The Human Gut Microbe Bacteroides thetaiotaomicron Suppresses Toxin Release from Clostridium difficile by Inhibiting Autolysis
Abstract
1. Introduction
2. Results
2.1. Effect of Bacteroides Species on CD Toxin Production
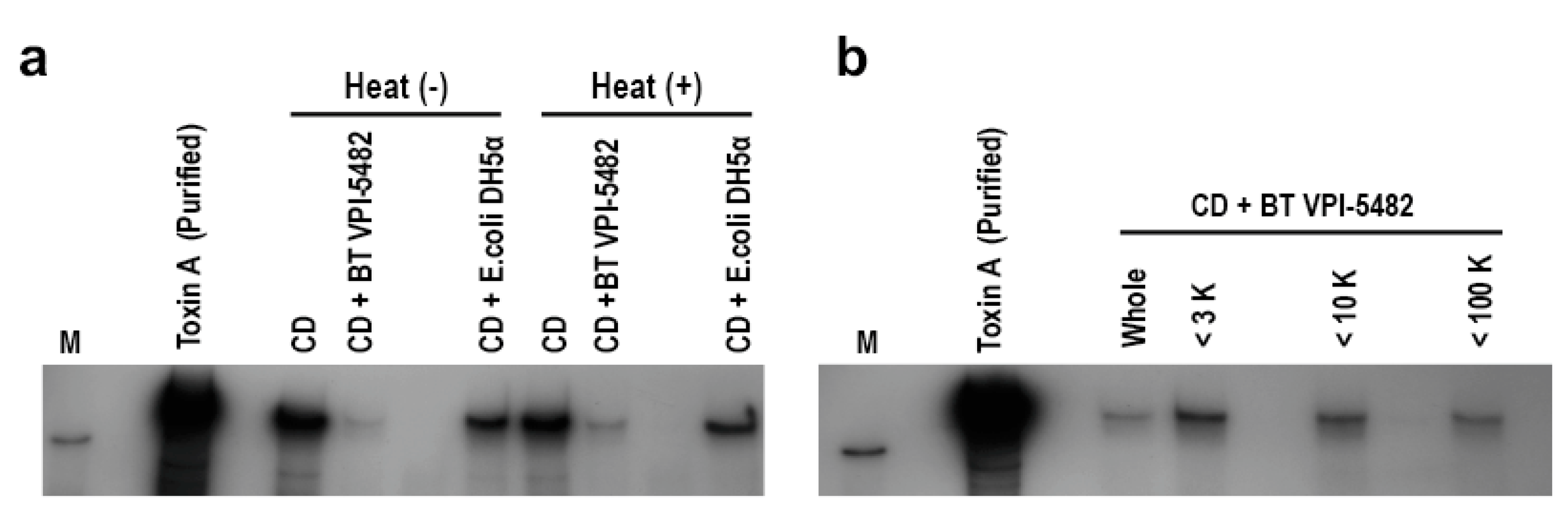
2.2. Characterization of BT-Derived Inhibitory Factors on CD Toxin Production
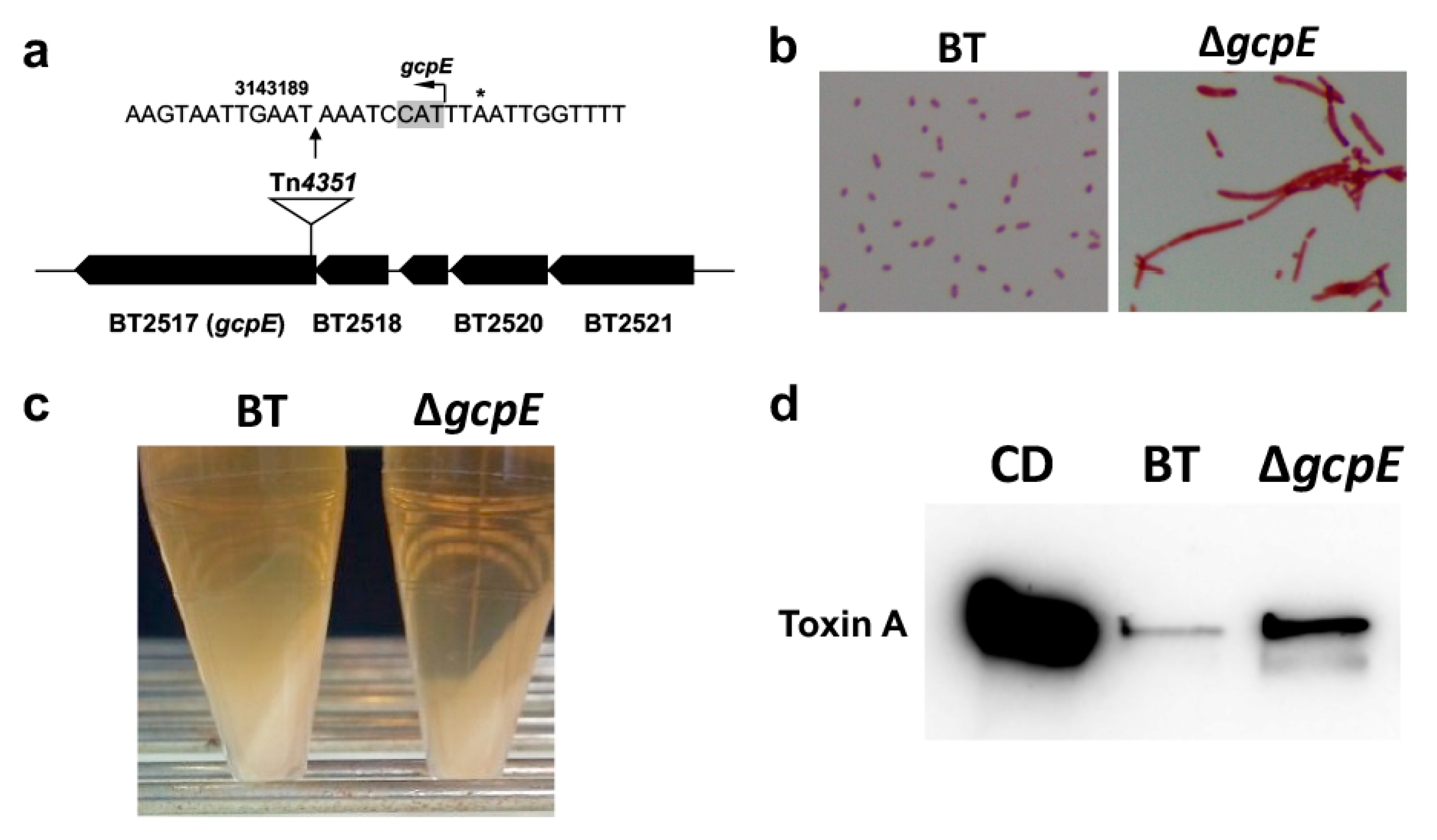
2.3. Construction of a Tn4351-Based Mutant Library and Screening to Identify the BT Genes Encoding Anti-Toxigenic Factors Against CD
2.4. Characterization of gcpE Mutant of BT
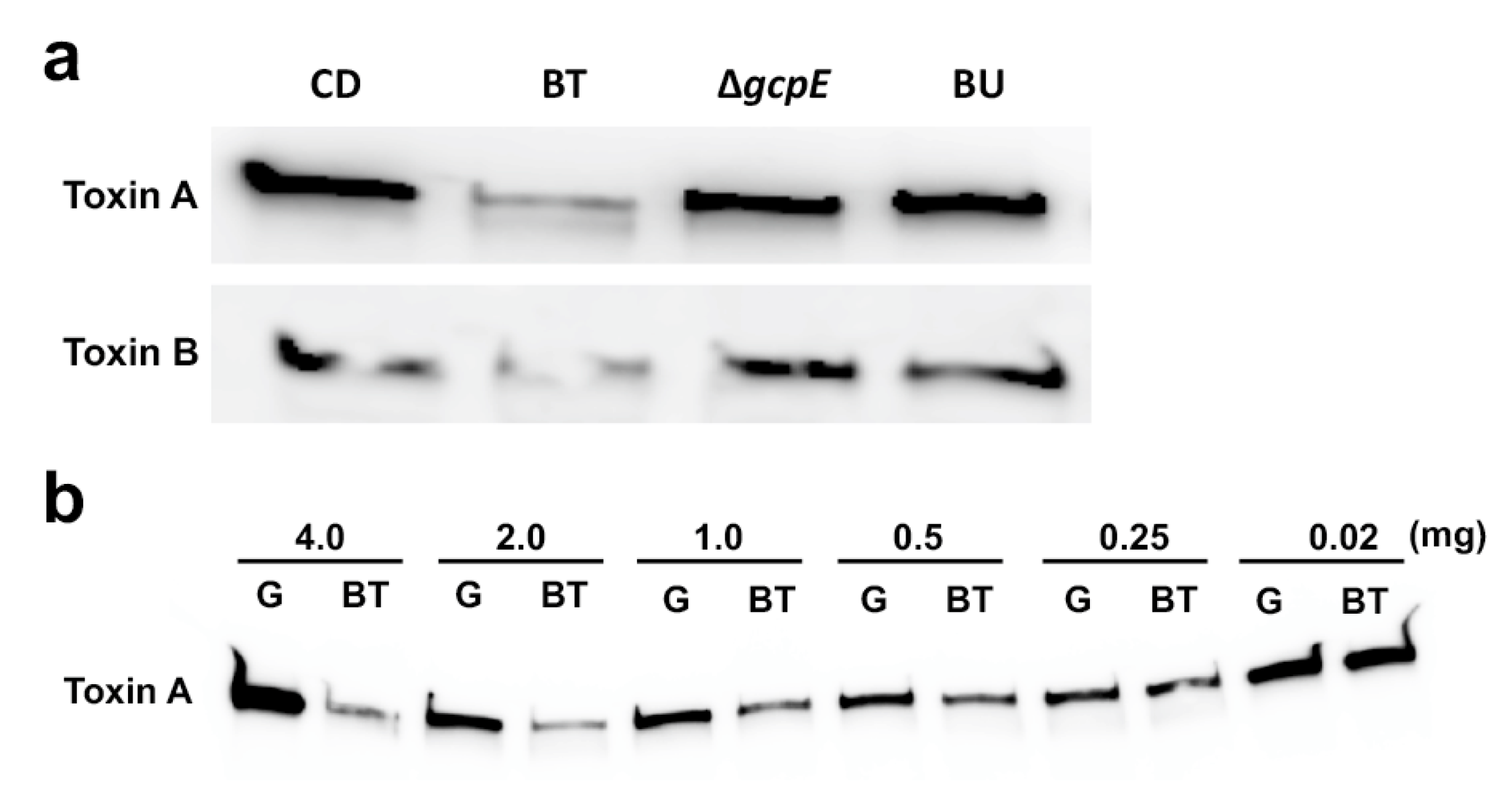
2.5. Inhibitory Effect of the Polysaccharide Fraction from BT Culture on CD Toxin Production
2.6. Transcriptional Analysis of PaLoc in CD
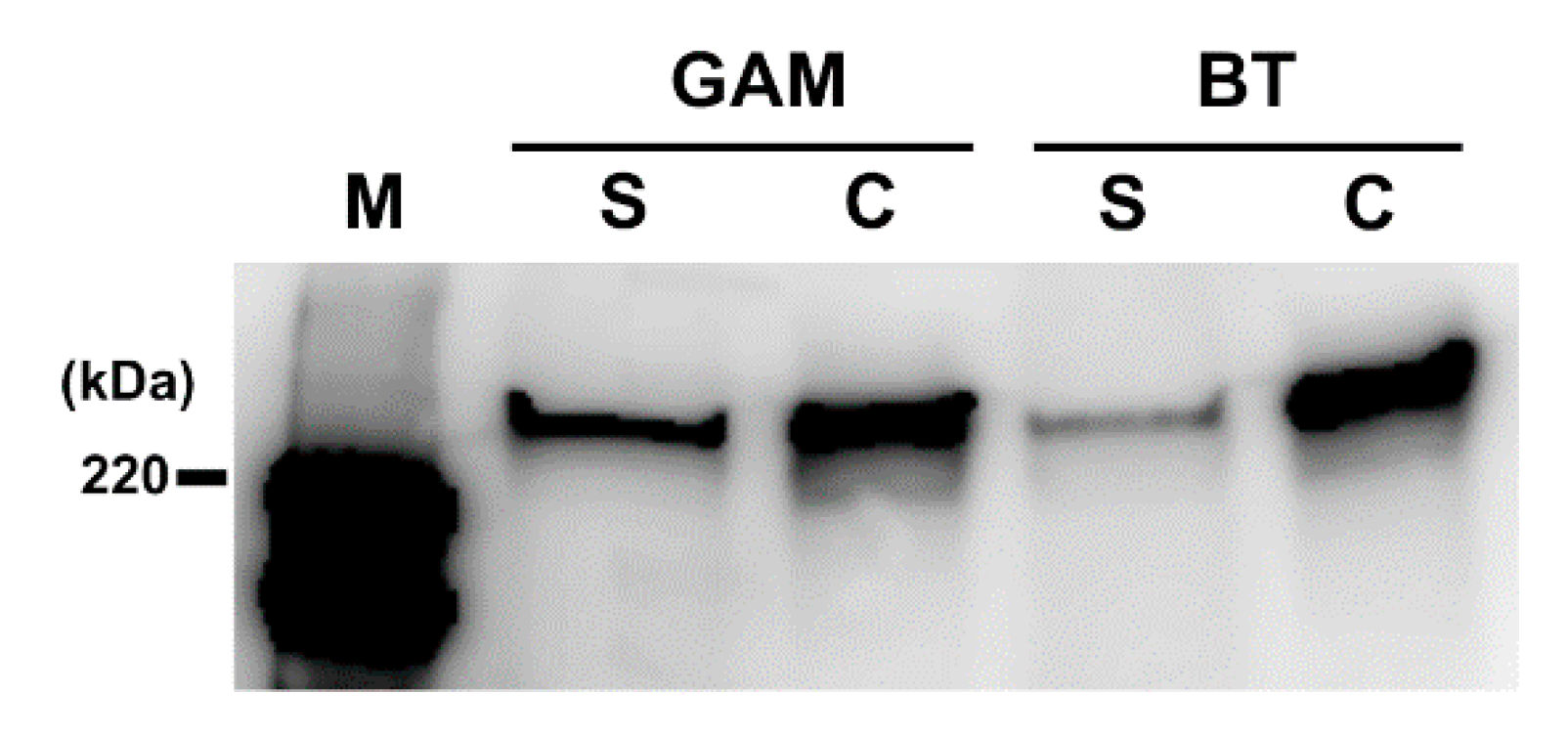
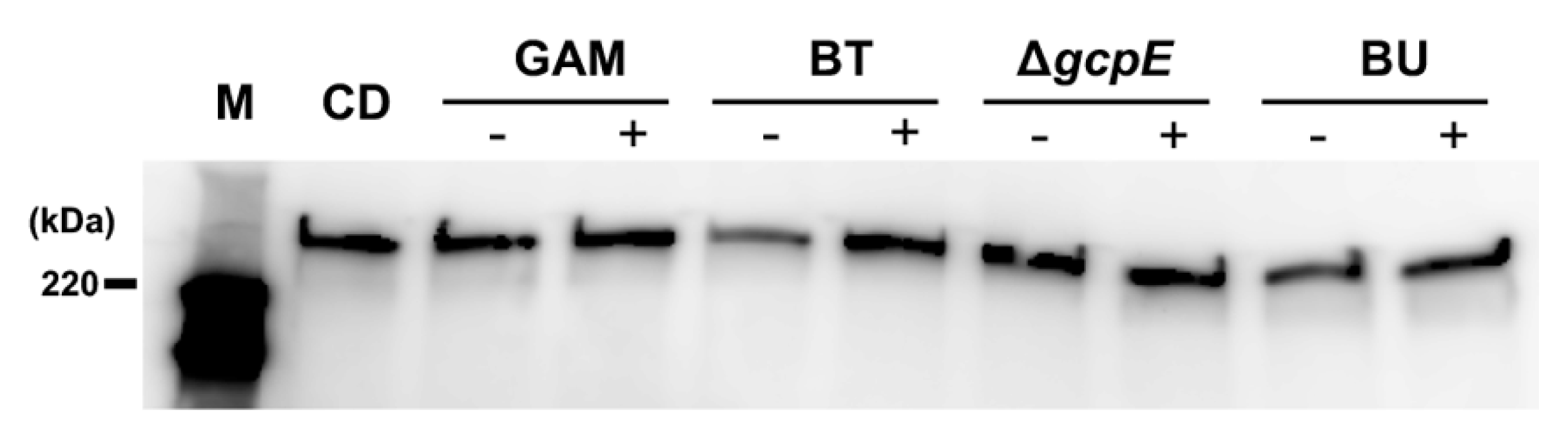
2.7. CD Toxin Localization Following Exposure to BT-Derived PF
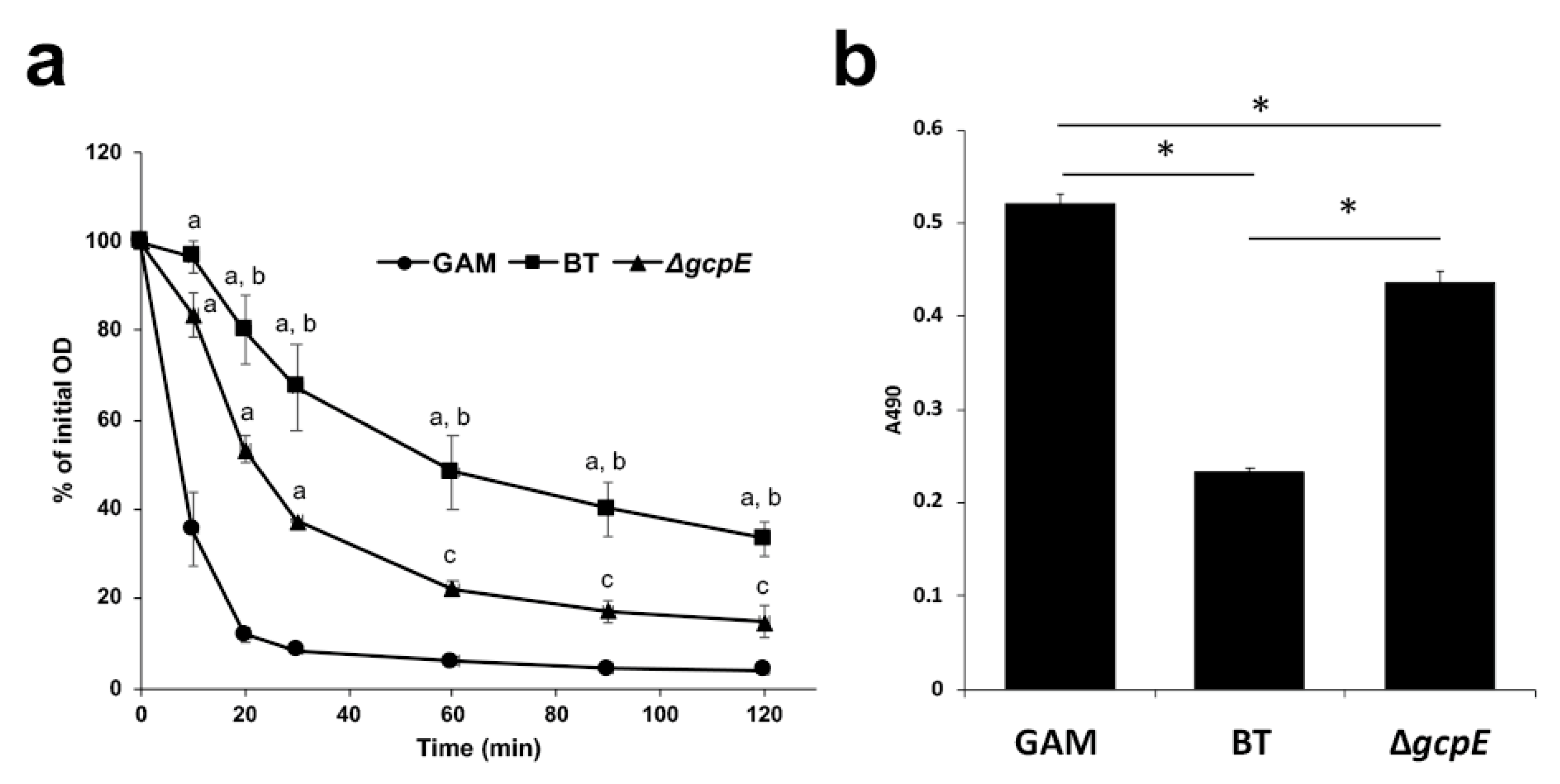
2.8. Autolysis Assay
2.9. Effect of Lysozyme Treatment
3. Discussion
4. Materials and Methods
4.1. Bacterial Strains and Growth Conditions
4.2. Preparation of Conditioned Medium
4.3. Cultivation of CD in Modified Medium
4.4. Microscopy Observation
4.5. Cytotoxicity Assay
4.6. Detection of Toxins A and B by Western Blotting
4.7. Characterization of the Inhibitory Components in BT Culture on CD Toxigenicity
4.8. Transposon Mutagenesis
4.9. Identification of Transposon Insertion Site
4.10. Partial Purification of Polysaccharide Fraction from Culture Supernatant
4.11. RNA Extraction and Reverse Transcription Quantitative PCR (qPCR)
4.12. Autolysis Assay
4.13. Measurement of Lactate Dehydrogenase (LDH) Activity
4.14. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McDonald, L.C.; Owings, M.; Jernigan, J.B. Clostridium difficile infection in patients discharged from US short-stay hospital, 1996 to 2003. Emerg. Infect. Dis. 2006, 12, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Luciano, J.A.; Zuckerbraun, B.S. Clostridium difficile infection: Prevention, treatment, and surgical management. Sug. Clin. North Am. 2014, 94, 1335–1349. [Google Scholar] [CrossRef]
- Martin, J.S.; Monaghan, T.M.; Wilcox, M.H. Clostridium difficile infection: Epidemiology, diagnosis and understanding transmission. Nat. Rev. Gastroenterol. Hepatol. 2016, 13, 206–216. [Google Scholar] [CrossRef] [PubMed]
- Dawson, L.F.; Valiente, E.; Donahue, E.H.; Birchenough, G.; Wren, B.W. Hypervirulent Clostridium difficile PCR ribotypes exhibit resistance to widely used disinfectants. PLoS ONE 2011, 6, e25754. [Google Scholar] [CrossRef]
- Zhang, S.; Palazuelos-Munoz, S.; Balsells, E.M.; Nair, H.; Chit, A.; Kyaw, M.H. Cost of hospital management of Clostridium difficile infection in United States-a meta-analysis and modelling study. BMC Infect. Dis. 2016, 16, 447. [Google Scholar] [CrossRef]
- von Eichel-Streiber, C.; Boquet, P.; Sauerborn, M.; Thelestam, M. Large clostridial cytotoxins - a family of glycosyltransferases modifying small GTP-binding proteins. Trends Microbiol. 1996, 4, 375–382. [Google Scholar] [CrossRef]
- Jank, T.; Giesemann, T.; Aktories, K. Rho-glucosylating Clostridium difficile toxins A and B: New insights into structure and function. Glycobiology 2007, 17, 15R–22R. [Google Scholar] [CrossRef] [PubMed]
- Aktories, K.; Schwan, C.; Jank, T. Clostridium difficile toxin biology. Annu Rev Microbiol. 2017, 71, 281–307. [Google Scholar] [CrossRef]
- Gerding, D.N.; Sambol, S.P.; Johnson, S. Non-toxigenic Clostridioides (Formerly Clostridium) difficile for prevention of C. difficile Infection: From bench to bedside back to bench and back to bedside. Front Microbiol. 2018, 9, 1700. [Google Scholar] [PubMed]
- Hunt, J.J.; Ballard, J.D. Variations in virulence and molecular biology among emerging strains of Clostridium difficile. Mol. Biol. Rev. 2013, 77, 567–581. [Google Scholar] [CrossRef] [PubMed]
- Hammond, G.A.; Johnson, J.L. The toxigenic element of Clostridium difficile strain VPI 10463. Microb. Pathog. 1995, 19, 203–213. [Google Scholar] [CrossRef]
- Hundsberger, T.; Braun, V.; Weidmann, M.; Leukel, P.; Sauerborn, M.; von Eichel-Streiber, C. Transcription analysis of the genes tcdA-E of the pathogenicity locus of Clostridium difficile. Eur. J. Biochem. 1997, 244, 735–742. [Google Scholar] [CrossRef]
- Mani, N.; Dupuy, B. Regulation of toxin synthesis in Clostridium difficile by an alternative RNA polymerase sigma factor. Proc. Natl. Acad. Sci. USA 2001, 98, 5844–5849. [Google Scholar] [CrossRef]
- Govind, R.; Dupuy, B. Secretion of Clostridium difficile toxins A and B requires the holin-like protein TcdE. PLoS Pathog. 2012, 8, e1002727. [Google Scholar] [CrossRef]
- McDonald, L.C.; Killgore, G.E.; Thompson, A.; Owens, R.C., Jr.; Kazakova, S.V.; Sambol, S.P.; Johnson, S.; Gerding, D.N. An epidemic, toxin gene-variant strain of Clostridium difficile. N. Engl. J. Med. 2005, 353, 2433–2441. [Google Scholar] [CrossRef]
- Bauer, K.A.; Johnston, J.E.W.; Wenzler, E.; Goff, D.A.; Cook, C.H.; Balada-Llasat, J.M.; Pancholi, P.; Mangino, J.E. Impact of the NAP-1 strain on disease severity, mortality, and recurrence of healthcare-associated Clostridium difficile infection. Anaerobe 2017, 48, 1–6. [Google Scholar] [CrossRef]
- Rao, K.; Micic, D.; Natarajan, M.; Winters, S.; Kiel, M.J.; Walk, S.T.; Santhosh, K.; Mogle, J.A.; Galecki, A.T.; LeBar, W.; et al. Clostridium difficile ribotype 027: Relationship to age, detectability of toxins A or B in stool with rapid testing, severe infection, and mortality. Clin. Infect. Dis. 2015, 61, 233–241. [Google Scholar] [CrossRef]
- Warny, M.; Pepin, J.; Fang, A.; Killgore, G.E.; Thompson, A.; Brazier, J.; Frost, E.; McDonald, L.C. Toxin production by an emerging strain of Clostridium difficile associated with outbreaks of severe disease in North America and Europe. Lancet 2005, 366, 1079–1084. [Google Scholar] [CrossRef]
- Loo, V.G.; Poirier, L.; Miller, M.A.; Oughton, M.; Libman, M.D.; Michaud, S.; Bourgault, A.M.; Nguyen, T.; Frenette, C.; Kelly, M.; et al. A predominantly clonal multi-institutional outbreak of Clostridium difficile-associated diarrhea with high morbidity and mortality. N. Engl. J. Med. 2005, 353, 2442–2449. [Google Scholar] [PubMed]
- Denève, C.; Janoir, C.; Poilane, I.; Fantinato, C.; Collignon, A. New trends in Clostridium difficile virulence and pathogenesis. Int. J. Antimicrob. Agents 2009, 33, S24–S28. [Google Scholar] [CrossRef]
- Mushtaq, A. New clinical recommendations for Clostridium difficile. Lancet Infect. Dis. 2018, 18, 384. [Google Scholar] [CrossRef]
- Kelly, C.P.; LaMont, J.T. Clostridium difficile – more difficult than ever. N. Engl. J. Med. 2008, 359, 1932–1940. [Google Scholar] [CrossRef]
- McFarland, L.V.; Surawicz, C.M.; Greenberg, R.N.; Fekety, R.; Elmer, G.W.; Moyer, K.A.; Melcher, S.A.; Bowen, K.E.; Cox, J.L.; Noorani, Z.; et al. A randomized placebo-controlled trial of Saccharomyces boulardii in combination with standard antibiotics for Clostridium difficile disease. JAMA 1994, 271, 1913–1918. [Google Scholar] [CrossRef] [PubMed]
- McFarland, L.V.; Elmer, G.W.; Surawics, C.M. Breaking the cycle: Treatment strategies for 163 cases of recurrent Clostridium difficile disease. Am. J. Gastroenterol. 2002, 97, 1769–1775. [Google Scholar] [CrossRef]
- van Nood, E.; Vrieze, A.; Nieuwdorp, M.; Fuentes, S.; Zoetendal, E.G.; de Vos, W.M.; Visser, C.E.; Kuijper, E.J.; Bartelsman, J.F.W.M.; Tijssen, J.G.P.; et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N. Engl. J. Med. 2013, 368, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Gough, E.; Shaikh, H.; Manges, A.R. Systematic review of intestinal microbiota transplantation (fecal bacteriotherapy) for recurrent Clostridium difficile infection. Clin. Infect. Dis. 2011, 53, 994–1002. [Google Scholar] [PubMed]
- Lawley, T.D.; Clare, S.; Walker, A.W.; Stares, M.D.; Connor, T.R.; Raisen, C.; Goulding, D.; Rad, R.; Schreiber, F.; Brandt, C.; et al. Targeted restoration of the intestinal microbiota with a simple, defined bacteriotherapy resolves relapsing Clostridium difficile disease in mice. PLoS Pathog. 2012, 8, e1002995. [Google Scholar] [CrossRef]
- Cordonnier, C.; Bihan, G.L.; Emond-Rheault, J.G.; Garrivier, A.; Harel, J.; Jubelin, G. Vitamin B12 uptake by the gut commensal bacteria Bacteroides thetaiotaomicron limits the production of Shiga toxin by enterohemorrhagic Escherichia coli. Toxins 2016, 8, 14. [Google Scholar] [CrossRef]
- Deng, H.; Yang, S.; Zhang, Y.; Qian, K.; Zhang, Z.; Liu, Y.; Wang, Y.; Bai, Y.; Fan, H.; Zhao, X.; et al. Bacteroides fragilis prevents Clostridium difficile infection in a mouse model by restoring gut barrier and microbiome regulation. Front Microbiol. 2018, 9, 2976. [Google Scholar] [CrossRef]
- Kelly, C.P. Fecal microbiota transplantation—An old therapy comes of age. N. Engl. J. Med. 2013, 368, 474–475. [Google Scholar] [CrossRef]
- Dupuy, B.; Sonenshein, A.L. Regulated transcription of Clostridium difficile toxin genes. Mol. Microbiol. 1998, 27, 107–120. [Google Scholar] [CrossRef]
- Egerer, M.; Giesemann, T.; Jank, T.; Satchell, K.J.; Aktories, K. Auto-catalytic cleavage of Clostridium difficile toxins A and B depends on cysteine protease activity. J. Biol. Chem. 2007, 282, 25314–25321. [Google Scholar] [CrossRef]
- Pruitt, R.N.; Lacy, D.B. Toward a structural understanding of Clostridium diffcile toxins A and B. Front. Cell Infect. Microbiol. 2012, 2, 28. [Google Scholar] [CrossRef] [PubMed]
- Reineke, J.; Tenzer, S.; Rupnik, M.; Koschinski, A.; Hasselmayer, O.; Schrattenholz, A.; Schild, H.; Von Eichel-Streiber, C. Autocatalytic cleavage of Clostridium difficile toxin B. Nature 2007, 446, 415–419. [Google Scholar] [CrossRef] [PubMed]
- Sebaihia, M.; Wren, B.W.; Mullany, P.; Fairweather, N.F.; Minton, N.; Stabler, R.; Thomson, N.R.; Roberts, A.P.; Cerdeño-Tárraga, A.M.; Wang, H.; et al. The multidrug-resistant human pathogen Clostridium difficile has a highly mobile, mosaic genome. Nature Genet. 2006, 38, 779–786. [Google Scholar] [CrossRef] [PubMed]
- Govind, R.; Fitzwater, L.; Nichols, R. Observations on the role of TcdE isoforms in Clostridium difficile toxin secretion. J. Bacteriol. 2015, 197, 2600–2609. [Google Scholar] [CrossRef]
- Olling, A.; Seehase, S.; Minton, N.P.; Tatge, H.; Schröter, S.; Kohlscheen, S.; Pich, A.; Just, I.; Gerhard, R. Release of TcdA and TcdB from Clostridium difficile cdi 630 is not affected by functional inactivation of the tcdE gene. Microb. Pathog. 2012, 52, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Wydau-Dematteis, S.; El Meouche, I.; Courtin, P.; Hamiot, A.; Lai-Kuen, R.; Saubaméa, B.; Fenaille, F.; Butel, M.J.; Pons, J.L.; Dupuy, B.; et al. Cwp19 is a novel lytic transglycosylase involved in stationary-phase autolysis resulting in toxin release in Clostridium difficile. mBio 2018, 9, e00648-18. [Google Scholar] [CrossRef] [PubMed]
- Shen, N.T.; Maw, A.; Tmanova, L.L.; Pino, A.; Ancy, K.; Crawford, C.V.; Simon, M.S.; Evans, A.T. Timely use of probiotics in hospitalized adults prevents Clostridium difficile infection: A systematic review with meta-regression analysis. Gastroenterology 2017, 152, 1889–1900.e9. [Google Scholar] [CrossRef]
- Yang, J.; Yang, H. Antibacterial activity of Bifidobacterium breve against Clostridioides difficile. Front. Cell Infect. Microbiol. 2019, 9, 288. [Google Scholar]
- Rätsep, M.; Kõljalg, S.; Sepp, E.; Smidt, I.; Truusalu, K.; Songisepp, E.; Stsepetova, J.; Naaber, P.; Mikelsaar, R.H.; Mikelsaar, M. A combination of the probiotic and prebiotic product can prevent the germination of Clostridium difficile spores and infection. Anaerobe 2017, 47, 94–103. [Google Scholar]
- Castagliuolo, I.; LaMont, J.T.; Nikulasson, S.T.; Pothoulakis, C. Saccharomyces boulardii protease inhibits Clostridium difficile toxin A effects in the rat ileum. Infect. Immun. 1996, 64, 5225–5232. [Google Scholar] [CrossRef]
- Bauer, M.P.; van Dissel, J.T.; Kuijper, E.J. Clostridium difficile: Controversies and approaches to management. Curr. Opin. Infect. Dis. 2009, 22, 517–524. [Google Scholar] [CrossRef] [PubMed]
- Kukla, M.; Adrych, K.; Dobrowolska, A.; Mach, T.; Reguła, J.; Rydzewska, G. Guidelines for Clostridium difficile infection in adults. Prz Gastroenterol. 2020, 15, 1–21. [Google Scholar]
- Medzhitov, R. Toll-like receptors and innate immunity. Nat. Rev. Immunol. 2001, 1, 135–145. [Google Scholar] [CrossRef]
- Pumbwe, L.; Skilbeck, C.A.; Wexler, H.M. The Bacteroides fragilis cell envelope: Quarterback, linebacker, coach-or all three? Anaerobe 2006, 12, 211–220. [Google Scholar] [CrossRef]
- Shah, I.M.; Laaberki, M.H.; Popham, D.; Dworkin, J. A eukaryotic-like Ser/Thr kinase signals bacteria to exit dormancy in response to peptidoglycan fragments. Cell 2008, 135, 486–496. [Google Scholar] [CrossRef]
- Elias, S.; Banin, E. Multi-species biofilms: Living with friendly neighbors. FEMS Microbiol. Rev. 2012, 36, 990–1004. [Google Scholar] [CrossRef] [PubMed]
- Kuwahara, T.; Yamashita, A.; Hirakawa, H.; Nakayama, H.; Toh, H.; Okada, N.; Kuhara, S.; Hattori, M.; Hayashi, T.; Ohnishi, Y. Genomic analysis of Bacteroides fragilis reveals extensive DNA inversions regulating cell surface adaptation. Proc. Natl. Acad. Sci. USA 2004, 101, 14919–14924. [Google Scholar] [CrossRef]
- Torres, J.; Camorlinga-Ponce, M.; Muñoz, O. Sensitivity in culture of epithelial cells from rhesus monkey kidney and human colon carcinoma to toxins A and B from Clostridium difficile. Toxicon 1992, 30, 419–426. [Google Scholar] [CrossRef]
- Ichimura, M.; Nakayama-Imaohji, H.; Wakimoto, S.; Morita, H.; Hayashi, T.; Kuwahara, T. Efficient electrotransformation of Bacteroides fragilis. Appl. Environ. Microbiol. 2010, 76, 3325–3332. [Google Scholar] [CrossRef] [PubMed]
- Ichimura, M.; Uchida, K.; Nakayama-Imaohji, H.; Hirakawa, H.; Tada, T.; Morita, H.; Yasutomo, K.; Okazaki, K.; Kuwahara, T. Mariner-based transposon mutagenesis for Bacteroides species. J. Basic Microbiol. 2014, 54, 558–567. [Google Scholar] [CrossRef] [PubMed]
- Camiade, E.; Peltier, J.; Bourgeois, I.; Couture-Tosi, E.; Courtin, P.; Antunes, A.; Chapot-Chartier, M.P.; Dupuy, B.; Pons, J.L. Characterization of Acp, a peptidoglycan hydrolase of Clostridium perfringens with N-acetylglucosaminidase activity that is implicated in cell separation and stress-induced autolysis. J. Bacteriol. 2010, 192, 2373–2384. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elahi, M.; Nakayama-Imaohji, H.; Hashimoto, M.; Tada, A.; Yamasaki, H.; Nagao, T.; Kuwahara, T. The Human Gut Microbe Bacteroides thetaiotaomicron Suppresses Toxin Release from Clostridium difficile by Inhibiting Autolysis. Antibiotics 2021, 10, 187. https://doi.org/10.3390/antibiotics10020187
Elahi M, Nakayama-Imaohji H, Hashimoto M, Tada A, Yamasaki H, Nagao T, Kuwahara T. The Human Gut Microbe Bacteroides thetaiotaomicron Suppresses Toxin Release from Clostridium difficile by Inhibiting Autolysis. Antibiotics. 2021; 10(2):187. https://doi.org/10.3390/antibiotics10020187
Chicago/Turabian StyleElahi, Miad, Haruyuki Nakayama-Imaohji, Masahito Hashimoto, Ayano Tada, Hisashi Yamasaki, Tamiko Nagao, and Tomomi Kuwahara. 2021. "The Human Gut Microbe Bacteroides thetaiotaomicron Suppresses Toxin Release from Clostridium difficile by Inhibiting Autolysis" Antibiotics 10, no. 2: 187. https://doi.org/10.3390/antibiotics10020187
APA StyleElahi, M., Nakayama-Imaohji, H., Hashimoto, M., Tada, A., Yamasaki, H., Nagao, T., & Kuwahara, T. (2021). The Human Gut Microbe Bacteroides thetaiotaomicron Suppresses Toxin Release from Clostridium difficile by Inhibiting Autolysis. Antibiotics, 10(2), 187. https://doi.org/10.3390/antibiotics10020187




