Needle-Shaped Biosensors for Precision Diagnoses: From Benchtop Development to In Vitro and In Vivo Applications
Abstract
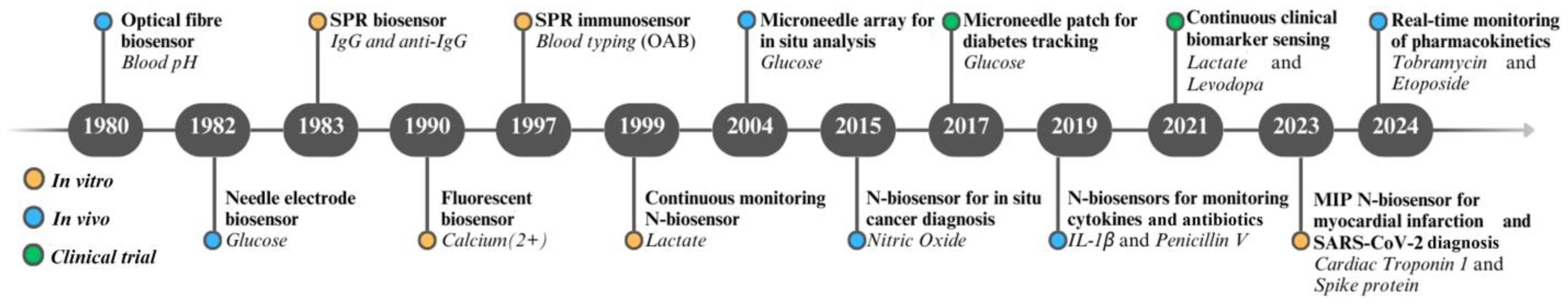
1. Introduction
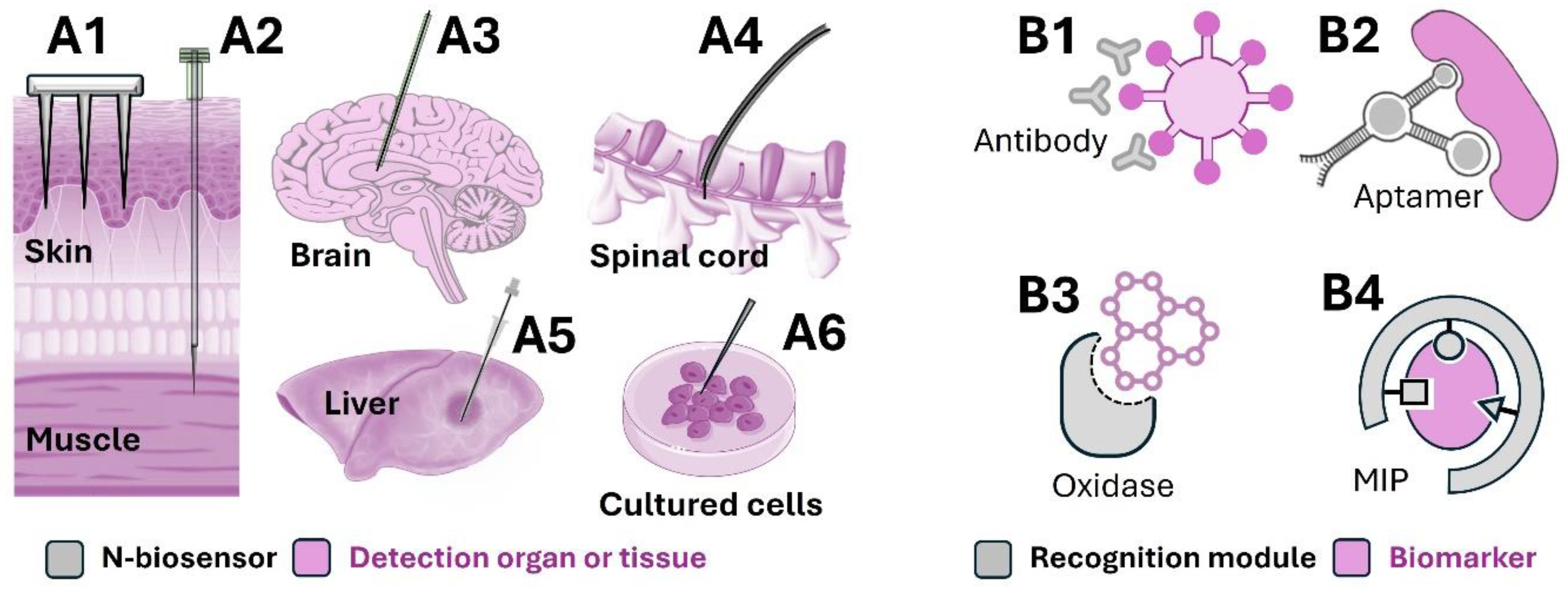
2. The Design of N-Biosensors
2.1. Options for N-Biosensor Components
2.1.1. Supporting Substrate and Functional Material
2.1.2. Recognition Module and Signal Transducer
2.2. Methods for Immobilisation of Recognition Modules
3. The In Vitro Application of N-Biosensors for Diagnoses in Clinical Specimens
4. In Vivo Applications of N-Biosensing
5. Conclusions and Future Prospects
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Blaschke, V.; Reich, K.; Blaschke, S.; Zipprich, S.; Neumann, C. Rapid quantitation of proinflammatory and chemoattractant cytokine expression in small tissue samples and monocyte-derived dendritic cells: Validation of a new real-time RT-PCR technology. J. Immunol. Methods 2000, 246, 79–90. [Google Scholar] [CrossRef] [PubMed]
- Callens, A.J.; Bartges, J.W. Urinalysis. Vet. Clin. Small Anim. Pract. 2015, 45, 621–637. [Google Scholar] [CrossRef] [PubMed]
- Mylonaki, M.; Langmead, L.; Pantes, A.; Johnson, F.; Rampton, D.S. Enteric infection in relapse of inflammatory bowel disease: Importance of microbiological examination of stool. Eur. J. Gastroenterol. Hepatol. 2004, 16, 775–778. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Ge, S.; Ge, L.; Yan, M.; Yu, J. Electrochemical DNA sensor based on three-dimensional folding paper device for specific and sensitive point-of-care testing. Electrochim. Acta 2012, 80, 334–341. [Google Scholar] [CrossRef]
- Quinn, J.G.; O‘Kennedy, R.; Smyth, M.; Moulds, J.; Frame, T. Detection of blood group antigens utilising immobilised antibodies and surface plasmon resonance. J. Immunol. Methods 1997, 206, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Jin, C.E.; Koo, B.; Lee, E.Y.; Kim, J.Y.; Kim, S.H.; Shin, Y. Simple and label-free pathogen enrichment via homobifunctional imidoesters using a microfluidic (SLIM) system for ultrasensitive pathogen detection in various clinical specimens. Biosens. Bioelectron. 2018, 111, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Mao, Z.; Zheng, H.; Wang, X.; Lin, S.; Sun, Y.; Jiang, B. DNA microarray for direct identification of bacterial pathogens in human stool samples. Digestion 2008, 78, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Arman, A.; Anwer, A.G.; Hutchinson, M.R.; Goldys, E.M. An optical fiber based immunosensor for localized detection of IL-1β in rat spinal cord. Sens. Actuators B Chem. 2019, 282, 122–129. [Google Scholar] [CrossRef]
- Deng, F.; Arman, A.; Goldys, E.M.; Hutchinson, M.R.; Liu, G. A method for in vivo quantification of cytokine IL-1β in the rat intrathecal space. ACS Appl. Bio Mater. 2019, 3, 539–546. [Google Scholar] [CrossRef]
- Yuen, C.; Liu, Q. Towards in vivo intradermal surface enhanced Raman scattering (SERS) measurements: Silver coated microneedle based SERS probe. J. Biophotonics 2014, 7, 683–689. [Google Scholar] [CrossRef]
- Deng, F.; Li, Y.; Hossain, M.J.; Kendig, M.D.; Arnold, R.; Goldys, E.M.; Morris, M.J.; Liu, G. Polymer brush based fluorescent immunosensor for direct monitoring of interleukin-1β in rat blood. Analyst 2019, 144, 5682–5690. [Google Scholar] [CrossRef] [PubMed]
- Ribaut, C.; Loyez, M.; Larrieu, J.C.; Chevineau, S.; Lambert, P.; Remmelink, M.; Wattiez, R.; Caucheteur, C. Cancer biomarker sensing using packaged plasmonic optical fiber gratings: Towards in vivo diagnosis. Biosens. Bioelectron. 2017, 92, 449–456. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Baratta, M.V.; Liu, G.; Frank, M.G.; Leslie, N.R.; Watkins, L.R.; Maier, S.F.; Hutchinson, M.R.; Goldys, E.M. A novel platform for in vivo detection of cytokine release within discrete brain regions. Brain Behav. Immun. 2018, 71, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Peterson, J.I.; Goldstein, S.R.; Fitzgerald, R.V.; Buckhold, D.K. Fiber optic pH probe for physiological use. Anal. Chem. 1980, 52, 864–869. [Google Scholar] [CrossRef] [PubMed]
- Shichiri, M.; Yamasaki, Y.; Kawamori, R.; Hakui, N.; Abe, H. Wearable artificial endocrine pancreas with needle-type glucose sensor. Lancet 1982, 320, 1129–1131. [Google Scholar] [CrossRef] [PubMed]
- Liedberg, B.; Nylander, C.; Lunström, I. Surface plasmon resonance for gas detection and biosensing. Sens. Actuators 1983, 4, 299–304. [Google Scholar] [CrossRef]
- Hahn, K.M.; Waggoner, A.S.; Taylor, D.L. A calcium-sensitive fluorescent analog of calmodulin based on a novel calmodulin-binding fluorophore. J. Biol. Chem. 1990, 265, 20335–20345. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Atanasov, P.; Wilkins, E. Needle-type lactate biosensor. Biosens. Bioelectron. 1999, 14, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Mukerjee, E.V.; Collins, S.D.; Isseroff, R.R.; Smith, R.L. Microneedle array for transdermal biological fluid extraction and in situ analysis. Sens. Actuators A Phys. 2004, 114, 267–275. [Google Scholar] [CrossRef]
- Keum, D.H.; Jung, H.S.; Wang, T.; Shin, M.H.; Kim, Y.-E.; Kim, K.H.; Ahn, G.O.; Hahn, S.K. Microneedle Biosensor for Real-Time Electrical Detection of Nitric Oxide for In Situ Cancer Diagnosis During Endomicroscopy. Adv. Healthc. Mater. 2015, 4, 1153–1158. [Google Scholar] [CrossRef] [PubMed]
- Emory University: Glucose Measurement Using Microneedle Patches (GUMP); ClinicalTrials.gov: Bethesda, MD, USA, 2017.
- Rawson, T.M.; Gowers, S.A.N.; Freeman, D.M.E.; Wilson, R.C.; Sharma, S.; Gilchrist, M.; MacGowan, A.; Lovering, A.; Bayliss, M.; Kyriakides, M.; et al. Microneedle biosensors for real-time, minimally invasive drug monitoring of phenoxymethylpenicillin: A first-in-human evaluation in healthy volunteers. Lancet Digit. Health 2019, 1, e335–e343. [Google Scholar] [CrossRef] [PubMed]
- Imperial College London: Minimally-Invasive Realtime Assessment of Continuous Lactate in Exercise (MIRACLE); ClinicalTrials.gov: Bethesda, MD, USA, 2021.
- University of California San Diego: Real-Time Levodopa Level Monitoring in Parkinson Disease; ClinicalTrials.gov: Bethesda, MD, USA, 2021.
- Choudhary, S.; Altintas, Z. Development of a Point-of-Care SPR Sensor for the Diagnosis of Acute Myocardial Infarction. Biosensors 2023, 13, 229. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Yin, Z.-Z.; Zheng, G.; Zhou, M.; Zhang, H.; Li, J.; Cai, W.; Kong, Y. Molecularly imprinted miniature electrochemical biosensor for SARS-CoV-2 spike protein based on Au nanoparticles and reduced graphene oxide modified acupuncture needle. Bioelectrochemistry 2023, 151, 108375. [Google Scholar] [CrossRef] [PubMed]
- Reynoso, M.; Chang, A.-Y.; Wu, Y.; Murray, R.; Suresh, S.; Dugas, Y.; Wang, J.; Arroyo-Currás, N. 3D-printed, aptamer-based microneedle sensor arrays using magnetic placement on live rats for pharmacokinetic measurements in interstitial fluid. Biosens. Bioelectron. 2024, 244, 115802. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Li, Q.; Han, Q. Needle-in-needle electrochemical sensor for in-vivo monitoring of anticancer drug etoposide. Biosens. Bioelectron. 2024, 258, 116348. [Google Scholar] [CrossRef]
- Zhang, F.; Deng, F.; Liu, G.-J.; Middleton, R.; Inglis, D.W.; Anwer, A.; Wang, S.; Liu, G. IFN-γ-induced signal-on fluorescence aptasensors: From hybridization chain reaction amplification to 3D optical fiber sensing interface towards a deployable device for cytokine sensing. Mol. Syst. Des. Eng. 2019, 4, 872–881. [Google Scholar] [CrossRef]
- Deng, F.; Goldys, E.M.; Liu, G. Molecularly imprinted polymer-based reusable biosensing device on stainless steel for spatially localized detection of cytokine IL-1β. Sens. Actuators B Chem. 2019, 292, 277–283. [Google Scholar] [CrossRef]
- Qi, M.; Huang, J.; Wei, H.; Cao, C.; Feng, S.; Guo, Q.; Goldys, E.M.; Li, R.; Liu, G. Graphene oxide thin film with dual function integrated into a nanosandwich device for in vivo monitoring of interleukin-6. ACS Appl. Mater. Interfaces 2017, 9, 41659–41668. [Google Scholar] [CrossRef] [PubMed]
- Russell, C.; Ward, A.C.; Vezza, V.; Hoskisson, P.; Alcorn, D.; Steenson, D.P.; Corrigan, D.K. Development of a needle shaped microelectrode for electrochemical detection of the sepsis biomarker interleukin-6 (IL-6) in real time. Biosens. Bioelectron. 2019, 126, 806–814. [Google Scholar] [CrossRef] [PubMed]
- Song, N.; Xie, P.; Shen, W.; Javanmard, M.; Allen, M.G. Microwell-array on a flexible needle: A transcutaneous insertable impedance sensor for label-free cytokine detection. In Proceedings of the 2018 IEEE Micro Electro Mechanical Systems (MEMS), Belfast, UK, 21–25 January 2018; pp. 392–395. [Google Scholar]
- Cao, C.; Jin, R.; Wei, H.; Liu, Z.; Ni, S.; Liu, G.J.; Young, H.A.; Chen, X.; Liu, G. Adaptive in vivo device for theranostics of inflammation: Real-time monitoring of interferon-gamma and aspirin. Acta Biomater. 2020, 101, 372–383. [Google Scholar] [CrossRef] [PubMed]
- Andreescu, S.; Luck, L.A. Studies of the binding and signaling of surface-immobilized periplasmic glucose receptors on gold nanoparticles: A glucose biosensor application. Anal. Biochem. 2008, 375, 282–290. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Yoon, H.S.; Xuan, X.; Park, J.Y.; Paik, S.-J.; Allen, M.G. A patch type non-enzymatic biosensor based on 3D SUS micro-needle electrode array for minimally invasive continuous glucose monitoring. Sens. Actuators B Chem. 2016, 222, 1144–1151. [Google Scholar] [CrossRef]
- Zhang, B.L.; Jin, X.; Sun, L.H.; Guo, X.D. Needle-shaped glucose sensor based on polypyrrole doped with glucose oxidase. Microchem. J. 2020, 158, 105217. [Google Scholar] [CrossRef]
- Vasylieva, N.; Marinesco, S.; Barbier, D.; Sabac, A. Silicon/SU8 multi-electrode micro-needle for in vivo neurochemical monitoring. Biosens. Bioelectron. 2015, 72, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Tsai, T.-C.; Han, H.-Z.; Cheng, C.-C.; Chen, L.-C.; Chang, H.-C.; Chen, J.-J.J. Modification of platinum microelectrode with molecularly imprinted over-oxidized polypyrrole for dopamine measurement in rat striatum. Sens. Actuators B Chem. 2012, 171–172, 93–101. [Google Scholar] [CrossRef]
- Aiassa, S.; Yilmaz, S.; Carrara, S.; Demarchi, D. Pencil graphite needle-shaped biosensor for anaesthetic monitoring in human serum. In Proceedings of the 2020 IEEE Sensors, Rotterdam, The Netherlands, 25–28 October 2020; pp. 1–4. [Google Scholar]
- Milardović, S.; Grabarić, Z.; Tkalčec, M.; Rumenjak, V. Determination of oxalate in urine, using an amperometric biosensor with oxalate oxidase immobilized on the surface of a chromium hexacyanoferrate-modified graphite electrode. J. AOAC Int. 2000, 83, 1212–1217. [Google Scholar] [CrossRef] [PubMed]
- Hajdukiewicz, J.; Boland, S.; Kavanagh, P.; Leech, D. An enzyme-amplified amperometric DNA hybridisation assay using DNA immobilised in a carboxymethylated dextran film anchored to a graphite surface. Biosens. Bioelectron. 2010, 25, 1037–1042. [Google Scholar] [CrossRef] [PubMed]
- Yun, J.; Hong, Y.-T.; Hong, K.-H.; Lee, J.-H. Ex vivo identification of thyroid cancer tissue using electrical impedance spectroscopy on a needle. Sens. Actuators B Chem. 2018, 261, 537–544. [Google Scholar] [CrossRef]
- Han, S.; Sun, J.; Wang, J.; Qian, W.; Dong, J. A built-in surface-enhanced Raman scattering-active microneedle for sampling in vivo and surface-enhanced Raman scattering detection ex vivo of NO. J. Raman Spectrosc. 2018, 49, 1747–1755. [Google Scholar] [CrossRef]
- Deng, F.; Li, Y.; Qiao, L.; Goldys, E. A CRISPR/Cas12a-assisted on-fibre immunosensor for ultrasensitive small protein detection in complex biological samples. Anal. Chim. Acta 2022, 1192, 339351. [Google Scholar] [CrossRef] [PubMed]
- Krupka, S.S.; Wiltschi, B.; Reuning, U.; Holscher, K.; Hara, M.; Sinner, E.K. In vivo detection of membrane protein expression using surface plasmon enhanced fluorescence spectroscopy (SPFS). Biosens. Bioelectron. 2006, 22, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Ratautaite, V.; Topkaya, S.N.; Mikoliunaite, L.; Ozsoz, M.; Oztekin, Y.; Ramanaviciene, A.; Ramanavicius, A. Molecularly imprinted polypyrrole for DNA determination. Electroanalysis 2013, 25, 1169–1177. [Google Scholar] [CrossRef]
- Arya, S.K.; Singh, A.; Naidoo, R.; Wu, P.; McDermott, M.T.; Evoy, S. Chemically immobilized T4-bacteriophage for specific Escherichia coli detection using surface plasmon resonance. Analyst 2011, 136, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Kulagina, N.V.; Lassman, M.E.; Ligler, F.S.; Taitt, C.R. Antimicrobial peptides for detection of bacteria in biosensor assays. Anal. Chem. 2005, 77, 6504–6508. [Google Scholar] [CrossRef] [PubMed]
- Taheri, R.A.; Rezayan, A.H.; Rahimi, F.; Mohammadnejad, J.; Kamali, M. Development of an immunosensor using oriented immobilized anti-OmpW for sensitive detection of Vibrio cholerae by surface plasmon resonance. Biosens. Bioelectron. 2016, 86, 484–488. [Google Scholar] [CrossRef] [PubMed]
- Bhadra, P.; Shajahan, M.S.; Patel, P.N.; Bhattacharya, E.; Chadha, A.; Sekhar, P.K. Immobilizing Siderophores on Solid Surfaces for Bacterial Detection. J. Electrochem. Soc. 2018, 165, B3017–B3022. [Google Scholar] [CrossRef]
- Wan, Y.; Kim, Y.T.; Li, N.; Cho, S.K.; Bachoo, R.; Ellington, A.D.; Iqbal, S.M. Surface-immobilized aptamers for cancer cell isolation and microscopic cytology. Cancer Res. 2010, 70, 9371–9380. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Qi, M.; Hutchinson, M.R.; Yang, G.; Goldys, E.M. Recent advances in cytokine detection by immunosensing. Biosens. Bioelectron. 2016, 79, 810–821. [Google Scholar] [CrossRef] [PubMed]
- Downs, A.M.; Plaxco, K.W. Real-Time, In Vivo Molecular Monitoring Using Electrochemical Aptamer Based Sensors: Opportunities and Challenges. ACS Sens. 2022, 7, 2823–2832. [Google Scholar] [CrossRef] [PubMed]
- Avseenko, N.V.; Morozova, T.Y.; Ataullakhanov, F.I.; Morozov, V.N. Immobilization of Proteins in Immunochemical Microarrays Fabricated by Electrospray Deposition. Anal. Chem. 2001, 73, 6047–6052. [Google Scholar] [CrossRef] [PubMed]
- Echeverri, D.; Garg, M.; Varon Silva, D.; Orozco, J. Phosphoglycan-sensitized platform for specific detection of anti-glycan IgG and IgM antibodies in serum. Talanta 2020, 217, 121117. [Google Scholar] [CrossRef]
- Du, H.; Strohsahl, C.M.; Camera, J.; Miller, B.L.; Krauss, T.D. Sensitivity and specificity of metal surface-immobilized “molecular beacon” biosensors. J. Am. Chem. Soc. 2005, 127, 7932–7940. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Liu, S.; Deng, Q.; Ling, L. A sensitive colorimetric DNA biosensor for specific detection of the HBV gene based on silver-coated glass slide and G-quadruplex-hemin DNAzyme. J. Med. Virol. 2018, 90, 699–705. [Google Scholar] [CrossRef] [PubMed]
- Häkkinen, H. The gold–sulfur interface at the nanoscale. Nat. Chem. 2012, 4, 443–455. [Google Scholar] [CrossRef] [PubMed]
- Della Ventura, B.; Schiavo, L.; Altucci, C.; Esposito, R.; Velotta, R. Light assisted antibody immobilization for bio-sensing. Biomed. Opt. Express 2011, 2, 3223–3231. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.-C.C.; Rieben, N.; Iversen, L.; Sørensen, B.S.; Park, J.; Nygård, J.; Martinez, K.L. Specific and reversible immobilization of histidine-tagged proteins on functionalized silicon nanowires. Nanotechnology 2010, 21, 245105. [Google Scholar] [CrossRef] [PubMed]
- Sener, G.; Ozgur, E.; Rad, A.Y.; Uzun, L.; Say, R.; Denizli, A. Rapid real-time detection of procalcitonin using a microcontact imprinted surface plasmon resonance biosensor. Analyst 2013, 138, 6422–6428. [Google Scholar] [CrossRef] [PubMed]
- Ertürk Bergdahl, G.; Andersson, T.; Allhorn, M.; Yngman, S.; Timm, R.; Lood, R. In Vivo Detection and Absolute Quantification of a Secreted Bacterial Factor from Skin Using Molecularly Imprinted Polymers in a Surface Plasmon Resonance Biosensor for Improved Diagnostic Abilities. ACS Sens. 2019, 4, 717–725. [Google Scholar] [CrossRef] [PubMed]
- Bisker, G.; Iverson, N.M.; Ahn, J.; Strano, M.S. A pharmacokinetic model of a tissue implantable insulin sensor. Adv. Health Mater. 2015, 4, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Landry, M.P.; Barone, P.W.; Kim, J.-H.; Lin, S.; Ulissi, Z.W.; Lin, D.; Mu, B.; Boghossian, A.A.; Hilmer, A.J. Molecular recognition using corona phase complexes made of synthetic polymers adsorbed on carbon nanotubes. Nat. Nanotechnol. 2013, 8, 959–968. [Google Scholar] [CrossRef]
- Goluch, E.D.; Stoeva, S.I.; Lee, J.S.; Shaikh, K.A.; Mirkin, C.A.; Liu, C. A microfluidic detection system based upon a surface immobilized biobarcode assay. Biosens. Bioelectron. 2009, 24, 2397–2403. [Google Scholar] [CrossRef] [PubMed]
- Song, M.S.; Sekhon, S.S.; Shin, W.R.; Rhee, S.K.; Ko, J.H.; Kim, S.Y.; Min, J.; Ahn, J.Y.; Kim, Y.H. Aptamer-Immobilized Surface Plasmon Resonance Biosensor for Rapid and Sensitive Determination of Virulence Determinant. J. Nanosci. Nanotechnol. 2018, 18, 3095–3101. [Google Scholar] [CrossRef] [PubMed]
- Milagres, B.G.; Kubota, L.T.; Neto, G.D.O. Immobilized ferrocene and glucose oxidase on titanium (IV) oxide grafted onto a silica gel surface and its application as an amperometric glucose biosensor. Electroanalysis 1996, 8, 489–493. [Google Scholar] [CrossRef]
- Gao, P.; Xu, G.; Shi, X.; Yuan, K.; Tian, J. Rapid detection of Staphylococcus aureus by a combination of monoclonal antibody-coated latex and capillary electrophoresis. Electrophoresis 2006, 27, 1784–1789. [Google Scholar] [CrossRef] [PubMed]
- Myung, J.H.; Roengvoraphoj, M.; Tam, K.A.; Ma, T.; Memoli, V.A.; Dmitrovsky, E.; Freemantle, S.J.; Hong, S. Effective capture of circulating tumor cells from a transgenic mouse lung cancer model using dendrimer surfaces immobilized with anti-EGFR. Anal. Chem. 2015, 87, 10096–10102. [Google Scholar] [CrossRef] [PubMed]
- Deng, F.; Qiao, L.; Li, Y. A fluorescent immunosensor on optical fibre for the multiplex detection of proinflammatory cytokines. Sens. Bio-Sens. Res. 2022, 37, 100501. [Google Scholar] [CrossRef]
- Zhu, X.; Xiong, S.; Zhang, J.; Zhang, X.; Tong, X.; Kong, S. Improving paper-based ELISA performance through covalent immobilization of antibodies. Sens. Actuators B Chem. 2018, 255, 598–604. [Google Scholar] [CrossRef]
- Malhotra, K.; Noor, M.O.; Krull, U.J. Detection of cystic fibrosis transmembrane conductance regulator DeltaF508 gene mutation using a paper-based nucleic acid hybridization assay and a smartphone camera. Analyst 2018, 143, 3049–3058. [Google Scholar] [CrossRef] [PubMed]
- Gao, D.; Wang, D.D.; Zhang, Q.; Yang, F.Q.; Xia, Z.N.; Zhang, Q.H.; Yuan, C.S. In Vivo Selective Capture and Rapid Identification of Luteolin and Its Metabolites in Rat Livers by Molecularly Imprinted Solid-Phase Microextraction. J. Agric. Food Chem. 2017, 65, 1158–1166. [Google Scholar] [CrossRef] [PubMed]
- Silberberg, Y.R.; Kawamura, R.; Ryu, S.; Fukazawa, K.; Ishihara, K.; Nakamura, C. Detection of microtubules in vivo using antibody-immobilized nanoneedles. J. Biosci. Bioeng. 2014, 117, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Tehrani, F.; Teymourian, H.; Wuerstle, B.; Kavner, J.; Patel, R.; Furmidge, A.; Aghavali, R.; Hosseini-Toudeshki, H.; Brown, C.; Zhang, F.; et al. An integrated wearable microneedle array for the continuous monitoring of multiple biomarkers in interstitial fluid. Nat. Biomed. Eng. 2022, 6, 1214–1224. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Molinero-Fernandez, A.; Casanova, A.; Titulaer, J.; Campillo-Brocal, J.C.; Konradsson-Geuken, Å.; Crespo, G.A.; Cuartero, M. Intradermal Glycine Detection with a Wearable Microneedle Biosensor: The First In Vivo Assay. Anal. Chem. 2022, 94, 11856–11864. [Google Scholar] [CrossRef] [PubMed]
- Fang, L.; Liang, B.; Yang, G.; Hu, Y.; Zhu, Q.; Ye, X. A needle-type glucose biosensor based on PANI nanofibers and PU/E-PU membrane for long-term invasive continuous monitoring. Biosens. Bioelectron. 2017, 97, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Tehrani, F.; Teymourian, H.; Mack, J.; Shaver, A.; Reynoso, M.; Kavner, J.; Huang, N.; Furmidge, A.; Duvvuri, A.; et al. Microneedle Aptamer-Based Sensors for Continuous, Real-Time Therapeutic Drug Monitoring. Anal. Chem. 2022, 94, 8335–8345. [Google Scholar] [CrossRef] [PubMed]
- Fang, L.; Ren, H.; Mao, X.; Zhang, S.; Cai, Y.; Xu, S.; Zhang, Y.; Li, L.; Ye, X.; Liang, B. Differential Amperometric Microneedle Biosensor for Wearable Levodopa Monitoring of Parkinson’s Disease. Biosensors 2022, 12, 102. [Google Scholar] [CrossRef] [PubMed]
- Garg, S.K.; Kipnes, M.; Castorino, K.; Bailey, T.S.; Akturk, H.K.; Welsh, J.B.; Christiansen, M.P.; Balo, A.K.; Brown, S.A.; Reid, J.L.; et al. Accuracy and Safety of Dexcom G7 Continuous Glucose Monitoring in Adults with Diabetes. Diabetes Technol. Ther. 2022, 24, 373–380. [Google Scholar] [CrossRef]
- Christiansen, M.P.; Garg, S.K.; Brazg, R.; Bode, B.W.; Bailey, T.S.; Slover, R.H.; Sullivan, A.; Huang, S.; Shin, J.; Lee, S.W.; et al. Accuracy of a Fourth-Generation Subcutaneous Continuous Glucose Sensor. Diabetes Technol. Ther. 2017, 19, 446–456. [Google Scholar] [CrossRef] [PubMed]
- Garg, S.K.; Liljenquist, D.; Bode, B.; Christiansen, M.P.; Bailey, T.S.; Brazg, R.L.; Denham, D.S.; Chang, A.R.; Akturk, H.K.; Dehennis, A.; et al. Evaluation of Accuracy and Safety of the Next-Generation Up to 180-Day Long-Term Implantable Eversense Continuous Glucose Monitoring System: The PROMISE Study. Diabetes Technol. Ther. 2021, 24, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Javaid, M.; Haleem, A.; Singh, R.P.; Rab, S.; Suman, R. Exploring the potential of nanosensors: A brief overview. Sens. Int. 2021, 2, 100130. [Google Scholar] [CrossRef]
- Li, Y.; Deng, F.; Goldys, E.M. A simple and versatile CRISPR/Cas12a-based immunosensing platform: Towards attomolar level sensitivity for small protein diagnostics. Talanta 2022, 246, 123469. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Tian, R.; Wu, J.; Liu, S.; Wang, Y.; Wen, M.; Shang, Y.; Liu, Q.; Li, Y.; Guo, Y. A DNA origami-based aptamer nanoarray for potent and reversible anticoagulation in hemodialysis. Nat. Commun. 2021, 12, 358. [Google Scholar] [CrossRef] [PubMed]
- Fercher, C.; Jones, M.L.; Mahler, S.M.; Corrie, S.R. Recombinant antibody engineering enables reversible binding for continuous protein biosensing. ACS Sens. 2021, 6, 764–776. [Google Scholar] [CrossRef] [PubMed]
- Bhave, G.; Chen, J.C.; Singer, A.; Sharma, A.; Robinson, J.T. Distributed sensor and actuator networks for closed-loop bioelectronic medicine. Mater. Today 2021, 46, 125–135. [Google Scholar] [CrossRef] [PubMed]
- Grahn, P.J.; Mallory, G.W.; Khurram, O.U.; Berry, B.M.; Hachmann, J.T.; Bieber, A.J.; Bennet, K.E.; Min, H.-K.; Chang, S.-Y.; Lee, K.H.; et al. A neurochemical closed-loop controller for deep brain stimulation: Toward individualized smart neuromodulation therapies. Front. Neurosci. 2014, 8, 169. [Google Scholar] [CrossRef] [PubMed]
- Güemes Gonzalez, A.; Etienne-Cummings, R.; Georgiou, P. Closed-loop bioelectronic medicine for diabetes management. Bioelectron. Med. 2020, 6, 11. [Google Scholar] [CrossRef] [PubMed]
| Signal Transducer | Supporting Substrate | Functional Material | Recognition Module | Immobilisation Method | Detected Biomarker |
|---|---|---|---|---|---|
| Fluorescence signal | Optical fibre | Gold nanoparticle | Antibody | N-(3-Dimethylaminopropyl)-N′-ethylcarbodiimide(EDC)/N-Hydroxysuccinimide (NHS) | IL-1β [13] |
| Optical fibre | Streptavidin | Antibody | Biotin/streptavidin | IL-1β [8] | |
| Optical fibre | Streptavidin | Aptamer | Biotin/streptavidin | IFN-γ [29] | |
| Stainless steel | Poly(ethylene glycol) methyl ether methacrylate (PEG-MA) | Antibody | 1,1′-Carbonyldiimidazole(CDI) | IL-1β [11] | |
| Stainless steel | Polydopamine | Molecularly imprinted polymer (MIPs) | Synthesis | IL-1β [30] | |
| Electrochemical signal | Gold electrode | Graphene oxide | Antibody | EDC/NHS | IL-6 [31] |
| Silicon microelectrode | Gold disc | Antibody | Sulfosuccinimidyl 6-[3′-(2-pyridyldithio) propionamido] hexanoate (sulfo-LC-SPDP) | IL-6 [32] | |
| Silicon microelectrode | Gold film | Antibody | Physical adsorption | TNF-α [33] | |
| Glassy carbon electrode | Streptavidin | Aptamer | Biotin/streptavidin | IFN-γ [34] | |
| Glassy carbon electrode | Gold nanoparticle | Glucose receptor | Cysteine | Glucose [35] | |
| Stainless steel microneedle | Platinum black | - | - | Glucose [36] | |
| Polymer needle | Gold nanoparticles | Glucose oxidase | Electrical adsorption | Glucose [37] | |
| Silicon microneedle | Platinum layer | Glucose oxidase and lactate oxidase | Glutaraldehyde | Glucose and lactate [38] | |
| Platinum microelectrode | Polypyrrole | MIP | Synthesis | Dopamine [39] | |
| Pencil graphite electrode | - | - | - | Propofol [40] | |
| Graphite electrode | Chromium (III) hexacyanoferrate | Oxalate oxidase | Glutaraldehyde | Oxalate [41] | |
| Graphite electrode | Carboxymethylated dextran film | DNA | EDC/NHS | cDNA [42] | |
| Hypodermic needle | Photoresist | - | Spray coating | Thyroid cancer tissue [43] | |
| SPR | Optical fibre | Gold coating | Antibody | EDC/NHS | Cytokeratin 17 (CK17) [12] |
| SERS | Acupuncture needle | Gold nanoshells | 3,4-diaminobenzene-thiol | Thiol | Nitric oxide [44] |
| Microneedle | Silver layer | - | - | Glucose [10] |
| Biomarker Type | N-Biosensor | Detection Range and Sensitivity | Clinical Sample | Biomarkers | Clinical Application |
|---|---|---|---|---|---|
| Small protein | Antibody-based SPR biosensor | Range: 0.33 × 109–2.40 × 109 RBC/mL LOD: 0.33 × 109 RBC/mL | Blood | Blood group antigen [5] | - |
| Antibody-based microfluidic system Glycosylphosphatidylinositol | Range: 40 pM–40 fM LOD: 10 fM | Serum | Prostate specific antigen [66] | Prostate disorders and cancer | |
| (GPI) bioreceptor based electrochemical biosensor | Range: 1.0–10.0 IU/mL LOD: 0.31 IU/mL | Serum | Anti-GPI IgG and IgM [56] | Toxoplasma gondii | |
| Aptamer-based SPR biosensor | Range: 0–100 ng/mL LOD: - | Stool | IpaH [67] | Shigellosis | |
| Small molecule | Glucose biosensor | Range: 0.1–0.8 mM LOD: 0.1 mM | Serum | Glucose [68] | Diabetes |
| Pencil graphite biosensor | Range: 30–240 µM LOD: 7.2 µM | Serum | Propofol [40] | Anaesthetic | |
| MIP-based SPR biosensor | Range: 20–1000 ng/mL LOD: 9.9 ng/mL | Plasma | Procalcitonin [62] | Sepsis | |
| Amperometric biosensor | Range: 2.5–100 μM LOD: 2.5 μM | Urine | Oxalate [41] | Renal stones | |
| DNA | Electrochemical DNA sensor | Range: 8 × 10−16–5 × 10−10 mmol/L LOD: 2 × 10−16 mmol/L | Serum | DNA [4] | - |
| Colourimetric DNA biosensor | Range: 0.5–100 nM LOD: 0.2 nM | Serum | DNA [58] | Hepatitis B virus (HBV) gene | |
| Microorganism | Microfluidic system | Range of E. coli: 1 × 10–1 × 104 cfu/mL; | Saliva | E. coli, hPIC-3, varicella-zoster Virus [6] | Pathogenic microorganism related disease |
| DNA microarray | LOD: 103 cfu/mL; | Stool | Bacterial pathogens [7] | Diarrhoea | |
| Capillary electrophoresis | LOD: 9.0 × 105 cfu/mL; | Stool | Staphylococcus aureus [69] | Gastroenteritis | |
| Cell | Aptamer assay | - | Tumour tissue | Cancer cells [52] | - |
| Antibody assay | - | Blood | Lung circulating tumour cells [70] | Lung cancer |
| Signal Transducer | N-Biosensor | Detection Range and Sensitivity | In Vivo Detection Site | Biomarkers | Clinical Application |
|---|---|---|---|---|---|
| Fluorescence | Optical fibre-based antibody assay | Range: 3.9–500 pg/mL LOD: 1.2 pg/mL | Rat discrete brain regions | IL-1β [13] | Neuroinflammatory |
| Optical fibre-based antibody assay | Range: 3.13–400 pg/mL LOD: 1.12 pg/mL | Rat spinal cord | IL-1β [8] | - | |
| Stainless steel-based antibody assay | Range: 12.5–200 pg/mL LOD: 3.2 pg/mL | Rat intrathecal space | IL-1β [9] | Spinal cord injury | |
| Electrochemical | Aptasensor | Range: 10–500 pg/mL LOD: 10 pg/mL | Subcutaneous pockets | IFN-γ [34] | Inflammation |
| Antibody biosensor | Range: 1–300 pg/mL LOD: 1 pg/mL | Rat brain | IL-6 [31] | - | |
| Antibody biosensor | Range: - LOD: 1 nM | Skin phantom | TNF-α [33] | - | |
| MIP-based biosensor | Range: 10–100 nM LOD: 4.5 nM | Striatum | Dopamine [39] | Parkinson’s Disease | |
| Oxidase biosensor | - | Cerebral cortex | Glucose and lactate [38] | Cerebral metabolism | |
| SPR | Optical fibre-based biosensor | Range: 1 pg/mL–1 μg/mL LOD: 1 pg/mL | Lung | Cytokeratin 17 (CK17) [12] | Lung cancer |
| SERS | Microneedle-based assay | Range: 0–150 nM LOD: - | Skin phantom | Glucose [10] | - |
| Acupuncture needle-based assay | Range: 0–100 μM LOD: 1 nM | Fascia, brain, muscle | Nitric oxide [44] | Paracrine | |
| HPLC | Stainless steel fibre-based MIP assay | Range: 2.01–100.91 μg/mL LOD: 0.01 μg/mL | Liver | Luteolin [74] | Metabolism |
| AFM | Nanoneedle-based antibody biosensor | - | NIH3T3 cells | Tubulin [75] | Cytoskeleton-associated diseases |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xue, R.; Deng, F.; Guo, T.; Epps, A.; Lovell, N.H.; Shivdasani, M.N. Needle-Shaped Biosensors for Precision Diagnoses: From Benchtop Development to In Vitro and In Vivo Applications. Biosensors 2024, 14, 391. https://doi.org/10.3390/bios14080391
Xue R, Deng F, Guo T, Epps A, Lovell NH, Shivdasani MN. Needle-Shaped Biosensors for Precision Diagnoses: From Benchtop Development to In Vitro and In Vivo Applications. Biosensors. 2024; 14(8):391. https://doi.org/10.3390/bios14080391
Chicago/Turabian StyleXue, Ruier, Fei Deng, Tianruo Guo, Alexander Epps, Nigel H. Lovell, and Mohit N. Shivdasani. 2024. "Needle-Shaped Biosensors for Precision Diagnoses: From Benchtop Development to In Vitro and In Vivo Applications" Biosensors 14, no. 8: 391. https://doi.org/10.3390/bios14080391
APA StyleXue, R., Deng, F., Guo, T., Epps, A., Lovell, N. H., & Shivdasani, M. N. (2024). Needle-Shaped Biosensors for Precision Diagnoses: From Benchtop Development to In Vitro and In Vivo Applications. Biosensors, 14(8), 391. https://doi.org/10.3390/bios14080391





