The Use of Biological Sensors and Instrumental Analysis to Discriminate COVID-19 Odor Signatures
Abstract
:1. Introduction
2. Materials and Methods
2.1. Collection of COVID-19 Samples
2.1.1. Approvals
2.1.2. Human Participant Recruitment and Follow-Up Health Survey
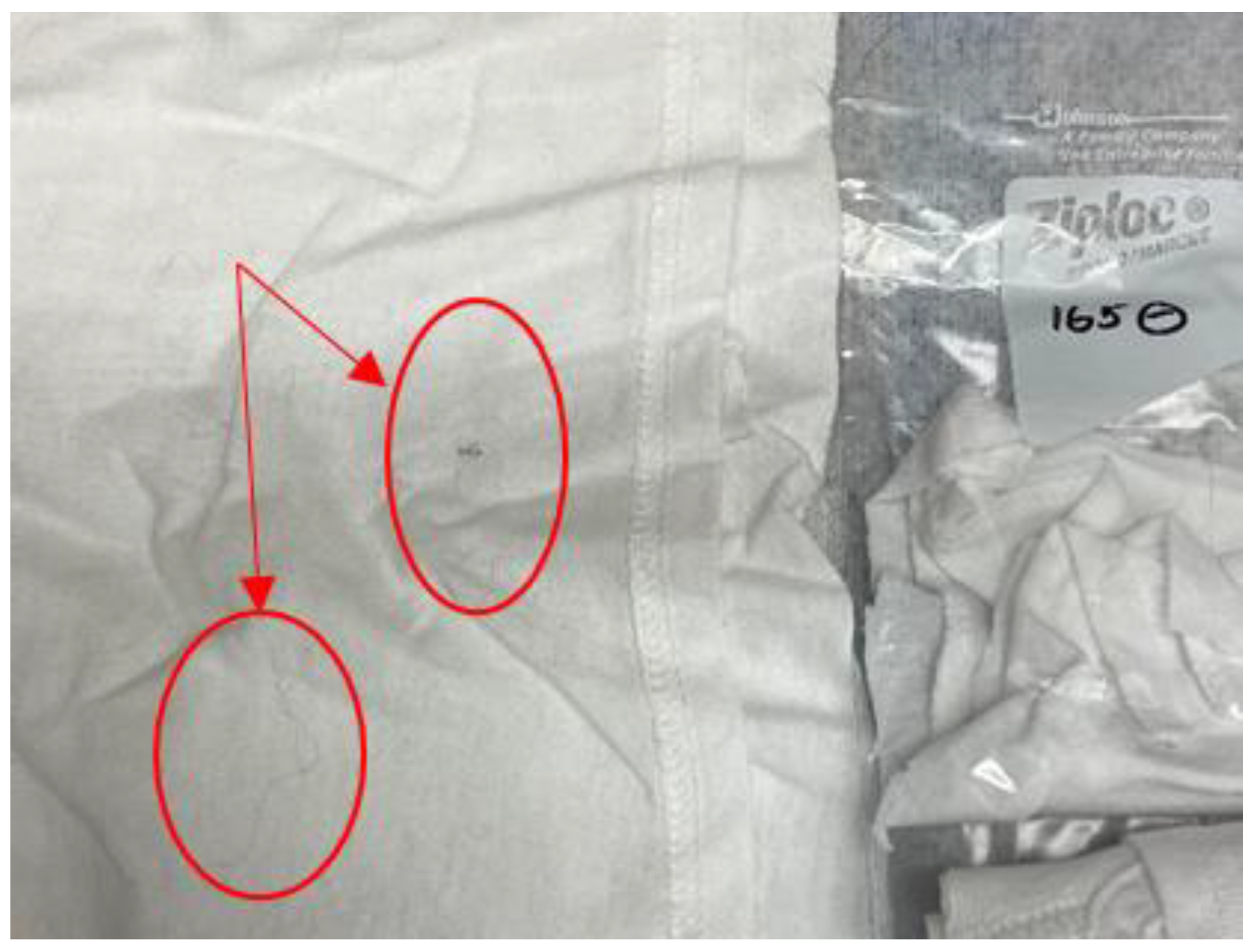
2.1.3. Preparation of Sample Collection Materials
2.1.4. Collected COVID-19 Positive and COVID-19 Negative T-Shirt Samples
2.2. Canine Odor Discrimination Methods
2.2.1. Canine Participants
2.2.2. Use of T-Shirt Samples in Training and Testing
2.2.3. Distractors
2.2.4. Training Procedure
2.2.5. Odor Learning Phase
2.2.6. Odor Learning Sessions on the Wheel
2.2.7. Training Phase 1
2.2.8. Training Phase 2–4
2.2.9. Test Phase
2.2.10. Behavioral Analysis
2.2.11. Statistical Analysis
2.3. HS-SPME-GC-MS Methods
2.3.1. Sample Set Demographics
2.3.2. HS-SPME-GC-MS Analysis Procedure
2.3.3. Statistical Analysis
2.3.4. Data Pre-Processing
3. Results
3.1. Canine Behavioral Coding Interrater Analysis
3.2. Canine Training Data
3.3. Testing Data
3.3.1. Factors Affecting Canine Behavior and Alert on Positive Samples
3.3.2. Factors Affecting Canine Behavior and Alert on Negative Samples
3.3.3. Factors Affecting Canine Behavior and Alert on Positive or Negative Samples
3.4. HS-SPME-GC-MS Results
Model Development
4. Discussion
4.1. Contrasts between Instrumental and Biological Methods Used for COVID-19 Positive/Negative Odor Discrimination
4.2. Limitations
4.3. Advantages and Disadvantages
4.4. Prospective Application of Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A
| COVID-19 Status/Presentation | Asymp. (+) | Symp. (+) | Asymp. (−) | Symp. (−) | |
|---|---|---|---|---|---|
| Race/ethnicity | Asian Or Asian American | - | 3 | 8 | 2 |
| Biracial | - | - | 1 | - | |
| Black Or African American | - | 1 | 2 | - | |
| Hispanic Or Latino | - | 3 | 11 | - | |
| Native Hawaiian or Other Pacific Islander | - | - | 1 | - | |
| White Or Caucasian | 9 | 69 | 141 | 33 | |
| Another race | - | 2 | 2 | 1 | |
| Not reported | - | 1 | 1 | 2 | |
| Identified gender | Female | 5 | 60 | 144 | 33 |
| Male | 4 | 19 | 21 | 5 | |
| Nonbinary/genderqueer | - | - | 2 | - | |
| Age group | 18–34 | 3 | 40 | 83 | 22 |
| 35–64 | 4 | 35 | 77 | 14 | |
| 65+ | 2 | 4 | 7 | 2 | |
| On medication? | Yes | 5 | 54 | 102 | 29 |
| No/NA | 4 | 24 | 64 | 9 | |
| NA | 0 | 1 | 1 | - | |
| Stress levels | 0–5 | 8 | 47 | 124 | 23 |
| 5–10 | 1 | 32 | 42 | 15 | |
| Unanswered | - | - | 1 | - | |
| Shared bed with another human? | Yes | 4 | 35 | 69 | 16 |
| No | 5 | 44 | 98 | 22 | |
| Shared bed with an animal? | Yes | 3 | 40 | 71 | 18 |
| No | 6 | 39 | 96 | 20 | |
| Total | 9 | 79 | 167 | 38 | |
| Sample Characteristic | Sample Categories | # of Correct Alerts from Above-Chance Dogs/ Total # of Times Samples with This Characteristic Were Seen by These Dogs |
|---|---|---|
| Gender | F M | 24/27 8/11 |
| Age | 25–34 35–44 45–54 55–65+ | 13/14 6/9 5/6 6/9 |
| Symptom count | 0 1–3 4–5 6–7 | 5/6 8/8 7/12 9/12 |
| Race/ethnicity | White Asian Hispanic African American | 20/23 5/6 3/6 2/3 |
| Bed shared with pet? | Yes No | 10/12 22/27 |
| Sample # | Test Used | Sample Status | Date Sample Placed in Collection Bag | Days until Sample Used in Earliest Test (Toby) | Days until Sample Used in Latest Test (Roxie) |
|---|---|---|---|---|---|
| 190 | Test 1 | negative | 10 September 20 | 168 | 229 |
| 284 | Test 1 | negative | 20 January 21 | 36 | 97 |
| 29 | Test 1 | negative | 19 September 20 | 159 | 220 |
| 208 | Test 1 | negative | 23 December 20 | 64 | 125 |
| 240 | Test 1 | negative | 6 January 21 | 50 | 111 |
| 218 | Test 1 | negative | 2 December 20 | 85 | 146 |
| 203 | Test 1 | negative | 27 November 20 | 90 | 151 |
| 3 | Test 1 | negative | 9 September 20 | 169 | 230 |
| 186 | Test 1 | negative | 3 July 20 | 237 | 298 |
| 268 | Test 1 | negative | 16 January 21 | 40 | 101 |
| 210 | Test 1 | negative | 15 December 20 | 72 | 133 |
| 69 | Test 1 | negative | 24 August 20 | 185 | 246 |
| 417 | Test 2 | negative | 2 February 21 | 35 | 93 |
| 28 | Test 2 | negative | 25 September 20 | 165 | 223 |
| 14 | Test 2 | negative | 13 August 20 | 208 | 266 |
| 90 | Test 2 | negative | 29 October 20 | 131 | 189 |
| 406 | Test 2 | negative | 31 January 21 | 37 | 95 |
| 261 | Test 2 | negative | 8 January 21 | 60 | 118 |
| 251 | Test 2 | negative | 12 January 21 | 66 | 124 |
| 273 | Test 2 | negative | 3 February 21 | 34 | 92 |
| 280 | Test 2 | negative | 19 January 21 | 49 | 107 |
| 452 | Test 2 | negative | 8 February 21 | 29 | 87 |
| 427 | Test 2 | negative | 16 February 21 | 21 | 79 |
| 453 | Test 2 | negative | 9 February 21 | 28 | 86 |
| 407 | Test 3 | negative | 28 January 21 | 54 | 110 |
| 426 | Test 3 | negative | 13 February 21 | 38 | 94 |
| 244 | Test 3 | negative | 16 December 20 | 97 | 153 |
| 271 | Test 3 | negative | 18 January 21 | 64 | 120 |
| 286 | Test 3 | negative | 21 January 21 | 61 | 117 |
| 162 | Test 3 | negative | 25 January 21 | 57 | 113 |
| 365 | Test 3 | negative | 19 February 21 | 32 | 88 |
| 290 | Test 3 | negative | 20 January 21 | 62 | 118 |
| 410 | Test 3 | negative | 4 February 21 | 47 | 103 |
| 308 | Test 3 | negative | 16 January 21 | 66 | 122 |
| 363 | Test 3 | negative | 16 February 21 | 35 | 91 |
| 341 | Test 3 | negative | 28 February 21 | 23 | 79 |
| 243 | Test 4 | negative | 20 January 21 | 77 | 128 |
| 292 | Test 4 | negative | 24 January 21 | 73 | 124 |
| 306 | Test 4 | negative | 13 January 21 | 84 | 135 |
| 344 | Test 4 | negative | 26 February 21 | 40 | 91 |
| 93 | Test 4 | negative | 10 November 20 | 148 | 199 |
| 192 | Test 4 | negative | 6 October 20 | 183 | 234 |
| 254 | Test 4 | negative | 11 January 21 | 86 | 137 |
| 287 | Test 4 | negative | 21 January 21 | 76 | 127 |
| 150 | Test 4 | negative | 30 December 20 | 98 | 149 |
| 129 | Test 4 | negative | 10 November 20 | 148 | 199 |
| 282 | Test 4 | negative | 20 January 21 | 77 | 128 |
| 236 | Test 4 | negative | 2 December 20 | 126 | 177 |
| 439 | Test 5 | negative | 9 March 21 | 84 | 145 |
| 437 | Test 5 | negative | 9 March 21 | 84 | 145 |
| 438 | Test 5 | negative | 10 March 21 | 83 | 144 |
| 515 | Test 5 | negative | 3 May 21 | 29 | 90 |
| 309 | Test 5 | negative | 18 January 21 | 134 | 195 |
| 291 | Test 5 | negative | 20 January 21 | 132 | 193 |
| 349 | Test 5 | negative | 16 March 21 | 77 | 138 |
| 355 | Test 5 | negative | 27 April 21 | 35 | 96 |
| 432 | Test 5 | negative | 26 February 21 | 95 | 156 |
| 316 | Test 5 | negative | 27 January 21 | 125 | 186 |
| 297 | Test 5 | negative | 22 January 21 | 130 | 191 |
| 508 | Test 5 | negative | 2 May 21 | 30 | 91 |
| 232 | Test 1 | positive | 18 November 20 | 99 | 160 |
| 223 | Test 1 | positive | 2 December 20 | 85 | 146 |
| 250 | Test 2 | positive | 1 January 21 | 67 | 128 |
| 113 | Test 2 | positive | 30 July 20 | 222 | 283 |
| 195 | Test 2 | positive | 10 November 20 | 119 | 180 |
| 146 | Test 3 | positive | 16 December 20 | 97 | 158 |
| 248 | Test 3 | positive | 11 December 20 | 102 | 163 |
| 312 | Test 3 | positive | 19 January 21 | 63 | 124 |
| 124 | Test 4 | positive | 10 September 20 | 209 | 270 |
| 262 | Test 4 | positive | 13 January 21 | 84 | 145 |
| 299 | Test 5 | positive | 1 January 21 | 151 | 212 |
| 108 | Test 5 | positive | 24 November 20 | 189 | 250 |
| 137 | Test 5 | positive | 30 November 20 | 183 | 244 |
References
- WHO. Coronavirus (COVID-19) Dashboard; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Jayaweera, M.; Perera, H.; Gunawardana, B.; Manatunge, J. Transmission of COVID-19 virus by droplets and aerosols: A critical review on the unresolved dichotomy. Environ. Res. 2020, 188, 109819. [Google Scholar] [CrossRef] [PubMed]
- Ali Rabaan, A.A.; Al-Ahmed, S.H.; Al-Malkey, M.; Alsubki, R.; Ezzikouri, S.; Al-Hababi, F.H.; Sah, R.; Al Mutair, A.; Alhumaid, S.; Al-Tawfiq, J.A.; et al. Airborne Transmission of SARS-CoV-2 is the Dominant Route of Transmission: Droplets and Aerosols. Le Infenzioni in Medicina. 2021, 29, 10–19. [Google Scholar]
- Geng, Y.; Wang, Y. Stability and transmissibility of SARS-CoV-2 in the environment. J. Med. Virol. 2022; 1–11, early view. [Google Scholar]
- Alene, M.; Yismaw, L.; Assemie, M.A.; Ketema, D.B.; Mengist, B.; Kassie, B.; Birhan, T.Y. Magnitude of asymptomatic COVID-19 cases throughout the course of infection: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0249090. [Google Scholar] [CrossRef]
- Salomon, J.A.; Reinhart, A.; Bilinski, A.; Chua, E.J.; La Motte-Ker, W.; Rönn, M.M.; Reitsma, M.B.; Morris, K.A.; LaRocca, S.; Farag, T.H.; et al. The US COVID-19 Trends and Impact Survey: Continuous real-time measurement of COVID-19 symptoms, risks, protective behaviors, testing, and vaccination. Proc. Natl. Acad. Sci. USA 2021, 118, e2111454118. [Google Scholar] [CrossRef]
- Zamani Rarani, F.; Zamani Rarani, M.; Hamblin, M.R.; Rashidi, B.; Hashemian, S.M.R.; Mirzaei, H. Comprehensive overview of COVID-19-related respiratory failure: Focus on cellular interactions. Cell Mol. Biol. Lett. 2022, 27, 63. [Google Scholar] [CrossRef] [PubMed]
- Shchendrygina, A.; Nagel, E.; Puntmann, V.O.; Valbuena-Lopez, S. COVID-19 myocarditis and prospective heart failure burden. Expert Rev. Cardiovasc. Ther. 2021, 19, 5–14. [Google Scholar] [CrossRef] [PubMed]
- Zafer, M.M.; El-Mahallawy, H.A.; Ashour, H.M. Severe COVID-19 and sepsis: Immune pathogenesis and laboratory markers. Microorganisms 2021, 9, 159. [Google Scholar] [CrossRef]
- Mouliou, D.S.; Gourgoulianis, K.I. False-positive and false-negative COVID-19 cases: Respiratory prevention and management strategies, vaccination, and further perspectives. Expert Rev. Respir. Med. 2021, 15, 993–1002. [Google Scholar] [CrossRef]
- West, C.P.; Montori, V.M.; Sampathkumar, P. COVID-19 testing: The threat of false-negative results. Mayo Clin. Proc. 2020, 95, 1127–1129. [Google Scholar] [CrossRef]
- Han, D.; Li, R.; Han, Y.; Zhang, R.; Li, J. COVID-19: Insight into the asymptomatic SARS-CoV-2 infection and transmission. Int. J. Biol. Sci. 2020, 16, 2803–2811. [Google Scholar] [CrossRef]
- Hardin, D.S.; Anderson, W.; Cattet, J. Dogs can be successfully trained to alert to hypoglycemia samples from patients with type 1 diabetes. Diabetes Ther. 2015, 6, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Buszewski, B.; Ligor, T.; Jezierski, T.; Wenda-Piesik, A.; Walczak, M.; Rudnicka, J. Identification of volatile lung cancer markers by gas chromatography-mass spectrometry: Comparison with discrimination by canines. Anal. Bioanal. Chem. 2012, 404, 141–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murarka, M.; Vesley-Gross, Z.I.; Essler, J.L.; Smith, P.G.; Hooda, G.; Drapkin, R.; Otto, C.M. Testing ovarian cancer cell lines to train dogs to detect ovarian cancer from blood plasma: A pilot study. J. Vet. Behav. 2019, 32, 42–48. [Google Scholar] [CrossRef]
- Kane, S.; Lee, Y.E.; Essler, J.L.; Mallikarjun, A.; Preti, G.; Plymouth, V.; Verta, A.; DeAngelo, A.; Otto, C.M. Canine discrimination of ovarian cancer through volatile organic compounds. Talanta 2022, 250, 123729. [Google Scholar] [CrossRef] [PubMed]
- Cornu, J.N.; Cancel-Tassin, G.; Ondet, V.; Girardet, C.; Cussenot, O. Olfactory detection of prostate cancer by dogs sniffing urine: A step forward in early diagnosis. Eur. Urol. 2011, 59, 197–201. [Google Scholar] [CrossRef]
- Koskinen, A.; Koskinen, H.; Bäck, L.; Saxen, H.; Klockars, T. A detection dog for paediatric urinary tract infection caused by Escherichia coli. Infect. Dis. 2017, 49, 874–877. [Google Scholar] [CrossRef]
- Eskandari, E.; Marzaleh, M.A.; Roudgari, H.; Farahani, R.H.; Nezami-Asl, A.; Laripour, R.; Aliyazdi, H.; Moghaddam, A.D.; Zibaseresht, R.; Akbarialiabad, H.; et al. Sniffer dogs as a screening/diagnostic tool for COVID-19: A proof of concept study. BMC Infect Dis. 2021, 21, 243, 1–8. [Google Scholar] [CrossRef]
- Essler, J.L.; Kane, S.A.; Nolan, P.; Akaho, E.H.; Berna, A.Z.; DeAngelo, A.; Berk, R.A.; Kaynaroglu, P.; Plymouth, V.; Frank, I.D.; et al. Discrimination of SARS-CoV-2 infected patient samples by detection dogs: A proof of concept study. PLoS ONE 2021, 16, e0250158. [Google Scholar] [CrossRef]
- Fathizadeh, H.; Taghizadeh, S.; Safari, R.; Khiabani, S.S.; Babak, B.; Hamzavi, F.; Ganbarov, K.; Esposito, S.; Zeinalzadeh, E.; Dao, S.; et al. Study presence of COVID-19 (SARS-CoV-2) in the sweat of patients infected with COVID-19. Microb. Pathog. 2020, 149, 104556. [Google Scholar] [CrossRef]
- Grandjean, D.; Sarkis, R.; Lecoq-Julien, C.; Benard, A.; Roger, V.; Levesque, E.; Bernes-Luciani, E.; Maestracci, B.; Morvan, P.; Gully, E.; et al. Can the detection dog alert on COVID-19 positive persons by sniffing axillary sweat samples? A proof-of-concept study. PLoS ONE 2020, 15, e0243122. [Google Scholar] [CrossRef]
- Jezierski, T.; Walczak, M.; Ligor, T.; Rudnicka, J.; Buszewski, B. Study of the art: Canine olfaction used for cancer detection on the basis of breath odour. Perspectives and limitations. J. Breath Res. 2015, 9, 027001. [Google Scholar] [CrossRef] [PubMed]
- Mendel, J.; Frank, K.; Edlin, L.; Hall, K.; Webb, D.; Mills, J.; Holness, H.K.; Furton, K.G.; Mills, D. Preliminary accuracy of COVID-19 odor detection by canines and HS-SPME-GC-MS using exhaled breath samples. Forensic Sci. Int. 2021, 3, 100155. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Qi, X.; Ma, J.; Zhang, C.; Feng, H.; Yao, M. Breath-borne VOC Biomarkers for COVID-19. medRxiv 2020. [Google Scholar] [CrossRef]
- Woollam, M.; Angarita-Rivera, P.; Siegel, A.P.; Kalra, V.; Kapoor, R.; Agarwal, M. Exhaled VOCs can discriminate subjects with COVID-19 from healthy controls. J. Breath Res. 2022, 16, 036002. [Google Scholar] [CrossRef] [PubMed]
- Broza, Y.Y.; Mochalski, P.; Ruzsanyi, V.; Amann, A.; Haick, H. Hybrid volatolomics and disease detection. Angew. Chem. 2015, 54, 11036–11048. [Google Scholar] [CrossRef] [PubMed]
- Giovannini, G.; Haick, H.; Garoli, D. Detecting COVID-19 from breath: A game changer for a big challenge. ACS Sens. 2021, 6, 1408–1417. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, W.; Cordell, R.L.; Wilde, M.J.; Richardson, M.; Carr, L.; Dasi, A.S.D.; Hargadon, B.; Free, R.C.; Monks, P.S.; Brightling, C.E.; et al. Diagnosis of covid-19 by exhaled breath analysis using gas chromatography–mass spectrometry. ERJ Open Res. 2021, 7, 1–10. [Google Scholar] [CrossRef]
- Leung, N.H.L.; Chu, D.K.W.; Shiu, E.Y.C.; Chan, K.H.; McDevitt, J.J.; Hau, B.J.P.; Yen, H.L.; Li, Y.; Ip, D.K.M.; Peiris, J.S.M.; et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 2020, 26, 676–680. [Google Scholar] [CrossRef] [Green Version]
- Ehsanifar, M. Airborne aerosols particles and COVID-19 transition. Environ. Res. 2021, 200, 111752. [Google Scholar] [CrossRef]
- Arslan, B.; Bercin, S.; Aydogan, S.; Islamogu, Y.; Dinc, B. SARS-CoV-2 is not found in the sweat of COVID-19 positive patients. Ir. J. Med. Sci. 2022, 191, 27–29. [Google Scholar] [CrossRef]
- Lamote, K.; Janssens, E.; Schillebeeckx, E.; Lapperre, T.S.; De Winter, B.Y.; van Meerbeeck, J.P. The scent of COVID-19: Viral (semi-)volatiles as fast diagnostic biomarkers? J. Breath Res. 2020, 14, 042001. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Chen, G.; Ye, N.; Kou, X.; Zhu, F.; Shen, J.; Ouyang, G. Solid-phase microextraction: An appealing alternative for the determination of endogenous substances—A review. Anal Chim Acta 2019, 1077, 67–86. [Google Scholar] [CrossRef] [PubMed]
- Harbourt, D.E.; Haddow, A.D.; Piper, A.E.; Bloomfield, H.; Kearney, B.J.; Fetterer, D.; Gibson, K.; Minogue, T. Modeling the stability of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) on skin, currency, and clothing. PLoS Negl. Trop. Dis. 2020, 14, e0008831. [Google Scholar] [CrossRef]
- Furton, K.G.; Beltz, K. Universal Detector Calibrant. US Patent 9250222, 2 February 2016. [Google Scholar]
- Mueller, M.M.; Palkovic, C.M.; Maynard, C.S. Errorless learning: Review and practical application for teaching children with pervasive developmental disorders. Psychol Sch. 2007, 44, 691–700. [Google Scholar] [CrossRef]
- Friard, O.; Gamba, M. BORIS: A free, versatile open-source event-logging software for video/audio coding and live observations. Methods Ecol. Evol. 2016, 7, 1325–1330. [Google Scholar] [CrossRef]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting linear mixed-effects models using lme4. J. Stat. Softw. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- Gokool, V.A.; Holness, H.K.; Furton, K.G. The influence of intra-personal variations in human hand odor on the determination of sample donor. Forensic Sci. Int. 2022, 334, 111235. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [Green Version]
- Angeletti, S.; Travaglino, F.; Spoto, S.; Pascarella, M.C.; Mansi, G.; De Cesaris, M.; Sartea, S.; Giovanetti, M.; Fogolari, M.; Plescia, D.; et al. COVID-19 sniffer dog experimental training: Which protocol and which implications for reliable sidentification? J. Med. Virol. 2021, 93, 5924–5930. [Google Scholar] [CrossRef]
- Chaber, A.; Hazel, S.; Matthews, B.; Withers, A.; Alvergnat, G.; Grandjean, D.; Caraguel, C. Evaluation of canine detection of COVID-19 infected individuals under controlled settings. Transbound Emerg. Dis. 2022, 69, e1951–e1958. [Google Scholar] [CrossRef]
- Grandjean, D.; Elie, C.; Gallet, C.; Julien, C.; Roger, V.; Desquilbet, L.; Alvergnat, A.; Delarue, S.; Gabassi, A.; Minier, M.; et al. Diagnostic accuracy of noninvasive detection of SARS-CoV-2 infection by canine olfaction. PLoS ONE 2022, 17, e0268382. [Google Scholar] [CrossRef] [PubMed]
- Gonder-Frederick, L.A.; Grabman, J.H.; Shepard, J.A.; Tripathi, A.V.; Ducar, D.M.; McElgunn, Z.R. Variability of Diabetes Alert Dog Accuracy in a Real-World Setting. J. Diabetes Sci. Technol. 2017, 11, 714–719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DeMatteo, K.E.; Davenport, B.; Wilson, L.E. Back to the basics with conservation detection dogs: Fundamentals for success. Wildl. Biol. 2019, 2019, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Sinn, D.L.; Gosling, S.D.; Hilliard, S. Personality and performance in military working dogs: Reliability and predictive validity of behavioral tests. Appl. Anim. Behav. Sci. 2010, 127, 51–65. [Google Scholar] [CrossRef]
- Sacharczuk, M.; Walczak, M.; Adamkiewicz, E.; Walasek, A.; Ensminger, J.; Presch, M.; Jezierski, T. Polymorphism of olfactory and neurotransmitters receptor genes in drug and explosives detection dogs can be associated with differences in detection performance. Appl. Anim. Behav. Sci. 2019, 215, 52–60. [Google Scholar] [CrossRef]
- Jamieson, L.T.J.; Baxter, G.S.; Murray, P.J. You are not my handler! impact of changing handlers on dogs’ behaviours and detection performance. Animals 2018, 8, 176. [Google Scholar] [CrossRef] [Green Version]
- Lit, L.; Schweitzer, J.B.; Oberbauer, A.M. Handler beliefs affect scent detection dog outcomes. Anim. Cogn. 2011, 14, 387–394. [Google Scholar] [CrossRef] [Green Version]
- Jiang, L.; Meng, D.; Yu, S.-I.; Lan, Z.; Shan, S.; Hauptmann, A.G. Self-paced learning with diversity. In Advances in Neural Information Processing Systems 27; Curran: Montreal, Canada, 2014; pp. 1–9. [Google Scholar]
- Angle, C.; Waggoner, L.P.; Ferrando, A.; Haney, P.; Passler, T. Canine detection of the volatilome: A review of implications for pathogen and disease detection. Front. Vet. Sci. 2016, 3, 47. [Google Scholar] [CrossRef]
- Hudson, D.T.; Curran, A.M.; Furton, K.G. The Stability of Collected Human Scent Under Various Environmental Conditions. J. Forensic Sci. 2009, 54, 1270–1277. [Google Scholar] [CrossRef]
- Kritikos, A.; Caruana, G.; Brouillet, R.; Miroz, J.-P.; Abed-Maillard, S.; Stieger, G.; Opota, O.; Croxatto, A.; Vollenweider, P.; Bart, P.-A.; et al. Sensitivity of Rapid Antigen Testing and RT-PCR Performed on Nasopharyngeal Swabs versus Saliva Samples in COVID-19 Hospitalized Patients: Results of a Prospective Comparative Trial (RESTART). Microorganisms 2021, 9, 1910. [Google Scholar] [CrossRef]
- Brihn, A.; Chang, J.; OYong, K.; Balter, S.; Terashita, D.; Rubin, Z.; Yeganeh, N. Diagnostic Performance of an Antigen Test with RT-PCR for the Detection of SARS-CoV-2 in a Hospital Setting—Los Angeles County, California, June–August 2020. Morb. Mortal. Wkly. Rep. 2021, 70, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Lefever, S.; Indevuyst, C.; Cuypers, L.; Dewaele, K.; Yin, N.; Cotton, F.; Padalko, E.; Oyaert, M.; Descy, J.; Cavalier, E.; et al. Comparison of the Quantitative DiaSorin Liaison Antigen Test to Reverse Transcription-PCR for the Diagnosis of COVID-19 in Symptomatic and Asymptomatic Outpatients. J. Clin. Microbiol. 2021, 59, e00374-21. [Google Scholar] [CrossRef] [PubMed]
- Devillier, P.; Gallet, C.; Salvator, H.; Lecoq-Julien, C.; Naline, E.; Roisse, D.; Levert, C.; Breton, E.; Galtat, A.; Decourtray, S.; et al. Biomedical detection dogs for the identification of SARS-CoV-2 infections from axillary sweat and breath samples **. J. Breath Res. 2022, 16, 037101. [Google Scholar] [CrossRef] [PubMed]
- Kantele, A.; Paajanen, J.; Turunen, S.; Pakkanen, S.H.; Patjas, A.; Itkonen, L.; Heiskanen, E.; Lappalainen, M.; Desquilbet, L.; Vapalahti, O.; et al. Scent dogs in detection of COVID-19: Triple-blinded randomised trial and operational real-life screening in airport setting. BMJ Glob. Health 2022, 7, e008024. [Google Scholar] [CrossRef]
- Mougang, Y.K.; Zazzo, L.D.; Minieri, M.; Capuano, R.; Catini, A.; Legramante, J.M.; Paolesse, R.; Bernardini, S.; Di Natale, C. Sensor array and gas chromatographic detection of the blood serum volatolomic signature of COVID-19. iScience 2021, 24, 102851. [Google Scholar] [CrossRef]
- Bordbar, M.; Samadinia, H.; Hajian, A.; Sheini, A.; Safaei, E.; Aboonajmi, J.; Arduini, F.; Sharghi, H.; Hashemi, P.; Khoshsafar, H.; et al. Mask assistance to colorimetric sniffers for detection of Covid-19 disease using exhaled breath metabolites. Sens. Actuators B Chem. 2022, 369, 132379. [Google Scholar] [CrossRef]
- Kny, E.; Reiner-Rozman, C.; Dostalek, J.; Hassel, A.-W.; Nöhammer, C.; Pfaffeneder-Mantai, F.; Szunerits, S.; Weber, V.; Knoll, W.; Kleber, C. State of the Art of Chemosensors in a Biomedical Context. Chemosensors 2022, 10, 199. [Google Scholar] [CrossRef]
- Fiebig, L.; Beyene, N.; Burny, R.; Fast, C.D.; Cox, C.; Mgode, G.F. From pests to tests: Training rats to diagnose tuberculosis. Eur. Respir. J. 2020, 55, 1902243. [Google Scholar] [CrossRef]






| Race/ Ethnicity | Identified Gender | COVID-19 Status/Presentation | Age Group | Shared Bed with | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Female | Male | NB/GQ | Asym. | Sym. | Neg. | 18–34 | 35–64 | 65+ | No One | Another Person | Person and Pet(s) | Pet(s) | UKN | |
| (+) | (+) | (-) | ||||||||||||
| Asian or Asian American | 12 | 1 | - | - | 3 | 10 | 11 | 2 | - | 5 | 5 | 2 | 1 | - |
| Biracial | 1 | - | - | - | - | 1 | - | 1 | - | - | - | - | 1 | - |
| Black or African American | 2 | 1 | - | - | 1 | 2 | 2 | 1 | - | 1 | - | - | 2 | - |
| Hispanic or Latino | 11 | 2 | 1 | - | 3 | 11 | 9 | 5 | - | 4 | 4 | 2 | 4 | - |
| Native Hawaiian or Other Pacific Islander | 1 | - | - | - | - | 1 | - | 1 | - | - | 1 | - | - | - |
| White or Caucasian | 206 | 45 | 1 | 9 | 69 | 174 | 120 | 118 | 14 | 82 | 70 | 36 | 62 | 2 |
| Another race | 5 | - | - | - | 2 | 3 | 4 | 1 | - | 2 | - | 1 | 2 | - |
| Not reported | 4 | - | - | - | 1 | 3 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | - |
| Total | 239 | 49 | 2 | 9 | 79 | 202 | 147 | 128 | 15 | 95 | 79 | 42 | 72 | 2 |
| Dog | Sex | Age (Years) | Breed | Previously Trained Odors |
|---|---|---|---|---|
| Griz | M | 6 | GSD | UDC, spotted lanternfly, Middle Eastern antiquities, live humans |
| Rico | M | 6 | GSD | UDC |
| Roxie | F | 6 | Labrador | UDC, narcotics, live humans |
| Toby | M | 3 | Small Munsterlander | UDC, spotted lanternfly, live humans |
| Tuukka | F | 7 | Husky/GSD mix | UDC |
| Phase | Holes in Negative Lid | Sensitivity Required to Advance | Specificity Required to Advance | Minimum # Sessions Required to Advance | # COVID-19 (+) Samples/Session | # COVID-19 (-) Samples/Session |
|---|---|---|---|---|---|---|
| Imprinting | 1 | 9/10 trials overall correct | 1 | 1 | 1 | |
| Phase 1 | 1 | 80% (5/6 correct) | 80% (10/12 correct) | 3 in a row | 2 | 4 |
| Phase 2 | 4 | 80% (5/6 correct) | 80% (10/12 correct) | 3 in a row | 2 | 4 |
| Phase 3 | 16 | 80% (5/6 correct) | 80% (10/12 correct) | 3 in a row | 2 | 4 |
| Phase 4 | Fully open | 80% (5/6 correct) | 80% (10/12 correct) | 3 in a row | 2 | 4 |
| Sensitivity = TP/(TP + FN) Rate of alert to positive samples Specificity = TN/(FP + TN) Rate of no alert to negative/blank samples | ||||||
| Race/ Ethnicity | Identified Gender | COVID-19 Status/Presentation | Age Group | Shared Bed With | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Female | Male | NB/GQ | Asymp. (+) | Sympt. (+) | Neg. (-) | 18–34 | 35–64 | 65+ | No One | Another Person | Person & Pet(s) | Pet(s) | |
| Asian or Asian American | 5 | - | - | - | 1 | 4 | 4 | 1 | - | 2 | 3 | - | - |
| Hispanic or Latino | 2 | 2 | 1 | - | 3 | 2 | 3 | 2 | - | 1 | 1 | 1 | 2 |
| White or Caucasian | 100 | 25 | 0 | 3 | 37 | 85 | 58 | 57 | 10 | 36 | 36 | 19 | 34 |
| Another Race | 2 | - | - | 1 | 1 | 2 | - | - | 1 | - | 1 | - | |
| Not Reported | - | - | - | 7 *× | 4 × | - | - | - | - | - | - | - | |
| Total | 109 | 27 | 1 | 3 | 49 | 96 | 67 | 60 | 10 | 40 | 40 | 21 | 36 |
| Dog | Sensitivity | Specificity |
|---|---|---|
| Griz | 11/12 * (91.7%) | 51/56 * (91.1%) |
| Toby | 11/13 (84.6%) | 59/60 (98.3%) |
| Tuukka | 9/13 (69.2%) | 55/60 (91.6%) |
| Rico | 5/13 (38.5%) | 56/60 (93.3%) |
| Roxie | 4/13 (30.8%) | 46/60 (76.6%) |
| Trial | # of Dogs who Correctly Alerted | # Correctly Alerted, above Chance Dogs | Gender | Age | SymptomCount | Race/ Ethnicity | Bed Shared with Pet? |
|---|---|---|---|---|---|---|---|
| 1 | 2/5 4/5 | 2/3 2/3 | F M | 45–54 35–44 | 5 5 | White Hispanic | No Yes, 1 dog |
| 2 | 4/5 3/5 3/5 | 3/3 1/3 2/3 | F F M | 25–34 35–44 55–64 | 3 6 5 | White Hispanic White | No Yes, 1 cat No |
| 3 | 3/5 3/5 4/5 | 2/3 3/3 2/3 | F F F | 25–34 25–34 55–64 | 4 0 7 | Asian White African American | No No Yes, 1 or more dogs |
| 4 | 2/5 3/5 | 2/3 3/3 | M F | 65+ 25–34 | 0 7 | White Asian | No No |
| 5 | 3/4 4/5 3/5 | 2/2 3/3 3/3 | M F F | 25–34 45–54 35–44 | 3 1 7 | White White White | No No Yes, 1 or more cats |
| Detection Method | Sample Medium | Average Specificity and/or Sensitivity | Reference |
|---|---|---|---|
| RT-PCR | Nasopharyngeal swab | 98% sensitivity 100% specificity | [54] |
| Saliva | 69% sensitivity 100% specificity | [54] | |
| Antigen test | Nasal swab | 72.1% sensitivity 98.7% specificity | [55] |
| Nasopharyngeal | 65.7% sensitivity 100% specificity | [56] | |
| Canine screening | Breath— face masks | 83.1% sensitivity 88.6% specificity | [57] |
| Face masks and clothes | 86% sensitivity 92.9% specificity | [19] | |
| Skin swab | 92% sensitivity 91% specificity | [58] | |
| Axillary sweat | 97% sensitivity 91% specificity | [44] | |
| Axillary sweat | 89.6% sensitivity 83.9%specificity | [57] | |
| Body odor—T-shirts (including axillary sweat) | 63% sensitivity 90% specificity | Current study | |
| HS-SPME-GC-MS | Body odor—T-shirts (including axillary sweat) | 100% sensitivity 100% specificity | Current study |
| SPME-GC-MS | Blood serum | 94% sensitivity 83% specificity | [59] |
| Quartz microbalance | Blood serum | 94% sensitivity 80% specificity | [59] |
| Colorimetric paper sensor | Breath | 78.3% sensitivity 83.6% specificity | [60] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gokool, V.A.; Crespo-Cajigas, J.; Mallikarjun, A.; Collins, A.; Kane, S.A.; Plymouth, V.; Nguyen, E.; Abella, B.S.; Holness, H.K.; Furton, K.G.; et al. The Use of Biological Sensors and Instrumental Analysis to Discriminate COVID-19 Odor Signatures. Biosensors 2022, 12, 1003. https://doi.org/10.3390/bios12111003
Gokool VA, Crespo-Cajigas J, Mallikarjun A, Collins A, Kane SA, Plymouth V, Nguyen E, Abella BS, Holness HK, Furton KG, et al. The Use of Biological Sensors and Instrumental Analysis to Discriminate COVID-19 Odor Signatures. Biosensors. 2022; 12(11):1003. https://doi.org/10.3390/bios12111003
Chicago/Turabian StyleGokool, Vidia A., Janet Crespo-Cajigas, Amritha Mallikarjun, Amanda Collins, Sarah A. Kane, Victoria Plymouth, Elizabeth Nguyen, Benjamin S. Abella, Howard K. Holness, Kenneth G. Furton, and et al. 2022. "The Use of Biological Sensors and Instrumental Analysis to Discriminate COVID-19 Odor Signatures" Biosensors 12, no. 11: 1003. https://doi.org/10.3390/bios12111003
APA StyleGokool, V. A., Crespo-Cajigas, J., Mallikarjun, A., Collins, A., Kane, S. A., Plymouth, V., Nguyen, E., Abella, B. S., Holness, H. K., Furton, K. G., Johnson, A. T. C., & Otto, C. M. (2022). The Use of Biological Sensors and Instrumental Analysis to Discriminate COVID-19 Odor Signatures. Biosensors, 12(11), 1003. https://doi.org/10.3390/bios12111003








