Lab on a Chip Device for Diagnostic Evaluation and Management in Chronic Renal Disease: A Change Promoting Approach in the Patients’ Follow Up
Abstract
:1. Introduction
2. LOCs Design, Available Technologies, and Detection Methods
2.1. LOCs-Related Technologies
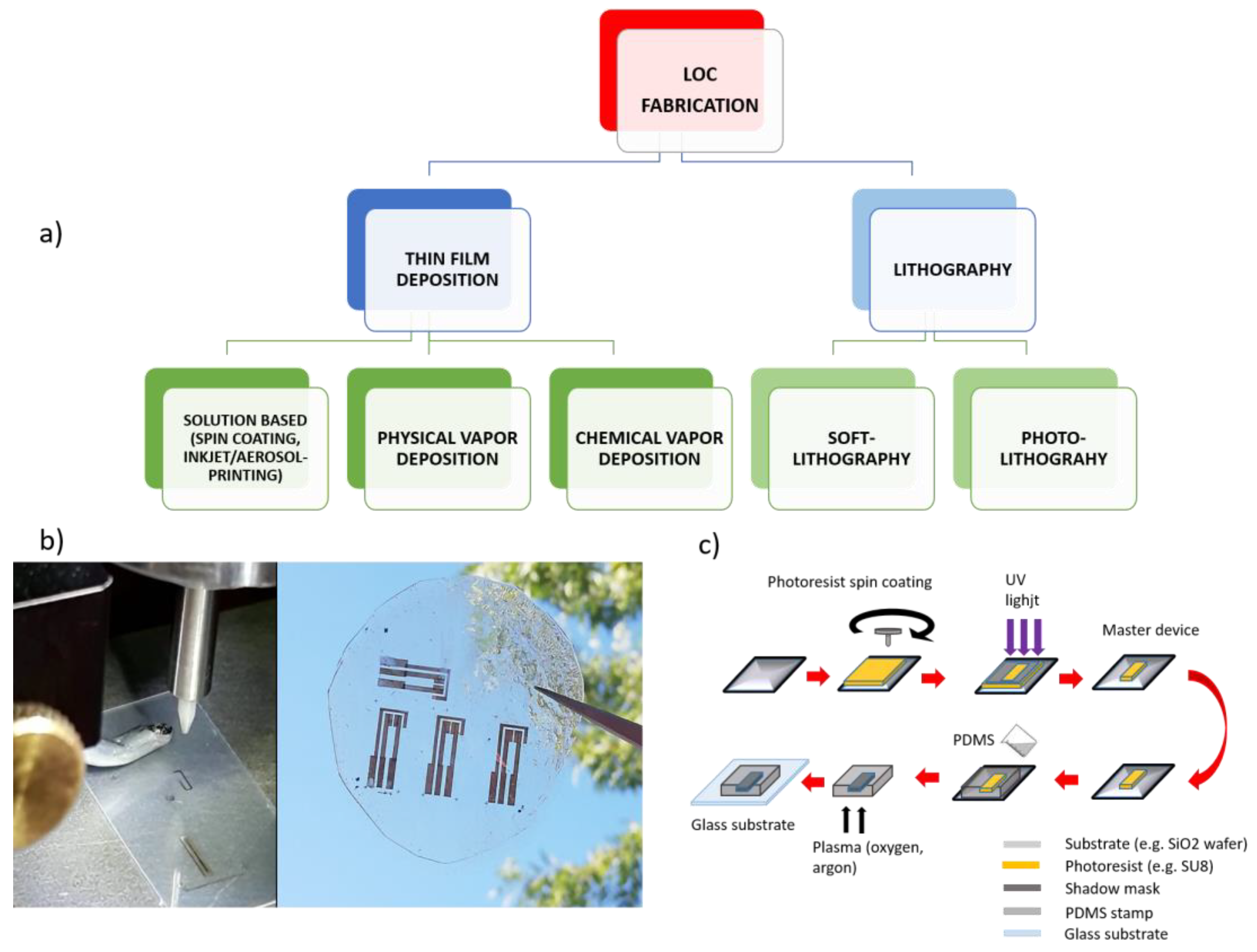
2.2. Techniques for LOC Devices Fabrication
2.3. Detection Methods for LOC Devices
- -
- Electrochemical: Electrochemical detection involves the interaction between chemical species and electrodes or probes. This interaction results in changes in the electrical signals. Different parameters can be measured, such as changes in the conductance/resistance due to the redox activity involving biological species and/or capacitance due to the electrical double layer formation at the active surface of the electrodes. The main advantages related to electrochemical detection are the possibility to improve a real time detection through low-cost electrodes. For these reasons, they are widely used in POCTs. On the other hand, the main drawbacks regard the need and the difficulty to control the ionic species concentration before detection, the complex and potentially ambiguous character of data analysis and interpretation, and, finally, the short shelf life of the electrochemical systems [59,60].
- -
- Mechanical: Mechanical systems generally refer to the use of micro-cantilevers. The detection is based on variations in the resonant frequency or surface stress of the mechanical sensor. Cantilever-based devices work in two different ways: (i) static deflection, where binding on one side of a cantilever causes unbalanced surface stress, resulting in a measurable deflection; (ii) dynamic mode, where binding on a cantilever causes variations in its mass, and consequently shifts the resonant frequency. The main advantage of mechanical detection is the label-free detection; the main disadvantages are the long response time (around 30 min) and the complex fabrication [61].
- -
- Optical: Among the detection methods, optical detection is likely the most suitable for LOCs because they offer the optimal compromise between the sensitivity and specificity of the detection. This method measures the variations in the light intensity, refractive index, or fluorescence intensity. Optical detection is characterized by negligible sample preparation, minimal interferences from artifacts in respect to the electrochemical methods, and real-time results. However, the employed opto-instrumentation is usually quite expensive [62]. Significantly, the high accessibility of smartphones and their improved technological features (cameras, connectivity, and computational power) have allowed smartphone integration with a wide range of analytical systems [63]. Accordingly, the use of smartphones’ sensors provides advantages not only in terms of lightweight and more affordable solutions, but also in terms of the abilities to process images by means of dedicated applications and to implement a wireless data sharing for a real time data analysis by remote computing [64]. Detection via smartphone is commonly based on various forms of optical measurements, including bright-field, colorimetric, luminescence, and/or fluorescence [27,65,66].
3. Chronic Kidney Disease
4. CKD Management and Available POCT
5. Current Limitations to LOCs Spreading in Clinical Setting
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Reyes, D.R.; Iossifidis, D.; Auroux, P.A.; Manz, A. Introduction, theory, and technology. Anal. Chem 2002, 74, 2623–2636. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, M.I. Lab-on-a-chip that takes the chip out of the lab. Nature 2022, 605, 429–430. [Google Scholar] [CrossRef]
- Taleghani, N.; Taghipour, F. Diagnosis of COVID-19 for controlling the pandemic: A review of the state-of-the-art. Biosens. Bioelectron. 2021, 174, 112830. [Google Scholar] [CrossRef] [PubMed]
- Prakash, R.; Pabbaraju, K.; Wong, S.; Tellier, R.; Kaler, K.V. Integrated sample-to-detection chip for nucleic acid test assays. Biomed Microdevices 2016, 18, 44. [Google Scholar] [CrossRef] [PubMed]
- Azizipour, N.; Avazpour, R.; Rosenzweig, D.H.; Sawan, M.; Ajji, A. Evolution of Biochip Technology: A Review from Lab-on-a-Chip to Organ-on-a-Chip. Micromachines 2020, 11, 599. [Google Scholar] [CrossRef]
- Yang, L.; Yi, W.; Sun, F.; Xu, M.; Zeng, Z.; Bi, X.; Dong, J.; Xie, Y.; Li, M. Application of Lab-on-Chip for Detection of Microbial Nucleic Acid in Food and Environment. Front. Microbiol. 2021, 12, 765375. [Google Scholar] [CrossRef] [PubMed]
- Büyüktiryaki, S.; Sümbelli, Y.; Keçili, R.; Hussain, C.M. Lab-On-Chip Platforms for Environmental Analysis. In Encyclopedia of Analytical Science, 3rd ed.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 267–273. [Google Scholar] [CrossRef]
- Shi, S.; Xie, Y.; Wang, G.; Luo, Y. Metabolite-based biosensors for natural product discovery and overproduction. Curr. Opin. Biotechnol. 2022, 75, 102699. [Google Scholar] [CrossRef]
- Hayden, O.; Luppa, P.B.; Min, J. Point-of-care testing-new horizons for cross-sectional technologies and decentralized application strategies. Anal. Bioanal Chem. 2022, 10, 3161. [Google Scholar] [CrossRef]
- Park, R.; Jeon, S.; Jeong, J.; Park, S.Y.; Han, D.W.; Hong, S.W. Recent Advances of Point-of-Care Devices Integrated with Molecularly Imprinted Polymers-Based Biosensors: From Biomolecule Sensing Design to Intraoral Fluid Testing. Biosensors 2022, 12, 136. [Google Scholar] [CrossRef]
- Rampoldi, E.; Patrucco, G.; Casati, M.; Morelli, B.; Carraro, P. Implementation and management of the point-of-care testing (POCT): Essential indications. Biochim. Clin. 2021, 45, 312–326. [Google Scholar]
- Wang, Y.; Yu, L.; Kong, X.; Sun, L. Application of nanodiagnostics in point-of-care tests for infectious diseases. Int. J. Nanomed. 2017, 12, 4789–4803. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Otoo, J.A.; Schlappi, T.S. REASSURED Multiplex Diagnostics: A Critical Review and Forecast. Biosensors 2022, 12, 124. [Google Scholar] [CrossRef] [PubMed]
- Romagnani, P.; Remuzzi, G.; Glassock, R.; Levin, A.; Jager, K.J.; Tonelli, M.; Massy, Z.; Wanner, C.; Anders, H.J. Chronic kidney disease. Nat. Rev. Dis. Prim. 2017, 23, 17088. [Google Scholar] [CrossRef]
- Wallace, E.L.; Rosner, M.H.; Alscher, M.D. Remote patient management for home dialysis patients. Kidney Int. Rep. 2017, 2, 1009–1017. [Google Scholar] [CrossRef] [Green Version]
- Chaudhuri, S.; Han, H.; Muchiutti, C. Remote treatment monitoring on hospitalization and technique failure rates in peritoneal dialysis patients. Kidney 360 2020, 1, 191–202. [Google Scholar] [CrossRef] [Green Version]
- Morosetti, M.; Fama, M.I. Clinical and social advantages of remote patient monitoring in home dialysis. Nephrol. Dial. Transpl. 2020, 35 (Suppl. 3), 140.MO029. [Google Scholar] [CrossRef]
- Li, L.; Perl, J. Can remote patient management improve out- comes in peritoneal dialysis? Contrib. Nephrol. 2019, 197, 113–123. [Google Scholar]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R.; Rab, S. Biosensors applications in medical field: A brief review. Sens. Int. 2021, 2, 100100. [Google Scholar] [CrossRef]
- Holt, H.; Freedman, D.B. Internal quality control in point-of-care testing: Where’s the evidence? Ann. Clin. Biochem. 2016, 53 Pt 2, 233–239. [Google Scholar] [CrossRef] [Green Version]
- Sumita, N.M.; Ferreira, C.E.S.; Martino, M.D.; Franca, C.N.; Faulhaber, A.C.L.; Scartezini, M.; Pinho, J.R.R.; Dias, C.M.; Cesar, K.R.; Pariz, V.M.; et al. Clinical Applications of Point-of-Care Testing in Different Conditions. Clin. Lab. 2018, 64, 1105–1112. [Google Scholar] [CrossRef]
- Verhees, B.; Van Kuijk, K.; Simonse, L. Care model design for E- health: Integration of point-of-care testing at Dutch general practices. Int. J. Environ. Res. Public Health 2017, 15, 4. [Google Scholar] [CrossRef] [Green Version]
- Bodington, R.; Kassianides, X.; Bhandari, S. Point-of-care testing technologies for the home in chronic kidney disease: A narrative review. Clin. Kidney J. 2021, 14, 2316–2331. [Google Scholar] [CrossRef] [PubMed]
- Christodouleas, D.C.; Kaur, B.; Chorti, P. From point-of-care testing to eHealth diagnostic devices (eDiagnostics). ACS Cent. Sci. 2018, 4, 1600–1616. [Google Scholar] [CrossRef]
- Liu, K.-Z.; Tian, G.; Ko, A.C.-T.; Geissler, M.; Brassard, D.; Veres, T. Detection of renal biomarkers in chronic kidney disease using microfluidics: Progress, challenges and opportunities. Biomed. Microdevices 2020, 22, 29. [Google Scholar] [CrossRef]
- St John, A.; Price, C.P. Existing and Emerging Technologies for Point-of-Care Testing. Clin. Biochem. Rev. 2014, 35, 155–167. [Google Scholar] [PubMed]
- Kong, L.; Gan, Y.; Liang, T.; Zhong, L.; Pan, Y.; Kirsanov, D.; Legin, A.; Wan, H.; Wang, P. A novel smartphone-based CD-spectrometer for high sensitive and cost-effective colorimetric detection of ascorbic acid. Anal. Chim. Acta 2020, 6, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Bambang, K.; Ali, A.E. Perspective—Paper-Based Biosensors: Trending Topic in Clinical Diagnostics Developments and Commercialization. J. Electrochem. Soc. 2020, 167, 037509. [Google Scholar] [CrossRef]
- Bahadır, E.B.; Sezgintürk, M.K. Lateral flow assays: Principles, designs and labels. TrAC Trends Anal. Chem. 2016, 82, 283–306. [Google Scholar] [CrossRef]
- Luka, G.S.; Nowak, E.; Kawchuk, J.; Hoorfar, M.; Najjaran, H. Portable device for the detection of colorimetric assays. R. Soc. Open Source 2017, 4, 171025. [Google Scholar] [CrossRef] [Green Version]
- Jessica, F.Y.F.; Yann, H.N.; Sing, M.N. Chapter 7-Carbon Dots as a New Class of Light Emitters for Biomedical Diagnostics and Therapeutic Applications; Grumezescu, A.M., Graphenes, F., Nanotubes, Eds.; William Andrew Publishing: Norwich, NY, USA, 2018; pp. 227–295. [Google Scholar]
- Peruzzi, C.; Battistoni, S.; Montesarchio, D.; Cocuzza, M.; Marasso, S.L.; Verna, A.; Pasquardini, L.; Verucchi, R.; Aversa, L.; Erokhin, V.; et al. Interfacing aptamers, nanoparticles and graphene in a hierarchical structure for highly selective detection of biomolecules in OECT devices. Sci. Rep. 2021, 11, 9380. [Google Scholar] [CrossRef] [PubMed]
- Bidinger, S.L.; Keene, S.T.; Han, S.; Plaxco, K.W.; Malliaras, G.G.; Hasan, T. Pulsed transistor operation enables miniaturization of electrochemical aptamer-based sensors. Sci. Adv. 2022, 8, eadd4111. [Google Scholar] [CrossRef]
- Naresh, V.; Lee, N. A review on biosensors and recent development of nanostructured materials-enabled biosensors. Sensors 2021, 21, 1109. [Google Scholar] [CrossRef]
- Pradeep, A.; Raveendran, J.; Babu, T.G.S. Design, fabrication and assembly of lab-on-a-chip and its uses. Prog. Mol. Biol. Transl. Sci. 2022, 187, 121–162. [Google Scholar] [PubMed]
- Seshan, K. Handbook of Thin-Film Deposition Processes and Techniques: Principles, Methods, Equipment and Application, 2nd ed.; Intel Corporation: Santa Clara, CA, USA, 2002. [Google Scholar] [CrossRef]
- Vernardou, D. Special Issue: Advances in Chemical Vapor Deposition. Materials 2020, 13, 4167. [Google Scholar] [CrossRef]
- Aléssio, P.; Constantino, C.J.; Job, A.E.; Aroca, R.; González, E.R. Molecular architecture of thin films fabricated via physical vapor deposition and containing a poly(azo)urethane. J. Nanosci. Nanotechnol. 2010, 10, 3012–3021. [Google Scholar] [CrossRef] [PubMed]
- LeGoues, F.K.; Rosenberg, R.; Meyerson, B.S. Kinetics and mechanism of oxidation of SiGe: Dry versus wet oxidation. Appl. Phys. Lett. 1989, 54, 644–646. [Google Scholar] [CrossRef]
- D’Angelo, P.; Barra, M.; Lombari, P.; Coppola, A.; Vurro, D.; Tarabella, G.; Marasso, S.L.; Borriello, M.; Chianese, F.; Perna, A.F.; et al. Homocysteine Solution-Induced Response in Aerosol Jet Printed OECTs by Means of Gold and Platinum Gate Electrodes. Int. J. Mol. Sci. 2021, 22, 1507. [Google Scholar] [CrossRef]
- Bhattacharjee, N.; Urrios, A.; Kang, S.; Folch, A. The upcoming 3D-printing revolution in microfluidics. Lab. Chip. 2016, 16, 1720–1742. [Google Scholar] [CrossRef] [Green Version]
- Nielsen, A.V.; Beauchamp, M.J.; Nordin, G.P.; Woolley, A.T. 3D Printed Microfluidics. Annu. Rev. Anal. Chem 2020, 12, 45–65. [Google Scholar] [CrossRef]
- Søndergaard, R.R.; Hösel, M. and Krebs, F.C. Roll-to-Roll fabrication of large area functional organic materials. J. Polym. Sci. B Polym. Phys. 2013, 51, 16–34. [Google Scholar] [CrossRef]
- Carlson, A.; Bowen, A.M.; Huang, Y.; Nuzzo, R.G. and Rogers, J.A. Transfer Printing Techniques for Materials Assembly and Micro/Nanodevice Fabrication. Adv. Mater. 2012, 24, 5284–5318. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Minett, M.; Hazen, E.; Wang, W.; Alvarez, C.; Griffin, J.; Jiang, N.; Chen, W. New Insights into Spin Coating of Polymer Thin Films in Both Wetting and Nonwetting Regimes. Langmuir 2022, 38, 12702–12710. [Google Scholar] [CrossRef] [PubMed]
- Iliescu, C.; Tan, K.L.; Tay, F.E.H.; Miao, J. Deep Wet and Dry Etching of Pyrex Glass: A Review; ICMAT: Singapore, 2005; pp. 75–78. [Google Scholar]
- Luttge, R. Chapter 4-Nanotechnology. In Micro and Nano Technologies, Microfabrication for Industrial Applications; Luttge, R., Ed.; William Andrew Publishing: Norwich, NY, USA, 2011; pp. 91–146. [Google Scholar]
- Sze, S.M.; Li, Y.; Ng, K.K. Physics of Semiconductor Devices, 3rd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2006. [Google Scholar] [CrossRef] [Green Version]
- Rose, M.A.; Bowen, J.J.; Morin, S.A. Emergent Soft Lithographic Tools for the Fabrication of Functional Polymeric Microstructures. ChemPhysChem 2019, 20, 909–925. [Google Scholar] [CrossRef] [PubMed]
- Banik, S.; Uchil, A.; Kalsang, T.; Chakrabarty, S.; Ali, M.A.; Srisungsitthisunti, P.; Mahato, K.K.; Surdo, S.; Mazumder, N. The revolution of PDMS microfluidics in cellular biology. Crit. Rev. Biotechnol. 2022, 11, 1–19. [Google Scholar] [CrossRef]
- D’Angelo, P.; Marasso, S.L.; Verna, A.; Ballesio, A.; Parmeggiani, M.; Sanginario, A.; Tarabella, G.; Demarchi, D.; Pirri, C.F.; Cocuzza, M.; et al. Scaling Organic Electrochemical Transistors Down to Nanosized Channels. Small 2019, 15, 1902332. [Google Scholar] [CrossRef]
- Wu, J.; Wang, R.; Yu, H.; Li, G.; Xu, K.; Tien, N.C.; Roberts, R.C.; Li, D. Inkjet-printed microelectrodes on PDMS as biosensors for functionalized microfluidic systems. Lab. Chip. 2015, 15, 690–695. [Google Scholar] [CrossRef]
- Tarabella, G.; Marasso, S.L.; Bertana, V.; Vurro, D.; D’Angelo, P.; Iannotta, S.; Cocuzza, M. Multifunctional Operation of an Organic Device with Three-Dimensional Architecture. Materials 2019, 12, 1357. [Google Scholar] [CrossRef] [Green Version]
- Tomaiuolo, G.M.; Barra, V.; Preziosi, A.; Cassinese, B.; Rotoli, S. Microfluidics analysis of red blood cell membrane viscoelasticity. Lab. Chip. 2011, 11, 449–454. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, J.; Pumera, M. 3D-printed biosensors for electrochemical and optical applications. TrAC Trends Anal. Chem. 2020, 128, 115933. [Google Scholar] [CrossRef]
- Kim, J.; Campbell, A.S.; de Ávila, B.E.-F.; Wang, J. Wearable biosensors for healthcare monitoring. Nat. Biotechnol. 2019, 37, 389–406. [Google Scholar] [CrossRef]
- Simon, D.; Ware, T.; Marcotte, R.; Lund, B.R.; Smith, D.W., Jr.; Di Prima, M.; Rennaker, R.L.; Voit, W. A comparison of polymer substrates for photolithographic processing of flexible bioelectronics. Biomed. Microdevices 2013, 15, 925–939. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Zhu, Y.; Cheng, W.; Chen, W.; Wu, Y.; Yu, H. Cellulose-Based Flexible Functional Materials for Emerging Intelligent Electronics. Adv. Mater. 2021, 33, e2000619. [Google Scholar] [CrossRef] [PubMed]
- Wongkaew, N.; He, P.; Kurth, V.; Surareungchai, W.; Baemner, A.J. Multi-channel PMMA microfluidic biosensor with integrated IDUAs for electrochemical detection. Anal. Bioanal. Chem. 2013, 405, 5965–5974. [Google Scholar] [CrossRef] [Green Version]
- Pires, N.M.; Dong, T.; Hanke, U.; Hoivik, N. Recent developments in optical detection technologies in lab-on-a-chip devices for biosensing applications. Sensors 2014, 14, 15458–15479. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferrari, M. Cancer nanotechnology: Opportunities and challenges. Nat. Rev. Cancer 2005, 5, 161–171. [Google Scholar] [CrossRef] [PubMed]
- Pennathur, S.; Fygenson, D.K. Improving fluorescence detection in lab on chip devices. Lab. Chip. 2008, 8, 649–652. [Google Scholar]
- Arshavsky-Graham, S.; Segal, E. Lab-on-a-Chip Devices for Point-of-Care Medical Diagnostics. Adv. Biochem. Eng. Biotechnol. 2022, 179, 247–265. [Google Scholar]
- Rizi, K.S. The smartphone biosensors for point-of-care detection of human infectious diseases: Overview and perspectives—A systematic review. Curr. Opin. Electrochem. 2022, 32, 100925. [Google Scholar] [CrossRef]
- Kanchi, S.; Sabela, M.I.; Mdluli, P.S.; Inamuddin; Bisetty, K. Smartphone based bioanalytical and diagnosis applications: A review. Biosens. Bioelectron. 2018, 102, 136–149. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Geng, Z.; Fan, Z.; Liu, J.; Chen, H. Point-of-care testing based on smartphone: The current state-of-the-art. Biosens. Bioelectron. 2017, 132, 17–37. [Google Scholar] [CrossRef] [PubMed]
- Gansevoort, R.T.; Matsushita, K.; Van der Velde, M.; Astor, B.C.; Woodward, M.; Levey, A.S.; De Jong, P.E.; Coresh, J. Chronic Kidney Disease Prognosis Consortium. Lower estimated GFR and higher albuminuria are associated with adverse kidney outcomes. A collaborative meta-analysis of general and high-risk population cohorts. Kidney Int. 2011, 80, 93–104. [Google Scholar] [CrossRef] [Green Version]
- Coppola, A.; Vigorito, C.; Lombari, P.; Martínez, Y.G.; Borriello, M.; Trepiccione, F.; Ingrosso, D.; Perna, A.F. Uremic Toxin Lanthionine Induces Endothelial Cell Mineralization In Vitro. Biomedicines 2022, 10, 444. [Google Scholar] [CrossRef]
- Franca, G.P.H.; Wolley, M.; Ranganathan, D.; Seguro, A.C. Vitamin D Deficiency in Chronic Kidney Disease: Recent Evidence and Controversies. Int. J. Environ. Res. Public Health 2018, 15, 1773. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jean, G.; Souberbielle, J.C.; Chazot, C. Vitamin D in Chronic Kidney Disease and Dialysis Patients. Nutrients 2017, 9, 328. [Google Scholar] [CrossRef] [PubMed]
- García-Martínez, Y.; Borriello, M.; Capolongo, G.; Ingrosso, D.; Perna, A.F. The Gut Microbiota in Kidney Transplantation: A Target for Personalized Therapy? Biology 2023, 12, 163. [Google Scholar] [CrossRef]
- Perna, A.F.; Glorieux, G.; Zacchia, M.; Trepiccione, F.; Capolongo, G.; Vigorito, C.; Anishchenko, E.; Ingrosso, D. The role of the intestinal microbiota in uremic solute accumulation: A focus on sulfur compounds. J. Nephrol. 2019, 32, 733–740. [Google Scholar] [CrossRef]
- Portolés, J.; Martín, L.; Broseta, J.J.; Cases, A. Anemia in Chronic Kidney Disease: From Pathophysiology and Current Treatments, to Future Agents. Front. Med. 2021, 8, 642296. [Google Scholar] [CrossRef]
- Kovesdy, C.P. Epidemiology of chronic kidney disease: An update 2022. Kidney Int. Suppl. 2022, 12, 7–11. [Google Scholar] [CrossRef]
- Perna, A.F.; D’Aniello, A.; Lowenson, J.D.; Clarke, S.; De Santo, N.G.; Ingrosso, D. D-Aspartate Content of Erytrocyte Membrane Proteins id Decreased in Uremia: Implication of the Repair of Damages Proteins. Am. Soc. Nephrol. 1997, 8, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Perna, A.F.; Ingrosso, D.; Satta, E.; Lombardi, C.; Galletti, P.; D’Aniello, A.; De Santo, N.G. Plasma protein aspartyl damage is increased in hemodialysis patients: Studies on causes and consequences. J. Am. Soc. Nephrol. 2004, 15, 2747–2754. [Google Scholar] [CrossRef] [Green Version]
- Hazara, A.M.; Durrans, K.; Bhandari, S. The role of patient portals in enhancing self-care in patients with renal conditions. Clin. Kidney J. 2020, 13, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kosack, C.S.; de Kieviet, W.; Bayrak, K.; Milovic, A.; Page, A.L. Evaluation of the Nova StatSensor® Xpress(TM) Creatinine point-of-care handheld analyzer. PLoS ONE 2015, 10, e0122433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarafidis, P.A.; Bakris, G.L. The antinatriuretic effect of insulin: An unappreciated mechanism for hypertension associated with insulin resistance? Am. J. Nephrol. 2007, 27, 44–54. [Google Scholar] [CrossRef]
- Sobieraj-Teague, M.; Daniel, D.; Farrelly, B.; Coghlan, D.; Gallus, A. Accuracy and clinical usefulness of the CoaguChek S and XS Point of Care devices when starting warfarin in a hospital outreach setting. Thromb. Res. 2009, 123, 909–913. [Google Scholar] [CrossRef]
- McCahon, D.; Roalfe, A.; Fitzmaurice, D.A. An evaluation of a coagulation system (Xprecia Stride) for utilisation in anticoagulation management. J. Clin. Pathol. 2018, 71, 20–26. [Google Scholar] [CrossRef] [Green Version]
- Singh, A.; Dubey, A.; Sonker, A.; Chaudhary, R. Evaluation of various methods of point-of-care testing of haemoglobin concentration in blood donors. Blood Transfus. 2015, 13, 233–239. [Google Scholar] [CrossRef]
- Bailey, T.; Bode, B.W.; Christiansen, M.P.; Klaff, L.J.; Alva, S. The Performance and Usability of a Factory-Calibrated Flash Glucose Monitoring System. Diabetes Technol. Ther. 2015, 17, 787–794. [Google Scholar] [CrossRef]
- Shephard, M.; Mathew, T. Point-of-care testing for kidney disease. In A Practical Guide to Global Point-of-Care Testing; CSIRO Publishing: Melbourne, Australia, 2016; Chapter 11; pp. 132–146. [Google Scholar]
- Yonel, Z.; Kuningas, K.; Sharma, P.; Dutton, M.; Jalal, Z.; Cockwell, P.; Webber, J.; Narendran, P.; Dietrich, T.; Chapple, L.C. Concordance of three point of care testing devices with clinical chemistry laboratory standard assays and patient-reported outcomes of blood sampling methods. BMC Med. Inform. Decis. Mak. 2022, 22, 248. [Google Scholar] [CrossRef]
- Li, J.; Li, Z.; Dou, Y.; Su, J.; Shi, J.; Zhou, Y.; Wang, L.; Song, S.; Fan, C. A nano-integrated microfluidic biochip for enzyme-based point-of-care detection of creatinine. Chem. Commun. 2021, 57, 4726–4729. [Google Scholar] [CrossRef] [PubMed]
- Tseng, C.; Ko, C.H.; Lu, S.Y.; Yang, C.E.; Fu, L.M.; Li, C.Y. Rapid electrochemical-biosensor microchip platform for determination of microalbuminuria in CKD patients. Anal. Chim. Acta. 2021, 1146, 70–76. [Google Scholar] [CrossRef]
- Gansevoort, R.T.; Nauta, F.L.; Bakker, S.J. Albuminuria: All you need to predict outcomes in chronic kidney disease? Curr. Opin. Nephrol. Hypertens. 2010, 19, 513. [Google Scholar] [CrossRef] [PubMed]
- Vutthikraivit, N.; Kiatamornrak, P.; Boonkrai, C.; Pisitkun, T.; Komolpis, K.; Puthong, S.; Lumlertgul, N.; Peerapornratana, S.; Thanawattano, C.; Tungsanga, S.; et al. Development and validation of point-of-care testing of albuminuria for early screening of chronic kidney disease. J. Clin. Lab. Anal. 2021, 35, 23729. [Google Scholar] [CrossRef] [PubMed]
- Perna, A.F.; Russo, L.; D’Esposito, V.; Formisano, P.; Bruzzese, D.; Vigorito, C.; Coppola, A.; Lombari, P.; Russo, D.; Ingrosso, D. Lanthionine, a Novel Uremic Toxin, in the Vascular Calcification of Chronic Kidney Disease: The Role of Proinflammatory Cytokines. Int. J. Mol. Sci. 2021, 22, 6875. [Google Scholar] [CrossRef]
- Peng, Y.S.; Ding, H.C.; Lin, Y.T.; Syu, J.P.; Chen, Y.; Wang, S.M. Uremic toxin p-cresol induces disassembly of gap junctions of cardiomyocytes. Toxicology 2012, 302, 11–17. [Google Scholar] [CrossRef]
- Sirangelo, I.; Borriello, M.; Liccardo, M.; Scafuro, M.; Russo, P.; Iannuzzi, C. Hydroxytyrosol Selectively Affects Non-Enzymatic Glycation in Human Insulin and Protects by AGEs Cytotoxicity. Antioxidants 2021, 10, 1127. [Google Scholar] [CrossRef]
- Moradi, M.; Soleymani, J.; Tayebi-Khosroshahi, H.; Khoubnasabjafari, M.; Jouyban, A. Simple Determination of p-Cresol in Plasma Samples Using Fluorescence Spectroscopy Technique. Iran J. Pharm. Res. 2021, 20, 68–78. [Google Scholar] [PubMed]
- Newman, A.W.; Behling-Kelly, E. Quality Assurance and Quality Control in Point-of-Care Testing. Top. Companion Anim. Med. 2016, 31, 2–10. [Google Scholar] [CrossRef]
- Erasmus, R.; Sahni, S.; El-Sharkawy, R. Connectivity Strategies in Managing a POCT Service. EJIFCC 2021, 32, 190–194. [Google Scholar] [PubMed]

| Features | Specification | |
|---|---|---|
| A | Affordable | Few than 10 dollars for Test—few than 500 dollars for machines |
| S | Sensitive | Minimal False Negative |
| S | Specific | Minimal False Positive |
| U | User-Friendly | Little training, easy to use |
| R | Rapid and Robust | Few than 30 min for result, minimal consumables, shelf life greater than one year at room temperature, high-throughput |
| E | Equipment-Free | Compact, on-site data analysis, battery powered |
| D | Delivered | Portable, Handheld |
| Method | Detection Measurement | Advantages | Disadvantages |
|---|---|---|---|
| Electrochemical | Variations in electrical parameters such as conductance, resistance or capacitance | Rapid detection, low costs of fabrication | Short shelf-life, matrix interferences, need to control ionic concentration before measurement |
| Mechanical | Variations in resonant frequency or surface stress of the mechanical sensor | Label free detection, monolithic sensing integration | Very slow detection time, complex fabrication |
| Optical | Variations in absorbance, turbidity, fluorescence, refractive index | Rapid detection, no sample preparation | Optical instrumentation is generally expensive, complex set-up |
| A1 | A2 | A3 | ||
|---|---|---|---|---|
| <30 mg/gCr | 30–300 mg/gCr | >300 mg/gCr | ||
| G1 | >90 mL/min/1.73 m2 | low | moderate | high |
| G2 | 60–89 mL/min/1.73 m2 | low | moderate | high |
| G3a | 45–59 mL/min/1.73 m2 | moderate | high | very high |
| G3b | 30–44 mL/min/1.73 m2 | high | very high | very high |
| G4 | 15–29 mL/min/1.73 m2 | very high | very high | very high |
| G5 | <15 mL/min/1.73 m2 | very high | very high | very high |
| Device | Test | Use at Home | Ref. | |
|---|---|---|---|---|
| 1 | Nova biomedical StatSensor and StatSensor Express cretinine | Creatinine and calculation of eGFR | No | [78] |
| 2 | Hemocue Albumin 201 | Urinary Albumin | No | [79] |
| 3 | Roche Diagnostics CoaguChek XS | Prothrombin time and INR | Yes | [80] |
| 4 | Siemens Healthcare Diagnostics Xprecia Stride | Prothrombin time and INR | No | [81] |
| 5 | Entia Luma | Hemoglobin | Yes | [23] |
| 6 | EKF Diagnostics HemoControl | Hemoglobin and estimated Hematocrit | No | [82] |
| 7 | Abbott Laboratories FreeStyle Libre | Glucose-oxidase enzyme-based sensor | Yes | [83] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borriello, M.; Tarabella, G.; D’Angelo, P.; Liboà, A.; Barra, M.; Vurro, D.; Lombari, P.; Coppola, A.; Mazzella, E.; Perna, A.F.; et al. Lab on a Chip Device for Diagnostic Evaluation and Management in Chronic Renal Disease: A Change Promoting Approach in the Patients’ Follow Up. Biosensors 2023, 13, 373. https://doi.org/10.3390/bios13030373
Borriello M, Tarabella G, D’Angelo P, Liboà A, Barra M, Vurro D, Lombari P, Coppola A, Mazzella E, Perna AF, et al. Lab on a Chip Device for Diagnostic Evaluation and Management in Chronic Renal Disease: A Change Promoting Approach in the Patients’ Follow Up. Biosensors. 2023; 13(3):373. https://doi.org/10.3390/bios13030373
Chicago/Turabian StyleBorriello, Margherita, Giuseppe Tarabella, Pasquale D’Angelo, Aris Liboà, Mario Barra, Davide Vurro, Patrizia Lombari, Annapaola Coppola, Elvira Mazzella, Alessandra F. Perna, and et al. 2023. "Lab on a Chip Device for Diagnostic Evaluation and Management in Chronic Renal Disease: A Change Promoting Approach in the Patients’ Follow Up" Biosensors 13, no. 3: 373. https://doi.org/10.3390/bios13030373
APA StyleBorriello, M., Tarabella, G., D’Angelo, P., Liboà, A., Barra, M., Vurro, D., Lombari, P., Coppola, A., Mazzella, E., Perna, A. F., & Ingrosso, D. (2023). Lab on a Chip Device for Diagnostic Evaluation and Management in Chronic Renal Disease: A Change Promoting Approach in the Patients’ Follow Up. Biosensors, 13(3), 373. https://doi.org/10.3390/bios13030373







