Dental Implant Survival Rates: Comprehensive Insights from a Large-Scale Electronic Dental Registry
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Source
2.2. Data Collection and Processing
2.3. Data Extraction Process
2.4. Data Processing and Preparation
2.5. Data Structuring for Analysis
2.6. Study Objectives and Outcome Measures
2.7. Statistical Analysis
2.8. Ethics Approval
3. Results
3.1. Study Population and Implant Types
- Implant scenarios: The implant procedures included bone grafting (28.8%), open sinus lifting (10.2%), closed sinus lifting (6.2%), and other unspecified procedures (54.8%). The highest failure rates were observed in closed sinus lifting procedures at 3.96% and the lowest in cases without sinus lifting or bone grafting at 2.01% (see Table 1).
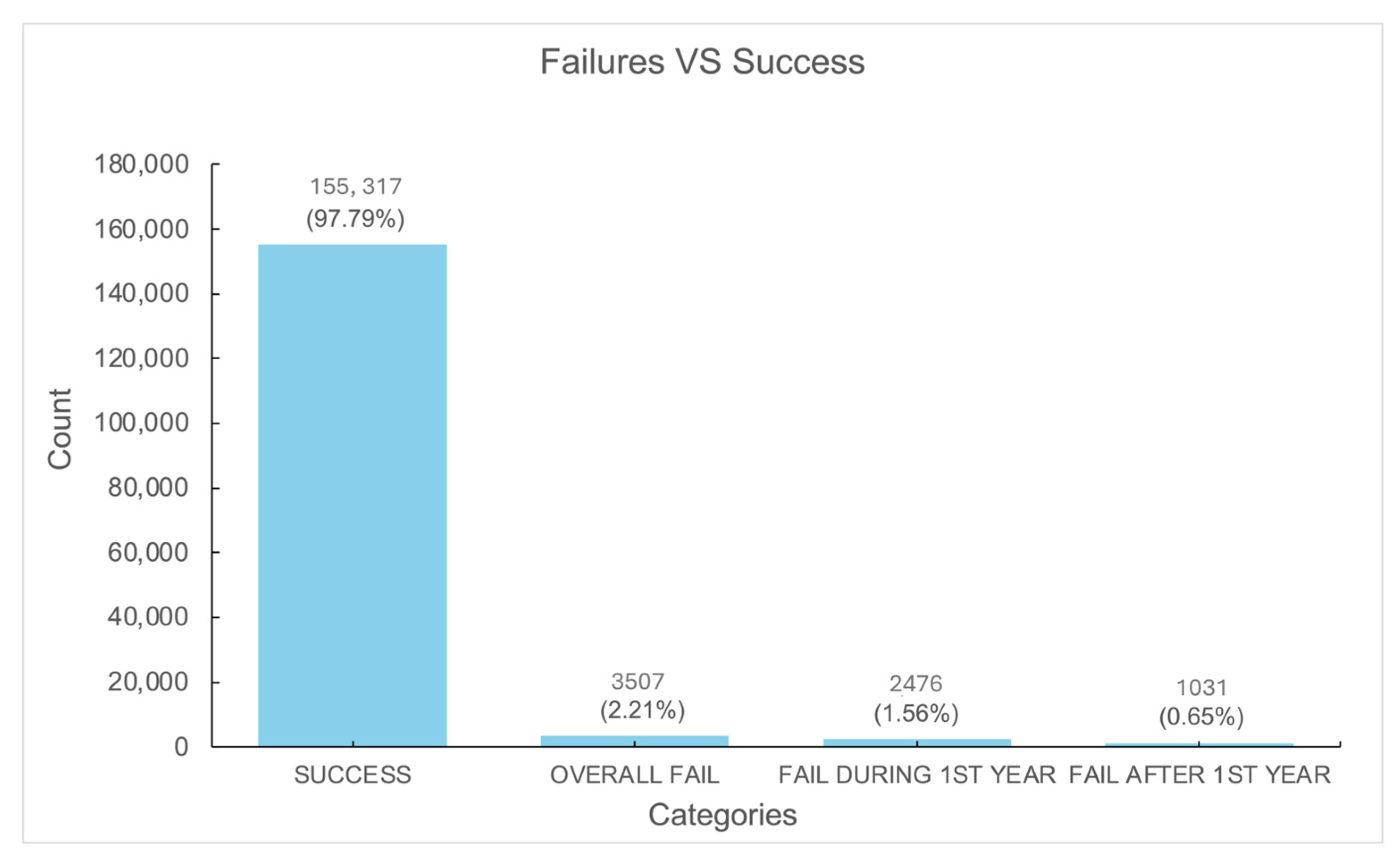
3.2. Implant Survival and Failure Rates
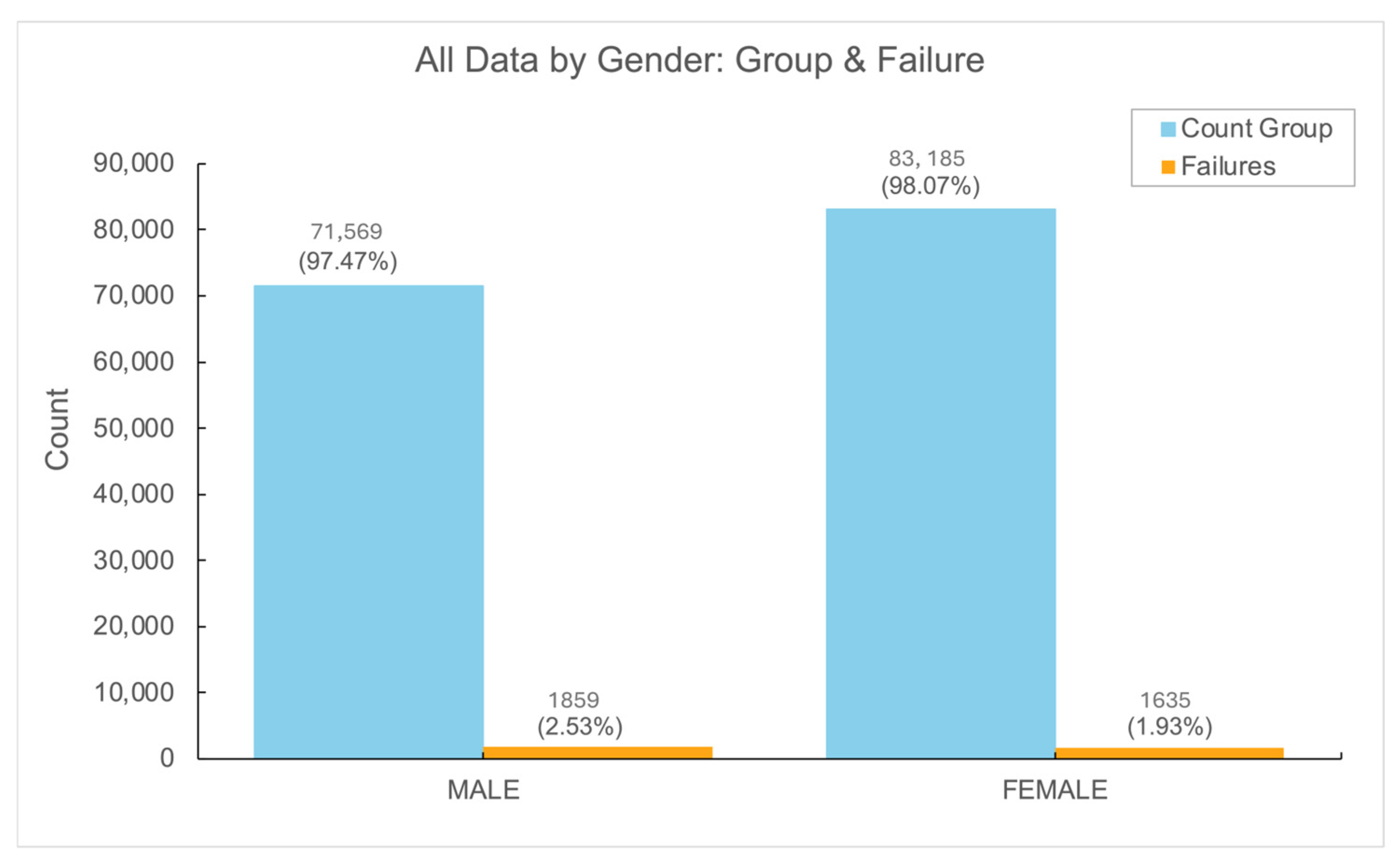
3.3. Gender Differences in Implant Outcomes
3.4. Socioeconomic Status and Implant Failure
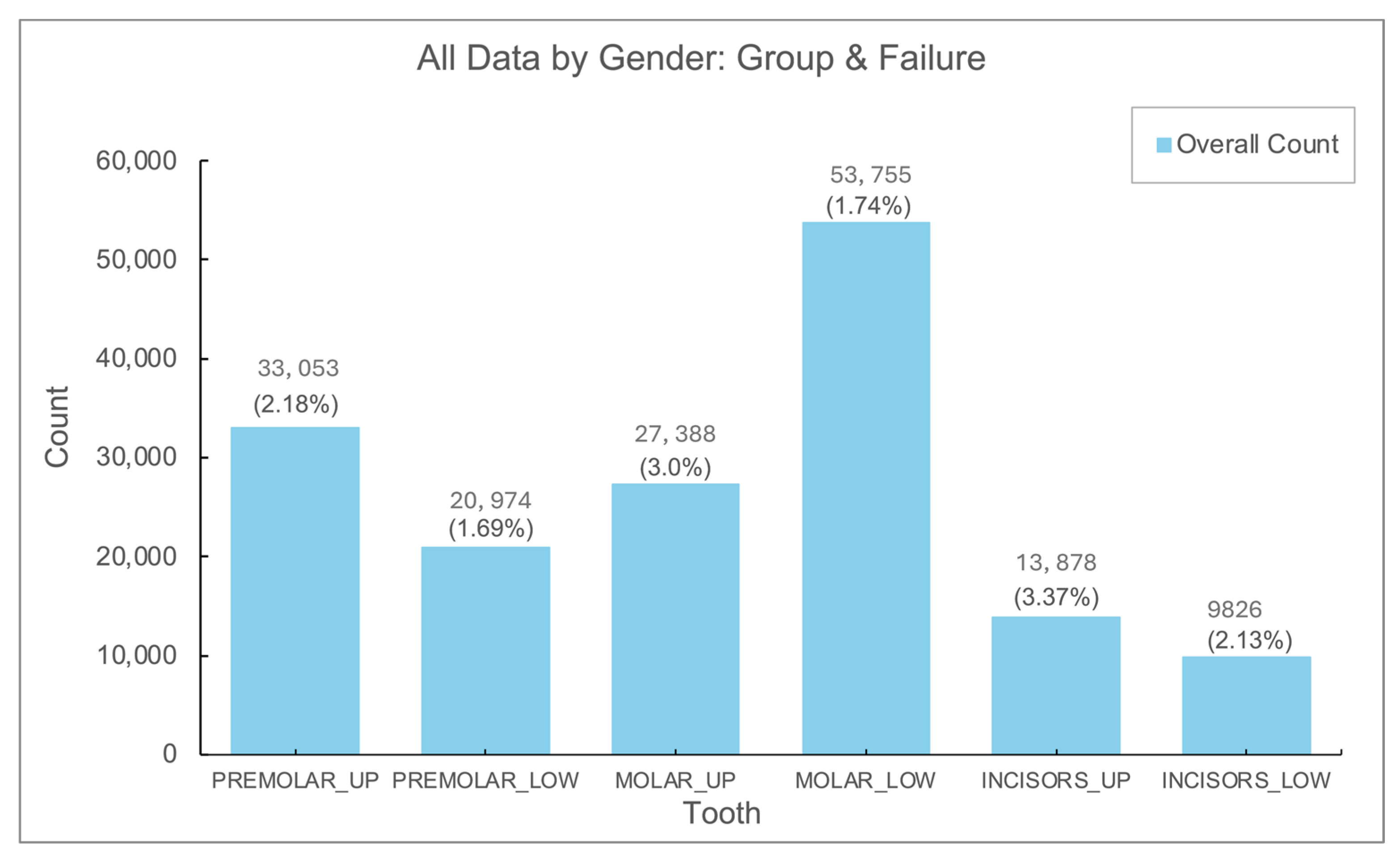
3.5. Implant Failure by Location
3.6. Rehabilitation Type and Failure Rates
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HMO | Health Maintenance Organization |
| GEE | generalized estimating equation |
References
- Guglielmotti, M.B.; Olmedo, D.G.; Cabrini, R.L. Research on implants and osseointegration. Periodontology 2000 2019, 79, 178–189. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, H.S.; Jansen, J.A. The development and future of dental implants. Dent. Mater. J. 2020, 39, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Palma-Carrió, C.; Maestre-Ferrín, L.; Peñarrocha-Oltra, D.; Peñarrocha-Diago, M.A.; Peñarrocha-Diago, M. Risk factors associated with early failure of dental implants. A literature review. Med. Oral Patol. Oral Cir. Bucal. 2011, 16, e514–e517. [Google Scholar] [CrossRef] [PubMed]
- Manzano, G.; Montero, J.; Martín-Vallejo, J.; Del Fabbro, M.; Bravo, M.; Testori, T. Risk Factors in Early Implant Failure: A Meta-Analysis. Implant Dent. 2016, 25, 272–280. [Google Scholar] [CrossRef] [PubMed]
- Levin, L. Dealing with dental implant failures. J. Appl. Oral Sci. 2008, 16, 171–175. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Staedt, H.; Rossa, M.; Lehmann, K.M.; Al-Nawas, B.; Kämmerer, P.W.; Heimes, D. Potential risk factors for early and late dental implant failure: A retrospective clinical study on 9080 implants. Int. J. Implant Dent. 2020, 6, 81. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- El Askary, A.S.; Meffert, R.M.; Griffin, T. Why do dental implants fail? Part II. Implant Dent. 1999, 8, 265–277. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, K.M.; Kämmerer, P.W.; Karbach, J.; Scheller, H.; Al-Nawas, B.; Wagner, W. Long-term effect of overdenture bar design on peri-implant tissues. Int. J. Oral Maxillofac. Implant. 2013, 28, 1126–1131. [Google Scholar] [CrossRef] [PubMed]
- Alsaadi, G.; Quirynen, M.; Komárek, A.; van Steenberghe, D. Impact of local and systemic factors on the incidence of late oral implant loss. Clin. Oral Implant. Res. 2008, 19, 670–676. [Google Scholar] [CrossRef] [PubMed]
- Tolstunov, L. Dental implant success-failure analysis: A concept of implant vulnerability. Implant Dent. 2006, 15, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Kim, Y.K.; Park, J.Y.; Kim, S.G.; Kim, M.J.; Yun, P.Y. Short-term clinical retrospective study of implants in geriatric patients older than 70 years. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 110, 442–446. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.Y.; Montero, E.; Wu, X.Y.; Palombo, D.; Wei, S.M.; Sanz-Sánchez, I. Bone preservation or augmentation simultaneous with or prior to dental implant placement: A systematic review of outcomes and outcome measures used in clinical trials in the last 10 years. J. Clin. Periodontol. 2023, 50 (Suppl. S25), 67–82. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Asgeirsson, A.G.; Zwahlen, M.; Sailer, I. Improvements in implant dentistry over the last decade: Comparison of survival and complication rates in older and newer publications. Int. J. Oral Maxillofac. Implant. 2014, 29, 308–324. [Google Scholar] [CrossRef] [PubMed]
- Zarb, G.A.; Albrektsson, T. Consensus report: Towards optimized treatment outcomes for dental implants. J. Prosthet. Dent. 1998, 80, 641. [Google Scholar] [CrossRef] [PubMed]
- Tian, J.; Cheng, W.; Zhang, Q.; Zhang, Y.; Guo, J.; Liu, Y. Analysis on Focus of Clinical Evaluation of Dental Implants (Systems). Zhongguo Yi Liao Qi Xie Za Zhi 2022, 46, 84–87. (In Chinese) [Google Scholar] [CrossRef] [PubMed]
- Buser, D.; Weber, H.P.; Lang, N.P. Tissue integration of non-submerged implants. 1-year results of a prospective study with 100 ITI hollow-cylinder and hollow-screw implants. Clin. Oral Implant. Res. 1990, 1, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Buser, D.; Mericske-Stern, R.; Bernard, J.P.; Behneke, A.; Behneke, N.; Hirt, H.P.; Belser, U.C.; Lang, N.P. Long-term evaluation of non-submerged ITI implants. Part 1: 8-year life table analysis of a prospective multi-center study with 2359 implants. Clin Oral Implant. Res. 1997, 8, 161–172. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.S.; Lee, B.A.; Choi, S.H.; Kim, Y.T. Evaluation of failed implants and reimplantation at sites of previous dental implant failure: Survival rates and risk factors. J. Periodontal Implant. Sci. 2022, 52, 230–241. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Abrishami, M.H.; Shiezadeh, F.; Samieirad, S.; Mollaei, M.; MohammadZadeh Mahrokh, F.; Khosravi, F. Analyzing the Causes and Frequency of Early Dental Implant Failure among Iranians: An Epidemiological Study. Int. J. Dent. 2023, 2023, 2107786. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chatzopoulos, G.S.; Wolff, L.F. Survival Rates and Factors Affecting the Outcome Following Immediate and Delayed Implant Placement: A Retrospective Study. J. Clin. Med. 2022, 11, 4598. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Simonis, P.; Dufour, T.; Tenenbaum, H. Long-term implant survival and success: A 10–16-year follow-up of non-submerged dental implants. Clin. Oral Implant. Res. 2010, 21, 772–777. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Hemavardhini, A.; Ranjan, M.; Pasricha, N.; Thakar, S.S.; Soni, K.J.; Hassan, S.; Goyal, K.; Singh, D. Evaluation of Survival Rates of Dental Implants and the Risk Factors: A Retrospective Follow-Up Study. Cureus 2024, 16, e55360. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Negri, M.; Galli, C.; Smerieri, A.; Macaluso, G.M.; Manfredi, E.; Ghiacci, G.; Toffoli, A.; Bonanini, M.; Lumetti, S. The effect of age, gender, and insertion site on marginal bone loss around endosseous implants: Results from a 3-year trial with premium implant system. Biomed. Res. Int. 2014, 2014, 369051. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Park, H.S.; Jeong, S.H.; Kwon, O.W. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am. J. Orthod. Dentofacial Orthop. 2006, 130, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Fouda, A.A.H. The impact of the alveolar bone sites on early implant failure: A systematic review with meta-analysis. J. Korean Assoc. Oral Maxillofac. Surg. 2020, 46, 162–173. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Verma, A.; Singh, S.V.; Arya, D.; Shivakumar, S.; Chand, P. Mechanical failures of dental implants and supported prostheses: A systematic review. J. Oral Biol. Craniofacial Res. 2023, 13, 306–314. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sailer, I.; Karasan, D.; Todorovic, A.; Ligoutsikou, M.; Pjetursson, B.E. Prosthetic failures in dental implant therapy. Periodontology 2000 2022, 88, 130–144. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cortellini, S.; Favril, C.; De Nutte, M.; Teughels, W.; Quirynen, M. Patient compliance as a risk factor for the outcome of implant treatment. Periodontology 2000 2019, 81, 209–225. [Google Scholar] [CrossRef] [PubMed]
| Group | Count Group (%) | Failure Rate |
|---|---|---|
| Dental Bone + Grafting | 45,715 (28.8) | 2.17% |
| Open Sinus Lifting | 16,211 (10.2) | 2.94% |
| Closed Sinus Lifting | 9820 (6.2) | 3.96% |
| Others | 87,078 (54.8) | 2.01% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tobias, G.; Chackartchi, T.; Haim, D.; Mann, J.; Findler, M. Dental Implant Survival Rates: Comprehensive Insights from a Large-Scale Electronic Dental Registry. J. Funct. Biomater. 2025, 16, 60. https://doi.org/10.3390/jfb16020060
Tobias G, Chackartchi T, Haim D, Mann J, Findler M. Dental Implant Survival Rates: Comprehensive Insights from a Large-Scale Electronic Dental Registry. Journal of Functional Biomaterials. 2025; 16(2):60. https://doi.org/10.3390/jfb16020060
Chicago/Turabian StyleTobias, Guy, Tali Chackartchi, Doron Haim, Jonathan Mann, and Mordechai Findler. 2025. "Dental Implant Survival Rates: Comprehensive Insights from a Large-Scale Electronic Dental Registry" Journal of Functional Biomaterials 16, no. 2: 60. https://doi.org/10.3390/jfb16020060
APA StyleTobias, G., Chackartchi, T., Haim, D., Mann, J., & Findler, M. (2025). Dental Implant Survival Rates: Comprehensive Insights from a Large-Scale Electronic Dental Registry. Journal of Functional Biomaterials, 16(2), 60. https://doi.org/10.3390/jfb16020060






