Carboxymethyl Chitosan Hydrogels for Effective Wound Healing—An Animal Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Chemicals
2.2. Hydrogel Manufacturing
2.3. Animals
2.4. Animal Experiments—Wound Healing
2.5. Statistical Analysis
3. Results and Discussion
3.1. Carboxymethyl Chitosan Hydrogel Formed using the Radiation Technique
3.2. Effectiveness of Wound Treatment with Hydrogel Dressings
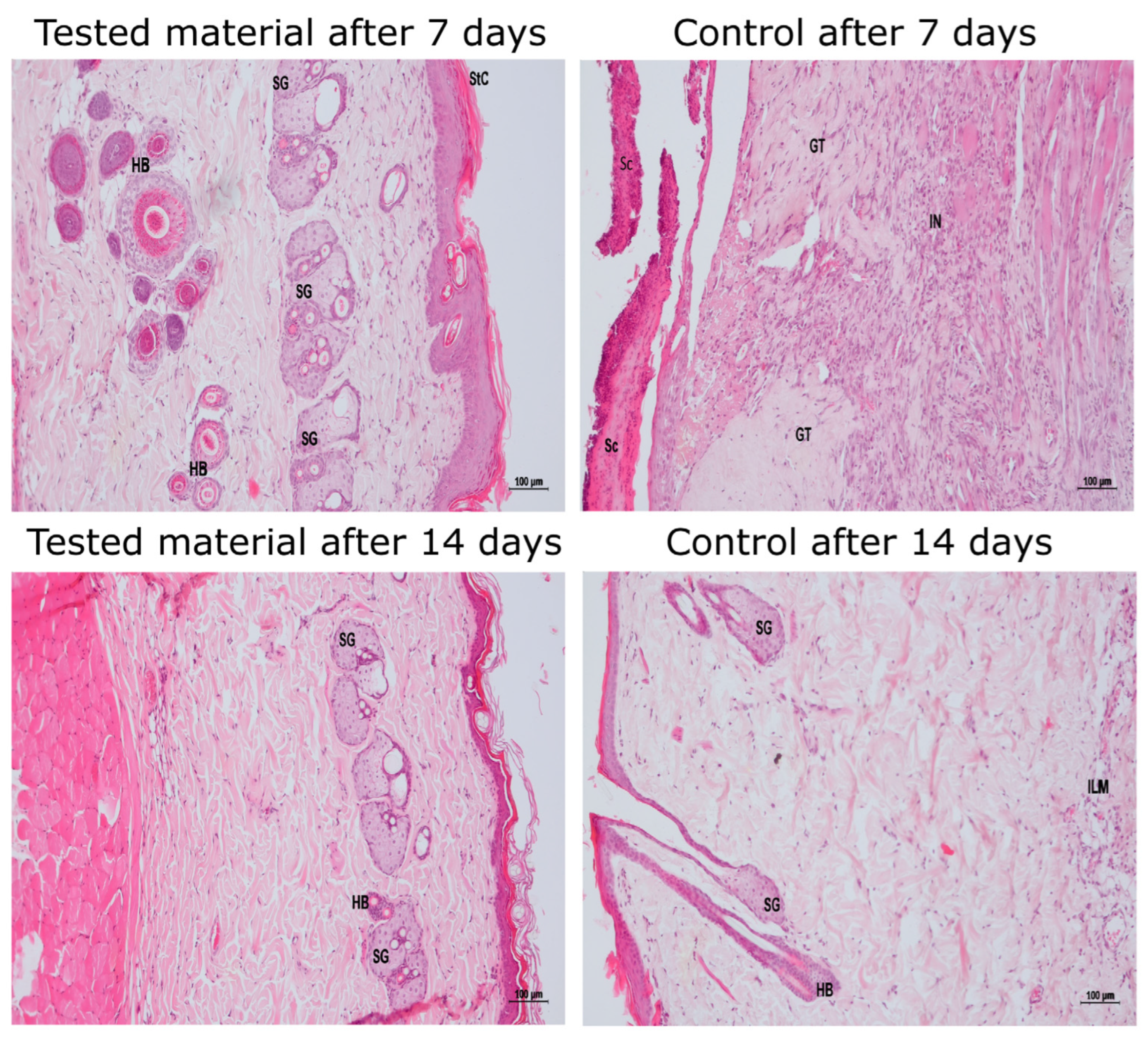
3.3. Histopathological Evaluation of the Effectiveness of the Hydrogel Dressings
3.3.1. Amount of Granulation Tissue
3.3.2. Intensity of Inflammatory Infiltration
3.3.3. Direction of Collagen Fibers
3.3.4. Collagen System
3.3.5. Amount of Young Collagen
3.3.6. Amount of Mature Collagen
3.3.7. Degree of Skin Formation
3.3.8. Disorders in Differentiation and Keratosis in the Young Epidermis
3.3.9. Qualitative Nature of the Inflammatory Infiltrate
3.3.10. General Evaluation of the Histopathological Results
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grubbs, H.; Manna, B. Wound Physiology; StatPearls: Treasure Island, FL, USA, 2023. [Google Scholar]
- Pazyar, N.; Houshmand, G.; Yaghoobi, R.; Hemmati, A.A.; Zeineli, Z.; Ghorbanzadeh, B. Wound healing effects of topical Vitamin K: A randomized controlled trial. Indian. J. Pharmacol. 2019, 51, 88–92. [Google Scholar] [CrossRef]
- Jarbrink, K.; Ni, G.; Sonnergren, H.; Schmidtchen, A.; Pang, C.; Bajpai, R.; Car, J. Prevalence and incidence of chronic wounds and related complications: A protocol for a systematic review. Syst. Rev. 2016, 5, 152. [Google Scholar] [CrossRef]
- Aswathy, S.H.; Narendrakumar, U.; Manjubala, I. Commercial hydrogels for biomedical applications. Heliyon 2020, 6, e03719. [Google Scholar] [CrossRef]
- Holbert, M.D.; Kimble, R.M.; Chatfield, M.; Griffin, B.R. Effectiveness of a hydrogel dressing as an analgesic adjunct to first aid for the treatment of acute paediatric burn injuries: A prospective randomised controlled trial. BMJ Open 2021, 11, e039981. [Google Scholar] [CrossRef]
- Ueno, T.; Yatsuoka, W.; Ishiki, H.; Miyano, K.; Uezono, Y. Effects of an oral mucosa protective formulation on chemotherapy- and/or radiotherapy-induced oral mucositis: A prospective study. BMC Cancer 2022, 22, 90. [Google Scholar] [CrossRef]
- Yang, Z.; Huang, R.; Zheng, B.; Guo, W.; Li, C.; He, W.; Wei, Y.; Du, Y.; Wang, H.; Wu, D.; et al. Highly Stretchable, Adhesive, Biocompatible, and Antibacterial Hydrogel Dressings for Wound Healing. Adv. Sci. 2021, 8, 2003627. [Google Scholar] [CrossRef]
- Barbosa, M.G.; Carvalho, V.F.; Paggiaro, A.O. Hydrogel enriched with sodium alginate and vitamins A and E for diabetic foot ulcer: A randomized controlled trial. Wounds 2022, 34, 229–235. [Google Scholar] [CrossRef]
- Gallelli, G.; Cione, E.; Serra, R.; Leo, A.; Citraro, R.; Matricardi, P.; Di Meo, C.; Bisceglia, F.; Caroleo, M.C.; Basile, S.; et al. Nano-hydrogel embedded with quercetin and oleic acid as a new formulation in the treatment of diabetic foot ulcer: A pilot study. Int. Wound J. 2020, 17, 485–490. [Google Scholar] [CrossRef]
- Klosinski, K.K.; Wach, R.A.; Girek-Bak, M.K.; Rokita, B.; Kolat, D.; Kaluzinska-Kolat, Z.; Klosinska, B.; Duda, L.; Pasieka, Z.W. Biocompatibility and Mechanical Properties of Carboxymethyl Chitosan Hydrogels. Polymers 2022, 15, 144. [Google Scholar] [CrossRef]
- Liang, Y.; Li, M.; Yang, Y.; Qiao, L.; Xu, H.; Guo, B. pH/Glucose Dual Responsive Metformin Release Hydrogel Dressings with Adhesion and Self-Healing via Dual-Dynamic Bonding for Athletic Diabetic Foot Wound Healing. ACS Nano 2022, 16, 3194–3207. [Google Scholar] [CrossRef]
- Feng, P.; Luo, Y.; Ke, C.; Qiu, H.; Wang, W.; Zhu, Y.; Hou, R.; Xu, L.; Wu, S. Chitosan-Based Functional Materials for Skin Wound Repair: Mechanisms and Applications. Front. Bioeng. Biotechnol. 2021, 9, 650598. [Google Scholar] [CrossRef]
- Tharanathan, R.N.; Kittur, F.S. Chitin--the undisputed biomolecule of great potential. Crit. Rev. Food Sci. Nutr. 2003, 43, 61–87. [Google Scholar] [CrossRef]
- Cherng, J.H.; Lin, C.J.; Liu, C.C.; Yeh, J.Z.; Fan, G.Y.; Tsai, H.D.; Chung, C.F.; Hsu, S.D. Hemostasis and Anti-Inflammatory Abilities of AuNPs-Coated Chitosan Dressing for Burn Wounds. J. Pers. Med. 2022, 12, 1089. [Google Scholar] [CrossRef]
- Wang, C.H.; Cherng, J.H.; Liu, C.C.; Fang, T.J.; Hong, Z.J.; Chang, S.J.; Fan, G.Y.; Hsu, S.D. Procoagulant and Antimicrobial Effects of Chitosan in Wound Healing. Int. J. Mol. Sci. 2021, 22, 7067. [Google Scholar] [CrossRef]
- Shariatinia, Z. Carboxymethyl chitosan: Properties and biomedical applications. Int. J. Biol. Macromol. 2018, 120, 1406–1419. [Google Scholar] [CrossRef]
- Geng, Y.; Xue, H.; Zhang, Z.; Panayi, A.C.; Knoedler, S.; Zhou, W.; Mi, B.; Liu, G. Recent advances in carboxymethyl chitosan-based materials for biomedical applications. Carbohydr. Polym. 2023, 305, 120555. [Google Scholar] [CrossRef]
- Goncalves, R.C.; Signini, R.; Rosa, L.M.; Dias, Y.S.P.; Vinaud, M.C.; Lino Junior, R.S. Carboxymethyl chitosan hydrogel formulations enhance the healing process in experimental partial-thickness (second-degree) burn wound healing. Acta Cir. Bras. 2021, 36, e360303. [Google Scholar] [CrossRef]
- Hao, Y.; Zhao, W.; Zhang, H.; Zheng, W.; Zhou, Q. Carboxymethyl chitosan-based hydrogels containing fibroblast growth factors for triggering diabetic wound healing. Carbohydr. Polym. 2022, 287, 119336. [Google Scholar] [CrossRef]
- Chaiwarit, T.; Sommano, S.R.; Rachtanapun, P.; Kantrong, N.; Ruksiriwanich, W.; Kumpugdee-Vollrath, M.; Jantrawut, P. Development of Carboxymethyl Chitosan Nanoparticles Prepared by Ultrasound-Assisted Technique for a Clindamycin HCl Carrier. Polymers 2022, 14, 1736. [Google Scholar] [CrossRef]
- Zhao, L.; Mitomo, H.; Nagasawa, N.; Yoshii, F.; Kume, T. Radiation synthesis and characteristic of the hydrogels based on carboxymethylated chitin derivatives. Carbohydr. Polym. 2003, 51, 169–175. [Google Scholar] [CrossRef]
- Wasikiewicz, J.M.; Mitomo, H.; Nagasawa, N.; Yagi, T.; Tamada, M.; Yoshii, F. Radiation crosslinking of biodegradable carboxymethylchitin and carboxymethylchitosan. J. Appl. Polym. Sci. 2006, 102, 758–767. [Google Scholar] [CrossRef]
- Czechowska-Biskup, R.; Wach, R.A.; Stojek, P.; Kamińska, M.; Rosiak, J.M.; Ulański, P. Synthesis of Chitosan and Carboxymethyl Chitosan Hydrogels by Electron Beam Irradiation. Prog. Chem. Appl. Chitin Its Deriv. 2016, 21, 27–45. [Google Scholar] [CrossRef]
- Kłosiński, K.K.; Pasieka, Z.; Arkuszewski, P.T.; Girek, M.K.; Szymański, P.B.; Wach, R.A.; Czechowska-Biskup, R. Synthesis and Potential Cytotoxicity Evaluation of Carboxymethyl Chitosan Hydrogels. Prog. Chem. Appl. Chitin Its Deriv. 2017, XXII, 82–96. [Google Scholar] [CrossRef]
- Francesko, A.; Petkova, P.; Tzanov, T. Hydrogel Dressings for Advanced Wound Management. Curr. Med. Chem. 2018, 25, 5782–5797. [Google Scholar] [CrossRef]
- PN-EN:ISO 10993-6:2016 Biological Evaluation of Medical Devices—Part 6: Tests for Local Effects after Implantation. Available online: https://www.iso.org/standard/61089.html (accessed on 10 September 2023).
- Ashfaq, A.; Clochard, M.-C.; Coqueret, X.; Dispenza, C.; Driscoll, M.S.; Ulanski, P.; Al-Sheikhly, M. Polymerization Reactions and Modifications of Polymers by Ionizing Radiation. Polymers 2020, 12, 2877. [Google Scholar] [CrossRef] [PubMed]
- Rosiak, J.M. Hydrogel dressings HDR. In Radiation Effects on Polymers; ACS Symposium Series, 475; Clough, R.C., Shalaby, S.W., Eds.; American Chemical Society: Washington, DC, USA, 1991; pp. 271–299. [Google Scholar]
- Ktari, N.; Trabelsi, I.; Bardaa, S.; Triki, M.; Bkhairia, I.; Ben Slama-Ben Salem, R.; Nasri, M.; Ben Salah, R. Antioxidant and hemolytic activities, and effects in rat cutaneous wound healing of a novel polysaccharide from fenugreek (Trigonella foenum-graecum) seeds. Int. J. Biol. Macromol. 2017, 95, 625–634. [Google Scholar] [CrossRef]
- Maalej, H.; Moalla, D.; Boisset, C.; Bardaa, S.; Ben Ayed, H.; Sahnoun, Z.; Rebai, T.; Nasri, M.; Hmidet, N. Rhelogical, dermal wound healing and in vitro antioxidant properties of exopolysaccharide hydrogel from Pseudomonas stutzeri AS22. Colloids Surf. B Biointerfaces 2014, 123, 814–824. [Google Scholar] [CrossRef]
- Ben Slima, S.; Trabelsi, I.; Ktari, N.; Bardaa, S.; Elkaroui, K.; Bouaziz, M.; Abdeslam, A.; Ben Salah, R. Novel Sorghum bicolor (L.) seed polysaccharide structure, hemolytic and antioxidant activities, and laser burn wound healing effect. Int. J. Biol. Macromol. 2019, 132, 87–96. [Google Scholar] [CrossRef]
- Agubata, C.O.; Okereke, C.; Nzekwe, I.T.; Onoja, R.I.; Obitte, N.C. Development and evaluation of wound healing hydrogels based on a quinolone, hydroxypropyl methylcellulose and biodegradable microfibres. Eur. J. Pharm. Sci. 2016, 89, 1–10. [Google Scholar] [CrossRef]
- Kharaziha, M.; Baidya, A.; Annabi, N. Rational Design of Immunomodulatory Hydrogels for Chronic Wound Healing. Adv. Mater. 2021, 33, e2100176. [Google Scholar] [CrossRef]
- Sultana, J.; Molla, M.R.; Kamal, M.; Shahidullah, M.; Begum, F.; Bashar, M.A. Histological differences in wound healing in Maxillofacial region in patients with or without risk factors. Bangladesh J. Pathol. 2009, 24, 3–8. [Google Scholar] [CrossRef]
- Villagomez, A.; Borja, T.; Pontón, P.; Segnini, G.; Barba, P.; Chiliquinga, A.; Yamberla, I.; Pupiales, C.; Suquillo, D.; Díaz, R.F.; et al. Histological and microbiological evaluation of surgical wound closure in mouse skin with cyanoacrylate (Histoacryl®) in comparison to poliglecaprone (Monocryl®) traditional suture. Vet. Anim. Sci. 2021, 13, 100180. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, J.; Seetharaman, S.; Wrice, N.L.; Christy, R.J.; Natesan, S. Delivery of silver sulfadiazine and adipose derived stem cells using fibrin hydrogel improves infected burn wound regeneration. PLoS ONE 2019, 14, e0217965. [Google Scholar] [CrossRef] [PubMed]
- Norahan, M.H.; Pedroza-Gonzalez, S.C.; Sanchez-Salazar, M.G.; Alvarez, M.M.; Trujillo de Santiago, G. Structural and biological engineering of 3D hydrogels for wound healing. Bioact. Mater. 2023, 24, 197–235. [Google Scholar] [CrossRef]
- Fan, F.; Saha, S.; Hanjaya-Putra, D. Biomimetic Hydrogels to Promote Wound Healing. Front. Bioeng. Biotechnol. 2021, 9, 718377. [Google Scholar] [CrossRef]
- Alven, S.; Aderibigbe, B.A. Chitosan and Cellulose-Based Hydrogels for Wound Management. Int. J. Mol. Sci. 2020, 21, 9656. [Google Scholar] [CrossRef]
- Zhang, S.; Ge, G.; Qin, Y.; Li, W.; Dong, J.; Mei, J.; Ma, R.; Zhang, X.; Bai, J.; Zhu, C.; et al. Recent advances in responsive hydrogels for diabetic wound healing. Mater. Today Bio. 2023, 18, 100508. [Google Scholar] [CrossRef]
- Huang, C.; Dong, L.; Zhao, B.; Lu, Y.; Huang, S.; Yuan, Z.; Luo, G.; Xu, Y.; Qian, W. Anti-inflammatory hydrogel dressings and skin wound healing. Clin. Transl. Med. 2022, 12, e1094. [Google Scholar] [CrossRef]
- Kasuya, A.; Tokura, Y. Attempts to accelerate wound healing. J. Dermatol. Sci. 2014, 76, 169–172. [Google Scholar] [CrossRef]
- Jung, S.H.; Jang, B.H.; Kwon, S.; Park, S.J.; Park, T.E.; Kang, J.H. Nematic Fibrin Fibers Enabling Vascularized Thrombus Implants Facilitate Scarless Cutaneous Wound Healing. Adv. Mater. 2023, 35, e2211149. [Google Scholar] [CrossRef]
- de Souza, K.S.; Cantaruti, T.A.; Azevedo, G.M., Jr.; Galdino, D.A.; Rodrigues, C.M.; Costa, R.A.; Vaz, N.M.; Carvalho, C.R. Improved cutaneous wound healing after intraperitoneal injection of alpha-melanocyte-stimulating hormone. Exp. Dermatol. 2015, 24, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Kim, J.W.; Lee, J.H.; Chung, K.J.; Kim, T.G.; Kim, Y.H.; Kim, K.J. Wound healing effects of paste type acellular dermal matrix subcutaneous injection. Arch. Plast. Surg. 2018, 45, 504–511. [Google Scholar] [CrossRef]
- Cunha, J.L.S.; Carvalho, F.M.A.; Pereira Filho, R.N.; Ribeiro, M.A.G.; de Albuquerque-Junior, R.L.C. Effects of Different Protocols of Low-Level Laser Therapy on Collagen Deposition in Wound Healing. Braz. Dent. J. 2019, 30, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Basha, S.I.; Ghosh, S.; Vinothkumar, K.; Ramesh, B.; Kumari, P.H.P.; Mohan, K.V.M.; Sukumar, E. Fumaric acid incorporated Ag/agar-agar hybrid hydrogel: A multifunctional avenue to tackle wound healing. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 111, 110743. [Google Scholar] [CrossRef] [PubMed]
- Brownhill, V.R.; Huddleston, E.; Bell, A.; Hart, J.; Webster, I.; Hardman, M.J.; Wilkinson, H.N. Pre-Clinical Assessment of Single-Use Negative Pressure Wound Therapy During In Vivo Porcine Wound Healing. Adv. Wound Care 2021, 10, 345–356. [Google Scholar] [CrossRef]
- Hong, C.; Chung, H.; Lee, G.; Kim, C.; Kim, D.; Oh, S.J.; Kim, S.H.; Lee, K. Hydrogel/Nanofiber Composite Wound Dressing Optimized for Skin Layer Regeneration through the Mechanotransduction-Based Microcellular Environment. ACS Appl. Bio Mater. 2023, 6, 1774–1786. [Google Scholar] [CrossRef]
- Shamloo, A.; Aghababaie, Z.; Afjoul, H.; Jami, M.; Bidgoli, M.R.; Vossoughi, M.; Ramazani, A.; Kamyabhesari, K. Fabrication and evaluation of chitosan/gelatin/PVA hydrogel incorporating honey for wound healing applications: An in vitro, in vivo study. Int. J. Pharm. 2021, 592, 120068. [Google Scholar] [CrossRef]
- Savitri, C.; Kwon, J.W.; Drobyshava, V.; Ha, S.S.; Park, K. M2 Macrophage-Derived Concentrated Conditioned Media Significantly Improves Skin Wound Healing. Tissue Eng. Regen. Med. 2022, 19, 617–628. [Google Scholar] [CrossRef]
- Jana, S.; Datta, P.; Das, H.; Jaiswal, S.; Ghosh, P.R.; Lahiri, D.; Kundu, B.; Nandi, S.K. Copper and cobalt doped bioactive glass-fish dermal collagen electrospun mat triggers key events of diabetic wound healing in full-thickness skin defect model. J. Mech. Behav. Biomed. Mater. 2022, 134, 105414. [Google Scholar] [CrossRef]
- Ge, B.; Wang, H.; Li, J.; Liu, H.; Yin, Y.; Zhang, N.; Qin, S. Comprehensive Assessment of Nile Tilapia Skin (Oreochromis niloticus) Collagen Hydrogels for Wound Dressings. Mar. Drugs 2020, 18, 178. [Google Scholar] [CrossRef]
- Chang, J.; Liu, W.; Han, B.; Peng, S.; He, B.; Gu, Z. Investigation of the skin repair and healing mechanism of N-carboxymethyl chitosan in second-degree burn wounds. Wound Repair. Regen. 2013, 21, 113–121. [Google Scholar] [CrossRef] [PubMed]
- He, C.; Ke, M.; Zhong, Z.; Ye, Q.; He, L.; Chen, Y.; Zhou, J. Effect of the Degree of Acetylation of Chitin Nonwoven Fabrics for Promoting Wound Healing. ACS Appl. Bio Mater. 2021, 4, 1833–1842. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.J.; Tatar, A.; Tu, Y.; Nobumori, C.; Yang, S.H.; Goulbourne, C.N.; Herrmann, H.; Fong, L.G.; Young, S.G. An absence of nuclear lamins in keratinocytes leads to ichthyosis, defective epidermal barrier function, and intrusion of nuclear membranes and endoplasmic reticulum into the nuclear chromatin. Mol. Cell Biol. 2014, 34, 4534–4544. [Google Scholar] [CrossRef] [PubMed]
- Hunter-Featherstone, E.; Young, N.; Chamberlain, K.; Cubillas, P.; Hulette, B.; Wei, X.; Tiesman, J.P.; Bascom, C.C.; Benham, A.M.; Goldberg, M.W.; et al. Culturing Keratinocytes on Biomimetic Substrates Facilitates Improved Epidermal Assembly In Vitro. Cells 2021, 10, 1177. [Google Scholar] [CrossRef] [PubMed]
- Yu, N.; Li, Y.; Wang, Y.; Xu, H.; Ye, F.; Fu, Q. Healing effect of carboxymethyl chitosan-plantamajoside hydrogel on burn wound skin. Burns 2022, 48, 902–914. [Google Scholar] [CrossRef]
- Yaseen, H.S.; Asif, M.; Saadullah, M.; Mahrukh; Asghar, S.; Shams, M.U.; Bazmi, R.R.; Saleem, M.; Yousaf, H.M.; Yaseen, M. Methanolic extract of Ephedra ciliata promotes wound healing and arrests inflammatory cascade in vivo through downregulation of TNF-alpha. Inflammopharmacology 2020, 28, 1691–1704. [Google Scholar] [CrossRef]
- Mozalewska, W.; Czechowska-Biskup, R.; Olejnik, A.K.; Wach, R.A.; Ulański, P.; Rosiak, J.M. Chitosan-containing hydrogel wound dressings prepared by radiation technique. Radiat. Phys. Chem. 2017, 134, 1–7. [Google Scholar] [CrossRef]
- Zhang, B.; Lv, Y.; Yu, C.; Zhang, W.; Song, S.; Li, Y.; Chong, Y.; Huang, J.; Zhang, Z. Au-Pt nanozyme-based multifunctional hydrogel dressing for diabetic wound healing. Biomater. Adv. 2022, 137, 212869. [Google Scholar] [CrossRef]
- Chang, G.; Dang, Q.; Liu, C.; Wang, X.; Song, H.; Gao, H.; Sun, H.; Zhang, B.; Cha, D. Carboxymethyl chitosan and carboxymethyl cellulose based self-healing hydrogel for accelerating diabetic wound healing. Carbohydr. Polym. 2022, 292, 119687. [Google Scholar] [CrossRef]
- Zhou, Z.; Zhang, X.; Xu, L.; Lu, H.; Chen, Y.; Wu, C.; Hu, P. A self-healing hydrogel based on crosslinked hyaluronic acid and chitosan to facilitate diabetic wound healing. Int. J. Biol. Macromol. 2022, 220, 326–336. [Google Scholar] [CrossRef]

| Amount of Granulation Tissue | One Week | |||
|---|---|---|---|---|
| Control Hydrogel | CMCS Hydrogel | |||
| N | Fraction | N | Fraction | |
| Abundant | 3 | 0.50 | - | - |
| Mean | 1 | 0.17 | - | - |
| Poor | - | - | 4 | 0.67 |
| Absent | 2 | 0.33 | 2 | 0.33 |
| Comparison of the tested material with the control material | Fisher’s exact test, p = 0.0563 (FDR < 0.25) | |||
| Two Weeks | ||||
| Abundant | 1 | 0.17 | 1 | 0.17 |
| Mean | 1 | 0.17 | 2 | 0.33 |
| Poor | 2 | 0.33 | 1 | 0.17 |
| Absent | 2 | 0.33 | 2 | 0.33 |
| Comparison of the tested material with the control material | Fisher’s exact test, p = 1.0000 (FDR > 0.25) | |||
| Inflammatory Infiltration (Intensification) | One Week | |||
|---|---|---|---|---|
| Control Hydrogel | CMCS Hydrogel | |||
| N | Fraction | N | Fraction | |
| Abundant | 4 | 0.67 | - | - |
| Moderate | - | - | 1 | 0.17 |
| Poor | 2 | 0.33 | 1 | 0.17 |
| Absent | - | - | 4 | 0.67 |
| Comparison of the tested material with the control material | Fisher’s exact test, p = 0.0129 (FDR < 0.25) | |||
| Two Weeks | ||||
| Abundant | - | - | 1 | 0.17 |
| Moderate | 4 | 0.67 | 1 | 0.17 |
| Poor | 2 | 0.33 | 2 | 0.33 |
| Absent | - | - | 2 | 0.33 |
| Comparison of the tested material with the control material | Fisher’s exact test, p = 0.1775 (FDR > 0.25) | |||
| Direction of Collagen Fibers | One Week | |||
|---|---|---|---|---|
| Control Hydrogel | CMCS Hydrogel | |||
| N | Fraction | N | Fraction | |
| Vertical | 2 | 0.33 | - | - |
| Mixed | 2 | 0.33 | 2 | 0.33 |
| Horizontal | 2 | 0.33 | 4 | 0.67 |
| Comparison of the tested material with the control material | Fisher’s Exact test, p = 0.4805 (FDR > 0.25) | |||
| Two Weeks | ||||
| Vertical | - | - | 1 | 0.17 |
| Mixed | 6 | 1.0 | 3 | 0.50 |
| Horizontal | - | - | 2 | 0.33 |
| Comparison of the tested material with the control material | Fisher’s exact test, p = 0.1818 (FDR > 0.25) | |||
| Collagen System | One Week | |||
|---|---|---|---|---|
| Control Hydrogel | CMCS Hydrogel | |||
| N | Fraction | N | Fraction | |
| Reticulate | 4 | 0.67 | 1 | 0.17 |
| Mixed | 1 | 0.17 | 1 | 0.17 |
| Bundle | 1 | 0.17 | 4 | 0.67 |
| Comparison of the tested material with the control material | Fisher’s exact test, p = 0.3506 (FDR > 0.25) | |||
| Two Weeks | ||||
| Reticulate | 1 | 0.17 | - | - |
| Mixed | 4 | 0.67 | 4 | 0.67 |
| Bundle | 1 | 0.17 | 2 | 0.33 |
| Comparison of the tested material with the control material | Fisher’s exact test, p = 1.0000 (FDR > 0.25) | |||
| Amount of Young Collagen | One Week | |||
|---|---|---|---|---|
| Control Hydrogel | CMCS Hydrogel | |||
| N | Fraction | N | Fraction | |
| Abundant | 3 | 0.50 | 1 | 0.17 |
| Moderate | 2 | 0.33 | 1 | 0.17 |
| Minimal | 1 | 0.17 | 2 | 0.33 |
| Absent | - | - | 2 | 0.33 |
| Comparison of the tested material with the control material | Fisher’s exact test, p = 0.4935 (FDR > 0.25) | |||
| Two Weeks | ||||
| Abundant | - | - | - | - |
| Moderate | 4 | 0.67 | 2 | 0.33 |
| Minimal | 2 | 0.33 | 4 | 0.67 |
| Absent | - | - | - | - |
| Comparison of the tested material with the control material | Fisher’s exact test, p = 0.5671 (FDR > 0.25) | |||
| Amount of Mature Collagen | One Week | |||
|---|---|---|---|---|
| Control Hydrogel | CMCS Hydrogel | |||
| N | Fraction | N | Fraction | |
| Abundant | 1 | 0.17 | 5 | 0.83 |
| Moderate | 2 | 0.33 | 1 | 0.17 |
| Minimal | 3 | 0.50 | - | - |
| Abstract | - | - | - | - |
| Comparison of the tested material with the control material | Fisher’s exact test, p = 0.0801 (FDR < 0.25) | |||
| Two Weeks | ||||
| Abundant | 1 | 0.17 | 1 | 0.17 |
| Moderate | 4 | 0.67 | 4 | 0.67 |
| Minimal | 1 | 0.17 | 1 | 0.17 |
| Abstract | - | - | - | - |
| Comparison of the tested material with the control material | Fisher’s exact test, p = 1.0000 (FDR > 0.25) | |||
| Degree of Skin Formation | One Week | |||
|---|---|---|---|---|
| Control Hydrogel | CMCS Hydrogel | |||
| N | Fraction | N | Fraction | |
| Lack | 2 | 0.33 | - | - |
| Short cuticle protrusions | 2 | 0.33 | - | - |
| Long epidermal bridges | - | - | - | - |
| Full coverage of the wound with epidermis | 2 | 0.33 | 6 | 1.0 |
| Comparison of the tested material with the control material | Fisher’s exact test, p = 0.0606 (FDR < 0.25) | |||
| Two Weeks | ||||
| Lack | - | - | 2 | 0.33 |
| Short cuticle protrusions | 2 | 0.33 | - | - |
| Long epidermal bridges | - | - | - | - |
| Full coverage of the wound with epidermis | 4 | 0.67 | 4 | 0.67 |
| Comparison of the tested material with the control material | Fisher’s exact test, p = 0.2121 (FDR > 0.25) | |||
| Differentiation and Keratosis Disorders | One Week | |||
|---|---|---|---|---|
| Control Hydrogel | CMCS Hydrogel | |||
| N | Fraction | N | Fraction | |
| Plentiful | 4 | 0.67 | - | - |
| Moderate | - | - | 1 | 0.17 |
| Significant | - | - | - | - |
| Minimal | 2 | 0.33 | 5 | 0.83 |
| Comparison of the tested material with the control material | Fisher’s exact test, p = 0.0606 (FDR < 0.25) | |||
| Two Weeks | ||||
| Plentiful | - | - | 2 | 0.33 |
| Moderate | 4 | 0.67 | 1 | 0.17 |
| Significant | 2 | 0.33 | - | - |
| Minimal | - | - | 3 | 0.50 |
| Comparison of the tested material with the control material | Fisher’s exact test, p = 0.0368 (FDR < 0.25) | |||
| Inflammatory Infiltrate (Composition) | One Week | |||
|---|---|---|---|---|
| Control Hydrogel | CMCS Hydrogel | |||
| N | Fraction | N | Fraction | |
| Neutrophilic | 4 | 0.67 | 1 | 0.17 |
| Lymphocytic | 1 | 0.17 | - | - |
| Lymphocytic–histiocytic | 1 | 0.17 | 1 | 0.17 |
| Mixed | - | - | - | - |
| Lack | - | - | 4 | 0.67 |
| Comparison of the tested material with the control material | Fisher’s exact test, p = 0.0693 (FDR < 0.25) | |||
| Two Weeks | ||||
| Neutrophilic | - | - | - | - |
| Lymphocytic | 1 | 0.17 | 1 | 0.17 |
| Lymphocytic–histiocytic | 3 | 0.50 | 2 | 0.33 |
| Mixed | 2 | 0.33 | 1 | 0.17 |
| Lack | - | - | 2 | 0.33 |
| Comparison of the tested material with the control material | Fisher’s exact test, p = 0.7403 (FDR > 0.25) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kłosiński, K.K.; Wach, R.A.; Kruczkowska, W.; Duda, Ł.; Kołat, D.; Kałuzińska-Kołat, Ż.; Arkuszewski, P.T.; Pasieka, Z.W. Carboxymethyl Chitosan Hydrogels for Effective Wound Healing—An Animal Study. J. Funct. Biomater. 2023, 14, 473. https://doi.org/10.3390/jfb14090473
Kłosiński KK, Wach RA, Kruczkowska W, Duda Ł, Kołat D, Kałuzińska-Kołat Ż, Arkuszewski PT, Pasieka ZW. Carboxymethyl Chitosan Hydrogels for Effective Wound Healing—An Animal Study. Journal of Functional Biomaterials. 2023; 14(9):473. https://doi.org/10.3390/jfb14090473
Chicago/Turabian StyleKłosiński, Karol Kamil, Radosław Aleksander Wach, Weronika Kruczkowska, Łukasz Duda, Damian Kołat, Żaneta Kałuzińska-Kołat, Piotr Tomasz Arkuszewski, and Zbigniew Włodzimierz Pasieka. 2023. "Carboxymethyl Chitosan Hydrogels for Effective Wound Healing—An Animal Study" Journal of Functional Biomaterials 14, no. 9: 473. https://doi.org/10.3390/jfb14090473
APA StyleKłosiński, K. K., Wach, R. A., Kruczkowska, W., Duda, Ł., Kołat, D., Kałuzińska-Kołat, Ż., Arkuszewski, P. T., & Pasieka, Z. W. (2023). Carboxymethyl Chitosan Hydrogels for Effective Wound Healing—An Animal Study. Journal of Functional Biomaterials, 14(9), 473. https://doi.org/10.3390/jfb14090473










