Effects of Polishing and Artificial Aging on Mechanical Properties of Dental LT Clear® Resin
Abstract
:1. Introduction
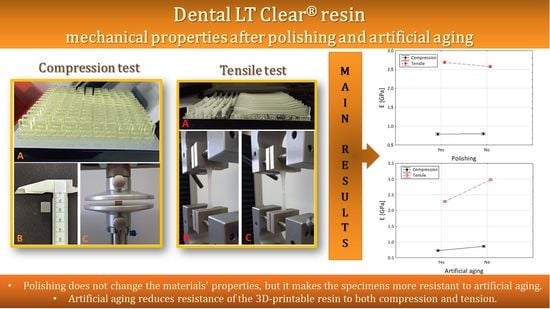
- There is no influence of polishing on the material’s durability.
- There is no influence of artificial aging on the material’s durability.
- There is no relation between application of polishing and artificial aging regarding the material’s durability.
- Polishing does not change the properties of the material in terms of artificial aging.
2. Materials and Methods
2.1. Materials
2.2. Specimens’ Preparation and Artificial Aging
2.3. Compression Test
2.4. Tensile Test
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Malysa, A.; Wezgowiec, J.; Danel, D.; Boening, K.; Walczak, K.; Wieckiewicz, M. Bond strength of modern self-adhesive resin cements to human dentin and different CAD/CAM ceramics. Acta Bioeng. Biomech. 2020, 22, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Karatas, O.; Gul, P.; Akgul, N.; Celik, N.; Gundogdu, M.; Duymus, Z.; Seven, N. Effect of staining and bleaching on the microhardness, surface roughness and color of different composite resins. Dent. Med. Probl. 2021, 58, 369–376. [Google Scholar] [CrossRef]
- Goracci, C.; Juloski, J.; D’Amico, C.; Balestra, D.; Volpe, A.; Juloski, J.; Vichi, A. Clinically Relevant Properties of 3D Printable Materials for Intraoral Use in Orthodontics: A Critical Review of the Literature. Materials 2023, 16, 2166. [Google Scholar] [CrossRef] [PubMed]
- Jindal, P.; Worcester, F.; Siena, F.L.; Forbes, C.; Juneja, M.; Breedon, P. Mechanical behaviour of 3D printed vs thermoformed clear dental aligner materials under non-linear compressive loading using FEM. J. Mech. Behav. Biomed. Mater. 2020, 112, 104045. [Google Scholar] [CrossRef] [PubMed]
- Skośkiewicz-Malinowska, K.; Mysior, M.; Rusak, A.; Kuropka, P.; Kozakiewicz, M.; Jurczyszyn, K. Application of Texture and Fractal Dimension Analysis to Evaluate Subgingival Cement Surfaces in Terms of Biocompatibility. Materials 2021, 14, 5857. [Google Scholar] [CrossRef]
- Paradowska-Stolarz, A.; Malysa, A.; Mikulewicz, M. Comparison of the Compression and Tensile Modulus of Two Chosen Resins Used in Dentistry for 3D Printing. Materials 2022, 15, 8956. [Google Scholar] [CrossRef]
- Warnecki, M.; Sarul, M.; Kozakiewicz, M.; Zięty, A.; Babiarczuk, B.; Kawala, B.; Jurczyszyn, K. Surface Evaluation of Aligners after Immersion in Coca-Cola and Orange Juice. Materials 2022, 15, 6341. [Google Scholar] [CrossRef]
- Memè, L.; Notarstefano, V.; Sampalmieri, F.; Orilisi, G.; Quinzi, V. ATR-FTIR Analysis of Orthodontic Invisalign® Aligners Subjected to Various In Vitro Aging Treatments. Materials 2021, 14, 818. [Google Scholar] [CrossRef]
- Kul, E.; Abdulrahim, R.; Bayındır, F.; Matori, K.A.; Gül, P. Evaluation of the color stability of temporary materials produced with CAD/CAM. Dent. Med. Probl. 2021, 58, 187–191. [Google Scholar] [CrossRef]
- Paradowska-Stolarz, A.; Wezgowiec, J.; Mikulewicz, M. Comparison of Two Chosen 3D Printing Resins Designed for Orthodontic Use: An In Vitro Study. Materials 2023, 16, 2237. [Google Scholar] [CrossRef]
- Vichi, A.; Balestra, D.; Scotti, N.; Louca, C.; Paolone, G. Translucency of CAD/CAM and 3D Printable Composite Materials for Permanent Dental Restorations. Polymers 2023, 15, 1443. [Google Scholar] [CrossRef] [PubMed]
- Franchi, L.; Vichi, A.; Marti, P.; Lampus, F.; Guercio, S.; Recupero, A.; Giuntini, V.; Goracci, C. 3D Printed Customized Facemask for Maxillary Protraction in the Early Treatment of a Class III Malocclusion: Proof-of-Concept Clinical Case. Materials 2022, 15, 3747. [Google Scholar] [CrossRef] [PubMed]
- Thurzo, A.; Šufliarsky, B.; Urbanová, W.; Čverha, M.; Strunga, M.; Varga, I. Pierre Robin Sequence and 3D Printed Personalized Composite Appliances in Interdisciplinary Approach. Polymers 2022, 14, 3858. [Google Scholar] [CrossRef] [PubMed]
- Paradowska-Stolarz, A.; Wieckiewicz, M.; Kozakiewicz, M.; Jurczyszyn, K. Mechanical Properties, Fractal Dimension, and Texture Analysis of Selected 3D-Printed Resins Used in Dentistry That Underwent the Compression Test. Polymers 2023, 15, 1772. [Google Scholar] [CrossRef]
- Tangpothitham, S.; Pongprueksa, P.; Inokoshi, M.; Mitrirattanakul, S. Effect of post-polymerization with autoclaving treatment on monomer elution and mechanical properties of 3D-printing acrylic resin for splint fabrication. J. Mech. Behav. Biomed. Mater. 2022, 126, 105015. [Google Scholar] [CrossRef]
- ISO 604:2003; Plastics—Determination of Compressive Properties. International Organization for Standardization: Geneva, Switzerland, 2003.
- ISO 527-1:2019; Plastics—Determination of Tensile Properties—Part 1: General Principles. International Organization for Standardization: Geneva, Switzerland, 2019.
- Drummond, J.L.; Savers, E.E. In vitro aging of a heat/pressure-cured composite. Dent. Mater. 1993, 9, 214–216. [Google Scholar] [CrossRef] [PubMed]
- Malysa, A.; Wezgowiec, J.; Grzebieluch, W.; Danel, D.P.; Wieckiewicz, M. Effect of Thermocycling on the Bond Strength of Self-Adhesive Resin Cements Used for Luting CAD/CAM Ceramics to Human Dentin. Int. J. Mol. Sci. 2022, 23, 745. [Google Scholar] [CrossRef]
- Riley, P.; Glenny, A.M.; Worthington, H.V.; Jacobsen, E.; Robertson, C.; Durham, J.; Davies, S.; Petersen, H.; Boyers, D. Oral splints for patients with temporomandibular disorders or bruxism: A systematic review and economic evaluation. Health Technol. Assess 2020, 24, 1–224. [Google Scholar] [CrossRef] [PubMed]
- Comino-Garayoa, R.; Peláez, J.; Tobar, C.; Rodríguez, V.; Suárez, M.J. Adhesion to Zirconia: A Systematic Review of Surface Pretreatments and Resin Cements. Materials 2021, 14, 2751. [Google Scholar] [CrossRef]
- Reymus, M.; Stawarczyk, B. In vitro study on the influence of postpolymerization and aging on the Martens parameters of 3D-printed occlusal devices. J. Prosthet. Dent. 2021, 125, 817–823. [Google Scholar] [CrossRef]
- Miletic, V.; Trifković, B.; Stamenković, D.; Tango, R.N.; Paravina, R.D. Effects of staining and artificial aging on optical properties of gingiva-colored resin-based restorative materials. Clin. Oral. Investig. 2022, 26, 6817–6827. [Google Scholar] [CrossRef] [PubMed]
- Valizadeh, S.; Asiaie, Z.; Kiomarsi, N.; Kharazifard, M.J. Color stability of self-adhering composite resins in different solutions. Dent. Med. Probl. 2020, 57, 31–38. [Google Scholar] [CrossRef] [PubMed]
- El-Rashidy, A.A.; Abdelraouf, R.M.; Habib, N.A. Effect of two artificial aging protocols on color and gloss of single-shade versus multi-shade resin composites. BMC Oral. Health 2022, 22, 321. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Polo, C.; Martín Casado, A.M.; Quispe, N.; Gallardo, E.R.; Montero, J. Colour Changes of Acetal Resins (CAD-CAM) In Vivo. Appl. Sci. 2023, 13, 181. [Google Scholar] [CrossRef]
- Edelmann, A.; English, J.D.; Chen, S.J.; Kasper, F.K. Analysis of the thickness of 3-dimensional printed orthodontic aligners. Am. J. Orthod. Dentofac. Orthop. 2020, 158, e91–e98. [Google Scholar] [CrossRef]
- Emam, M.; Ghanem, L.; Abdel Sadek, H.M. Effect of different intraoral scanners and post-space depths on the trueness of digital impressions. Dent. Med. Probl. 2023; ahead of print. [Google Scholar] [CrossRef]
- Wezgowiec, J.; Paradowska-Stolarz, A.; Malysa, A.; Orzeszek, S.; Seweryn, P.; Wieckiewicz, M. Effects of Various Disinfection Methods on the Material Properties of Silicone Dental Impressions of Different Types and Viscosities. Int. J. Mol. Sci. 2022, 23, 10859. [Google Scholar] [CrossRef]
- Iwasaki, Y.; Hiraguchi, H.; Iwasaki, E.; Yoneyama, T. Effects of immersion disinfection of agar-alginate combined impressions on the surface properties of stone casts. Dent. Mater. J. 2016, 35, 45–50. [Google Scholar] [CrossRef]
- Al Mortadi, N.; Al-Khatib, A.; Alzoubi, K.H.; Khabour, O.F. Disinfection of dental impressions: Knowledge and practice among dental technicians. Clin. Cosmet. Investig. Dent. 2019, 11, 103–108. [Google Scholar] [CrossRef]
- Grymak, A.; Aarts, J.M.; Ma, S.; Waddell, J.N.; Choi, J.J.E. Comparison of hardness and polishability of various occlusal splint materials. J. Mech. Behav. Biomed. Mater. 2021, 115, 104270. [Google Scholar] [CrossRef]
- Aretxabaleta, M.; Xepapadeas, A.B.; Poets, C.F.; Koos, B.; Spintzyk, S. Fracture Load of an Orthodontic Appliance for Robin Sequence Treatment in a Digital Workflow. Materials 2021, 14, 344. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.S.; Nassar, M.; Elsayed, M.A.; Jameel, D.B.; Ahmad, T.T.; Rahman, M.M. In Vitro Optical and Physical Stability of Resin Composite Materials with Different Filler Characteristics. Polymers 2023, 15, 2121. [Google Scholar] [CrossRef] [PubMed]






| Resin | Application |
|---|---|
| Dental LT Clear Resin | Characteristics:
Use:
|
| Formula | Explanations | |
|---|---|---|
| Compressive modulus | Compressive stress Nominal strain | F—force [N] A—initial cross sectional area measurement [mm2] L—the initial distance between the compression plates [mm] ΔL—the decrease in the distance between the plates after the test [mm] |
| Tensile modulus | Tensile stress Nominal strain | F—force [N] A—initial cross sectional area measurement [mm2] L—the initial distance between the grips [mm] ΔL—the increase in the distance between the grips after the test [mm] σ1—the stress in MPa measured at a strain of 0.0005 (ε1) σ2—the stress in MPa measured at a strain of 0.0025 (ε2) |
| E (GPa) | Polishing | Aging | N | M ± SD | Me [Q1–Q3] | Min–Max |
|---|---|---|---|---|---|---|
| Compression Ec | No | No | 30 | 0.87 ± 0.02 | 0.87 [0.86–0.88] | 0.81–0.89 |
| No | Yes | 30 | 0.73 ± 0.03 | 0.73 [0.71–0.74] | 0.67–0.80 | |
| Yes | No | 32 | 0.86 ± 0.03 | 0.87 [0.85–0.88] | 0.74–0.90 | |
| Yes | Yes | 30 | 0.73 ± 0.05 | 0.73 [0.69–0.77] | 0.62–0.81 | |
| Tensile Et | No | No | 32 | 2.96 ± 0.20 | 2.97 [2.84–3.07] | 2.31–3.33 |
| No | Yes | 32 | 2.20 ± 0.10 | 2.23 [2.13–2.26] | 2.01–2.39 | |
| Yes | No | 28 | 3.00 ± 0.11 | 3.00 [2.93–3.08] | 2.77–3.23 | |
| Yes | Yes | 36 | 2.38 ± 0.16 | 2.43 [2.25–2.51] | 1.95–2.62 |
| Effect | SS | df | MS | F | p |
|---|---|---|---|---|---|
| Constant | 731.1 | 1 | 731.1 | 60901 | <0.001 |
| Direct | 210.1 | 1 | 210.1 | 17502 | <0.001 |
| Polishing | 0.166 | 1 | 0.166 | 13.8 | <0.001 |
| Artificial aging | 10.60 | 1 | 10.60 | 883 | <0.001 |
| Direct Polishing | 0.213 | 1 | 0.213 | 17.7 | <0.001 |
| Polishing + Artificial aging | 4.773 | 1 | 4.773 | 398 | <0.001 |
| Artificial aging + Polishing | 0.078 | 1 | 0.078 | 6.49 | 0.011 |
| Direct Polishing + Artificial aging | 0.060 | 1 | 0.060 | 5.02 | 0.026 |
| Error | 2.9052 | 242 | 0.012 |
| Effect | SS | df | MS | F | p |
|---|---|---|---|---|---|
| Constant | 77.10 | 1 | 77.10 | 62136 | 0.000 |
| Polishing | 0.001 | 1 | 0.001 | 1.16 | 0.283 |
| Artificial aging | 0.562 | 1 | 0.562 | 452.6 | 0.000 |
| Artificial aging + Polishing | 0.001 | 1 | 0.001 | 0.44 | 0.506 |
| Error | 0.146 | 118 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paradowska-Stolarz, A.; Wezgowiec, J.; Malysa, A.; Wieckiewicz, M. Effects of Polishing and Artificial Aging on Mechanical Properties of Dental LT Clear® Resin. J. Funct. Biomater. 2023, 14, 295. https://doi.org/10.3390/jfb14060295
Paradowska-Stolarz A, Wezgowiec J, Malysa A, Wieckiewicz M. Effects of Polishing and Artificial Aging on Mechanical Properties of Dental LT Clear® Resin. Journal of Functional Biomaterials. 2023; 14(6):295. https://doi.org/10.3390/jfb14060295
Chicago/Turabian StyleParadowska-Stolarz, Anna, Joanna Wezgowiec, Andrzej Malysa, and Mieszko Wieckiewicz. 2023. "Effects of Polishing and Artificial Aging on Mechanical Properties of Dental LT Clear® Resin" Journal of Functional Biomaterials 14, no. 6: 295. https://doi.org/10.3390/jfb14060295