Microfluidic Devices for HIV Diagnosis and Monitoring at Point-of-Care (POC) Settings
Abstract
1. Introduction
2. HIV, CD4+ T Cells, and AIDs
3. Sample Preparation: A Major Challenge for HIV Testing
4. Microfluidic Devices for Point-of-Care Applications
4.1. Polymerase Chain Reaction (PCR)-Based Devices
4.2. Isothermal Amplification-Based Devices
4.2.1. Loop-Mediated Isothermal Amplification Devices
4.2.2. Recombinase Polymerase Amplification
4.3. ELISA
4.4. ELISA Alternatives
| Method | Advantages | Disadvantages | References |
|---|---|---|---|
| LAMP/RT-LAMP | No thermal cycler needed, isothermal cycling, inexpensive ($9.98–$28.34), highly specific, alternate power sources (magnesium oxidation), rapid testing, 4–6 primers used | Lower sensitivity than qPCR, multiple steps for preparation, potential contamination as sample is prepared off-chip, difficulty in multiplexing | [64,65,113] |
| PCR/RT-PCR | Highly sensitive (>99%) and specific (>98%), can include fluorophores, fast thermal cycling | Thermal cyclers are expensive ($17,000–$25,000), requires a trained technician for benchtop apparatus, off-chip sample preparation, long wait time (hours–days) | [47,52,53,54] |
| RPA/RT-RPA | No thermal cycler needed, can include fluorophores, minimal sample preparation, rapid, highly sensitive (97.7%) and specific, reagents can be stored for up to 3 months at 25 °C, 2–3 primers used, affordable ($4.45) | Precise control of amplification is necessary, risk of photobleaching of probes, risk of contamination with ICS-RPA | [33,71,75,76,77] |
| ELISA | Highly sensitive (100%) and specific (>99.5%), portable, reliable results, can include fluorescent conjugates, can be utilized in cell counting | Benchtop has a long wait time (days) to obtain results, antibodies can be expensive to purchase | [80,83,84,85,88] |
| P-ELISA | Affordable, small reagent volumes, simple equipment, results in under an hour, capable of multiplexing | Less sensitive (10× lower) than normal ELISA, sensitivity and specificity vary between devices, reagents can be evaporated during transport | [98,99,103] |
| HOLMES | Detect HIV p24 as low as 10 aM, rapid, works on proteins and nucleic acids | Antibodies can be expensive to purchase, fluorescent microscope needed if using fluorescent labels | [105] |
| µWestern Blot | Rapid, include fluorescent antibodies, multiplexing, small reagent volumes | Antibodies can be expensive to purchase, smaller pore size can cause large antibody probes to be immobilized irreversibly | [109] |
| POCKET Immunoassay | Sensitive, affordable, antibodies conjugated to gold catalyze the reaction, reusable | Manual pipetting into the microwells poses a risk for contamination | [106] |
| Smartphone-based Detection | Replaces need for thermocycler or microscopes, can interface with microfluidic chips, affordable assays, powerful imaging, data analysis through applications, highly sensitive | Privacy and security concerns when storing medical data on applications, manual functionalization can result in chip-to-chip variability, manual pipetting has a risk for contamination | [114,115,116,117] |
5. Smartphone-Based Devices
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Boasso, A.; Shearer, G.; Chougnet, C. Immune dysregulation in human immunodeficiency virus infection: Know it, fix it, prevent it? J. Intern. Med. 2009, 265, 78–96. [Google Scholar] [CrossRef] [PubMed]
- Merson, M.H. The HIV–AIDS pandemic at 25—The global response. N. Eng. J. Med. 2006, 354, 2414–2417. [Google Scholar] [CrossRef] [PubMed]
- Rana, A.I.; Castillo-Mancilla, J.R.; Tashima, K.T.; Landovitz, R.L. Advances in long-acting agents for the treatment of HIV infection. Drugs 2020, 80, 535–545. [Google Scholar] [CrossRef] [PubMed]
- UNAIDS. Global HIV & AIDS Statistics—2020 Fact Sheet. Available online: http://www.unaids.org/en/resources/fact-sheet (accessed on 27 April 2022).
- Blood, G.A.C. Human immunodeficiency virus (HIV). Transfus. Med. Hemother. 2016, 43, 203. [Google Scholar]
- Ghys, P.D.; Fransen, K.; Diallo, M.O.; Ettiègne-Traoré, V.; Coulibaly, I.-M.; Yeboué, K.M.; Kalish, M.L.; Maurice, C.; Whitaker, J.P.; Greenberg, A.E. The associations between cervicovaginal HIV shedding, sexually transmitted diseases and immunosuppression in female sex workers in Abidjan, Cote d’Ivoire. Aids 1997, 11, F85–F93. [Google Scholar] [CrossRef]
- VAN DER LOEFF, M.S.; Aaby, P. Towards a better understanding of the epidemiology of HIV-2. AIDS 1999, 13, S69–S84. [Google Scholar]
- Soriano, V.; Gomes, P.; Heneine, W.; Holguín, A.; Doruana, M.; Antunes, R.; Mansinho, K.; Switzer, W.M.; Araujo, C.; Shanmugam, V. Human immunodeficiency virus type 2 (HIV-2) in Portugal: Clinical spectrum, circulating subtypes, virus isolation, and plasma viral load. J. Med. Virol. 2000, 61, 111–116. [Google Scholar] [CrossRef]
- Camacho-Gonzalez, A.F.; Wallins, A.; Toledo, L.; Murray, A.; Gaul, Z.; Sutton, M.Y.; Gillespie, S.; Leong, T.; Graves, C.; Chakraborty, R. Risk factors for HIV transmission and barriers to HIV disclosure: Metropolitan Atlanta youth perspectives. AIDS Patient Care STDs 2016, 30, 18–24. [Google Scholar] [CrossRef]
- Johnson, A.S.; Hall, H.I.; Hu, X.; Lansky, A.; Holtgrave, D.R.; Mermin, J. Trends in diagnoses of HIV infection in the United States, 2002–2011. JAMA 2014, 312, 432–434. [Google Scholar] [CrossRef]
- Prejean, J.; Song, R.; Hernandez, A.; Ziebell, R.; Green, T.; Walker, F.; Lin, L.S.; An, Q.; Mermin, J.; Lansky, A. Estimated HIV incidence in the United States, 2006–2009. PLoS ONE 2011, 6, e17502. [Google Scholar] [CrossRef]
- Pellowski, J.A.; Kalichman, S.C.; Matthews, K.A.; Adler, N. A pandemic of the poor: Social disadvantage and the US HIV epidemic. Am. Psychol. 2013, 68, 197. [Google Scholar] [CrossRef] [PubMed]
- Türmen, T. Gender and HIV/aids. Int. J. Gynecol. Obstet. 2003, 82, 411–418. [Google Scholar] [CrossRef]
- Heckman, T.G.; Somlai, A.; Peters, J.; Walker, J.; Otto-Salaj, L.; Galdabini, C.; Kelly, J. Barriers to care among persons living with HIV/AIDS in urban and rural areas. AIDS Care 1998, 10, 365–375. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, S.; Kadiyala, S.; Greener, R. Is poverty or wealth driving HIV transmission? Aids 2007, 21, S5–S16. [Google Scholar] [CrossRef]
- Mishra, V.; Bignami-Van Assche, S.; Greener, R.; Vaessen, M.; Hong, R.; Ghys, P.D.; Boerma, J.T.; Van Assche, A.; Khan, S.; Rutstein, S. HIV infection does not disproportionately affect the poorer in sub-Saharan Africa. AIDS 2007, 21, S17–S28. [Google Scholar] [CrossRef]
- Chin, C.D.; Linder, V.; Sia, S.K. Commercialization of microfluidic point-of-care diagnostic devices. Lab Chip 2012, 12, 2118–2134. [Google Scholar] [CrossRef]
- Wu, G.; Zaman, M.H. Low-cost tools for diagnosing and monitoring HIV infection in low-resource settings. Bull. World Health Organ. 2012, 90, 914–920. [Google Scholar] [CrossRef]
- Calmy, A.; Ford, N.; Hirschel, B.; Reynolds, S.J.; Lynen, L.; Goemaere, E.; De La Vega, F.G.; Perrin, L.; Rodriguez, W. HIV viral load monitoring in resource-limited regions: Optional or necessary? Clin. Infect. Dis. 2007, 44, 128–134. [Google Scholar] [CrossRef]
- Mtapuri-Zinyowera, S.; Chideme, M.; Mangwanya, D.; Mugurungi, O.; Gudukeya, S.; Hatzold, K.; Mangwiro, A.; Bhattacharya, G.; Lehe, J.; Peter, T. Evaluation of the PIMA point-of-care CD4 analyzer in VCT clinics in Zimbabwe. JAIDS J. Acquir. Immune Defic. Syndr. 2010, 55, 1–7. [Google Scholar] [CrossRef]
- Ganser-Pornillos, B.K.; Yeager, M.; Sundquist, W.I. The structural biology of HIV assembly. Curr. Opin. Struct. Biol. 2008, 18, 203–217. [Google Scholar] [CrossRef]
- Doitsh, G.; Greene, W.C. Dissecting how CD4 T cells are lost during HIV infection. Cell Host Microbe 2016, 19, 280–291. [Google Scholar] [CrossRef] [PubMed]
- Doitsh, G.; Galloway, N.L.; Geng, X.; Yang, Z.; Monroe, K.M.; Zepeda, O.; Hunt, P.W.; Hatano, H.; Sowinski, S.; Muñoz-Arias, I. Cell death by pyroptosis drives CD4 T-cell depletion in HIV-1 infection. Nature 2014, 505, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Swingler, S.; Mann, A.; Jacque, J.-M.; Brichacek, B.; Sasseville, V.; Williams, K.; Lackner, A.; Janoff, E.; Wang, R.; Fisher, D. HIV-1 Nef mediates lymphocyte chemotaxis and activation by infected macrophages. Nat. Med. 1999, 5, 997–1003. [Google Scholar] [CrossRef] [PubMed]
- Yates, A.; Stark, J.; Klein, N.; Antia, R.; Callard, R. Understanding the slow depletion of memory CD4+ T cells in HIV infection. PLoS Med. 2007, 4, e177. [Google Scholar] [CrossRef]
- Belaunzarán-Zamudio, P.F.; Caro-Vega, Y.N.; Shepherd, B.E.; Rebeiro, P.F.; Crabtree-Ramírez, B.E.; Cortes, C.P.; Grinsztejn, B.; Gotuzzo, E.; Mejia, F.; Padgett, D. The population impact of late presentation with advanced HIV disease and delayed antiretroviral therapy in adults receiving HIV care in Latin America. Am. J. Epidemiol. 2020, 189, 564–572. [Google Scholar] [CrossRef]
- Rice, B.; Boulle, A.; Schwarcz, S.; Shroufi, A.; Rutherford, G.; Hargreaves, J. The continuing value of CD4 cell count monitoring for differential HIV care and surveillance. JMIR Public Health Surveill. 2019, 5, e11136. [Google Scholar] [CrossRef] [PubMed]
- Prakash, O.; Pankey, G. HIV eradication: Progress and challenges. Ochsner J. 2001, 3, 98–101. [Google Scholar]
- Zhang, J.L.; Crumpacker, C. Eradication of HIV and Cure of AIDS, Now and How? Front. Immunol. 2013, 4, 337. [Google Scholar] [CrossRef]
- Chun, T.-W.; Moir, S.; Fauci, A.S. HIV reservoirs as obstacles and opportunities for an HIV cure. Nat. Immunol. 2015, 16, 584–589. [Google Scholar] [CrossRef]
- Finzi, D.; Hermankova, M.; Pierson, T.; Carruth, L.M.; Buck, C.; Chaisson, R.E.; Quinn, T.C.; Chadwick, K.; Margolick, J.; Brookmeyer, R. Identification of a reservoir for HIV-1 in patients on highly active antiretroviral therapy. Science 1997, 278, 1295–1300. [Google Scholar] [CrossRef]
- Hill, A.L.; Rosenbloom, D.I.; Fu, F.; Nowak, M.A.; Siliciano, R.F. Predicting the outcomes of treatment to eradicate the latent reservoir for HIV-1. Proc. Natl. Acad. Sci. USA 2014, 111, 13475–13480. [Google Scholar] [CrossRef] [PubMed]
- Crannell, Z.A.; Rohrman, B.; Richards-Kortum, R. Quantification of HIV-1 DNA using real-time recombinase polymerase amplification. Anal. Chem. 2014, 86, 5615–5619. [Google Scholar] [CrossRef] [PubMed]
- Glass, T.R.; Sterne, J.A.; Schneider, M.-P.; De Geest, S.; Nicca, D.; Furrer, H.; Günthard, H.F.; Bernasconi, E.; Calmy, A.; Rickenbach, M. Self-reported nonadherence to antiretroviral therapy as a predictor of viral failure and mortality. Aids 2015, 29, 2195–2200. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Xu, F.; Demirci, U. Advances in developing HIV-1 viral load assays for resource-limited settings. Biotechnol. Adv. 2010, 28, 770–781. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Kabir, M.A.; Asghar, W. Lab-on-a-chip zika detection with reverse transcription Loop-mediated isothermal amplification–based assay for point-of-care settings. Arch. Pathol. Lab. Med. 2020, 144, 1335–1343. [Google Scholar] [CrossRef]
- Phillips, E.A.; Moehling, T.J.; Ejendal, K.F.; Hoilett, O.S.; Byers, K.M.; Basing, L.A.; Jankowski, L.A.; Bennett, J.B.; Lin, L.-K.; Stanciu, L.A. Microfluidic rapid and autonomous analytical device (microRAAD) to detect HIV from whole blood samples. Lab Chip 2019, 19, 3375–3386. [Google Scholar] [CrossRef]
- Coarsey, C.; Coleman, B.; Kabir, M.A.; Sher, M.; Asghar, W. Development of a flow-free magnetic actuation platform for an automated microfluidic ELISA. RSC Adv. 2019, 9, 8159–8168. [Google Scholar] [CrossRef]
- Liu, T.; Choi, G.; Tang, Z.; Kshirsagar, A.; Politza, A.J.; Guan, W. Fingerpick Blood-Based Nucleic Acid Testing on A USB Interfaced Device towards HIV self-testing. Biosens. Bioelectron. 2022, 209, 114255. [Google Scholar] [CrossRef]
- Safavieh, M.; Kaul, V.; Khetani, S.; Singh, A.; Dhingra, K.; Kanakasabapathy, M.K.; Draz, M.S.; Memic, A.; Kuritzkes, D.R.; Shafiee, H. Paper microchip with a graphene-modified silver nano-composite electrode for electrical sensing of microbial pathogens. Nanoscale 2017, 9, 1852–1861. [Google Scholar] [CrossRef]
- Choi, J.R.; Hu, J.; Tang, R.; Gong, Y.; Feng, S.; Ren, H.; Wen, T.; Li, X.; Abas, W.A.B.W.; Pingguan-Murphy, B. An integrated paper-based sample-to-answer biosensor for nucleic acid testing at the point of care. Lab Chip 2016, 16, 611–621. [Google Scholar] [CrossRef]
- Kabir, M.A.; Zilouchian, H.; Caputi, M.; Asghar, W. Advances in HIV diagnosis and monitoring. Crit. Rev. Biotechnol. 2020, 40, 623–638. [Google Scholar] [CrossRef] [PubMed]
- Muzammil, I.; Aqib, A.I.; Tanveer, Q.; Muzmmal, S.; Naseer, M.A.; Tahir, M. COVID-19 diagnosis—Myths and protocols. In Data Science for COVID-19; Elsevier: Amsterdam, The Netherlands, 2022; pp. 335–353. [Google Scholar]
- Abdallah, B.; Ros, A. Surface coatings for microfluidic-based biomedical devices. In Microfluidic Devices for Biomedical Applications; Elsevier: Amsterdam, The Netherlands, 2013; pp. 63–99. [Google Scholar]
- Mauk, M.; Song, J.; Bau, H.H.; Gross, R.; Bushman, F.D.; Collman, R.G.; Liu, C. Miniaturized devices for point of care molecular detection of HIV. Lab Chip 2017, 17, 382–394. [Google Scholar] [CrossRef] [PubMed]
- Root, B.E.; Agarwal, A.K.; Kelso, D.M.; Barron, A.E. Purification of HIV RNA from serum using a polymer capture matrix in a microfluidic device. Anal. Chem. 2011, 83, 982–988. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Kim, S.-W.; Kang, J.Y.; Ahn, C.H. A polymer lab-on-a-chip for reverse transcription (RT)-PCR based point-of-care clinical diagnostics. Lab Chip 2008, 8, 2121–2127. [Google Scholar] [CrossRef]
- Hashimoto, M.; Chen, P.-C.; Mitchell, M.W.; Nikitopoulos, D.E.; Soper, S.A.; Murphy, M.C. Rapid PCR in a continuous flow device. Lab Chip 2004, 4, 638–645. [Google Scholar] [CrossRef]
- Hataoka, Y.; Zhang, L.; Mori, Y.; Tomita, N.; Notomi, T.; Baba, Y. Analysis of specific gene by integration of isothermal amplification and electrophoresis on poly (methyl methacrylate) microchips. Anal. Chem. 2004, 76, 3689–3693. [Google Scholar] [CrossRef]
- Thorsen, T.; Maerkl, S.J.; Quake, S.R. Microfluidic large-scale integration. Science 2002, 298, 580–584. [Google Scholar] [CrossRef]
- Park, S.; Zhang, Y.; Lin, S.; Wang, T.-H.; Yang, S. Advances in microfluidic PCR for point-of-care infectious disease diagnostics. Biotechnol. Adv. 2011, 29, 830–839. [Google Scholar] [CrossRef]
- Bu, M.; Melvin, T.; Ensell, G.; Wilkinson, J.S.; Evans, A.G. Design and theoretical evaluation of a novel microfluidic device to be used for PCR. J. Micromech. Microeng. 2003, 13, S125. [Google Scholar] [CrossRef]
- Murtagh, M. UNITAIDS Technical Report: HIV/AIDS Diagnostic Landscape; World Health Organisation: Geneva, Switzerland, 2011. [Google Scholar]
- Jangam, S.R.; Agarwal, A.K.; Sur, K.; Kelso, D.M. A point-of-care PCR test for HIV-1 detection in resource-limitedsettings. Biosens. Bioelectron. 2013, 42, 69–75. [Google Scholar] [CrossRef]
- Cai, S.; Jung, C.; Bhadra, S.; Ellington, A.D. Phosphorothioated primers lead to loop-mediated isothermal amplification at low temperatures. Anal. Chem. 2018, 90, 8290–8294. [Google Scholar] [CrossRef] [PubMed]
- Nzelu, C.O.; Kato, H.; Peters, N.C. Loop-mediated isothermal amplification (LAMP): An advanced molecular point-of-care technique for the detection of Leishmania infection. PLoS Neglected Trop. Dis. 2019, 13, e0007698. [Google Scholar] [CrossRef] [PubMed]
- Keikha, M. LAMP method as one of the best candidates for replacing with PCR method. Malays. J. Med. Sci. 2018, 25, 121–123. [Google Scholar] [CrossRef] [PubMed]
- Thi, V.L.D.; Herbst, K.; Boerner, K.; Meurer, M.; Kremer, L.P.; Kirrmaier, D.; Freistaedter, A.; Papagiannidis, D.; Galmozzi, C.; Stanifer, M.L. A colorimetric RT-LAMP assay and LAMP-sequencing for detecting SARS-CoV-2 RNA in clinical samples. Sci. Transl. Med. 2020, 12, 556. [Google Scholar]
- Huang, W.E.; Lim, B.; Hsu, C.C.; Xiong, D.; Wu, W.; Yu, Y.; Jia, H.; Wang, Y.; Zeng, Y.; Ji, M. RT-LAMP for rapid diagnosis of coronavirus SARS-CoV-2. Microb. Biotechnol. 2020, 13, 950–961. [Google Scholar] [CrossRef]
- Ocwieja, K.E.; Sherrill-Mix, S.; Liu, C.; Song, J.; Bau, H.; Bushman, F.D. A reverse transcription loop-mediated isothermal amplification assay optimized to detect multiple HIV subtypes. PLoS ONE 2015, 10, e0117852. [Google Scholar] [CrossRef] [PubMed]
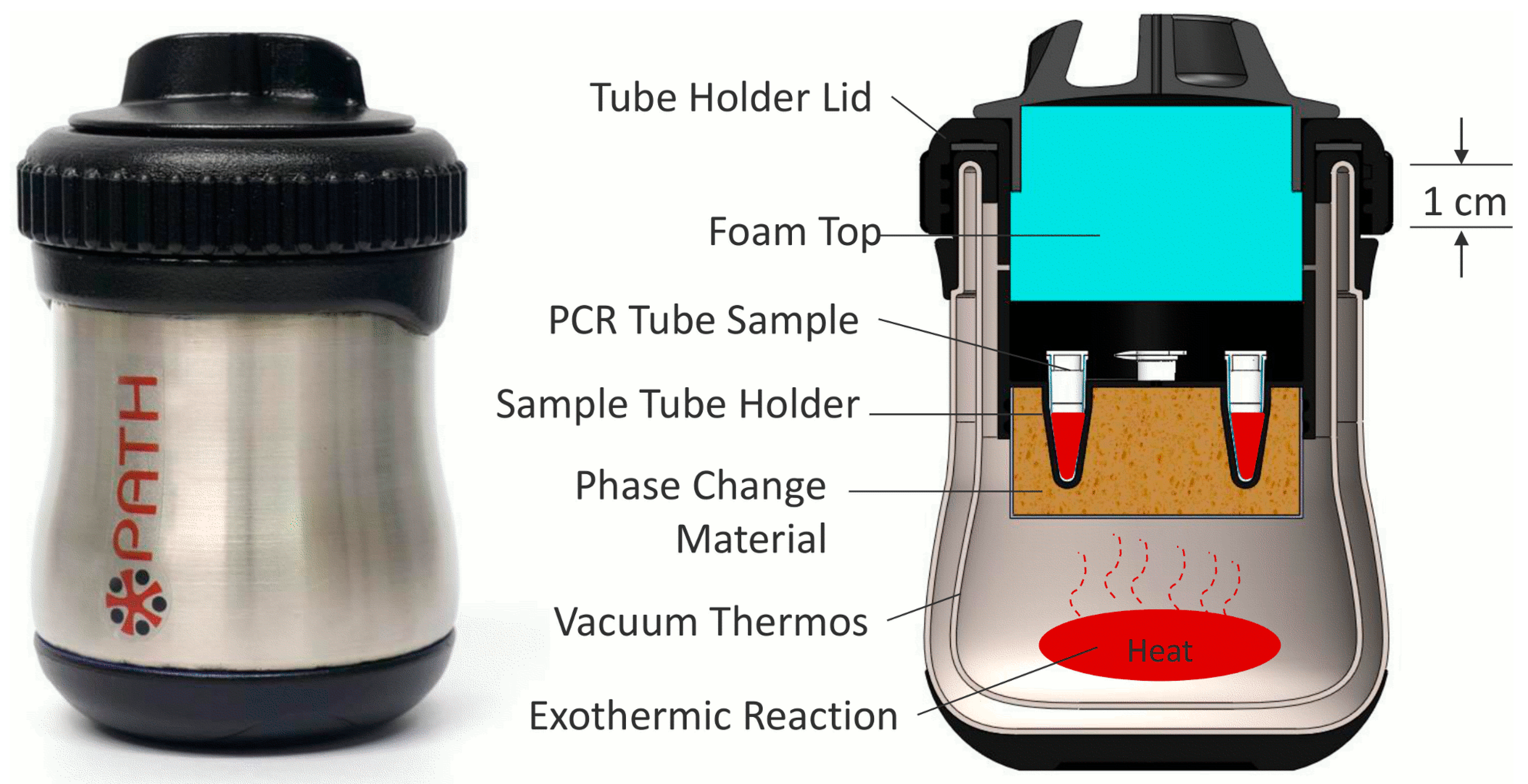
- Singleton, J.; Osborn, J.L.; Lillis, L.; Hawkins, K.; Guelig, D.; Price, W.; Johns, R.; Ebels, K.; Boyle, D.; Weigl, B. Electricity-free amplification and detection for molecular point-of-care diagnosis of HIV-1. PLoS ONE 2014, 9, e113693. [Google Scholar] [CrossRef]
- Curtis, K.A.; Rudolph, D.L.; Morrison, D.; Guelig, D.; Diesburg, S.; McAdams, D.; Burton, R.A.; LaBarre, P.; Owen, M. Single-use, electricity-free amplification device for detection of HIV-1. J. Virol. Methods 2016, 237, 132–137. [Google Scholar] [CrossRef]
- Gurrala, R.; Lang, Z.; Shepherd, L.; Davidson, D.; Harrison, E.; McClure, M.; Kaye, S.; Toumazou, C.; Cooke, G. Novel pH sensing semiconductor for point-of-care detection of HIV-1 viremia. Sci. Rep. 2016, 6, 1–6. [Google Scholar] [CrossRef]
- Kaneko, H.; Kawana, T.; Fukushima, E.; Suzutani, T. Tolerance of loop-mediated isothermal amplification to a culture medium and biological substances. J. Biochem. Biophys. Methods 2007, 70, 499–501. [Google Scholar] [CrossRef]
- Poon, L.L.; Wong, B.W.; Ma, E.H.; Chan, K.H.; Chow, L.M.; Abeyewickreme, W.; Tangpukdee, N.; Yuen, K.Y.; Guan, Y.; Looareesuwan, S. Sensitive and inexpensive molecular test for falciparum malaria: Detecting Plasmodium falciparum DNA directly from heat-treated blood by loop-mediated isothermal amplification. Clin. Chem. 2006, 52, 303–306. [Google Scholar] [CrossRef] [PubMed]
- Nliwasa, M.; MacPherson, P.; Chisala, P.; Kamdolozi, M.; Khundi, M.; Kaswaswa, K.; Mwapasa, M.; Msefula, C.; Sohn, H.; Flach, C. The sensitivity and specificity of loop-mediated isothermal amplification (LAMP) assay for tuberculosis diagnosis in adults with chronic cough in Malawi. PLoS ONE 2016, 11, e0155101. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The Use of Loop-Mediated Isothermal Amplification (TB-LAMP) for the Diagnosis of Pulmonary Tuberculosis: Policy Guidance; World Health Organization: Geneva, Switzerland, 2016; pp. 1–40. [Google Scholar]
- Euler, M.; Wang, Y.; Otto, P.; Tomaso, H.; Escudero, R.; Anda, P.; Hufert, F.T.; Weidmann, M. Recombinase polymerase amplification assay for rapid detection of Francisella tularensis. J. Clin. Microbiol. 2012, 50, 2234–2238. [Google Scholar] [CrossRef] [PubMed]
- Lobato, I.M.; O'Sullivan, C.K. Recombinase polymerase amplification: Basics, applications and recent advances. Trac Trends Anal. Chem. 2018, 98, 19–35. [Google Scholar] [CrossRef]
- Wong, G.; Wong, I.; Chan, K.; Hsieh, Y.; Wong, S. A rapid and low-cost PCR thermal cycler for low resource settings. PLoS ONE 2015, 10, e0131701. [Google Scholar] [CrossRef]
- Boyle, D.S.; Lehman, D.A.; Lillis, L.; Peterson, D.; Singhal, M.; Armes, N.; Parker, M.; Piepenburg, O.; Overbaugh, J. Rapid detection of HIV-1 proviral DNA for early infant diagnosis using recombinase polymerase amplification. mBio 2013, 4, e00135-13. [Google Scholar] [CrossRef]
- Lau, Y.L.; Ismail, I.b.; Mustapa, N.I.b.; Lai, M.Y.; Tuan Soh, T.S.; Haji Hassan, A.; Peariasamy, K.M.; Lee, Y.L.; Abdul Kahar, M.K.B.; Chong, J. Development of a reverse transcription recombinase polymerase amplification assay for rapid and direct visual detection of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). PLoS ONE 2021, 16, e0245164. [Google Scholar]
- Nassir, A.A.; Baptiste, M.J.; Mwikarago, I.; Habimana, M.R.; Ndinkabandi, J.; Murangwa, A.; Nyatanyi, T.; Muvunyi, C.M.; Nsanzimana, S.; Leon, M. RPA-Based Method For The Detection Of SARS-CoV2. medRxiv 2020, 1–23. [Google Scholar] [CrossRef]
- Rohrman, B.A.; Richards-Kortum, R.R. A paper and plastic device for performing recombinase polymerase amplification of HIV DNA. Lab Chip 2012, 12, 3082–3088. [Google Scholar] [CrossRef]
- Denny, T.; Yogev, R.; Gelman, R.; Skuza, C.; Oleske, J.; Chadwick, E.; Cheng, S.-C.; Connor, E. Lymphocyte subsets in healthy children during the first 5 years of life. JAMA 1992, 267, 1484–1488. [Google Scholar] [CrossRef]
- Lillis, L.; Lehman, D.A.; Siverson, J.B.; Weis, J.; Cantera, J.; Parker, M.; Piepenburg, O.; Overbaugh, J.; Boyle, D.S. Cross-subtype detection of HIV-1 using reverse transcription and recombinase polymerase amplification. J. Virol. Methods 2016, 230, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Lillis, L.; Siverson, J.; Lee, A.; Cantera, J.; Parker, M.; Piepenburg, O.; Lehman, D.A.; Boyle, D.S. Factors influencing Recombinase polymerase amplification (RPA) assay outcomes at point of care. Mol. Cell. Probes 2016, 30, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Lifson, M.A.; Inci, F.; Liang, L.-G.; Sheng, Y.-F.; Demirci, U. Advances in addressing technical challenges of point-of-care diagnostics in resource-limited settings. Expert Rev. Mol. Diagn. 2016, 16, 449–459. [Google Scholar] [CrossRef] [PubMed]
- Kong, M.; Li, Z.; Wu, J.; Hu, J.; Sheng, Y.; Wu, D.; Lin, Y.; Li, M.; Wang, X.; Wang, S. A wearable microfluidic device for rapid detection of HIV-1 DNA using recombinase polymerase amplification. Talanta 2019, 205, 120155. [Google Scholar] [CrossRef]
- Alhajj, M.; Farhana, A. Enzyme Linked Immunosorbent Assay (ELISA). In StatPearls; StatPearls Publishing: Tampa, FL, USA, 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK555922/ (accessed on 20 August 2022).
- Yeom, J.-S.; Lee, J.-B.; Ryu, S.-H.; Kang, H.-J.; Kim, S.; Kim, Y.-A.; Ahn, S.-Y.; Cha, J.-E.; Park, J.-W. Evaluation of a new third-generation ELISA for the detection of HIV infection. Ann. Clin. Lab. Sci. 2006, 36, 73–78. [Google Scholar]
- Von Sydow, M.; Gaines, H.; Sönnerborg, A.; Forsgren, M.; Pehrson, P.; Strannegård, Ö. Antigen detection in primary HIV infection. Br. Med. J. 1988, 296, 238–240. [Google Scholar] [CrossRef][Green Version]
- Han, H.; Huang, Y.; Dong, Q.; Huang, Y.; Lu, J.; Wang, W.; Chen, K. Clinical Application Evaluation of a Fourth-Generation HIV Antigen Antibody Combination Screening Assay. Clin. Lab. 2019, 65, 10. [Google Scholar] [CrossRef]
- Saville, R.D.; Constantine, N.T.; Cleghorn, F.R.; Jack, N.; Bartholomew, C.; Edwards, J.; Gomez, P.; Blattner, W.A. Fourth-generation enzyme-linked immunosorbent assay for the simultaneous detection of human immunodeficiency virus antigen and antibody. J. Clin. Microbiol. 2001, 39, 2518–2524. [Google Scholar] [CrossRef]
- Sujatha, K.; Vaisakhi, K. Comparative study of 3rd generation v/s 4 th generation ELISA in blood donors for early diagnosis of HIV in rural population. Int. J. Curr. Microbiol. Appl. Sci. 2017, 6, 1183–1193. [Google Scholar] [CrossRef]
- Giri, B.; Liu, Y.; Nchocho, F.N.; Corcoran, R.C.; Dutta, D. Microfluidic ELISA employing an enzyme substrate and product species with similar detection properties. Analyst 2018, 143, 989–998. [Google Scholar] [CrossRef]
- Tan, X.; Oo, M.K.K.; Gong, Y.; Li, Y.; Zhu, H.; Fan, X. Glass capillary based microfluidic ELISA for rapid diagnostics. Analyst 2017, 142, 2378–2385. [Google Scholar] [CrossRef] [PubMed]
- Chin, C.D.; Laksanasopin, T.; Cheung, Y.K.; Steinmiller, D.; Linder, V.; Parsa, H.; Wang, J.; Moore, H.; Rouse, R.; Umviligihozo, G. Microfluidics-based diagnostics of infectious diseases in the developing world. Nat. Med. 2011, 17, 1015. [Google Scholar] [CrossRef] [PubMed]
- Gray, R.H.; Makumbi, F.; Serwadda, D.; Lutalo, T.; Nalugoda, F.; Opendi, P.; Kigozi, G.; Reynolds, S.J.; Sewankambo, N.K.; Wawer, M.J. Limitations of rapid HIV-1 tests during screening for trials in Uganda: Diagnostic test accuracy study. BMJ 2007, 335, 188. [Google Scholar] [CrossRef] [PubMed]
- Klarkowski, D.B.; Wazome, J.M.; Lokuge, K.M.; Shanks, L.; Mills, C.F.; O'Brien, D.P. The evaluation of a rapid in situ HIV confirmation test in a programme with a high failure rate of the WHO HIV two-test diagnostic algorithm. PLoS ONE 2009, 4, e4351. [Google Scholar] [CrossRef] [PubMed]
- Posthuma-Trumpie, G.A.; Korf, J.; van Amerongen, A. Lateral flow (immuno) assay: Its strengths, weaknesses, opportunities and threats. A literature survey. Anal. Bioanal. Chem. 2009, 393, 569–582. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Tasoglu, S.; Chen, P.Z.; Chen, M.; Akbas, R.; Wach, S.; Ozdemir, C.I.; Gurkan, U.A.; Giguel, F.F.; Kuritzkes, D.R. Micro-a-fluidics ELISA for rapid CD4 cell count at the point-of-care. Sci. Rep. 2014, 4, 1–9. [Google Scholar] [CrossRef]
- Fennell, R.D.; Sher, M.; Asghar, W. Development of a Microfluidic Device for CD4+ T Cell Isolation and Automated Enumeration from Whole Blood. Biosensors 2021, 12, 12. [Google Scholar] [CrossRef]
- Sher, M.; Asghar, W. Development of a multiplex fully automated assay for rapid quantification of CD4+ T cells from whole blood. Biosens. Bioelectron. 2019, 142, 111490. [Google Scholar] [CrossRef]
- Li, X.; Tian, J.; Garnier, G.; Shen, W. Fabrication of paper-based microfluidic sensors by printing. Colloids Surf. B Biointerfaces 2010, 76, 564–570. [Google Scholar] [CrossRef]
- Li, X.; Tian, J.; Nguyen, T.; Shen, W. Paper-based microfluidic devices by plasma treatment. Anal. Chem. 2008, 80, 9131–9134. [Google Scholar] [CrossRef]
- Lu, Y.; Shi, W.; Qin, J.; Lin, B. Fabrication and characterization of paper-based microfluidics prepared in nitrocellulose membrane by wax printing. Anal. Chem. 2010, 82, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.M.; Martinez, A.W.; Gong, J.; Mace, C.R.; Phillips, S.T.; Carrilho, E.; Mirica, K.A.; Whitesides, G.M. Paper-based ELISA. Angew. Chem. Int. Ed. 2010, 49, 4771–4774. [Google Scholar] [CrossRef] [PubMed]
- Zhao, C.; Liu, X. A portable paper-based microfluidic platform for multiplexed electrochemical detection of human immunodeficiency virus and hepatitis C virus antibodies in serum. Biomicrofluidics 2016, 10, 024119. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Cheng, C.; Martinez, A.; Mirica, K.; Li, X.; Phillips, S.; Mascarenas, M.; Whitesides, G. A portable microfluidic paper-based device for ELISA. In Proceedings of the 2011 IEEE 24th International Conference on Micro Electro Mechanical Systems, Cancun, Mexico, 23–27 January 2011; pp. 75–78. [Google Scholar]
- Rodriguez, N.M.; Wong, W.S.; Liu, L.; Dewar, R.; Klapperich, C.M. A fully integrated paperfluidic molecular diagnostic chip for the extraction, amplification, and detection of nucleic acids from clinical samples. Lab Chip 2016, 16, 753–763. [Google Scholar] [CrossRef]
- Leng, S.X.; McElhaney, J.E.; Walston, J.D.; Xie, D.; Fedarko, N.S.; Kuchel, G.A. ELISA and multiplex technologies for cytokine measurement in inflammation and aging research. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2008, 63, 879–884. [Google Scholar] [CrossRef]
- Sher, M.; Zhuang, R.; Demirci, U.; Asghar, W. Paper-based analytical devices for clinical diagnosis: Recent advances in the fabrication techniques and sensing mechanisms. Expert Rev. Mol. Diagn. 2017, 17, 351–366. [Google Scholar] [CrossRef]
- Liu, J.; Du, B.; Zhang, P.; Haleyurgirisetty, M.; Zhao, J.; Ragupathy, V.; Lee, S.; DeVoe, D.L.; Hewlett, I.K. Development of a microchip Europium nanoparticle immunoassay for sensitive point-of-care HIV detection. Biosens. Bioelectron. 2014, 61, 177–183. [Google Scholar] [CrossRef]
- Ouyang, W.; Han, J. Universal amplification-free molecular diagnostics by billion-fold hierarchical nanofluidic concentration. Proc. Natl. Acad. Sci. USA 2019, 116, 16240–16249. [Google Scholar] [CrossRef]
- Sia, S.K.; Linder, V.; Parviz, B.A.; Siegel, A.; Whitesides, G.M. An integrated approach to a portable and low-cost immunoassay for resource-poor settings. Angew. Chem. Int. Ed. 2004, 43, 498–502. [Google Scholar] [CrossRef]
- Eid, J.; Mougel, M.; Socol, M. Advances in continuous microfluidics-based technologies for the study of HIV infection. Viruses 2020, 12, 982. [Google Scholar] [CrossRef]
- Kelley, S.O.; Mirkin, C.A.; Walt, D.R.; Ismagilov, R.F.; Toner, M.; Sargent, E.H. Advancing the speed, sensitivity and accuracy of biomolecular detection using multi-length-scale engineering. Nat. Nanotechnol. 2014, 9, 969. [Google Scholar] [CrossRef] [PubMed]
- Hughes, A.J.; Herr, A.E. Microfluidic western blotting. Proc. Natl. Acad. Sci. USA 2012, 109, 21450–21455. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, R.; Gilda, J.E.; Gomes, A.V. The necessity of and strategies for improving confidence in the accuracy of western blots. Expert Rev. Proteom. 2014, 11, 549–560. [Google Scholar] [CrossRef] [PubMed]
- Recommendations, C. Interpretation and use of the western blot assay for serodiagnosis of human immunodeficiency virus type 1 infections. MMWR 1989, 38, 1–7. [Google Scholar]
- Newman, G.R.; Jasani, B. Silver development in microscopy and bioanalysis: Past and present. J. Pathol. A J. Pathol. Soc. Great Br. Irel. 1998, 186, 119–125. [Google Scholar] [CrossRef]
- Khan, M.; Wang, R.; Li, B.; Liu, P.; Weng, Q.; Chen, Q. Comparative evaluation of the LAMP assay and PCR-based assays for the rapid detection of Alternaria solani. Front. Microbiol. 2018, 9, 2089. [Google Scholar] [CrossRef]
- Turbé, V.; Gray, E.R.; Lawson, V.E.; Nastouli, E.; Brookes, J.C.; Weiss, R.A.; Pillay, D.; Emery, V.C.; Verrips, C.T.; Yatsuda, H. Towards an ultra-rapid smartphone-connected test for infectious diseases. Sci. Rep. 2017, 7, 1–11. [Google Scholar]
- Damhorst, G.L.; Duarte-Guevara, C.; Chen, W.; Ghonge, T.; Cunningham, B.T.; Bashir, R. Smartphone-imaged HIV-1 reverse-transcription loop-mediated isothermal amplification (RT-LAMP) on a chip from whole blood. Engineering 2015, 1, 324–335. [Google Scholar] [CrossRef]
- Chen, A.; Wang, R.; Bever, C.R.; Xing, S.; Hammock, B.D.; Pan, T. Smartphone-interfaced lab-on-a-chip devices for field-deployable enzyme-linked immunosorbent assay. Biomicrofluidics 2014, 8, 064101. [Google Scholar] [CrossRef]
- Majumder, S.; Deen, M.J. Smartphone sensors for health monitoring and diagnosis. Sensors 2019, 19, 2164. [Google Scholar] [CrossRef]
- Center, P.R.; Mobile Fact Sheet. Pew Research Center. 2018. Available online: https://www.pewresearch.org/internet/fact-sheet/mobile/ (accessed on 7 October 2020).
- Silver, L.; Johnson, C. Majorities in Sub-Saharan Africa Own Mobile Phones, but Smartphone Adoption Is Modest. Available online: https://www.pewresearch.org/global/2018/10/09/majorities-in-sub-saharan-africa-own-mobile-phones-but-smartphone-adoption-is-modest/ (accessed on 9 December 2020).
- Navruz, I.; Coskun, A.F.; Wong, J.; Mohammad, S.; Tseng, D.; Nagi, R.; Phillips, S.; Ozcan, A. Smart-phone based computational microscopy using multi-frame contact imaging on a fiber-optic array. Lab Chip 2013, 13, 4015–4023. [Google Scholar] [CrossRef] [PubMed]
- Oncescu, V.; Mancuso, M.; Erickson, D. Cholesterol testing on a smartphone. Lab Chip 2014, 14, 759–763. [Google Scholar] [CrossRef] [PubMed]
- Stedtfeld, R.D.; Tourlousse, D.M.; Seyrig, G.; Stedtfeld, T.M.; Kronlein, M.; Price, S.; Ahmad, F.; Gulari, E.; Tiedje, J.M.; Hashsham, S.A. Gene-Z: A device for point of care genetic testing using a smartphone. Lab Chip 2012, 12, 1454–1462. [Google Scholar] [CrossRef] [PubMed]
- Coleman, B.; Coarsey, C.; Asghar, W. Cell phone based colorimetric analysis for point-of-care settings. Analyst 2019, 144, 1935–1947. [Google Scholar] [CrossRef] [PubMed]
- Coleman, B.; Coarsey, C.; Kabir, M.A.; Asghar, W. Point-of-care colorimetric analysis through smartphone video. Sens. Actuators B Chem. 2019, 282, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Ning, B.; Yu, T.; Zhang, S.; Huang, Z.; Tian, D.; Lin, Z.; Niu, A.; Golden, N.; Hensley, K.; Threeton, B. A smartphone-read ultrasensitive and quantitative saliva test for COVID-19. Sci. Adv. 2021, 7, eabe3703. [Google Scholar] [CrossRef]
- Wang, S.; Zhao, X.; Khimji, I.; Akbas, R.; Qiu, W.; Edwards, D.; Cramer, D.W.; Ye, B.; Demirci, U. Integration of cell phone imaging with microchip ELISA to detect ovarian cancer HE4 biomarker in urine at the point-of-care. Lab Chip 2011, 11, 3411–3418. [Google Scholar] [CrossRef]
- Hasan, M.M.; Alam, M.W.; Wahid, K.A.; Miah, S.; Lukong, K.E. A low-cost digital microscope with real-time fluorescent imaging capability. PLoS ONE 2016, 11, e0167863. [Google Scholar] [CrossRef]
- Gray, E.R.; Turbé, V.; Lawson, V.E.; Page, R.H.; Cook, Z.C.; Ferns, R.B.; Nastouli, E.; Pillay, D.; Yatsuda, H.; Athey, D. Ultra-rapid, sensitive and specific digital diagnosis of HIV with a dual-channel SAW biosensor in a pilot clinical study. NPJ Digit. Med. 2018, 1, 1–8. [Google Scholar] [CrossRef]
- Pope, J. Ransomware: Minimizing the risks. Innov. Clin. Neurosci. 2016, 13, 37. [Google Scholar]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tharakan, S.; Faqah, O.; Asghar, W.; Ilyas, A. Microfluidic Devices for HIV Diagnosis and Monitoring at Point-of-Care (POC) Settings. Biosensors 2022, 12, 949. https://doi.org/10.3390/bios12110949
Tharakan S, Faqah O, Asghar W, Ilyas A. Microfluidic Devices for HIV Diagnosis and Monitoring at Point-of-Care (POC) Settings. Biosensors. 2022; 12(11):949. https://doi.org/10.3390/bios12110949
Chicago/Turabian StyleTharakan, Shebin, Omair Faqah, Waseem Asghar, and Azhar Ilyas. 2022. "Microfluidic Devices for HIV Diagnosis and Monitoring at Point-of-Care (POC) Settings" Biosensors 12, no. 11: 949. https://doi.org/10.3390/bios12110949
APA StyleTharakan, S., Faqah, O., Asghar, W., & Ilyas, A. (2022). Microfluidic Devices for HIV Diagnosis and Monitoring at Point-of-Care (POC) Settings. Biosensors, 12(11), 949. https://doi.org/10.3390/bios12110949






