Effect of Anti-COVID-19 Mouthwashes on Shear Bond Strength of Resin-Matrix Ceramics Repaired with Resin Composite Using Universal Adhesive: An In Vitro Study
Abstract
:1. Introduction
2. Materials and Methods
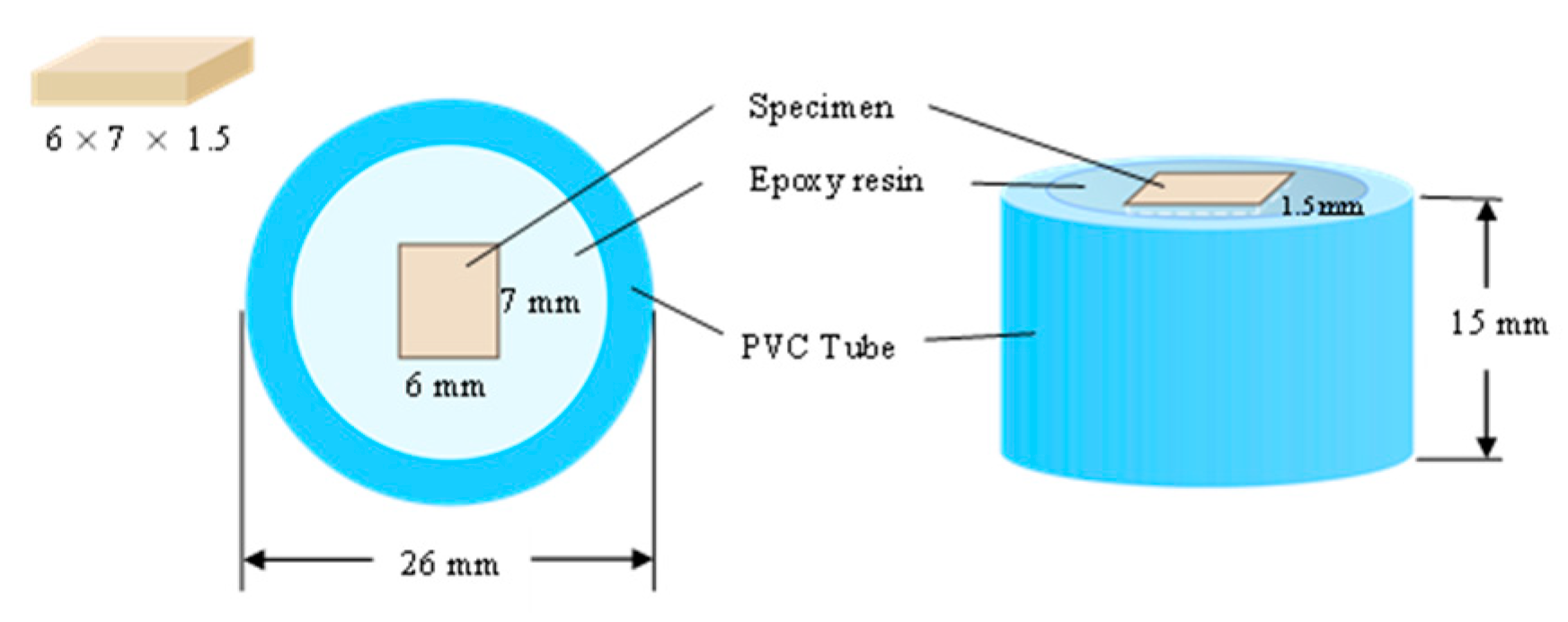
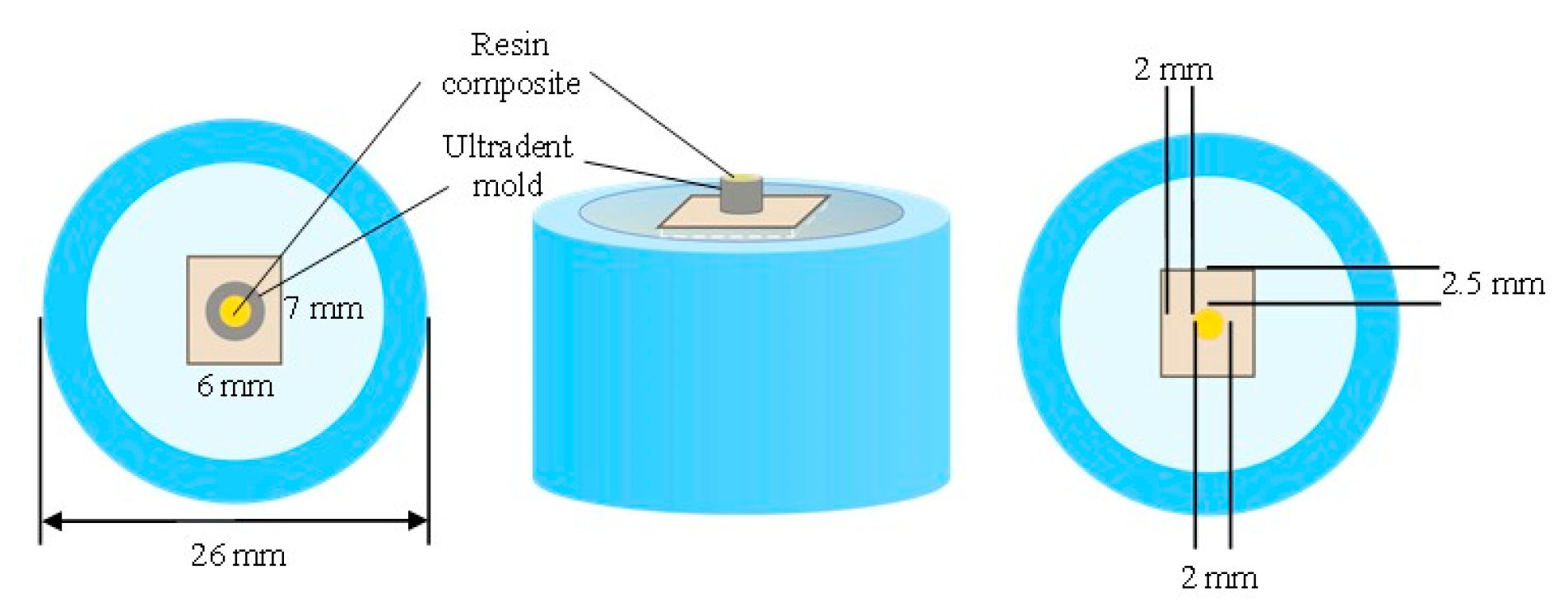
2.1. Specimen Preparation
2.2. Storing in Anti-COVID-19 Mouthwash
2.3. Surface Treatment and Repair Procedure
2.4. SBS Test
2.5. Mode of Failure Analysis
- (a)
- Adhesive failure: over 75% of the failure occurs at the interface between the resin-matrix hybrid material and the universal adhesive.
- (b)
- Cohesive failure: over 75% of the failure occurs within the universal adhesive or composite.
- (c)
- Mixed failure: 25–75% of the failure occurs as a combination of cohesive and adhesive failure.
2.6. Statistical Analysis
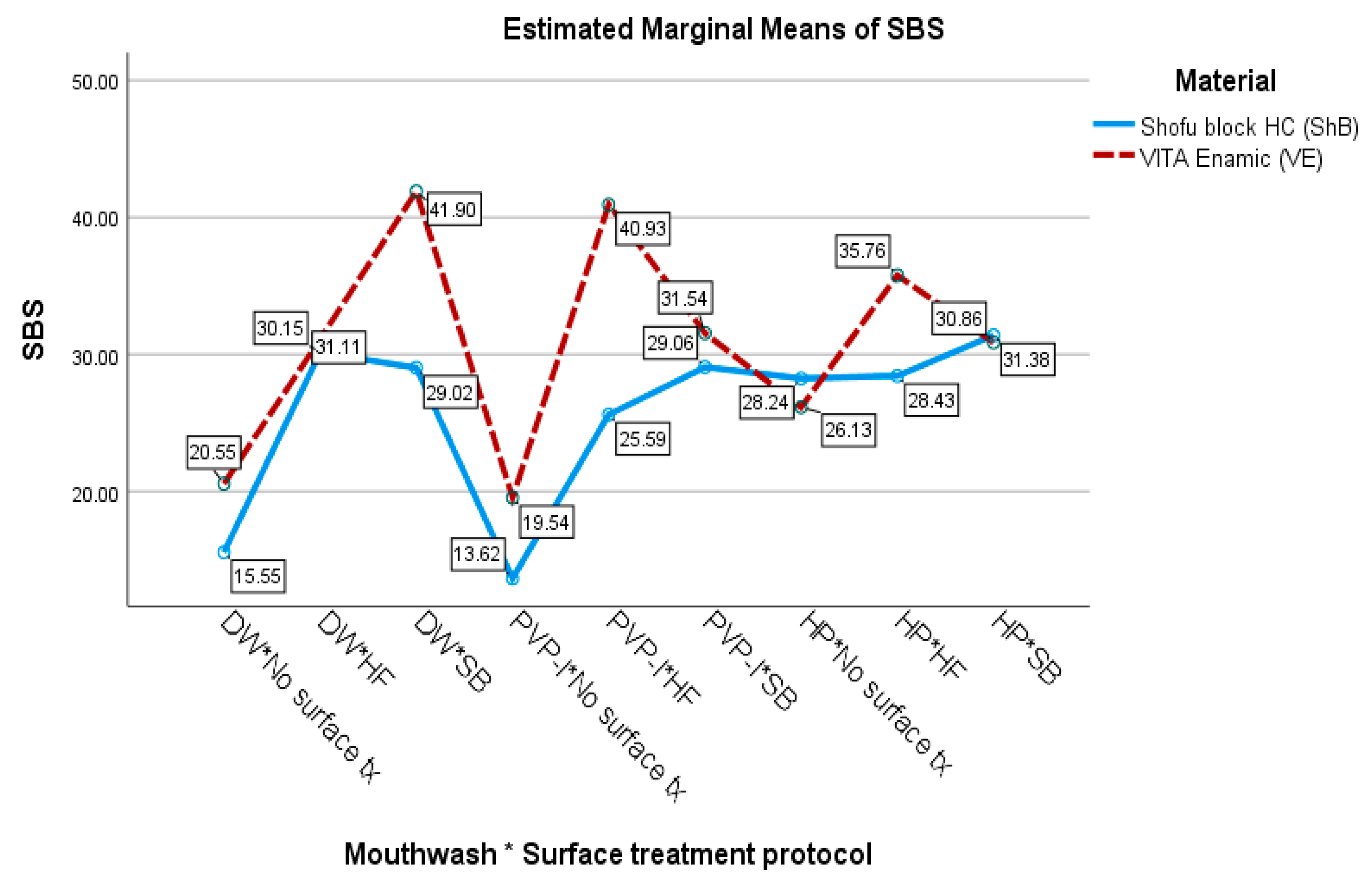
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yoon, J.G.; Yoon, J.; Song, J.Y.; Yoon, S.Y.; Lim, C.S.; Seong, H.; Noh, J.Y.; Cheong, H.J.; Kim, W.J. Clinical Significance of a High SARS-CoV-2 Viral Load in the Saliva. J. Korean Med. Sci. 2020, 35, e195. [Google Scholar] [CrossRef]
- To, K.K.; Tsang, O.T.; Yip, C.C.; Chan, K.H.; Wu, T.C.; Chan, J.M.; Leung, W.S.; Chik, T.S.; Choi, C.Y.; Kandamby, D.H.; et al. Consistent Detection of 2019 Novel Coronavirus in Saliva. Clin. Infect. Dis. 2020, 71, 841–843. [Google Scholar] [CrossRef] [Green Version]
- Harrel, S.K.; Molinari, J. Aerosols and splatter in dentistry: A brief review of the literature and infection control implications. J. Am. Dent. Assoc. 2004, 135, 429–437. [Google Scholar] [CrossRef]
- Peng, X.; Xu, X.; Li, Y.; Cheng, L.; Zhou, X.; Ren, B. Transmission routes of 2019-nCoV and controls in dental practice. Int. J. Oral Sci. 2020, 12, 9. [Google Scholar] [CrossRef] [Green Version]
- Carrouel, F.; Gonçalves, L.S.; Conte, M.P.; Campus, G.; Fisher, J.; Fraticelli, L.; Gadea-Deschamps, E.; Ottolenghi, L.; Bourgeois, D. Antiviral Activity of Reagents in Mouth Rinses against SARS-CoV-2. J. Dent. Res. 2021, 100, 124–132. [Google Scholar] [CrossRef]
- Atukorallaya, D.S.; Ratnayake, R.K. Oral Mucosa, Saliva, and COVID-19 Infection in Oral Health Care. Front. Med. 2021, 8, 656926. [Google Scholar] [CrossRef]
- Conrad, H.J.; Seong, W.J.; Pesun, I.J. Current ceramic materials and systems with clinical recommendations: A systematic review. J. Prosthet. Dent. 2007, 98, 389–404. [Google Scholar] [CrossRef] [PubMed]
- Ruse, N.D.; Sadoun, M.J. Resin-composite blocks for dental CAD/CAM applications. J. Dent. Res. 2014, 93, 1232–1234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coldea, A.; Swain, M.V.; Thiel, N. Mechanical properties of polymer-infiltrated-ceramic-network materials. Dent. Mater. 2013, 29, 419–426. [Google Scholar] [CrossRef]
- Hickel, R.; Brüshaver, K.; Ilie, N. Repair of restorations--criteria for decision making and clinical recommendations. Dent. Mater. 2013, 29, 28–50. [Google Scholar] [CrossRef] [PubMed]
- Filho, A.M.; Vieira, L.C.; Araújo, E.; Monteiro Júnior, S. Effect of different ceramic surface treatments on resin microtensile bond strength. J. Prosthodont. 2004, 13, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Blum, I.R.; Jagger, D.C.; Wilson, N.H. Defective dental restorations: To repair or not to repair? Part 2: All-ceramics and porcelain fused to metal systems. Dent. Update 2011, 38, 150–152, 154–156, 158. [Google Scholar] [CrossRef]
- Javidi, H.; Tickle, M.; Aggarwal, V.R. Repair vs. replacement of failed restorations in general dental practice: Factors influencing treatment choices and outcomes. Br. Dent. J. 2015, 218, E2. [Google Scholar] [CrossRef] [PubMed]
- de Silva, J.M.G.; Botta, A.C.; Barcellose, C.D.; Pagani, C.; Torres, C.R.G. Effect of antioxidant agents on bond strength of composite to bleached enamel with 38% hydrogen peroxide. Mater. Res. 2011, 14, 235–238. [Google Scholar] [CrossRef] [Green Version]
- Demir, A.; Malkoc, S.; Sengun, A.; Koyuturk, A.E.; Sener, Y. Effects of chlorhexidine and povidone-iodine mouth rinses on the bond strength of an orthodontic composite. Angle Orthod. 2005, 75, 392–396. [Google Scholar]
- Bayraktar, Y.; Karaduman, K.; Ayhan, B.; Karsiyaka Hendek, M. The effect of SARS-CoV-2 effective mouthwashes on the staining, translucency and surface roughness of a nanofill resin composite. Am. J. Dent. 2021, 34, 166–170. [Google Scholar] [PubMed]
- de Moraes Porto, I.C.; das Neves, L.E.; de Souza, C.K.; Parolia, A.; Barbosa dos Santos, N. A comparative effect of mouthwashes with different alcohol concentrations on surface hardness, sorption and solubility of composite resins. Oral Health Dent. Manag. 2014, 13, 502–506. [Google Scholar]
- Festuccia, M.S.; Garcia Lda, F.; Cruvinel, D.R.; Pires-De-Souza Fde, C. Color stability, surface roughness and microhardness of composites submitted to mouthrinsing action. J. Appl. Oral Sci. 2012, 20, 200–205. [Google Scholar] [CrossRef]
- Pelino, J.E.P.; Passero, A.; Martin, A.A.; Charles, C.A. In vitro effects of alcohol-containing mouthwashes on human enamel and restorative materials. Braz. Oral Res. 2018, 32, e25. [Google Scholar] [CrossRef] [Green Version]
- Kutuk, Z.B.; Oz, A.; Yazici, A.R. Influence of preprocedural antiseptic mouthrinses against COVID-19 on enamel/dentin bond strength of a universal adhesive. J. Adhes. Sci. Technol. 2021, 35, 2288–2300. [Google Scholar] [CrossRef]
- Özduman, Z.C.; Oglakci, B.; Doğan, M.; Deger, C.; Eliguzeloglu Dalkilic, E. How does antiseptic mouthwashes against SARS-COV-2 affect the bond strength of universal adhesive to enamel? Microsc. Res. Tech. 2022, 85, 1199–1208. [Google Scholar] [CrossRef] [PubMed]
- Elsaka, S.E. Repair bond strength of resin composite to a novel CAD/CAM hybrid ceramic using different repair systems. Dent. Mater. J. 2015, 34, 161–167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klaisiri, A.; Krajangta, N.; Thamrongananskul, N. The durability of zirconia/resin composite shear bond strength using different functional monomer of universal adhesives. Eur. J. Dent. 2022, 16, 756–760. [Google Scholar] [CrossRef]
- Fouquet, V.; Lachard, F.; Abdel-Gawad, S.; Dursun, E.; Attal, J.P.; François, P. Shear Bond Strength of a Direct Resin Composite to CAD-CAM Composite Blocks: Relative Contribution of Micromechanical and Chemical Block Surface Treatment. Materials 2022, 15, 5018. [Google Scholar] [CrossRef] [PubMed]
- Demirel, G.; Baltacıoğlu, İ.H. Influence of different universal adhesives on the repair performance of hybrid CAD-CAM materials. Restor. Dent. Endod. 2019, 44, e23. [Google Scholar] [CrossRef]
- Klaisiri, A.; Krajangta, N.; Phumpatrakom, P.; Sriamporn, T.; Thamrongananskul, N. The use of silane coupling agents on lithium disilicate glass ceramic repaired with resin composite. J. Int. Dent. Med. Res. 2021, 14, 169–172. [Google Scholar]
- Klaisiri, A.; Krajangta, N.; Peampring, C.; Sriamporn, T.; Thamrongananskul, N.; Neff, A.; Pitak-Arnnop, P. Shear bond strength of different functional monomer in universal adhesives at the resin composite/base metal alloys interface. J. Int. Dent. Med. Res. 2021, 14, 187–191. [Google Scholar]
- Baldi, A.; Carossa, M.; Comba, A.; Alovisi, M.; Femiano, F.; Pasqualini, D.; Berutti, E.; Scotti, N. Wear Behaviour of Polymer-Infiltrated Network Ceramics, Lithium Disilicate and Cubic Zirconia against Enamel in a Bruxism-Simulated Scenario. Biomedicines 2022, 10, 1682. [Google Scholar] [CrossRef]
- Arkoy, S.; Ulusoy, M. Effect of Different Surface Treatments on Repair Bond Strength of CAD/CAM Resin-Matrix Ceramics. Materials 2022, 15, 6314. [Google Scholar] [CrossRef]
- Sharif, M.O.; Catleugh, M.; Merry, A.; Tickle, M.; Dunne, S.M.; Brunton, P.; Aggarwal, V.R.; Chong, L.Y. Replacement versus repair of defective restorations in adults: Resin composite. Cochrane Database Syst. Rev. 2014, 2014, CD005971. [Google Scholar] [CrossRef]
- Yoo, J.Y.; Yoon, H.I.; Park, J.M.; Park, E.J. Porcelain repair—Influence of different systems and surface treatments on resin bond strength. J. Adv. Prosthodont. 2015, 7, 343–348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Erdemir, U.; Sancakli, H.S.; Sancakli, E.; Eren, M.M.; Ozel, S.; Yucel, T.; Yildiz, E. Shear bond strength of a new self-adhering flowable composite resin for lithium disilicate-reinforced CAD/CAM ceramic material. J. Adv. Prosthodont. 2014, 6, 434–443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tarib, N.A.; Anuar, N.; Ahmad, M. Shear bond strength of veneering ceramic to coping materials with different pre-surface treatments. J. Adv. Prosthodont. 2016, 8, 339–344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klaisiri, A.; Maneenacarith, A.; Jirathawornkul, N.; Suthamprajak, P.; Sriamporn, T.; Thamrongananskul, N. The effect of multiple applications of phosphate-containing primer on shear bond strength between zirconia and resin composite. Polymers 2022, 14, 4174. [Google Scholar] [CrossRef]
- Klaisiri, A.; Phumpatrakom, P.; Thamrongananskul, N. Chemical surface modification methods of resin composite repaired with resin-modified glass-ionomer cement. Eur. J. Dent 2022. ahead of print. [Google Scholar] [CrossRef]
- Leelaponglit, S.; Maneenacarith, A.; Wutikhun, T.; Klaisiri, A. The various silane agents in universal adhesives on repair strength of resin composite to resin composite. J. Compos. Sci. 2023, 7, 7. [Google Scholar] [CrossRef]
- Koenig, A.; Schmidtke, J.; Schmohl, L.; Schneider-Feyrer, S.; Rosentritt, M.; Hoelzig, H.; Kloess, G.; Vejjasilpa, K.; Schulz-Siegmund, M.; Fuchs, F.; et al. Characterisation of the Filler Fraction in CAD/CAM Resin-Based Composites. Materials 2021, 14, 1986. [Google Scholar] [CrossRef] [PubMed]
- Subaşı, M.G.; Alp, G. Repair bond strengths of non-aged and aged resin nanoceramics. J. Adv. Prosthodont. 2017, 9, 364–370. [Google Scholar] [CrossRef] [Green Version]
- Bidra, A.S.; Pelletier, J.S.; Westover, J.B.; Frank, S.; Brown, S.M.; Tessema, B. Comparison of In Vitro Inactivation of SARS CoV-2 with Hydrogen Peroxide and Povidone-Iodine Oral Antiseptic Rinses. J. Prosthodont. 2020, 29, 599–603. [Google Scholar] [CrossRef]
- Güngör, M.B.; Nemli, S.K.; Bal, B.T.; Ünver, S.; Doğan, A. Effect of surface treatments on shear bond strength of resin composite bonded to CAD/CAM resin-ceramic hybrid materials. J. Adv. Prosthodont. 2016, 8, 259–266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wiegand, A.; Stucki, L.; Hoffmann, R.; Attin, T.; Stawarczyk, B. Repairability of CAD/CAM high-density PMMA- and composite-based polymers. Clin. Oral Investig. 2015, 19, 2007–2013. [Google Scholar] [CrossRef]
- Mainjot, A.K.; Dupont, N.M.; Oudkerk, J.C.; Dewael, T.Y.; Sadoun, M.J. From Artisanal to CAD-CAM Blocks: State of the Art of Indirect Composites. J. Dent. Res. 2016, 95, 487–495. [Google Scholar] [CrossRef]
- Gracis, S.; Thompson, V.P.; Ferencz, J.L.; Silva, N.R.; Bonfante, E.A. A new classification system for all-ceramic and ceramic-like restorative materials. Int. J. Prosthodont. 2015, 28, 227–235. [Google Scholar] [CrossRef] [Green Version]
- Spitznagel, F.A.; Vuck, A.; Gierthmühlen, P.C.; Blatz, M.B.; Horvath, S.D. Adhesive Bonding to Hybrid Materials: An Overview of Materials and Recommendations. Compend Contin. Educ. Dent. 2016, 37, 630–637. [Google Scholar]
- Blatz, M.B.; Sadan, A.; Kern, M. Resin-ceramic bonding: A review of the literature. J. Prosthet. Dent. 2003, 89, 268–274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tanthanuch, S.; Kukiattrakoon, B.; Naiyanart, C.; Promtong, T.; Yothinwatthanabamrung, P.; Pumpua, S. Effect of Mouthwashes for COVID-19 Prevention on Surface Changes of Resin Composites. Int. Dent. J. 2022, 20. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- da Silva, N.R.; Calamia, C.S.; Coelho, G.; Carrilho, M.R.; de Carvalho, R.M.; Caufield, P.; Thompson, V.P. Effect of 2% iodine disinfecting solution on bond strength to dentin. J. Appl. Oral Sci. 2006, 14, 399–404. [Google Scholar] [CrossRef] [Green Version]
- El-Ashkar, A.S.; Nabil, O. Recent Developments and Potential Challenges in Dealing with Internal and External Surfaces of Glass Matrix and Resin Matrix Ceramic Materials. A Literature Review. Acta Sci. Dent. Sci. 2022, 6, 61–72. [Google Scholar] [CrossRef]



| Material Name | Compositions | Lot Number |
|---|---|---|
| VITA Enamic (VITA Zahnfabrik, Bad Sackingen, Germany) | TEGDMA, UDMA Filler: Feldspar ceramic enriched with aluminum oxide, 86% by weight (75% by vol.) [24,25] | 90001, 93140 |
| Shofu Block HC (Shofu Inc., Kyoto, Japan) | TEGDMA, UDMA Filler: Zirconium silicate, Silica powder, micro fumed silica, 80% by weight (61% by vol.) [24,25] | 0720695 |
| Scotchbond Universal Plus adhesive; 3M ESPE, St. Paul, MN, USA | 10-MDP, HEMA, vitrebond copolymer, filler, ethanol/water, initiators, silane, universal dual cure activator (separate vial), dimethacrylate resins containing BisGMA, APTES, and γ-MPTES | 8904597 |
| Filtek Z350 XT; 3M ESPE, St. Paul, MN, USA | TEGDMA, bis-GMA, bis-EMA, UDMA, silane treated silica, silane treated zirconia, sliane treated ceramic | NE81667 |
| Povidone–iodine (PVP-I) (BETADINE® Mouthwash/Gargle, Thai Meiji Pharmaceutical, Bangkok, Thailand) | Active ingredient: 7% W/V PVP-I Other ingredients: Glycerol, menthol, methyl salicylate, ethanol, saccharin sodium, and purified water | 213033 |
| Hydrogen peroxide (HP) (Siribuncha® Siribuncha corporation, Bangkok, Thailand) | 3% Hydrogen peroxide | 02310146 |
| Source | df | Mean Square | F | Sig. |
|---|---|---|---|---|
| material | 1 | 2606.627 | 50.609 | 0.000 |
| mouthwashes | 2 | 374.390 | 7.269 | 0.001 |
| surface treatment | 2 | 5596.447 | 108.658 | 0.000 |
| material * mouthwash | 2 | 342.264 | 6.645 | 0.001 |
| material * surface treatment | 2 | 194.589 | 3.778 | 0.024 |
| mouthwash * surface treatment | 4 | 703.749 | 13.664 | 0.000 |
| material * mouthwash * surface treatment | 4 | 462.774 | 8.985 | 0.000 |
| Type of Ceramic | Mouthwashes | Surface Treatment | Mean SBS ± SD | Percentage of Failure Mode | ||
|---|---|---|---|---|---|---|
| Adhesive | Mixed | Cohesive | ||||
| VITA ENAMIC | DW | No surface treatment | 20.55 (6.52) ABC | 71.43 | 14.29 | 14.29 |
| HF | 31.11 (8.94) DE | 0 | 14.29 | 85.71 | ||
| Sandblast | 41.90 (8.17) F | 4.76 | 23.81 | 71.43 | ||
| PVP-I | No surface treatment | 19.54 (5.49) AB | 100 | 0 | 0 | |
| HF | 40.93 (8.13) F | 14.29 | 4.76 | 80.95 | ||
| Sandblast | 31.54 (7.49) DE | 14.29 | 9.52 | 76.19 | ||
| HP | No surface treatment | 26.13 (8.20) BCD | 57.14 | 4.76 | 38.10 | |
| HF | 35.76 (7.00) EF | 0 | 19.05 | 80.95 | ||
| Sandblast | 30.86 (5.80) DE | 0 | 0 | 100 | ||
| Shofu Block HC | DW | No surface treatment | 15.55 (6.92) A | 85.71 | 0 | 14.29 |
| HF | 30.15 (9.45) DE | 33.33 | 0 | 66.67 | ||
| Sandblast | 29.02 (7.27) DE | 9.52 | 9.52 | 80.96 | ||
| PVP-I | No surface treatment | 13.62 (4.04) A | 100 | 0 | 0 | |
| HF | 25.59 (7.18) BCD | 4.76 | 23.81 | 71.43 | ||
| Sandblast | 29.06 (7.12) DE | 4.76 | 14.29 | 80.95 | ||
| HP | No surface treatment | 28.24 (7.53) CDE | 57.14 | 9.52 | 33.33 | |
| HF | 28.43 (5.14) DE | 19.05 | 23.81 | 57.14 | ||
| Sandblast | 31.38 (6.65) DE | 4.76 | 33.33 | 61.90 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Limsiriwong, W.; Klaisiri, A.; Krajangta, N. Effect of Anti-COVID-19 Mouthwashes on Shear Bond Strength of Resin-Matrix Ceramics Repaired with Resin Composite Using Universal Adhesive: An In Vitro Study. J. Funct. Biomater. 2023, 14, 158. https://doi.org/10.3390/jfb14030158
Limsiriwong W, Klaisiri A, Krajangta N. Effect of Anti-COVID-19 Mouthwashes on Shear Bond Strength of Resin-Matrix Ceramics Repaired with Resin Composite Using Universal Adhesive: An In Vitro Study. Journal of Functional Biomaterials. 2023; 14(3):158. https://doi.org/10.3390/jfb14030158
Chicago/Turabian StyleLimsiriwong, Wichuda, Awiruth Klaisiri, and Nantawan Krajangta. 2023. "Effect of Anti-COVID-19 Mouthwashes on Shear Bond Strength of Resin-Matrix Ceramics Repaired with Resin Composite Using Universal Adhesive: An In Vitro Study" Journal of Functional Biomaterials 14, no. 3: 158. https://doi.org/10.3390/jfb14030158
APA StyleLimsiriwong, W., Klaisiri, A., & Krajangta, N. (2023). Effect of Anti-COVID-19 Mouthwashes on Shear Bond Strength of Resin-Matrix Ceramics Repaired with Resin Composite Using Universal Adhesive: An In Vitro Study. Journal of Functional Biomaterials, 14(3), 158. https://doi.org/10.3390/jfb14030158








