Adjuvant Transgingival Therapy with Visible Light Plus Water-Filtered Infrared-A (VIS + wIRA) in Periodontal Therapy—A Randomized, Controlled, Stratified, Double-Blinded Clinical Trial
Abstract
:1. Introduction
2. Results
2.1. Plaque Control Record (PCR)
2.2. Papilla Bleeding Index (PBI)
2.3. Probing Depths (PDs)
2.4. Bleeding on Probing (BOP)
2.5. Clinical Attachment Level (CAL)
2.6. Furcation
2.7. Tooth Mobility
2.8. Temperature Measurement
3. Discussion
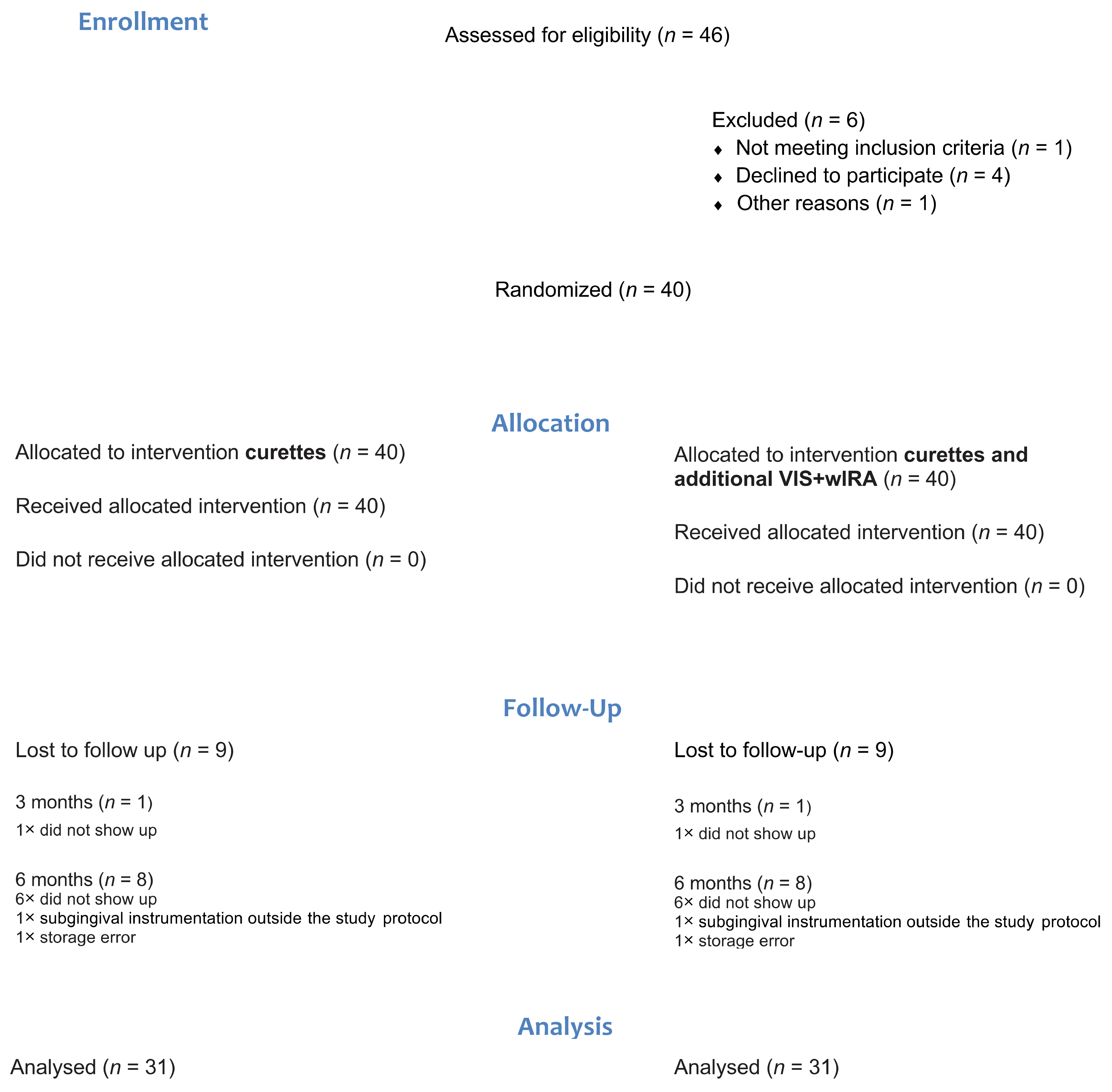
4. Materials and Methods
4.1. Inclusion Criteria
- Age ≥ 18 years;
- Untreated periodontal disease (at least two teeth with a probing depth (PD) ≥4 mm and ≤8 mm in diverse quadrants (the following combinations were possible: I/II, I/III, II/IV);
- No systematic periodontal treatment in the last 12 months;
- No antibiotic intake in the last 6 months [46];
- Maximum 30% smokers [47].
4.2. Exclusion Criteria
- Surgical periodontal therapy;
- Antibiotic intake during the study period;
- Pregnancy;
- Serious systemic conditions (for example, HIV, immunosuppression);
- Patients who needed antibiotic prophylaxis prior to the periodontal examination;
- Special anatomical tooth position such as infraposition, strong inclination, gingival overgrowth.
4.3. Care-Giver and Patient Recruitment
4.4. Clinical Measurements and Procedures
4.5. Temperature Measurement
4.6. Pain Perception
4.7. Sample Size and Statistical Considerations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kassebaum, N.J.; Bernabé, E.; Dahiya, M.; Bhandari, B.; Murray, C.J.L.; Marcenes, W. Global Burden of Severe Periodontitis in 1990–2010. J. Dent. Res. 2014, 93, 1045–1053. [Google Scholar] [CrossRef]
- Jepsen, S.; Deschner, J.; Braun, A.; Schwarz, F.; Eberhard, J. Calculus removal and the prevention of its formation. Periodontol. 2000 2010, 55, 167–188. [Google Scholar] [CrossRef]
- Slots, J. Position Paper: Systemic Antibiotics in Periodontics. J. Periodontol. 2004, 75, 1553–1565. [Google Scholar] [CrossRef]
- Anwar, H.; Strap, J.L.; Costerton, J.W. Establishment of aging biofilms: Possible mechanism of bacterial resistance to antimicrobial therapy. Antimicrob. Agents Chemother. 1992, 36, 1347–1351. [Google Scholar] [CrossRef] [Green Version]
- Rams, T.E.; Degener, J.E.; Van Winkelhoff, A.J. Antibiotic Resistance in Human Chronic Periodontitis Microbiota. J. Periodontol. 2014, 85, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, G.; Hartel, M.; Mercer, J.B. Heat for wounds–water-filtered infrared-A (wIRA) for wound healing—A review. Ger. Med. Sci. 2016, 14, Doc08. [Google Scholar]
- Fuchs, S.M.; Fluhr, J.W.; Bankova, L.; Tittelbach, J.; Hoffmann, G.; Elsner, P. Photodynamic therapy (PDT) and waterfiltered infrared A (wIRA) in patients with recalcitrant common hand and foot warts. Ger. Med. Sci. 2004, 2, Doc08. [Google Scholar] [PubMed]
- Bühring, M.; Kraft, K.; Matthiessen, P.F.; Resch, K.D.; Stange, R.; Stiller, N.; Uehleke, B. Hydro- und Thermotherapie. Naturheilverfahren: Und Unkonventionelle Medizinische Richtungen. Grundlagen, Methoden, Nachweissituationen, 31st ed.; Springer: Berlin/Heidelberg, Germany, 2004. [Google Scholar]
- Ostberg, J.R.; Repasky, E.A. Emerging evidence indicates that physiologically relevant thermal stress regulates dendritic cell function. Cancer Immunol. Immunother. 2006, 55, 292–298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Bruggen, I.; Robertson, T.; Papadimitriou, J. The effect of mild hyperthermia on the morphology and function of murine resident peritoneal macrophages. Exp. Mol. Pathol. 1991, 55, 119–134. [Google Scholar] [CrossRef]
- Yan, X.; Xiu, F.; An, H.; Wang, X.; Wang, J.; Cao, X. Fever range temperature promotes TLR4 expression and signaling in dendritic cells. Life Sci. 2007, 80, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Berglundh, T.; Donati, M. Aspects of adaptive host response in periodontitis. J. Clin. Periodontol. 2005, 32, 87–107. [Google Scholar] [CrossRef]
- Kinane, D.F.; Bartold, P.M. Clinical relevance of the host responses of periodontitis. Periodontol. 2000 2007, 43, 278–293. [Google Scholar] [CrossRef]
- Ohlrich, E.J.; Cullinan, M.P.; Seymour, G.J. The immunopathogenesis of periodontal disease. Aust. Dent. J. 2009, 54, S2–S10. [Google Scholar] [CrossRef]
- A Mackowiak, P.; Marling-Cason, M. Hyperthermic enhancement of serum antimicrobial activity: Mechanism by which fever might exert a beneficial effect on the outcome of gram-negative sepsis. Infect. Immun. 1983, 39, 38–42. [Google Scholar] [CrossRef] [Green Version]
- Curtis, M.A.; Percival, R.S.; Devine, D.; Darveau, R.P.; Coats, S.R.; Rangarajan, M.; Tarelli, E.; Marsh, P.D. Temperature-Dependent Modulation ofPorphyromonas gingivalisLipid A Structure and Interaction with the Innate Host Defenses. Infect. Immun. 2011, 79, 1187–1193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Percival, R.S.; Marsh, P.D.; Devine, D.A.; Rangarajan, M.; Aduse-Opoku, J.; Shepherd, P.; Curtis, M.A. Effect of temperature on growth, hemagglutination, and protease activity of Porphyromonas gingivalis. Infect. Immun. 1999, 67, 1917–1921. [Google Scholar] [CrossRef]
- Rattan, S.I.S.; Sejersen, H.; Fernandes, R.A.; Luo, W. Stress-Mediated Hormetic Modulation of Aging, Wound Healing, and Angiogenesis in Human Cells. Ann. N. Y. Acad. Sci. 2007, 1119, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Chung, E.; Sampson, A.C.; Rylander, M.N. Influence of Heating and Cyclic Tension on the Induction of Heat Shock Proteins and Bone-Related Proteins by MC3T3-E1 Cells. BioMed Res. Int. 2014, 2014, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Shui, C.; Scutt, A. Mild Heat Shock Induces Proliferation, Alkaline Phosphatase Activity, and Mineralization in Human Bone Marrow Stromal Cells and Mg-63 Cells In Vitro. J. Bone Miner. Res. 2001, 16, 731–741. [Google Scholar] [CrossRef]
- Karygianni, L.; Ruf, S.; Follo, M.; Hellwig, E.; Bucher, M.; Anderson, A.C.; Vach, K.; Al-Ahmad, A. Novel Broad-Spectrum Antimicrobial Photoinactivation ofIn SituOral Biofilms by Visible Light plus Water-Filtered Infrared A. Appl. Environ. Microbiol. 2014, 80, 7324–7336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hartel, M.; Hoffmann, G.; Wente, M.N.; Martignoni, M.E.; Büchler, M.W.; Friess, H. Randomized clinical trial of the influence of local water-filtered infrared A irradiation on wound healing after abdominal surgery. BJS 2006, 93, 952–960. [Google Scholar] [CrossRef] [PubMed]
- Künzli, B.M.; Liebl, F.; Nuhn, P.; Schuster, T.; Friess, H.; Hartel, M. Impact of Preoperative Local Water-Filtered Infrared A Irradiation on Postoperative Wound Healing. Ann. Surg. 2013, 258, 887–894. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, G. Principles and working mechanisms of water-filtered infrared-A (wIRA) in relation to wound healing. GMS Krankenhhyg Interdiszip. 2007, 2, 54. [Google Scholar]
- Hartel, M.; Illing, P.; Mercer, J.B.; Lademann, J.; Daeschlein, G.; Hoffmann, G. Therapy of acute wounds with water-filtered infrared-A (wIRA). GMS Krankenhhyg Interdiszip. 2007, 2, Doc53. [Google Scholar]
- Dirschka, T.; Radny, P.; Dominicus, R.; Mensing, H.; Brüning, H.; Jenne, L.; Karl, L.; Sebastian, M.; Oster-Schmidt, C.; Klövekorn, W.; et al. Photodynamic therapy with BF-200 ALA for the treatment of actinic keratosis: Results of a multicentre, randomized, observer-blind phase III study in comparison with a registered methyl-5-aminolaevulinate cream and placebo. Br. J. Dermatol. 2011, 166, 137–146. [Google Scholar] [CrossRef]
- Von Felbert, V.; Schumann, H.; Mercer, J.B.; Strasser, W.; Daeschlein, G.; Hoffmann, G. Therapy of chronic wounds with water-filtered infrared-A (wIRA). GMS Krankenhhyg Interdiszip. 2008, 2, Doc52. [Google Scholar]
- Rad, M.R.; Wise, G.E.; Brooks, H.; Flanagan, M.B.; Yao, S. Activation of proliferation and differentiation of dental follicle stem cells (DFSCs) by heat stress. Cell Prolif. 2012, 46, 58–66. [Google Scholar] [CrossRef]
- Mercer, J.B.; Nielsen, S.P.; Hoffmann, G. Improvement of wound healing by water-filtered infrared-A (wIRA) in patients with chronic venous stasis ulcers of the lower legs including evaluation using infrared thermography. Ger Med Sci 2008, 6, 19675738. [Google Scholar]
- Weerakoon, A.T.; Meyers, I.A.; Symons, A.L.; Walsh, L.J. Pulpal heat changes with newly developed resin photopolymerisa-tion systems. Aust. Endod. J. 2002, 28, 108–111. [Google Scholar] [CrossRef] [Green Version]
- A Copulos, T.; Low, S.B.; Walker, C.B.; Trebilcock, Y.Y.; Hefti, A.F. Comparative Analysis Between a Modified Ultrasonic Tip and Hand Instruments on Clinical Parameters of Periodontal Disease. J. Periodontol. 1993, 64, 694–700. [Google Scholar] [CrossRef]
- Haffajee, A.D.; Cugini, M.A.; Dibart, S.; Smith, C.; Kent, R.L.; Socransky, S.S. The effect of SRP on the clinical and microbiological parameters of periodontal diseases. J. Clin. Periodontol. 1997, 24, 324–334. [Google Scholar] [CrossRef]
- Kinane, D.F.; Radvar, M. A six-month comparison of three periodontal local antimicrobial therapies in persistent perio-dontal pockets. J. Periodontol. 1999, 70, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Pihlstrom, B.L.; McHuon, R.B.; Oliphant, T.H.; Ortiz-Campos, C. Comparison of surgical and nonsurgical treatment of periodontal disease A review of current studies and additional results after 6 1/2 years. J. Clin. Periodontol. 1983, 10, 524–541. [Google Scholar] [CrossRef] [PubMed]
- Badersten, A.; Nilveus, R.; Egelberg, J. Effect of nonsurgical periodontal therapy III. Single versus repeated instrumentation. J. Clin. Periodontol. 1984, 11, 114–124. [Google Scholar] [CrossRef]
- Badersten, A.; Nilveus, R.; Egelberg, J. Effect of nonsurgical periodontal therapy. I. Moderately advanced periodontitis. J. Clin. Periodontol. 1981, 8, 57–72. [Google Scholar] [CrossRef] [PubMed]
- Cugini, M.A.; Haffajee, A.D.; Smith, C.; Kent, R.L.; Socransky, S.S. The effect of scaling and root planing on the clinical and microbiological parameters of periodontal diseases: 12-month results. J. Clin. Periodontol. 2000, 27, 30–36. [Google Scholar] [CrossRef]
- Morrison, E.C.; Ramfjord, S.P.; Hill, R.W. Short-term effects of initial, nonsurgical periodontal treatment (hygienic phase). J. Clin. Periodontol. 1980, 7, 199–211. [Google Scholar] [CrossRef] [Green Version]
- Cobb, C.M. Clinical significance of non-surgical periodontal therapy: An evidence-based perspective of scaling and root planing. J. Clin. Periodontol. 2002, 29, 22–32. [Google Scholar] [CrossRef] [Green Version]
- Reddy, M.S.; Aichelmann-Reidy, M.E.; Avila-Ortiz, G.; Klokkevold, P.R.; Murphy, K.G.; Rosen, P.S.; Schallhorn, R.G.; Sculean, A.; Wang, H.-L. Periodontal Regeneration – Furcation Defects: A Consensus Report From the AAP Regeneration Workshop. J. Periodontol. 2015, 86, S131–S133. [Google Scholar] [CrossRef] [Green Version]
- Kruse, A.B.; Akakpo, D.L.; Maamar, R.; Woelber, J.P.; Al-Ahmad, A.; Vach, K.; Ratka-Krueger, P. Trehalose powder for subgingival air-polishing during periodontal maintenance therapy: A randomized controlled trial. J. Periodontol. 2018, 90, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Al-Ahmad, A.; Tennert, C.; Karygianni, L.; Wrbas, K.T.; Hellwig, E.; Altenburger, M.J. Antimicrobial photodynamic therapy using visible light plus water-filtered infrared-A (wIRA). J. Med Microbiol. 2013, 62, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Mongardini, C.; Di Tanna, G.L.; Pilloni, A. Light-activated disinfection using a light-emitting diode lamp in the red spec-trum: Clinical and microbiological short-term findings on periodontitis patients in maintenance. A randomized controlled split-mouth clinical trial. Lasers Med. Sci. 2014, 29, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Arweiler, N.B.; Pietruska, M.; Pietruski, J.; Skurska, A.; Dolińska, E.; Heumann, C.; Auschill, T.M.; Sculean, A. Six-month results following treatment of aggressive periodontitis with antimicrobial photodynamic therapy or amoxicillin and metronidazole. Clin. Oral Investig. 2014, 18, 2129–2135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Oliveira, R.R.; Schwartz-Filho, H.O.; Novaes, A.B.; Taba, M. Antimicrobial photodynamic therapy in the non-surgical treatment of aggressive periodontitis: A preliminary randomized controlled clinical study. J. Periodontol. 2007, 78, 965–973. [Google Scholar] [CrossRef] [PubMed]
- Goodrich, J.K.; Di Rienzi, S.C.; Poole, A.C.; Koren, O.; Walters, W.A.; Caporaso, J.G.; Knight, R.; Ley, R.E. Conducting a Microbiome Study. Cell 2014, 158, 250–262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lampert, T.; Von Der Lippe, E.; Muters, S. Verbreitung des Rauchens in der Erwachsenenbevölkerung in Deutschland. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2013, 56, 802–808. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ainamo, J.; Barmes, D.; Beagrie, G.; Cutress, T.; Martin, J.; Sardo-Infirri, J. Development of the World Health Organization (WHO) community periodontal index of treatment needs (CPITN). Int. Dent. J. 1982, 32, 281–291. [Google Scholar]
- O’>Leary, T.J.; Drake, R.B.; Naylor, J.E. The Plaque Control Record. J. Periodontol. 1972, 43, 38. [Google Scholar] [CrossRef]
- Saxer, U.P.; Mühlemann, H.R. Motivation und Aufklärung [Motivation and education]. SSO Schweiz Monatsschr Zahnheilkd. 1975, 85, 905–919. [Google Scholar]
- Grossi, S.G.; Dunford, R.G.; Ho, A.; Koch, G.; Machtei, E.E.; Genco, R.J. Sources of error for periodontal probing measurements. J. Periodontal Res. 1996, 31, 330–336. [Google Scholar] [CrossRef]
- Braun, A.; Jepsen, S.; Deimling, D.; Ratka-Krüger, P. Subjective intensity of pain during supportive periodontal treatment using a sonic scaler or an Er:YAG laser. J. Clin. Periodontol. 2010, 37, 340–345. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Parameter | |
|---|---|
| Participants | 40 (18 female, 22 male) |
| Number of treated quadrants (split-mouth) | n = 40 (VIS + wIRA); n = 40 (control) |
| Age, years | 54.43 (± 10.57) |
| Smoking status | 72.75% non-smokers, 27.5% smokers |
| Variable | Group | Baseline = BL (n Control = 113, n Test = 112) | Difference Value BL vs. 3 Months (n = 39) | p-Value | Difference Value BL vs. 6 Months (n = 31) | p-Value | |
|---|---|---|---|---|---|---|---|
| PCR % | Control | 21.46 (23.59) | 2.92 (0.22) | p = 0.375 | 2.80 (0.21) | p = 0.833 | |
| Test | 22.76 (23.38) | −0.59 (0.20) | 4.97 (0.26) | ||||
| PBI % | Control | 39.82 (75.04) | −5.08 (0.77) | p = 0.173 | −17.74 (0.71) | p = 0.265 | |
| Test | 42.85 (86.69) | −11.15 (0.79) | −23.27 (0.82) | ||||
| PD 1 (mm) | Control | 4.58 (0.65) | −0.83 (0.62) | p = 0.453 | −0.93 (0.53) | p = 0.278 | |
| Test | 4.58 (0.67) | −0.88 (0.53) | −1.03 (0.55) | ||||
| PD 2 (mm) | Control | 4.55 (0.68) | −0,86 (0.61) | p = 0.047 * | −1.10 (0.86) | p = 0.065 | |
| Test | 4.54 (0.67) | −0,99 (0.53) | −1.22 (0.86) | ||||
| BOP % | Control | 55.01 (28.68) | −16.64 (0.29) | p = 0.639 | −22.90 (0.30) | p = 0.991 | |
| Test | 51.63 (28.64) | −18.61 (0.22) | −25.12 (0.23) | ||||
| CAL (mm) | Control | 5.23 (1.40) | −0.86 (0.77) | p = 0.708 | −0.92 (0.69) | p = 0.794 | |
| Test | 5.22 (1.33) | −0.91 (0.68) | −0.95 (0.68) | ||||
| Furcation | mesial # | Control | 0.23 (0.60) | −0.01 (0.33) | p = 0.540 | 0.02 (0.33) | p = 0.992 |
| Test | 0.32 (0.75) | 0.03 (0.22) | −0.02 (0.50) | ||||
| distal # | Control | 0.59 (0.91) | −0.14 (0.60) | p = 0.576 | −0.16 (0.66) | p = 0.716 | |
| Test | 0.47 (0.79) | −0.11 (0.63) | −0.13 (0.68) | ||||
| vestibular # | Control | 0.56 (0.86) | −0.09 (0.56) | p = 0.920 | −0.13 (0.59) | p = 0.113 | |
| Test | 0.54 (0.78) | −0.06 (0.52) | −0.17 (0.56) | ||||
| Mobility # | Control | 0.25 (0.58) | −0.05 (0.38) | p = 0.519 | −0.08 (0.46) | p = 0.638 | |
| Test | 0.13 (0.43) | −0.02 (0.38) | −0.05 (0.40) |
| n | Mean | Std. Dev. | |||
|---|---|---|---|---|---|
| Sublingual temperature | 37 | 36.13 °C | 0.43 °C | ||
| Temperature posterior region | 0 min | Control | 37 | 35.38 °C | 0.73 °C |
| VIS + wIRA | 37 | 35.27 °C | 0.74 °C | ||
| 20 min | Control | 37 | 36.06 °C | 0.58 °C | |
| VIS + wIRA | 37 | 39.00 °C | 0.55 °C |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peikert, S.A.; Fischer, A.; Kruse, A.B.; Al-Ahmad, A.; Woelber, J.P.; Vach, K.; Braun, A.; Ratka-Krüger, P. Adjuvant Transgingival Therapy with Visible Light Plus Water-Filtered Infrared-A (VIS + wIRA) in Periodontal Therapy—A Randomized, Controlled, Stratified, Double-Blinded Clinical Trial. Antibiotics 2021, 10, 251. https://doi.org/10.3390/antibiotics10030251
Peikert SA, Fischer A, Kruse AB, Al-Ahmad A, Woelber JP, Vach K, Braun A, Ratka-Krüger P. Adjuvant Transgingival Therapy with Visible Light Plus Water-Filtered Infrared-A (VIS + wIRA) in Periodontal Therapy—A Randomized, Controlled, Stratified, Double-Blinded Clinical Trial. Antibiotics. 2021; 10(3):251. https://doi.org/10.3390/antibiotics10030251
Chicago/Turabian StylePeikert, Stefanie Anna, Anil Fischer, Anne Brigitte Kruse, Ali Al-Ahmad, Johan Peter Woelber, Kirstin Vach, Andreas Braun, and Petra Ratka-Krüger. 2021. "Adjuvant Transgingival Therapy with Visible Light Plus Water-Filtered Infrared-A (VIS + wIRA) in Periodontal Therapy—A Randomized, Controlled, Stratified, Double-Blinded Clinical Trial" Antibiotics 10, no. 3: 251. https://doi.org/10.3390/antibiotics10030251
APA StylePeikert, S. A., Fischer, A., Kruse, A. B., Al-Ahmad, A., Woelber, J. P., Vach, K., Braun, A., & Ratka-Krüger, P. (2021). Adjuvant Transgingival Therapy with Visible Light Plus Water-Filtered Infrared-A (VIS + wIRA) in Periodontal Therapy—A Randomized, Controlled, Stratified, Double-Blinded Clinical Trial. Antibiotics, 10(3), 251. https://doi.org/10.3390/antibiotics10030251










