Food Safety in Post-COVID-19 Pandemic: Challenges and Countermeasures
Abstract
:1. Introduction
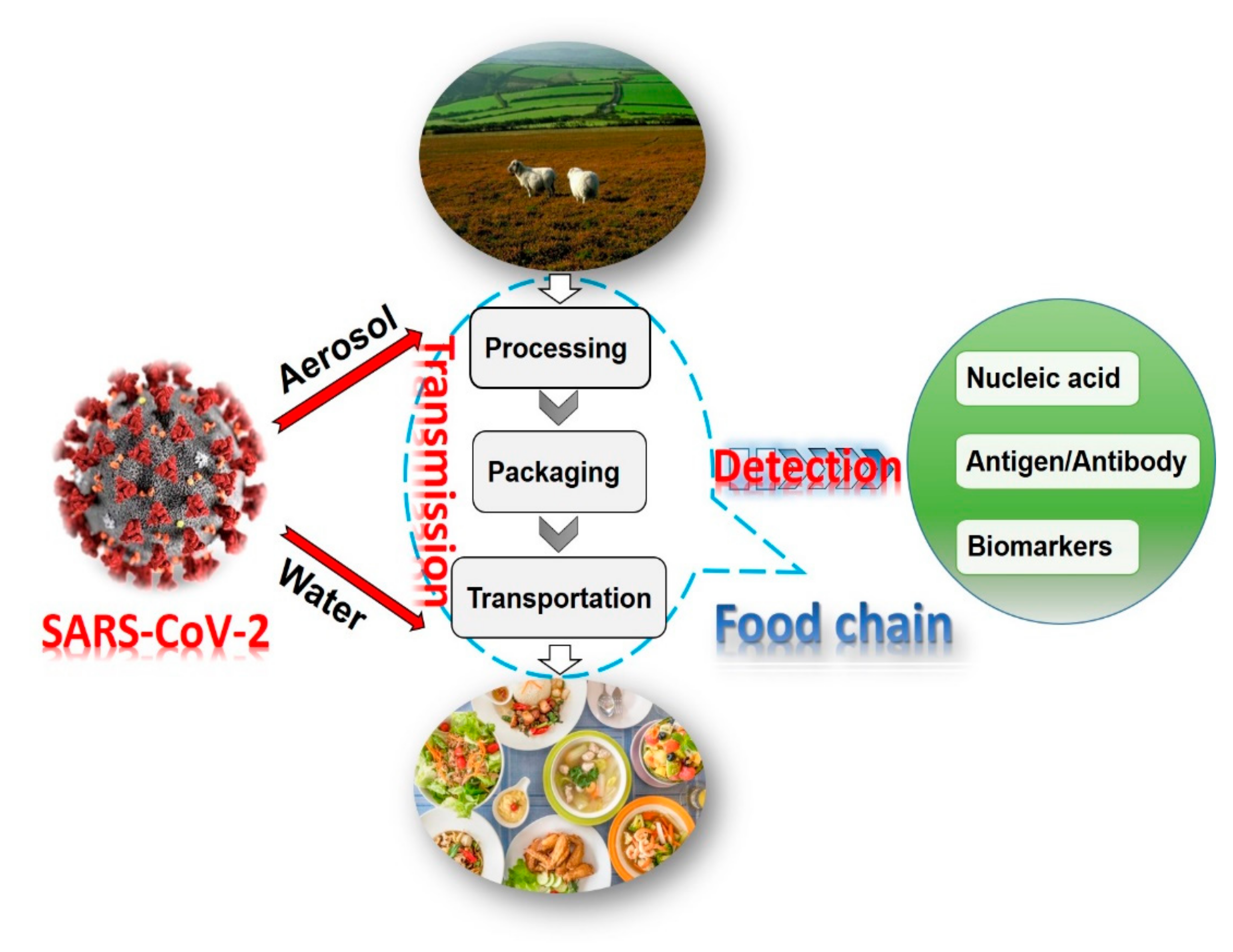
2. Transmission in Food Supply Chain
3. Sample Pretreatment in Different Detection Platforms for SARS-CoV-2
3.1. Nucleic Acid Assays
3.1.1. Pretreatment of Water Samples
3.1.2. Pretreatment of Fruits, Vegetables, and Their Products
3.1.3. Pretreatment of Meat and Its Products
3.2. Immunoassays
3.2.1. Pretreatment Based on Virus Detection Methods
3.2.2. Pretreatment Based on Antibody Detection Methods
3.2.3. Pretreatment Based on Other Detection Methods
4. Advances in Methods for Detection of SARS-CoV-2 in Foods
4.1. Nucleic Acid Detection
4.2. Antibody Detection
4.3. Virus Protein Detection

5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Feng, Y.; Marchal, T.; Sperry, T.; Yi, H. Influence of wind and relative humidity on the social distancing effectiveness to prevent COVID-19 airborne transmission: A numerical study. J. Aerosol Sci. 2020, 147, 105585. [Google Scholar] [CrossRef]
- Rabaan, A.A.; Al-Ahmed, S.H.; Haque, S.; Sah, R.; Tiwari, R.; Malik, Y.S.; Rodriguez-Morales, A.J. SARS-CoV-2, SARS-CoV, and MERS-CoV: A comparative overview. Infez. Med. 2020, 28, 174–184. [Google Scholar]
- Yan, R.; Zhang, Y.; Li, Y.; Xia, L.; Guo, Y.; Zhou, Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science 2020, 367, 1444–1448. [Google Scholar] [CrossRef] [Green Version]
- Su, S.; Wong, G.; Shi, W.; Liu, J.; Lai, A.C.; Zhou, J.; Liu, W.; Bi, Y.; Gao, G.F. Epidemiology, Genetic Recombination, and Pathogenesis of Coronaviruses. Trends Microbiol. 2016, 24, 490–502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, P.; Wang, X. COVID-19: A new challenge for human beings. Cell. Mol. Immunol. 2020, 17, 555–557. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta BioMed. 2020, 91, 157–160. [Google Scholar] [PubMed]
- Benzigar, M.R.; Bhattacharjee, R.; Baharfar, M.; Liu, G. Current methods for diagnosis of human coronaviruses: Pros and cons. Anal. Bioanal. Chem. 2020, 1–20. [Google Scholar] [CrossRef]
- Rizou, M.; Galanakis, I.M.; Aldawoud, T.M.; Galanakis, C.M. Safety of foods, food supply chain and environment within the COVID-19 pandemic. Trends Food Sci. Technol. 2020, 102, 293–299. [Google Scholar] [CrossRef]
- World Health Organization. COVID-19 and Food Safety: Guidance for Food Businesses: Interim Guidance. Available online: https://www.who.int/publications-detail/covid-19-and-food-safety-guidance-for-food-businesses (accessed on 7 April 2020).
- He, D.; Zhao, S.; Lin, Q.; Zhuang, Z.; Cao, P.; Wang, M.H.; Yang, L. Re-Analysis of the Relative Transmissibility of Asymptomatic Cases among Close Contacts. SSRN Electron. J. 2020, 94, 145–147. [Google Scholar] [CrossRef]
- Zhang, N.; Chen, W.; Chan, P.T.J.; Yen, H.-L.; Tang, J.W.-T.; Li, Y. Close contact behavior in indoor environment and transmission of respiratory infection. Indoor Air 2020, 30, 645–661. [Google Scholar] [CrossRef]
- Li, Y.; Qian, H.; Hang, J.; Chen, X.; Hong, L.; Liang, P.; Li, J.; Xiao, S.; Wei, J.; Liu, L.; et al. Evidence for probable aerosol transmission of SARS-CoV-2 in a poorly ventilated restaurant. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Anderson, E.L.; Turnham, P.; Griffin, J.R.; Clarke, C.C. Consideration of the Aerosol Transmission for COVID-19 and Public Health. Risk Anal. 2020, 40, 902–907. [Google Scholar] [CrossRef]
- Galbadage, T.; Peterson, B.M.; Gunasekera, R.S. Does COVID-19 Spread Through Droplets Alone? Front. Public Heal. 2020, 8, 163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, D.H.T.; Mak, S.T.; Yip, N.K.F.; Li, K.K.W. Protective shields for ophthalmic equipment to minimise droplet transmission of COVID-19. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 258, 1571–1573. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.H.; Lui, R.N.; Sung, J.J. Covid-19 and the digestive system. J. Gastroenterol. Hepatol. 2020, 35, 744–748. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Zhang, L.; Wang, Y. COVID-19 indirect contact transmission through the oral mucosa must not be ignored. J. Oral Pathol. Med. 2020, 49, 450–451. [Google Scholar] [CrossRef] [Green Version]
- Wilson, N.M.; Norton, A.; Young, F.P.; Collins, D.W. Airborne transmission of severe acute respiratory syndrome coronavirus-2 to healthcare workers: A narrative review. Anaesthesia 2020, 75, 1086–1095. [Google Scholar] [CrossRef]
- European Food Safety Authority [EFSA]. Coronavirus: No Evidence That Food is a Source or Transmission Route; EFSA: Parma, Italy, 2020. [Google Scholar]
- Olaimat, A.N.; Shahbaz, H.M.; Fatima, N.; Munir, S.; Holley, R.A. Food Safety During and After the Era of COVID-19 Pandemic. Front. Microbiol. 2020, 11, 1854. [Google Scholar] [CrossRef]
- Carducci, A.; Federigi, I.; Liu, D.; Thompson, J.R.; Verani, M. Making Waves: Coronavirus detection, presence and persistence in the water environment: State of the art and knowledge needs for public health. Water Res. 2020, 179, 115907. [Google Scholar] [CrossRef]
- Hayashi, T.; Aboko, K.; Mandan, M.; Yaegashi, N.; Konishi, I. Molecular analysis of binding region of an ACE2 as a receptor for SARS-CoV-2 between humans and mammals. bioRxiv 2020. [Google Scholar] [CrossRef]
- Galanakis, C.M. The Food Systems in the Era of the Coronavirus (COVID-19) Pandemic Crisis. Foods 2020, 9, 523. [Google Scholar] [CrossRef] [PubMed]
- Jiang, F.; Deng, L.; Zhang, L.; Cai, Y.; Cheung, C.W.; Xia, Z. Review of the Clinical Characteristics of Coronavirus Disease 2019 (COVID-19). J. Gen. Intern. Med. 2020, 35, 1545–1549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deng, J.; Jin, Y.; Liu, Y.; Sun, J.; Hao, L.; Bai, J.; Huang, T.; Lin, D.; Jin, Y.; Tian, K. Serological survey of SARS-CoV-2 for experimental, domestic, companion and wild animals excludes intermediate hosts of 35 different species of animals. Transbound. Emerg. Dis. 2020, 67, 1745–1749. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Zhang, H.; Gao, J.; Huang, K.; Yang, Y.; Hui, X.; He, X.; Li, C.; Gong, W.; Zhang, Y.; et al. A serological survey of SARS-CoV-2 in cat in Wuhan. Emerg. Microbes Infect. 2020, 9, 2013–2019. [Google Scholar] [CrossRef]
- Liu, Y.; Ning, Z.; Chen, Y.; Guo, M.; Liu, Y.; Gali, N.K.; Sun, L.; Duan, Y.; Cai, J.; Westerdahl, D.; et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature 2020, 582, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Jalava, K. First respiratory transmitted food borne outbreak? Int. J. Hyg. Environ. Health 2020, 226, 113490. [Google Scholar] [CrossRef] [PubMed]
- Ong, S.W.X.; Tan, Y.K.; Chia, P.Y.; Lee, T.H.; Ng, O.T.; Wong, M.S.Y.; Marimuthu, K. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA 2020, 323, 1610–1612. [Google Scholar] [CrossRef] [Green Version]
- Hadei, M.; Hopke, P.K.; Jonidi, A.; Shahsavani, A. A letter about the airborne transmission of SARS-CoV-2 based on the current evidence. Aerosol Air Qual. Res. 2020, 20, 911–914. [Google Scholar] [CrossRef] [Green Version]
- Otter, J.A.; Donskey, C.; Yezli, S.; Douthwaite, S.; Goldenberg, S.; Weber, D.J. Transmission of SARS and MERS corona-viruses and influenza virus in healthcare settings: The possible role of dry surface contamination. J. Hosp. Infect. 2016, 92, 235–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Lloyd-Smith, J.O. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef] [PubMed]
- Ling, Y.; Xu, S.B.; Lin, Y.X.; Tian, D.; Zhu, Z.Q.; Dai, F.H.; Wu, F.; Song, Z.G.; Huang, W.; Chen, J.; et al. Persistence and clearance of viral RNA in 2019 novel coronavirus disease reha-bilitation patients. Chin. Med. J. 2020, 133, 1039–1043. [Google Scholar] [CrossRef] [PubMed]
- Chin, A.W.; Poon, L.L. Stability of SARS-CoV-2 in different environmental conditions–Authors’ reply. Lancet Microbe 2020, 1, e146. [Google Scholar] [CrossRef]
- General Administration of Customs of the People’s Republic of China (GAC, 2020). Press Conference of the Joint Prevention and Control Mechanism of Epidemic Import the State Council. Available online: http://fangtan.customs.gov.cn/tabid/1071/Default.aspx (accessed on 10 July 2020).
- Ahmed, W.; Angel, N.; Edson, J.; Bibby, K.; Bivins, A.; O’Brien, J.W.; Choi, P.M.; Kitajima, M.; Simpson, S.L.; Li, J.; et al. First confirmed detec-tion of SARS-CoV-2 in untreated wastewater in Australia: A proof of concept for the wastewater surveillance of COVID-19 in the community. Sci. Total Environ. 2020, 728, 138764. [Google Scholar] [CrossRef]
- Gormley, M.; Aspray, T.J.; Kelly, D.A. COVID-19: Mitigating transmission via wastewater plumbing systems. Lancet Glob. Heal. 2020, 8, e643. [Google Scholar] [CrossRef] [Green Version]
- Laura, R. Meat Processing Plants Are Closing due to covid-19 Outbreaks. Beef Shortfalls May Follow. Available online: https://www.washingtonpost.com/business/2020/04/16/meat-processing-plants-are-closing-due-covid-19-outbreaks-beef-shortfalls-may-follow/2020 (accessed on 16 April 2020).
- Fakruddin, M.; Mannan, K.S.B.; Chowdhury, A.; Mazumdar, R.M.; Hossain, M.N.; Islam, S.; Chowdhury, M.A. Nucleic acid amplification: Alternative methods of polymerase chain reaction. J. Pharm. Bioallied Sci. 2013, 5, 245. [Google Scholar] [CrossRef] [PubMed]
- Stals, A.; van Coillie, E.; Uyttendaele, M. Viral genes everywhere: Public health implications of PCR-based testing of foods. Curr. Opin. Virol. 2013, 3, 69–73. [Google Scholar] [CrossRef]
- Srivastava, N.; Kapoor, R.; Kumar, R.; Kumar, S.; Saritha, R.K.; Kumar, S.; Baranwal, V.K. Rapid diagnosis of cucumber mosaic virus in banana plants using a fluorescence-based real-time isothermal reverse transcription-recombinase polymerase amplification assay. J. Virol. Methods 2019, 270, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Yue, H.; Zhou, Y.; Wang, P.; Wang, X.; Wang, Z.; Wang, L.; Fu, Z. A facile label-free electrochemiluminescent biosensor for specific detection of Staphylococcus aureus utilizing the binding between immunoglobulin G and protein A. Talanta 2016, 153, 401–406. [Google Scholar] [CrossRef]
- Guo, Y.; Zhao, C.; Liu, Y.; Nie, H.; Guo, X.; Song, X.-L.; Xu, K.; Li, J.; Wang, J. A novel fluorescence method for the rapid and effective detection of Listeria monocytogenes using aptamer-conjugated magnetic nanoparticles and aggregation-induced emission dots. Analyst 2020, 145, 3857–3863. [Google Scholar] [CrossRef]
- Qi, X.; Wang, Z.; Lu, R.; Liu, J.; Li, Y.; Chen, Y. One-step and DNA amplification-free detection of Listeria monocytogenes in ham samples: Combining magnetic relaxation switching and DNA hybridization reaction. Food Chem. 2021, 338, 127837. [Google Scholar] [CrossRef]
- Broughton, J.P.; Deng, X.; Yu, G.; Fasching, C.L.; Servellita, V.; Singh, J.; Zorn, K. CRISPR–Cas12-based detection of SARS-CoV-2. Nat. Biotechnol. 2020, 38, 870–874. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, Z.; Cui, H.; Song, W.; Ru, X.; Zhou, W.; Yu, X. A simple magnetic nanoparticles-based viral RNA extraction method for efficient detection of SARS-CoV-2. bioRxiv 2020. [Google Scholar] [CrossRef]
- Ikner, L.A.; Soto-Beltran, M.; Bright, K.R. New Method Using a Positively Charged Microporous Filter and Ultrafiltration for Concentration of Viruses from Tap Water. Appl. Environ. Microbiol. 2011, 77, 3500–3506. [Google Scholar] [CrossRef] [Green Version]
- Hennechart-Collette, C.; Martin-Latil, S.; Guillier, L.; Perelle, S. Determination of which virus to use as a process control when testing for the presence of hepatitis A virus and norovirus in food and water. Int. J. Food Microbiol. 2015, 202, 57–65. [Google Scholar] [CrossRef]
- Yang, Z.; Mammel, M.; Papafragkou, E.; Hida, K.; Elkins, C.A.; Kulka, M. Application of next generation sequencing to-ward sensitive detection of enteric viruses isolated from celery samples as an example of produce. Int. J. Food Microbiol. 2017, 261, 73–81. [Google Scholar] [CrossRef]
- Gil-Melgaço, F.; Victoria, M.; Corrêa, A.A.; Ganime, A.C.; Malta, F.C.; Brandão, M.L.L.; Medeiros, V.D.M.; Rosas, C.D.O.; Bricio, S.M.L.; Miagostovich, M.P. Virus recovering from strawberries: Evaluation of a skimmed milk organic flocculation method for assessment of microbiological contamination. Int. J. Food Microbiol. 2016, 217, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Tahk, H.; Lee, K.B.; Lee, M.H.; Seo, D.J.; Cheon, D.-S.; Choi, C. Development of reverse transcriptase polymerase chain reaction enzyme-linked immunosorbent assay for the detection of hepatitis A virus in vegetables. Food Control 2012, 23, 210–214. [Google Scholar] [CrossRef]
- Das, A.; Spackman, E.; Thomas, C.; Swayne, D.E.; Suarez, D.L. Detection of H5N1 High-Pathogenicity Avian Influenza Virus in Meat and Tracheal Samples from Experimentally Infected Chickens. Avian Dis. 2008, 52, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Rutjes, S.A.; Lodder-Verschoor, F.; van der Poel, W.H.; van Duijnhoven, Y.T.; de Roda Husman, A.M. Detection of no-roviruses in foods: A study on virus extraction procedures in foods implicated in outbreaks of human gastroenteritis. J. Food Prot. 2006, 69, 1949–1956. [Google Scholar] [CrossRef]
- Althof, N.; Trojnar, E.; Böhm, T.; Burkhardt, S.; Carl, A.; Contzen, M.; Kilwinski, J.; Mergemeier, S.; Moor, D.; Mäde, D.; et al. Interlaboratory Validation of a Method for Hepatitis E Virus RNA Detection in Meat and Meat Products. Food Environ. Virol. 2019, 11, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Xue, L.; Gao, J.; Cai, W.; Jiang, Y.; Zuo, Y.; Liao, Y.; Qin, Z.; Wu, H.; Cheng, T.; et al. Development of a high-efficient concentrated pretreatment method for noroviruses detection in independent oysters: An ex-tension of the ISO/TS 15216-2: 2013 standard method. Food Control 2020, 111, 107032. [Google Scholar] [CrossRef]
- Di Bartolo, I.; Angeloni, G.; Ponterio, E.; Ostanello, F.; Ruggeri, F.M. Detection of hepatitis E virus in pork liver sausages. Int. J. Food Microbiol. 2015, 193, 29–33. [Google Scholar] [CrossRef]
- Markantonis, N.; Vasickova, P.; Kubankova, M.; Mikel, P.; Botsaris, G. Detection of foodborne viruses in ready-to-eat meat products and meat processing plants. J. Food Saf. 2018, 38, e12436. [Google Scholar] [CrossRef]
- Kim, J.-H.; Oh, S.-W. Development of a filtration-based LAMP–LFA method as sensitive and rapid detection of E. coli O157:H7. J. Food Sci. Technol. 2019, 56, 2576–2583. [Google Scholar] [CrossRef]
- Wu, F.; Zhao, S.; Yu, B.; Chen, Y.M.; Wang, W.; Song, Z.G.; Yuan, M.L. A new coronavirus associated with human respiratory disease in China. Nature 2020, 579, 265–269. [Google Scholar] [CrossRef] [Green Version]
- Wu, L.; Li, X.; Shao, K.; Ye, S.; Liu, C.; Zhang, C.; Han, H. Enhanced immunoassay for porcine circovirus type 2 antibody using enzyme-loaded and quantum dots-embedded shell–core silica nanospheres based on enzyme-linked immunosorbent assay. Anal. Chim. Acta 2015, 887, 192–200. [Google Scholar] [CrossRef]
- Shao, K.; Zhang, C.; Ye, S.; Cai, K.; Wu, L.; Wang, B.; Zou, C.; Lu, Z.; Han, H. Near-infrared electrochemiluminesence bio-sensor for high sensitive detection of porcine reproductive and respiratory syndrome virus based on cyclodextrin-grafted po-rous Au/PtAu nanotube. Sens. Actuators B Chem. 2017, 240, 586–594. [Google Scholar] [CrossRef]
- Wu, L.; Li, G.; Xu, X.; Zhu, L.; Huang, R.; Chen, X. Application of nano-ELISA in food analysis: Recent advances and challenges. TrAC Trends Anal. Chem. 2019, 113, 140–156. [Google Scholar] [CrossRef]
- Oh, S.; Kim, J.; Tran, V.T.; Lee, D.K.; Ahmed, S.R.; Hong, J.C.; Lee, J.; Park, E.Y.; Lee, J. Magnetic nanozyme-linked im-munosorbent assay for ultrasensitive influenza A virus detection. ACS Appl. Mater. Interfaces 2018, 10, 12534–12543. [Google Scholar] [CrossRef] [PubMed]
- Weerathunge, P.; Ramanathan, R.; Torok, V.A.; Hodgson, K.; Xu, Y.; Goodacre, R.; Behera, B.K.; Bansal, V. Ultrasensitive Colorimetric Detection of Murine Norovirus Using NanoZyme Aptasensor. Anal. Chem. 2019, 91, 3270–3276. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Zeng, T.; Guo, W.J.; Bai, Y.Y.; Pang, D.W.; Zhang, Z.L. Digital single virus immunoassay for ultrasensitive mul-tiplex avian influenza virus detection based on fluorescent magnetic multifunctional nanospheres. ACS Appl. Mater. Interfaces 2019, 11, 5762–5770. [Google Scholar] [CrossRef]
- Cao, C.; Zhang, F.; Goldys, E.M.; Gao, F.; Liu, G. Advances in structure-switching aptasensing towards real time detection of cytokines. TrAC Trends Anal. Chem. 2018, 102, 379–396. [Google Scholar] [CrossRef]
- Ragan, I.K.; Davis, A.S.; McVey, D.S.; Richt, J.A.; Rowland, R.R.; Wilson, W.C. Evaluation of Fluorescence Microsphere Immunoassay for Detection of Antibodies to Rift Valley Fever Virus Nucleocapsid Protein and Glycoproteins. J. Clin. Microbiol. 2018, 56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ga, G.; Sizhu, S. Molecular Detection of Hepatitis E Virus in Tibetan Swine. Pak. J. Zool. 2020, 52, 1563–1569. [Google Scholar] [CrossRef]
- Chen, L.; Liu, W.; Zhang, Q.; Xu, K.; Ye, G.; Wu, W.; Mei, Y. RNA based mNGS approach identifies a novel human coro-navirus from two individual pneumonia cases in 2019 Wuhan outbreak. Emerg. Microbes Infect. 2020, 9, 313–319. [Google Scholar] [CrossRef]
- Roche’s Cobas SARS-CoV-2 Test to Detect Novel Coronavirus Receives FDA Emergency Use Authorization and Is Available in Markets Accepting the CE Mark. Available online: https://www.roche.com/dam/jcr:fcdc2329-235a-4010-86cd-a328c3e1db0a/en/13032020-mr-cobas-sar-cov-2-euaandceiv-en.pdf (accessed on 13 March 2020).
- Kam, K.-Q.; Yung, C.F.; Cui, L.; Lin, R.T.P.; Mak, T.M.; Maiwald, M.; Li, J.; Chong, C.Y.; Nadua, K.; Tan, N.W.H.; et al. A Well Infant with Coronavirus Disease 2019 with High Viral Load. Clin. Infect. Dis. 2020, 71, 847–849. [Google Scholar] [CrossRef]
- Park, G.-S.; Ku, K.; Baek, S.-H.; Kim, S.-J.; Kim, S.I.; Kim, B.-T.; Maeng, J.-S. Development of Reverse Transcription Loop-Mediated Isothermal Amplification Assays Targeting Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). J. Mol. Diagn. 2020, 22, 729–735. [Google Scholar] [CrossRef]
- Guo, L.; Sun, X.; Wang, X.; Liang, C.; Jiang, H.; Gao, Q.; Dai, M.; Qu, B.; Fang, S.; Mao, Y.; et al. SARS-CoV-2 detection with CRISPR diagnostics. Cell Discov. 2020, 6, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Xue, G.; Li, S.; Zhang, W.; Du, B.; Cui, J.; Yan, C.; Huang, L.; Chen, L.; Zhao, L.; Sun, Y.; et al. Reverse-Transcription Recombinase-Aided Amplification Assay for Rap-id Detection of the 2019 Novel Coronavirus (SARS-CoV-2). Anal. Chem. 2020, 92, 9699–9705. [Google Scholar] [CrossRef]
- Van Tan, L.; Man, D.N.H.; Hang, V.T.T.; Khanh, P.N.Q.; Xuan, T.C.; Phong, N.T.; Yen, L.M. SARS-CoV-2 and co-infections detection in nasopharyngeal throat swabs of COVID-19 patients by metagenomics. J. Infect. 2020, 81, e174–e175. [Google Scholar] [CrossRef]
- Wu, L.; Zhou, M.; Wang, Y.; Liu, J. Nanozyme and aptamer- based immunosorbent assay for aflatoxin B1. J. Hazard. Mater. 2020, 399, 123154. [Google Scholar] [CrossRef]
- Wu, L.; Zhang, M.; Zhu, L.; Li, J.; Li, Z.; Xie, W. Nanozyme-linked immunosorbent assay for porcine circovirus type 2 an-tibody using HAuCl4/H2O2 coloring system. Microchem. J. 2020, 157, 105079. [Google Scholar] [CrossRef]
- Li, Z.; Yi, Y.; Luo, X.; Xiong, N.; Liu, Y.; Li, S.; Zhang, Y. Development and clinical application of a rapid IgM-IgG com-bined antibody test for SARS-CoV-2 infection diagnosis. J. Med. Virol. 2020, 92, 1518–1524. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Zhang, Z.; Zhai, X.; Li, Y.; Lin, L.; Zhao, H.; Bian, L.; Li, P.; Yu, L.; Wu, Y.; et al. Rapid and Sensitive Detection of anti-SARS-CoV-2 IgG, Using Lanthanide-Doped Nanoparticles-Based Lateral Flow Immunoassay. Anal. Chem. 2020, 92, 7226–7231. [Google Scholar] [CrossRef] [PubMed]
- Roy, V.; Fischinger, S.; Atyeo, C.; Slein, M.; Loos, C.; Balazs, A.; Charles, R. SARS-CoV-2-specific ELISA development. J. Immunol. Methods 2020, 484, 112832. [Google Scholar] [CrossRef]
- Tré-Hardy, M.; Wilmet, A.; Beukinga, I.; Favresse, J.; Dogné, J.M.; Douxfils, J.; Blairon, L. Analytical and clinical validation of an ELISA for specific SARS-CoV-2 IgG, IgA, and IgM antibodies. J. Med. Virol. 2020, 93, 803–811. [Google Scholar] [CrossRef]
- Seo, G.; Lee, G.; Kim, M.J.; Baek, S.H.; Choi, M.; Ku, K.B.; Lee, C.S.; Jun, S.; Park, D.; Kim, H.G.; et al. Rapid detection of COVID-19 causative virus (SARS-CoV-2) in human nasopharyngeal swab specimens using field-effect transistor-based biosensor. ACS Nano 2020, 14, 5135–5142. [Google Scholar] [CrossRef] [Green Version]
- Baek, Y.H.; Um, J.; Antigua, K.J.C.; Park, J.H.; Kim, Y.; Oh, S.; Kim, Y.; Choi, W.S.; Kim, S.G.; Jeong, J.H.; et al. Development of a reverse transcrip-tion-loop-mediated isothermal amplification as a rapid early-detection method for novel SARS-CoV-2. Emerg. Microbes Infect. 2020, 9, 998–1007. [Google Scholar] [CrossRef] [Green Version]
- Wang, M.; Fu, A.; Hu, B.; Tong, Y.; Liu, R.; Liu, Z.; Shen, G. Nanopore targeted sequencing for the accurate and compre-hensive detection of SARS-CoV-2 and other respiratory viruses. Small 2020, 16, 2002169. [Google Scholar] [CrossRef]
- Moitra, P.; Alafeef, M.; Dighe, K.; Frieman, M.; Pan, D. Selective Naked-Eye Detection of SARS-CoV-2 Mediated by N Gene Targeted Antisense Oligonucleotide Capped Plasmonic Nanoparticles. ACS Nano 2020, 14, 7617–7627. [Google Scholar] [CrossRef]
- Becherer, L.; Borst, N.; Bakheit, M.; Frischmann, S.; Zengerle, R.; Von Stetten, F. Loop-mediated isothermal amplification (LAMP)—review and classification of methods for sequence-specific detection. Anal. Methods 2020, 12, 717–746. [Google Scholar] [CrossRef] [Green Version]
- Petherick, A. Developing antibody tests for SARS-CoV-2. Lancet 2020, 395, 1101–1102. [Google Scholar] [CrossRef]
- Long, Q.X.; Liu, B.Z.; Deng, H.J.; Wu, G.C.; Deng, K.; Chen, Y.K.; Huang, A.L. Antibody responses to SARS-CoV-2 in patients with COVID-19. Nat. Med. 2020, 26, 845–848. [Google Scholar] [CrossRef] [PubMed]
- Mak, G.C.; Cheng, P.K.; Lau, S.S.; Wong, K.K.; Lau, C.S.; Lam, E.T.; Tsang, D.N. Evaluation of rapid antigen test for detection of SARS-CoV-2 virus. J. Clin. Virol. 2020, 129, 104500. [Google Scholar] [CrossRef] [PubMed]
- Lassaunière, R.; Frische, A.; Harboe, Z.B.; Nielsen, A.C.; Fomsgaard, A.; Krogfelt, K.A.; Jørgensen, C.S. Evaluation of nine commercial SARS-CoV-2 immunoassays. MedRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Garg, M.; Sharma, A.L.; Singh, S. Advancement in biosensors for inflammatory biomarkers of SARS-CoV-2 during 2019–2020. Biosens. Bioelectron. 2020, 171, 112703. [Google Scholar] [CrossRef] [PubMed]
- Park, H.H.; Kim, H.N.; Kim, H.; Yoo, Y.; Shin, H.; Choi, E.Y.; Lee, W. Acetylated K676 TGFBIp as a severity diagnostic blood biomarker for SARS-CoV-2 pneumonia. Sci. Adv. 2020, 6, eabc1564. [Google Scholar] [CrossRef]





| Detection Methods | Pretreatment | Assay Time | Accuracy | Advantages | Disadvantages | References |
|---|---|---|---|---|---|---|
| Nucleic acid assay | Elution and concentration; extraction/ultra-filtration; organic flocculation; protease K and PEG precipitation | ≈1 to 6 h | >95% | High efficiency and sensitivity, easy to realize large-scale detection | Require professional technicians, high cost and time-consuming | [46,87] |
| Antibody detection | Elution and concentration; extraction/ultra-filtration | ≈15 min | >75% | Simple pretreatment and detection procedures, high sensitivity | Long window period, difficulty in early diagnosis | [88,89] |
| Antigen detection | Elution and concentration; centrifugation; extraction/ultra-filtration; | ≈30 min | 28.6%–81.8% | Simple operations, high selectivity, easy to be constructed | Lack of stability and relatively low sensitivity | [90,91] |
| Biomarker detection | Elution and concentration; centrifugation; extraction/ultra-filtration | ≈1 h | Not applicable | High sensitivity and selectivity, easy and little sampling | Difficult to obtain stable biomarkers, lack of standard | [92,93] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, W.; He, H.; Zhu, L.; Liu, G.; Wu, L. Food Safety in Post-COVID-19 Pandemic: Challenges and Countermeasures. Biosensors 2021, 11, 71. https://doi.org/10.3390/bios11030071
Zhang W, He H, Zhu L, Liu G, Wu L. Food Safety in Post-COVID-19 Pandemic: Challenges and Countermeasures. Biosensors. 2021; 11(3):71. https://doi.org/10.3390/bios11030071
Chicago/Turabian StyleZhang, Weimin, Huiyu He, Lin Zhu, Guozhen Liu, and Long Wu. 2021. "Food Safety in Post-COVID-19 Pandemic: Challenges and Countermeasures" Biosensors 11, no. 3: 71. https://doi.org/10.3390/bios11030071








