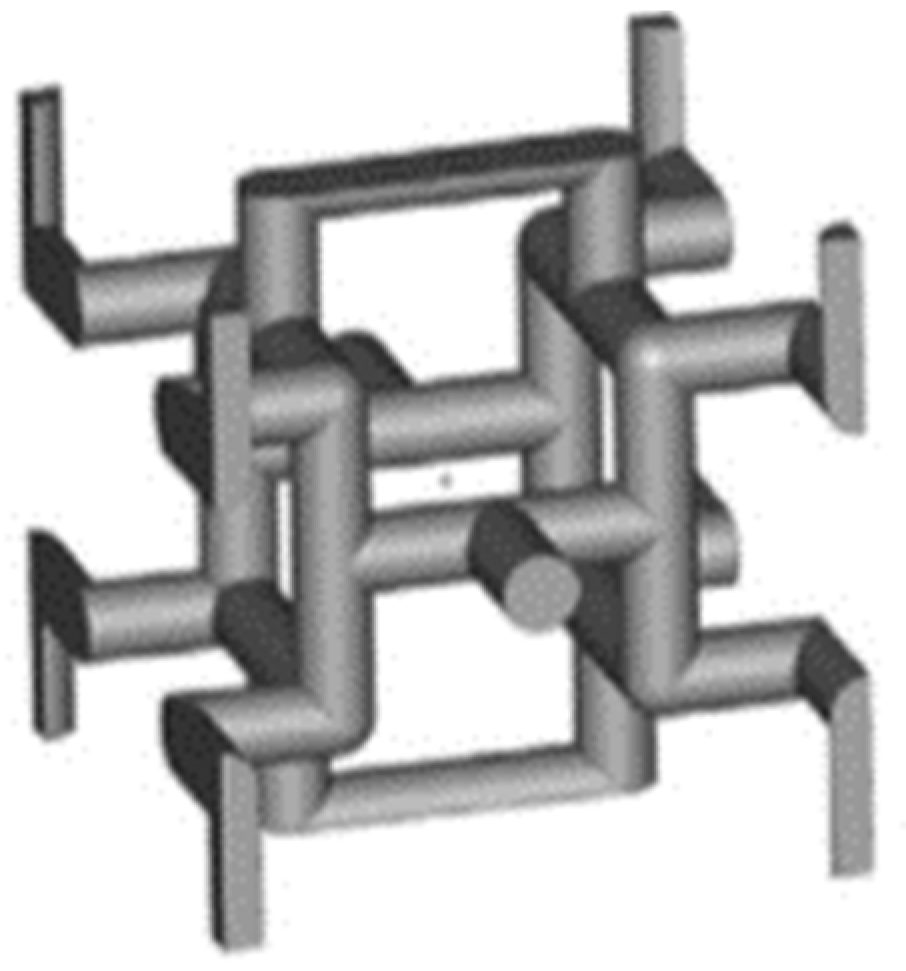
2. Classification of Lattice Structures
3. Current Status of Additive Manufacturing Technologies
4. Mechanical and Morphological Requirements for Biomedical Applications
4.1. Effect of Pore Size
4.2. Effect of Surface Roughness
4.3. Effect of Elastic Modulus
5. The Gibson–Ashby Model
5.1. Compressive Behaviour
5.2. Comparison of Experimental Data for Different Lattice Materials
6. Biomedical Device Case Studies
7. Concluding Remarks
- Data analysis of the results of the pore size effect on the bone ingrowth of eleven studies showed a wide range of optimal pore sizes from 100 up to 1000 μm, with an optimal mean value of 522 μm. The comparison showed little discrepancies, since works that evaluated comparable ranges of pore sizes found different optimal results.
- The analysis of the effect of surface roughness showed that minimal differences in the roughness values do not affect the cell adhesion and proliferation. In other studies, the comparison of a wide range values from 3 to 8 μm showed that the optimal surface roughness values are between 6 and 8 μm.
- Findings on the effect of the elastic modulus showed that reducing the implant stiffness to that of human bone improves stress stimulation and reduces stress shielding. Several studies with implants having an elastic modulus comparable to that of human bone revealed no significant influence of elastic material properties on bone ingrowth.
- The Gibson–Ashby model is useful for comparing the mechanical performance of lattice structures and confirmed the suitability of the Ti6Al4V alloy for biomedical applications. Indeed, the collected results showed that the elastic modulus of the selected lattice materials, with relative densities under 30%, falls within the range of the cancellous bone elastic modulus.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Nomenclature
| TPMS | triply periodic minimal surface |
| AM | additive manufacturing |
| SLM | selective laser melting |
| SLS | selective laser sintering |
| DMLS | direct metal laser sintering |
| EBM | electron beam melting |
| BCC | body-centred cubic |
| FCC | face-centred cubic |
| BCCZ | body-centred cubic with vertical struts |
| FCCZ | face-centred cubic with vertical struts |
| SCBCC | simple cubic body-centred cubic |
| TC | truncated cube |
| TO | truncated octahedron |
| RCO | rhombicuboctahedron |
| TCO | truncated cuboctahedron |
| RD | rhombic dodecahedron |
| TAOR | triply arranged octagonal rings |
| τ | complex variable |
| θ | Bonnet angle |
| R(τ) | TPMS function |
| γ | position vector in the Euclidean space |
| Ak | amplitude factor |
| hk | kth grid vector in the reciprocal space |
| λk | periodic wavelength |
| pk | phase offset |
| C | constant factor related to porosity |
| M | Maxwell number |
| S | number of struts |
| N | number of nodes |
| E* | elastic modulus of the lattice structure |
| σ* | compressive strength of the lattice structure |
| Es | elastic modulus of the parent material |
| σs | compressive strength of the parent material |
| FEA | finite element analysis |
| PEEK | polyetheretherketone |
| CT | computed tomography |
References
- Zadpoor, A.A. Mechanical Performance of Additively Manufactured Meta-Biomaterials. Acta Biomater. 2019, 85, 41–59. [Google Scholar] [CrossRef]
- Gibson, L.J.; Ashby, M.F. Cellular Solids—Structure and Properties; Cambridge University Press: Cambridge, UK, 1997. [Google Scholar]
- Al-Ketan, O.; Rowshan, R.; Abu Al-Rub, R.K. Topology-Mechanical Property Relationship of 3D Printed Strut, Skeletal, and Sheet Based Periodic Metallic Cellular Materials. Addit. Manuf. 2018, 19, 167–183. [Google Scholar] [CrossRef]
- Ngo, T.D.; Kashani, A.; Imbalzano, G.; Nguyen, K.T.Q.; Hui, D. Additive Manufacturing (3D Printing): A Review of Materials, Methods, Applications and Challenges. Compos. Part B Eng. 2018, 143, 172–196. [Google Scholar] [CrossRef]
- Huang, Y.; Leu, M.C.; Mazumder, J.; Donmez, A. Additive Manufacturing: Current State, Future Potential, Gaps and Needs, and Recommendations. J. Manuf. Sci. Eng. 2015, 137, 014001. [Google Scholar] [CrossRef] [Green Version]
- Bhushan, S.; Singh, S.; Maiti, T.K.; Sharma, C.; Dutt, D.; Sharma, S.; Li, C.; Tag Eldin, E.M. Scaffold Fabrication Techniques of Biomaterials for Bone Tissue Engineering: A Critical Review. Bioengineering 2022, 9, 728. [Google Scholar] [CrossRef] [PubMed]
- Louvis, E.; Fox, P.; Sutcliffe, C.J. Selective Laser Melting of Aluminium Components. J. Mater. Process. Technol. 2011, 211, 275–284. [Google Scholar] [CrossRef]
- Mazzoli, A. Selective Laser Sintering in Biomedical Engineering. Med. Biol. Eng. Comput. 2013, 51, 245–256. [Google Scholar] [CrossRef]
- Simchi, A.; Petzoldt, F.; Pohl, H. On the Development of Direct Metal Laser Sintering for Rapid Tooling. J. Mater. Process. Technol. 2003, 141, 319–328. [Google Scholar] [CrossRef]
- Körner, C. Additive Manufacturing of Metallic Components by Selective Electron Beam Melting—A Review. Int. Mater. Rev. 2016, 61, 361–377. [Google Scholar] [CrossRef] [Green Version]
- Maconachie, T.; Leary, M.; Tran, P.; Harris, J.; Liu, Q.; Lu, G.; Ruan, D.; Faruque, O.; Brandt, M. The Effect of Topology on the Quasi-Static and Dynamic Behaviour of SLM AlSi10Mg Lattice Structures. Int. J. Adv. Manuf. Technol. 2022, 118, 4085–4104. [Google Scholar] [CrossRef]
- Kim, T.; Zhao, C.Y.; Lu, T.J.; Hodson, H.P. Convective Heat Dissipation with Lattice-Frame Materials. Mech. Mater. 2004, 36, 767–780. [Google Scholar] [CrossRef]
- du Plessis, A.; Yadroitsava, I.; Yadroitsev, I.; le Roux, S.G.; Blaine, D.C. Numerical Comparison of Lattice Unit Cell Designs for Medical Implants by Additive Manufacturing. Virtual Phys. Prototyp. 2018, 13, 266–281. [Google Scholar] [CrossRef]
- Vilardell, A.M.; Takezawa, A.; du Plessis, A.; Takata, N.; Krakhmalev, P.; Kobashi, M.; Yadroitsava, I.; Yadroitsev, I. Topology Optimization and Characterization of Ti6Al4V ELI Cellular Lattice Structures by Laser Powder Bed Fusion for Biomedical Applications. Mater. Sci. Eng. A 2019, 766, 138330. [Google Scholar] [CrossRef]
- Yan, C.; Hao, L.; Hussein, A.; Young, P. Ti-6Al-4V Triply Periodic Minimal Surface Structures for Bone Implants Fabricated via Selective Laser Melting. J. Mech. Behav. Biomed. Mater. 2015, 51, 61–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caiazzo, F.; Alfieri, V.; Bujazha, B.D. Additive Manufacturing of Biomorphic Scaffolds for Bone Tissue Engineering. Int. J. Adv. Manuf. Technol. 2021, 113, 2909–2923. [Google Scholar] [CrossRef]
- Liu, X.; Chu, P.K.; Ding, C. Surface Modification of Titanium, Titanium Alloys, and Related Materials for Biomedical Applications. Mater. Sci. Eng. R Rep. 2004, 47, 49–121. [Google Scholar] [CrossRef] [Green Version]
- Abdel-Hady Gepreel, M.; Niinomi, M. Biocompatibility of Ti-Alloys for Long-Term Implantation. J. Mech. Behav. Biomed. Mater. 2013, 20, 407–415. [Google Scholar] [CrossRef]
- Long, M.; Rack, H.J. Titanium Alloys in Total Joint Replacement—A Materials Science Perspective. Biomaterials 1998, 19, 1621–1639. [Google Scholar] [CrossRef]
- Petersen, A.; Joly, P.; Bergmann, C.; Korus, G.; Duda, G.N. The Impact of Substrate Stiffness and Mechanical Loading on Fibroblast-Induced Scaffold Remodeling. Tissue Eng. Part A 2012, 18, 1804–1817. [Google Scholar] [CrossRef]
- Breuls, R.G.M.; Jiya, T.U.; Smit, T.H. Scaffold Stiffness Influences Cell Behavior: Opportunities for Skeletal Tissue Engineering. Open Orthop. J. 2008, 2, 103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rack, H.J.; Qazi, J.I. Titanium Alloys for Biomedical Applications. Mater. Sci. Eng. C 2006, 26, 1269–1277. [Google Scholar] [CrossRef]
- Li, F.; Li, J.; Xu, G.; Liu, G.; Kou, H.; Zhou, L. Fabrication, Pore Structure and Compressive Behavior of Anisotropic Porous Titanium for Human Trabecular Bone Implant Applications. J. Mech. Behav. Biomed. Mater. 2015, 46, 104–114. [Google Scholar] [CrossRef] [PubMed]
- Chang, B.; Song, W.; Han, T.; Yan, J.; Li, F.; Zhao, L.; Kou, H.; Zhang, Y. Influence of Pore Size of Porous Titanium Fabricated by Vacuum Diffusion Bonding of Titanium Meshes on Cell Penetration and Bone Ingrowth. Acta Biomater. 2016, 33, 311–321. [Google Scholar] [CrossRef]
- Rnjak-Kovacina, J.; Wise, S.G.; Li, Z.; Maitz, P.K.M.; Young, C.J.; Wang, Y.; Weiss, A.S. Tailoring the Porosity and Pore Size of Electrospun Synthetic Human Elastin Scaffolds for Dermal Tissue Engineering. Biomaterials 2011, 32, 6729–6736. [Google Scholar] [CrossRef] [PubMed]
- Shalabi, M.M.; Gortemaker, A.; Van’t Hof, M.A.; Jansen, J.A.; Creugers, N.H.J. Implant Surface Roughness and Bone Healing: A Systematic Review. J. Dent. Res. 2006, 85, 496–500. [Google Scholar] [CrossRef] [PubMed]
- Krishna Alla, R.; Ginjupalli, K.; Upadhya, N.; Shammas, M.; Krishna Ravi, R.; Sekhar, R. Surface Roughness of Implants: A Review. Trends Biomater. Artif. Organs 2011, 25, 112–118. [Google Scholar]
- Gibson, L.J.; Ashby, M.F. Mechanics of Three-Dimensional Cellular Materials. Proc. R. Soc. Lond. A. Math. Phys. Sci. 1982, 382, 43–59. [Google Scholar] [CrossRef]
- Maconachie, T.; Leary, M.; Lozanovski, B.; Zhang, X.; Qian, M.; Faruque, O.; Brandt, M. SLM Lattice Structures: Properties, Performance, Applications and Challenges. Mater. Des. 2019, 183, 108137. [Google Scholar] [CrossRef]
- Deshpande, V.S.; Fleck, N.A.; Ashby, M.F. Effective Properties of the Octet-Truss Lattice Material. J. Mech. Phys. Solids 2001, 49, 1747–1769. [Google Scholar] [CrossRef] [Green Version]
- Peng, C.; Tran, P.; Nguyen-Xuan, H.; Ferreira, A.J.M. Mechanical Performance and Fatigue Life Prediction of Lattice Structures: Parametric Computational Approach. Compos. Struct. 2020, 235, 111821. [Google Scholar] [CrossRef]
- Wu, M.W.; Chen, J.K.; Lin, B.H.; Chiang, P.H.; Tsai, M.K. Compressive Fatigue Properties of Additive-Manufactured Ti-6Al-4V Cellular Material with Different Porosities. Mater. Sci. Eng. A 2020, 790, 139695. [Google Scholar] [CrossRef]
- Chen, J.K.; Wu, M.W.; Cheng, T.L.; Chiang, P.H. Continuous Compression Behaviors of Selective Laser Melting Ti-6Al-4V Alloy with Cuboctahedron Cellular Structures. Mater. Sci. Eng. C 2019, 100, 781–788. [Google Scholar] [CrossRef] [PubMed]
- Hedayati, R.; Sadighi, M.; Mohammadi-Aghdam, M.; Zadpoor, A.A. Mechanical Properties of Regular Porous Biomaterials Made from Truncated Cube Repeating Unit Cells: Analytical Solutions and Computational Models. Mater. Sci. Eng. C 2016, 60, 163–183. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, S.M.; Yavari, S.A.; Wauthle, R.; Pouran, B.; Schrooten, J.; Weinans, H.; Zadpoor, A.A. Additively Manufactured Open-Cell Porous Biomaterials Made from Six Different Space-Filling Unit Cells: The Mechanical and Morphological Properties. Materials 2015, 8, 1871–1896. [Google Scholar] [CrossRef] [Green Version]
- Guerra Silva, R.; Salinas Estay, C.; Morales Pavez, G.; Torres, M.J.; Zahr Viñuela, J. Assessment of Analytical Relationships for Mechanical Properties of Truncated Octahedron and Diamond Lattice Structures. Mater. Today Commun. 2021, 29, 102756. [Google Scholar] [CrossRef]
- Qi, D.; Yu, H.; Liu, M.; Huang, H.; Xu, S.; Xia, Y.; Qian, G.; Wu, W. Mechanical Behaviors of SLM Additive Manufactured Octet-Truss and Truncated-Octahedron Lattice Structures with Uniform and Taper Beams. Int. J. Mech. Sci. 2019, 163, 105091. [Google Scholar] [CrossRef] [Green Version]
- Hedayati, R.; Sadighi, M.; Mohammadi-Aghdam, M.; Zadpoor, A.A. Mechanics of Additively Manufactured Porous Biomaterials Based on the Rhombicuboctahedron Unit Cell. J. Mech. Behav. Biomed. Mater. 2016, 53, 272–294. [Google Scholar] [CrossRef] [PubMed]
- Hedayati, R.; Sadighi, M.; Mohammadi-Aghdam, M.; Zadpoor, A.A. Mechanical Behavior of Additively Manufactured Porous Biomaterials Made from Truncated Cuboctahedron Unit Cells. Int. J. Mech. Sci. 2016, 106, 19–38. [Google Scholar] [CrossRef]
- Xiao, L.; Song, W. Additively-Manufactured Functionally Graded Ti-6Al-4V Lattice Structures with High Strength under Static and Dynamic Loading: Experiments. Int. J. Impact. Eng. 2018, 111, 255–272. [Google Scholar] [CrossRef]
- Ma, S.; Song, K.; Lan, J.; Ma, L. Biological and Mechanical Property Analysis for Designed Heterogeneous Porous Scaffolds Based on the Refined TPMS. J. Mech. Behav. Biomed. Mater. 2020, 107, 103727. [Google Scholar] [CrossRef]
- Michielsen, K.; Kole, S. Photonic Band Gaps in Materials with Triply Periodic Surfaces and Related Tubular Structures. Phys. Rev. B 2003, 68, 115107. [Google Scholar] [CrossRef] [Green Version]
- Khaleghi, S.; Dehnavi, F.N.; Baghani, M.; Safdari, M.; Wang, K.; Baniassadi, M. On the Directional Elastic Modulus of the TPMS Structures and a Novel Hybridization Method to Control Anisotropy. Mater. Des. 2021, 210, 110074. [Google Scholar] [CrossRef]
- Yang, E.; Leary, M.; Lozanovski, B.; Downing, D.; Mazur, M.; Sarker, A.; Khorasani, A.M.; Jones, A.; Maconachie, T.; Bateman, S.; et al. Effect of Geometry on the Mechanical Properties of Ti-6Al-4V Gyroid Structures Fabricated via SLM: A Numerical Study. Mater. Des. 2019, 184, 108165. [Google Scholar] [CrossRef]
- Ataee, A.; Li, Y.; Fraser, D.; Song, G.; Wen, C. Anisotropic Ti-6Al-4V Gyroid Scaffolds Manufactured by Electron Beam Melting (EBM) for Bone Implant Applications. Mater. Des. 2018, 137, 345–354. [Google Scholar] [CrossRef]
- Maszybrocka, J.; Gapiński, B.; Dworak, M.; Skrabalak, G.; Stwora, A. The Manufacturability and Compression Properties of the Schwarz Diamond Type Ti6Al4V Cellular Lattice Fabricated by Selective Laser Melting. Int. J. Adv. Manuf. Technol. 2019, 105, 3411–3425. [Google Scholar] [CrossRef] [Green Version]
- Kadkhodapour, J.; Montazerian, H.; Darabi, A.C.; Zargarian, A.; Schmauder, S. The Relationships between Deformation Mechanisms and Mechanical Properties of Additively Manufactured Porous Biomaterials. J. Mech. Behav. Biomed. Mater. 2017, 70, 28–42. [Google Scholar] [CrossRef]
- Li, Z.; Chen, Z.; Chen, X.; Zhao, R. Effect of Unit Configurations and Parameters on the Properties of Ti–6Al–4V Unit-Stacked Scaffolds: A Trade-off between Mechanical and Permeable Performance. J. Mech. Behav. Biomed. Mater. 2021, 116, 104332. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Ding, J.; Li, X.; Qu, S.; Song, X.; Fuh, J.Y.H.; Lu, W.F.; Zhai, W. Enhancement in the Mechanical Behaviour of a Schwarz Primitive Periodic Minimal Surface Lattice Structure Design. Int. J. Mech. Sci. 2022, 216, 106977. [Google Scholar] [CrossRef]
- Lee, D.W.; Khan, K.A.; Abu Al-Rub, R.K. Stiffness and Yield Strength of Architectured Foams Based on the Schwarz Primitive Triply Periodic Minimal Surface. Int. J. Plast. 2017, 95, 1–20. [Google Scholar] [CrossRef]
- Gao, T.; Liu, K.; Wang, X.; Li, Z.; Wang, Z. Elastic Mechanical Property Hybridization of Configuration-Varying TPMS with Geometric Continuity. Mater. Des. 2022, 221, 110995. [Google Scholar] [CrossRef]
- Khan, K.A.; Abu Al-Rub, R.K. Time Dependent Response of Architectured Neovius Foams. Int. J. Mech. Sci. 2017, 126, 106–119. [Google Scholar] [CrossRef]
- Dalaq, A.S.; Abueidda, D.W.; Abu Al-Rub, R.K.; Jasiuk, I.M. Finite Element Prediction of Effective Elastic Properties of Interpenetrating Phase Composites with Architectured 3D Sheet Reinforcements. Int. J. Solids Struct. 2016, 83, 169–182. [Google Scholar] [CrossRef]
- Dong, G.; Zhao, Y.F. Numerical and Experimental Investigation of the Joint Stiffness in Lattice Structures Fabricated by Additive Manufacturing. Int. J. Mech. Sci. 2018, 148, 475–485. [Google Scholar] [CrossRef]
- Abate, K.M.; Nazir, A.; Yeh, Y.P.; Chen, J.E.; Jeng, J.Y. Design, Optimization, and Validation of Mechanical Properties of Different Cellular Structures for Biomedical Application. Int. J. Adv. Manuf. Technol. 2020, 106, 1253–1265. [Google Scholar] [CrossRef]
- Abate, K.M.; Nazir, A.; Chen, J.E.; Jeng, J.Y. Design, Optimization, and Evaluation of Additively Manufactured Vintiles Cellular Structure for Acetabular Cup Implant. Processes 2020, 8, 25. [Google Scholar] [CrossRef] [Green Version]
- Alomar, Z.; Concli, F. Compressive Behavior Assessment of a Newly Developed Circular Cell-Based Lattice Structure. Mater. Des. 2021, 205, 109716. [Google Scholar] [CrossRef]
- Distefano, F.; Mineo, R.; Epasto, G. Mechanical Behaviour of a Novel Biomimetic Lattice Structure for Bone Scaffold. J. Mech. Behav. Biomed. Mater. 2023, 138, 105656. [Google Scholar] [CrossRef]
- Parisien, A.; ElSayed, M.S.A.; Frei, H. Mechanoregulation Modelling of Stretching versus Bending Dominated Periodic Cellular Solids. Mater. Today Commun. 2022, 33, 104315. [Google Scholar] [CrossRef]
- Ghouse, S.; Babu, S.; van Arkel, R.J.; Nai, K.; Hooper, P.A.; Jeffers, J.R.T. The Influence of Laser Parameters and Scanning Strategies on the Mechanical Properties of a Stochastic Porous Material. Mater. Des. 2017, 131, 498–508. [Google Scholar] [CrossRef]
- Gao, W.; Zhang, Y.; Ramanujan, D.; Ramani, K.; Chen, Y.; Williams, C.B.; Wang, C.C.L.; Shin, Y.C.; Zhang, S.; Zavattieri, P.D. The Status, Challenges, and Future of Additive Manufacturing in Engineering. CAD Comput. Aided Des. 2015, 69, 65–89. [Google Scholar] [CrossRef]
- Lin, K.; Yuan, L.; Gu, D. Influence of Laser Parameters and Complex Structural Features on the Bio-Inspired Complex Thin-Wall Structures Fabricated by Selective Laser Melting. J. Mater. Process. Technol. 2019, 267, 34–43. [Google Scholar] [CrossRef]
- Sachs, E.M. Powder Dispensing Apparatus Using Vibration. U.S. Patent No. 6,036,777, 14 May 2000. Washington, DC: U.S. Patent and Trademark Office. [Google Scholar]
- Zhang, L.; Zhang, S.; Zhu, H.; Hu, Z.; Wang, G.; Zeng, X. Horizontal Dimensional Accuracy Prediction of Selective Laser Melting. Mater. Des. 2018, 160, 9–20. [Google Scholar] [CrossRef]
- Nawada, S.; Dimartino, S.; Fee, C. Dispersion Behavior of 3D-Printed Columns with Homogeneous Microstructures Comprising Differing Element Shapes. Chem. Eng. Sci. 2017, 164, 90–98. [Google Scholar] [CrossRef]
- Abdulhameed, O.; Al-Ahmari, A.; Ameen, W.; Mian, S.H. Additive Manufacturing: Challenges, Trends, and Applications. Adv. Mech. Eng. 2019, 11. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Xu, S.; Zhou, S.; Xu, W.; Leary, M.; Choong, P.; Qian, M.; Brandt, M.; Xie, Y.M. Topological Design and Additive Manufacturing of Porous Metals for Bone Scaffolds and Orthopaedic Implants: A Review. Biomaterials 2016, 83, 127–141. [Google Scholar] [CrossRef]
- Abbasi, N.; Hamlet, S.; Love, R.M.; Nguyen, N.T. Porous Scaffolds for Bone Regeneration. J. Sci. Adv. Mater. Devices 2020, 5, 1–9. [Google Scholar] [CrossRef]
- Bose, S.; Vahabzadeh, S.; Bandyopadhyay, A. Bone Tissue Engineering Using 3D Printing. Mater. Today 2013, 16, 496–504. [Google Scholar] [CrossRef]
- Mayfield, C.K.; Ayad, M.; Lechtholz-Zey, E.; Chen, Y.; Lieberman, J.R. 3D-Printing for Critical Sized Bone Defects: Current Concepts and Future Directions. Bioengineering 2022, 9, 680. [Google Scholar] [CrossRef]
- Abdulmaged, A.I.; Soon, C.F.; Talip, B.A.; Zamhuri, S.A.A.; Mostafa, S.A.; Zhou, W. Characterization of Alginate–Gelatin–Cholesteryl Ester Liquid Crystals Bioinks for Extrusion Bioprinting of Tissue Engineering Scaffolds. Polymers 2022, 14, 1021. [Google Scholar] [CrossRef] [PubMed]
- Harrysson, O.L.A.; Cansizoglu, O.; Marcellin-Little, D.J.; Cormier, D.R.; West, H.A. Direct Metal Fabrication of Titanium Implants with Tailored Materials and Mechanical Properties Using Electron Beam Melting Technology. Mater. Sci. Eng. C 2008, 28, 366–373. [Google Scholar] [CrossRef]
- Kolken, H.M.A.; de Jonge, C.P.; van der Sloten, T.; Garcia, A.F.; Pouran, B.; Willemsen, K.; Weinans, H.; Zadpoor, A.A. Additively Manufactured Space-Filling Meta-Implants. Acta Biomater. 2021, 125, 345–357. [Google Scholar] [CrossRef] [PubMed]
- Liverani, E.; Rogati, G.; Pagani, S.; Brogini, S.; Fortunato, A.; Caravaggi, P. Mechanical Interaction between Additive-Manufactured Metal Lattice Structures and Bone in Compression: Implications for Stress Shielding of Orthopaedic Implants. J. Mech. Behav. Biomed. Mater. 2021, 121, 104608. [Google Scholar] [CrossRef] [PubMed]
- Pei, X.; Wu, L.; Lei, H.; Zhou, C.; Fan, H.; Li, Z.; Zhang, B.; Sun, H.; Gui, X.; Jiang, Q.; et al. Fabrication of Customized Ti6AI4V Heterogeneous Scaffolds with Selective Laser Melting: Optimization of the Architecture for Orthopedic Implant Applications. Acta Biomater. 2021, 126, 485–495. [Google Scholar] [CrossRef]
- Epasto, G.; Distefano, F.; Mineo, R.; Guglielmino, E. Subject-Specific Finite Element Analysis of a Lumbar Cage Produced by Electron Beam Melting. Med. Biol. Eng. Comput. 2019, 57, 2771–2781. [Google Scholar] [CrossRef] [PubMed]
- Günther, F.; Wagner, M.; Pilz, S.; Gebert, A.; Zimmermann, M. Design Procedure for Triply Periodic Minimal Surface Based Biomimetic Scaffolds. J. Mech. Behav. Biomed. Mater. 2022, 126, 104871. [Google Scholar] [CrossRef]
- Cucinotta, F.; Mineo, R.; Raffaele, M.; Salmeri, F.; Sfravara, F. Customized Implant of Cervical Prostheses Exploiting a Predictive Analysis of Range of Motion. Comput. Aided Des. Appl. 2023, 20, 122–133. [Google Scholar] [CrossRef]
- Distefano, F.; Epasto, G.; Guglielmino, E.; Amata, A.; Mineo, R. Subsidence of a Partially Porous Titanium Lumbar Cage Produced by Electron Beam Melting Technology. J. Biomed. Mater. Res. B Appl. Biomater. 2023, 111, 590–598. [Google Scholar] [CrossRef]
- Li, Y.; Yang, C.; Zhao, H.; Qu, S.; Li, X.; Li, Y. New Developments of Ti-Based Alloys for Biomedical Applications. Materials 2014, 7, 1709–1800. [Google Scholar] [CrossRef] [Green Version]
- Che, Z.; Sun, Y.; Luo, W.; Zhu, L.; Li, Y.; Zhu, C.; Liu, T.; Huang, L. Bifunctionalized Hydrogels Promote Angiogenesis and Osseointegration at the Interface of Three-Dimensionally Printed Porous Titanium Scaffolds. Mater. Des. 2022, 223, 111118. [Google Scholar] [CrossRef]
- Zhao, H.; Shen, S.; Zhao, L.; Xu, Y.; Li, Y.; Zhuo, N. 3D Printing of Dual-Cell Delivery Titanium Alloy Scaffolds for Improving Osseointegration through Enhancing Angiogenesis and Osteogenesis. BMC Musculoskelet. Disord. 2021, 22, 734. [Google Scholar] [CrossRef]
- Gao, P.; Fan, B.; Yu, X.; Liu, W.; Wu, J.; Shi, L.; Yang, D.; Tan, L.; Wan, P.; Hao, Y.; et al. Biofunctional Magnesium Coated Ti6Al4V Scaffold Enhances Osteogenesis and Angiogenesis in Vitro and in Vivo for Orthopedic Application. Bioact. Mater. 2020, 5, 680–693. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Lu, Y.; Li, S.; Guo, S.; He, M.; Luo, K.; Lin, J. Copper-Modified Ti6Al4V Alloy Fabricated by Selective Laser Melting with pro-Angiogenic and Anti-Inflammatory Properties for Potential Guided Bone Regeneration Applications. Mater. Sci. Eng. C 2018, 90, 198–210. [Google Scholar] [CrossRef] [PubMed]
- Lv, J.; Xiu, P.; Tan, J.; Jia, Z.; Cai, H.; Liu, Z. Enhanced Angiogenesis and Osteogenesis in Critical Bone Defects by the Controlled Release of BMP-2 and VEGF: Implantation of Electron Beam Melting-Fabricated Porous Ti6Al4V Scaffolds Incorporating Growth Factor-Doped Fibrin Glue. Biomed. Mater. 2015, 10, 035013. [Google Scholar] [CrossRef] [PubMed]
- Efraim, Y.; Schoen, B.; Zahran, S.; Davidov, T.; Vasilyev, G.; Baruch, L.; Zussman, E.; Machluf, M. 3D Structure and Processing Methods Direct the Biological Attributes of ECM-Based Cardiac Scaffolds. Sci. Rep. 2019, 9, 5578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Bael, S.; Chai, Y.C.; Truscello, S.; Moesen, M.; Kerckhofs, G.; van Oosterwyck, H.; Kruth, J.P.; Schrooten, J. The Effect of Pore Geometry on the in Vitro Biological Behavior of Human Periosteum-Derived Cells Seeded on Selective Laser-Melted Ti6Al4V Bone Scaffolds. Acta Biomater. 2012, 8, 2824–2834. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.; Humayun, A.; Cohen, D.J.; Boyan, B.D.; Schwartz, Z. Additively Manufactured 3D Porous Ti-6Al-4V Constructs Mimic Trabecular Bone Structure and Regulate Osteoblast Proliferation, Differentiation and Local Factor Production in a Porosity and Surface Roughness Dependent Manner. Biofabrication 2014, 6, 045007. [Google Scholar] [CrossRef] [PubMed]
- Prananingrum, W.; Naito, Y.; Galli, S.; Bae, J.; Sekine, K.; Hamada, K.; Tomotake, Y.; Wennerberg, A.; Jimbo, R.; Ichikawa, T. Bone Ingrowth of Various Porous Titanium Scaffolds Produced by a Moldless and Space Holder Technique: An in Vivo Study in Rabbits. Biomed. Mater. 2016, 11, 015012. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Wang, L.; Pan, W.; Yang, F.; Jiang, W.; Wu, X.; Kong, X.; Dai, K.; Hao, Y. In Vitro and In Vivo Study of Additive Manufactured Porous Ti6Al4V Scaffolds for Repairing Bone Defects. Sci. Rep. 2016, 6, 34072. [Google Scholar] [CrossRef] [Green Version]
- Taniguchi, N.; Fujibayashi, S.; Takemoto, M.; Sasaki, K.; Otsuki, B.; Nakamura, T.; Matsushita, T.; Kokubo, T.; Matsuda, S. Effect of Pore Size on Bone Ingrowth into Porous Titanium Implants Fabricated by Additive Manufacturing: An in Vivo Experiment. Mater. Sci. Eng. C 2016, 59, 690–701. [Google Scholar] [CrossRef] [Green Version]
- Kapat, K.; Srivas, P.K.; Rameshbabu, A.P.; Maity, P.P.; Jana, S.; Dutta, J.; Majumdar, P.; Chakrabarti, D.; Dhara, S. Influence of Porosity and Pore-Size Distribution in Ti6Al4 v Foam on Physicomechanical Properties, Osteogenesis, and Quantitative Validation of Bone Ingrowth by Micro-Computed Tomography. ACS Appl. Mater. Interfaces 2017, 9, 39235–39248. [Google Scholar] [CrossRef]
- Ran, Q.; Yang, W.; Hu, Y.; Shen, X.; Yu, Y.; Xiang, Y.; Cai, K. Osteogenesis of 3D Printed Porous Ti6Al4V Implants with Different Pore Sizes. J. Mech. Behav. Biomed. Mater. 2018, 84, 1–11. [Google Scholar] [CrossRef]
- Luan, H.Q.; Wang, L.T.; Ren, W.Y.; Chu, Z.W.; Huang, Y.F.; Lu, C.L.; Fan, Y.B. The Effect of Pore Size and Porosity of Ti6Al4V Scaffolds on MC3T3-E1 Cells and Tissue in Rabbits. Sci. China Technol. Sci. 2019, 62, 1160–1168. [Google Scholar] [CrossRef]
- Ouyang, P.; Dong, H.; He, X.; Cai, X.; Wang, Y.; Li, J.; Li, H.; Jin, Z. Hydromechanical Mechanism behind the Effect of Pore Size of Porous Titanium Scaffolds on Osteoblast Response and Bone Ingrowth. Mater. Des. 2019, 183, 108151. [Google Scholar] [CrossRef]
- Chen, Z.; Yan, X.; Yin, S.; Liu, L.; Liu, X.; Zhao, G.; Ma, W.; Qi, W.; Ren, Z.; Liao, H.; et al. Influence of the Pore Size and Porosity of Selective Laser Melted Ti6Al4V ELI Porous Scaffold on Cell Proliferation, Osteogenesis and Bone Ingrowth. Mater. Sci. Eng. C 2020, 106, 110289. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Xu, D.; Lin, L.; Li, S.; Hou, W.; He, Y.; Sheng, L.; Yi, C.; Zhang, X.; Li, H.; et al. Large-Pore-Size Ti6Al4V Scaffolds with Different Pore Structures for Vascularized Bone Regeneration. Mater. Sci. Eng. C 2021, 131, 112499. [Google Scholar] [CrossRef] [PubMed]
- Sidambe, A.T. Biocompatibility of Advanced Manufactured Titanium Implants-A Review. Materials 2014, 7, 8168–8188. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Z.; Jones, D.; Yue, S.; Lee, P.D.; Jones, J.R.; Sutcliffe, C.J.; Jones, E. Hierarchical Tailoring of Strut Architecture to Control Permeability of Additive Manufactured Titanium Implants. Mater. Sci. Eng. C 2013, 33, 4055–4062. [Google Scholar] [CrossRef]
- Chen, C.; Hao, Y.; Bai, X.; Ni, J.; Chung, S.M.; Liu, F.; Lee, I.S. 3D Printed Porous Ti6Al4V Cage: Effects of Additive Angle on Surface Properties and Biocompatibility; Bone Ingrowth in Beagle Tibia Model. Mater. Des. 2019, 175, 107824. [Google Scholar] [CrossRef]
- Li, Z.; Liu, C.; Wang, B.; Wang, C.; Wang, Z.; Yang, F.; Gao, C.; Liu, H.; Qin, Y.; Wang, J. Heat Treatment Effect on the Mechanical Properties, Roughness and Bone Ingrowth Capacity of 3D Printing Porous Titanium Alloy. RSC Adv. 2018, 8, 12471–12483. [Google Scholar] [CrossRef] [Green Version]
- Beese, A.M.; Carroll, B.E. Review of Mechanical Properties of Ti-6Al-4V Made by Laser-Based Additive Manufacturing Using Powder Feedstock. JOM 2016, 68, 724–734. [Google Scholar] [CrossRef]
- Epasto, G.; Palomba, G.; D’Andrea, D.; Guglielmino, E.; di Bella, S.; Traina, F. Ti-6Al-4V ELI Microlattice Structures Manufactured by Electron Beam Melting: Effect of Unit Cell Dimensions and Morphology on Mechanical Behaviour. Mater. Sci. Eng. A 2019, 753, 31–41. [Google Scholar] [CrossRef]
- Osterhoff, G.; Morgan, E.F.; Shefelbine, S.J.; Karim, L.; Mcnamara, L.M.; Augat, P. Bone Mechanical Properties and Changes with Osteoporosis. Injury 2016, 47 (Suppl. 2), S11–S20. [Google Scholar] [CrossRef] [Green Version]
- Sharir, A.; Barak, M.M.; Shahar, R. Whole Bone Mechanics and Mechanical Testing. Vet. J. 2008, 177, 8–17. [Google Scholar] [CrossRef]
- Mirzaali, M.J.; Schwiedrzik, J.J.; Thaiwichai, S.; Best, J.P.; Michler, J.; Zysset, P.K.; Wolfram, U. Mechanical Properties of Cortical Bone and Their Relationships with Age, Gender, Composition and Microindentation Properties in the Elderly. Bone 2016, 93, 196–211. [Google Scholar] [CrossRef]
- Hansen, U.; Zioupos, P.; Simpson, R.; Currey, J.D.; Hynd, D. The Effect of Strain Rate on the Mechanical Properties of Human Cortical Bone. J. Biomech. Eng. 2008, 130, 011011. [Google Scholar] [CrossRef]
- Currey, J.D. Bones: Structure and Mechanics; Princetion University Press: Princeton, NJ, USA, 2006. [Google Scholar]
- Keaveny, T.M.; Morgan, E.F.; Niebur, G.L.; Yeh, O.C. Biomechanics of Trabecular Bone. Annu. Rev. Biomed. Eng. 2001, 3, 307–333. [Google Scholar] [CrossRef] [Green Version]
- Homminga, J.; Mccreadie, B.R.; Ciarelli, T.E.; Weinans, H.; Goldstein, S.A.; Huiskes, R. Cancellous Bone Mechanical Properties From Normals and Patients With Hip Fractures Differ on the Structure Level, Not on the Bone Hard Tissue Level. Bone 2002, 30, 759–764. [Google Scholar] [CrossRef]
- Nune, K.C.; Misra, R.D.K.; Li, S.J.; Hao, Y.L.; Zhang, W. The Functional Response of Bioactive Titania-Modified Three-Dimensional Ti-6Al-4V Mesh Structure toward Providing a Favorable Pathway for Intercellular Communication and Osteoincorporation. J. Biomed. Mater. Res. A 2016, 104, 2488–2501. [Google Scholar] [CrossRef]
- Sing, S.L.; Yeong, W.Y.; Wiria, F.E. Selective Laser Melting of Titanium Alloy with 50 Wt% Tantalum: Microstructure and Mechanical Properties. J. Alloys Compd. 2016, 660, 461–470. [Google Scholar] [CrossRef]
- Hollister, S.J. Scaffold Design and Manufacturing: From Concept to Clinic. Adv. Mater. 2009, 21, 3330–3342. [Google Scholar] [CrossRef] [PubMed]
- Ghouse, S.; Reznikov, N.; Boughton, O.R.; Babu, S.; Ng, K.C.G.; Blunn, G.; Cobb, J.P.; Stevens, M.M.; Jeffers, J.R.T. The Design and in Vivo Testing of a Locally Stiffness-Matched Porous Scaffold. Appl. Mater. Today 2019, 15, 377–388. [Google Scholar] [CrossRef] [PubMed]
- Wieding, J.; Lindner, T.; Bergschmidt, P.; Bader, R. Biomechanical Stability of Novel Mechanically Adapted Open-Porous Titanium Scaffolds in Metatarsal Bone Defects of Sheep. Biomaterials 2015, 46, 35–47. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Wang, Q.; Cai, D.; Gu, W.; Ma, Y.; Sun, Y.; Wei, Y.; Yuan, F. A Lattice Topology Optimization of Cervical Interbody Fusion Cage and Finite Element Comparison with ZK60 and Ti-6Al-4V Cages. BMC Musculoskelet. Disord. 2021, 22, 390. [Google Scholar] [CrossRef] [PubMed]
- Ashby, M.F. The Properties of Foams and Lattices. Philos. Trans. R. Soc. A Math. Phys. Eng. Sci. 2006, 364, 15–30. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, V.S.; Ashby, M.F.; Fleck, N.A. Foam Topology Bending versus Stretching Dominated Architectures. Acta Mater. 2001, 49, 1035–1040. [Google Scholar] [CrossRef]
- Wang, N.; Meenashisundaram, G.K.; Kandilya, D.; Fuh, J.Y.H.; Dheen, S.T.; Kumar, A.S. A Biomechanical Evaluation on Cubic, Octet, and TPMS Gyroid Ti6Al4V Lattice Structures Fabricated by Selective Laser Melting and the Effects of Their Debris on Human Osteoblast-like Cells. Biomater. Adv. 2022, 137, 212829. [Google Scholar] [CrossRef]
- Crupi, V.; Kara, E.; Epasto, G.; Guglielmino, E.; Aykul, H. Static Behavior of Lattice Structures Produced via Direct Metal Laser Sintering Technology. Mater. Des. 2017, 135, 246–256. [Google Scholar] [CrossRef]
- Bai, L.; Xu, Y.; Chen, X.; Xin, L.; Zhang, J.; Li, K.; Sun, Y. Improved Mechanical Properties and Energy Absorption of Ti6Al4V Laser Powder Bed Fusion Lattice Structures Using Curving Lattice Struts. Mater. Des. 2021, 211, 110140. [Google Scholar] [CrossRef]
- Horn, T.J.; Harrysson, O.L.A.; Marcellin-Little, D.J.; West, H.A.; Lascelles, B.D.X.; Aman, R. Flexural Properties of Ti6Al4V Rhombic Dodecahedron Open Cellular Structures Fabricated with Electron Beam Melting. Addit. Manuf. 2014, 1, 2–11. [Google Scholar] [CrossRef]
- Sun, Q.; Sun, J.; Guo, K.; Wang, L. Compressive Mechanical Properties and Energy Absorption Characteristics of SLM Fabricated Ti6Al4V Triply Periodic Minimal Surface Cellular Structures. Mech. Mater. 2022, 166, 104241. [Google Scholar] [CrossRef]
- Sokollu, B.; Gulcan, O.; Konukseven, E.I. Mechanical Properties Comparison of Strut-Based and Triply Periodic Minimal Surface Lattice Structures Produced by Electron Beam Melting. Addit. Manuf. 2022, 60, 103199. [Google Scholar] [CrossRef]
- Naghavi, S.A.; Tamaddon, M.; Marghoub, A.; Wang, K.; Babamiri, B.B.; Hazeli, K.; Xu, W.; Lu, X.; Sun, C.; Wang, L.; et al. Mechanical Characterisation and Numerical Modelling of TPMS-Based Gyroid and Diamond Ti6Al4V Scaffolds for Bone Implants: An Integrated Approach for Translational Consideration. Bioengineering 2022, 9, 504. [Google Scholar] [CrossRef] [PubMed]
- Alabort, E.; Barba, D.; Reed, R.C. Design of Metallic Bone by Additive Manufacturing. Scr. Mater. 2019, 164, 110–114. [Google Scholar] [CrossRef]
- Polley, C.; Radlof, W.; Hauschulz, F.; Benz, C.; Sander, M.; Seitz, H. Morphological and Mechanical Characterisation of Three-Dimensional Gyroid Structures Fabricated by Electron Beam Melting for the Use as a Porous Biomaterial. J. Mech. Behav. Biomed. Mater. 2022, 125, 104882. [Google Scholar] [CrossRef]
- Ataee, A.; Li, Y.; Brandt, M.; Wen, C. Ultrahigh-Strength Titanium Gyroid Scaffolds Manufactured by Selective Laser Melting (SLM) for Bone Implant Applications. Acta Mater. 2018, 158, 354–368. [Google Scholar] [CrossRef]
- Gao, H.; Li, X.; Wang, C.; Ji, P.; Wang, C. Mechanobiologically Optimization of a 3D Titanium-Mesh Implant for Mandibular Large Defect: A Simulated Study. Mater. Sci. Eng. C 2019, 104, 109934. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Su, Y.; Yang, W.; Wu, K.; Du, R.; Zhong, Y. A Novel Design Method of Gradient Porous Structure for Stabilized and Lightweight Mandibular Prosthesis. Bioengineering 2022, 9, 424. [Google Scholar] [CrossRef]
- Bittredge, O.; Hassanin, H.; El-Sayed, M.A.; Eldessouky, H.M.; Alsaleh, N.A.; Alrasheedi, N.H.; Essa, K.; Ahmadein, M. Fabrication and Optimisation of Ti-6Al-4V Lattice-Structured Total Shoulder Implants Using Laser Additive Manufacturing. Materials 2022, 15, 3095. [Google Scholar] [CrossRef]
- Fogel, G.; Martin, N.; Lynch, K.; Pelletier, M.H.; Wills, D.; Wang, T.; Walsh, W.R.; Williams, G.M.; Malik, J.; Peng, Y.; et al. Subsidence and Fusion Performance of a 3D-Printed Porous Interbody Cage with Stress-Optimized Body Lattice and Microporous Endplates—A Comprehensive Mechanical and Biological Analysis. Spine J. 2022, 22, 1028–1037. [Google Scholar] [CrossRef]
- Cuzzocrea, F.; Ivone, A.; Jannelli, E.; Fioruzzi, A.; Ferranti, E.; Vanelli, R.; Benazzo, F. PEEK versus Metal Cages in Posterior Lumbar Interbody Fusion: A Clinical and Radiological Comparative Study. Musculoskelet. Surg. 2019, 103, 237–241. [Google Scholar] [CrossRef]
- Nemoto, O.; Asazuma, T.; Yato, Y.; Imabayashi, H.; Yasuoka, H.; Fujikawa, A. Comparison of Fusion Rates Following Transforaminal Lumbar Interbody Fusion Using Polyetheretherketone Cages or Titanium Cages with Transpedicular Instrumentation. Eur. Spine J. 2014, 23, 2150–2155. [Google Scholar] [CrossRef] [PubMed]
- Tanida, S.; Fujibayashi, S.; Otsuki, B.; Masamoto, K.; Takahashi, Y.; Nakayama, T.; Matsuda, S. Vertebral Endplate Cyst as a Predictor of Nonunion after Lumbar Interbody Fusion: Comparison of Titanium And Polyetheretherketone Cages. Spine 2016, 41, E1216–E1222. [Google Scholar] [CrossRef] [PubMed]
- Gok, M.G. Creation and Finite-Element Analysis of Multi-Lattice Structure Design in Hip Stem Implant to Reduce the Stress-Shielding Effect. Proc. Inst. Mech. Eng. Part L J. Mater. Des. Appl. 2022, 236, 429–439. [Google Scholar] [CrossRef]





















 | |
 | |
 | |
 | |
 | |
 |
| Research | Optimal Pore Size [μm] | Tested Pore Size Range [μm] |
|---|---|---|
| Van Bael et al. [87] | 1000 | 500–1000 |
| Cheng et al. [88] | 300 | 200–400 |
| Prananingrum et al. [89] | 100 | 60–600 |
| Li et al. [90] | 400 | 300–700 |
| Taniguchi et al. [91] | 632 | 300–900 |
| Kapat et al. [92] | 178 | 92–297 |
| Ran et al. [93] | 600 | 400–800 |
| Luan et al. [94] | 383 | 334–401 |
| Ouyang et al. [95] | 650 | 400–1100 |
| Chen et al. [96] | 500 | 500–700 |
| Wang et al. [97] | 1000 | 800–1000 |
| Unit Cell Topology | Cubic | BCC | Diamond | Octet-Truss | TC | RD | RCO | TCO |
|---|---|---|---|---|---|---|---|---|
| S | 12 | 8 | 9 | 36 | 36 | 24 | 48 | 72 |
| N | 8 | 9 | 7 | 14 | 24 | 14 | 24 | 48 |
| M | −6 | −13 | −6 | 0 | −30 | −12 | −18 | −66 |
| Unit Cell Topology | Elastic Modulus (GPa) | Compressive Strength (MPa) | ||
|---|---|---|---|---|
| C1 | n1 | C2 | n2 | |
| Cubic [35] | 0.11 | 0.92 | 1.15 | 1.75 |
| Cubic [119] | 0.55 | 2.82 | 1.34 | 1.85 |
| BCC [120] | 0.15 | 2 | 0.57 | 1.9 |
| BCC [121] | 0.15 | 2 | 0.23 | 1.5 |
| Diamond [118] | 0.17 | 1.68 | 0.56 | 1.58 |
| Octet-truss [119] | 0.51 | 2.33 | 1.37 | 1.37 |
| TC [118] | 0.32 | 1.5 | 1.49 | 1.9 |
| RD [118] | 0.42 | 2.34 | 1.29 | 2.27 |
| RD [122] | 1.08 | 1.9 | 0.6 | 1.31 |
| RCO [118] | 0.17 | 1.25 | 0.97 | 1.62 |
| TCO [118] | 0.14 | 1.18 | 0.99 | 1.78 |
| Kelvin [58] | 0.6 | 2.3 | 0.3 | 1.5 |
| TAOR [58] | 0.8 | 2.3 | 0.6 | 1.5 |
| Schwarz Primitive [123] | 0.09 | 1.15 | 0.34 | 1.25 |
| Schwarz Primitive [124] | 1.38 | 2 | 0.98 | 1.5 |
| Diamond Sheet [125] | 0.71 | 1.21 | 0.42 | 1.14 |
| Diamond Sheet [123] | 0.12 | 1.06 | 1.66 | 1.89 |
| Diamond Skeletal [15] | 0.17 | 1.64 | 1.39 | 1.95 |
| Diamond Skeletal [126] | 0.7 | 2.7 | 1.17 | 2.6 |
| Gyroid Sheet [127] | 0.2 | 1.2 | 0.67 | 1.3 |
| Gyroid Sheet [123] | 0.12 | 1.1 | 2.07 | 2.03 |
| Gyroid Skeletal [15] | 0.19 | 1.71 | 1.31 | 1.83 |
| Gyroid Skeletal [128] | 0.29 | 2 | 0.46 | 1.5 |
| Neovius [126] | 0.31 | 2.3 | 1.43 | 2.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Distefano, F.; Pasta, S.; Epasto, G. Titanium Lattice Structures Produced via Additive Manufacturing for a Bone Scaffold: A Review. J. Funct. Biomater. 2023, 14, 125. https://doi.org/10.3390/jfb14030125
Distefano F, Pasta S, Epasto G. Titanium Lattice Structures Produced via Additive Manufacturing for a Bone Scaffold: A Review. Journal of Functional Biomaterials. 2023; 14(3):125. https://doi.org/10.3390/jfb14030125
Chicago/Turabian StyleDistefano, Fabio, Salvatore Pasta, and Gabriella Epasto. 2023. "Titanium Lattice Structures Produced via Additive Manufacturing for a Bone Scaffold: A Review" Journal of Functional Biomaterials 14, no. 3: 125. https://doi.org/10.3390/jfb14030125







