Risk Factors of Daptomycin-Induced Eosinophilic Pneumonia in a Population with Osteoarticular Infection
Abstract
:1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Design, Setting, and Inclusion/Exclusion Criteria
4.2. Definitions and Clinical Data
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Osmon, D.R.; Berbari, E.F.; Berendt, A.R.; Lew, D.; Zimmerli, W.; Steckelberg, J.M.; Rao, N.; Hanssen, A.; Wilson, W.R. Diagnosis and management of prosthetic joint infection: Clinical practice guidelines by the infectious diseases Society of America. Clin. Infect. Dis. 2013, 56, 1–25. [Google Scholar] [CrossRef] [Green Version]
- Ariza, J.; Cobo, J.R.; Artetxe, J.B.-E.; de Benito Hernandez, N.; Tuneu, G.B.; Cabo, J.; Perez-Cardona, P.C.; Moreno, J.E.; Horcajada Gallego, J.P.; Lora-Tamayo, J.; et al. Management of Prosthetic Joint Infections. Clinical Practice Guidelines by the Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC). Available online: https://seimc.org/contenidos/gruposdeestudio/geio/dcientificos/documentos/geio-dc-2017-Guia_IPAS_EIMC.pdf (accessed on 1 April 2021).
- Falagas, M.E.; Giannopoulou, K.P.; Ntziora, F.; Papagelopoulos, P.J. Daptomycin for treatment of patients with bone and joint infections: A systematic review of the clinical evidence. Int. J. Antimicrob. Agents 2007, 30, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.-J.; Lee, M.S.; Lee, C.-H.; Lin, P.-C.; Kuo, F.-C. Daptomycin treatment in patients with resistant staphylococcal periprosthetic joint infection. BMC Infect. Dis. 2017, 17, 736. [Google Scholar] [CrossRef] [PubMed]
- Lora-Tamayo, J.; Parra-Ruiz, J.; Rodríguez-Pardo, D.; Barberán, J.; Ribera, A.; Tornero, E.; Pigrau, C.; Mensa, J.; Ariza, J.; Soriano, A. High doses of daptomycin (10 mg/kg/d) plus rifampin for the treatment of staphylococcal prosthetic joint infection managed with implant retention: A comparative study. Diagn. Microbiol. Infect. Dis. 2014, 80, 66–71. [Google Scholar] [CrossRef] [PubMed]
- He, W.; Zhang, Y.; Chen, H.; Zhao, C.; Wang, H. Efficacy and safety of daptomycin for the treatment of infectious disease: A meta-analysis based on randomized controlled trials. J. Antimicrob. Chemother. 2014, 69, 3181–3189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benvenuto, M.; Benziger, D.P.; Yankelev, S.; Vigliani, G. Pharmacokinetics and Tolerability of Daptomycin at Doses up to 12 Milligrams per Kilogram of Body Weight Once Daily in Healthy Volunteers. Antimicrob. Agents Chemother. 2006, 50, 3245–3249. [Google Scholar] [CrossRef] [Green Version]
- Silverman, J.A.; Mortin, L.I.; VanPraagh, A.D.G.; Li, T.; Alder, J. Inhibition of Daptomycin by Pulmonary Surfactant: In Vitro Modeling and Clinical Impact. J. Infect. Dis. 2005, 191, 2149–2152. [Google Scholar] [CrossRef] [PubMed]
- Allen, J.N. Drug-induced eosinophilic lung disease. Clin. Chest Med. 2004, 25, 77–88. [Google Scholar] [CrossRef]
- Hayes, D.; Anstead, M.I.; Kuhn, R.J. Eosinophilic pneumonia induced by daptomycin. J. Infect. 2007, 54, e211–e213. [Google Scholar] [CrossRef]
- Cobb, E.; Kimbrough, R.C.; Nugent, K.M.; Phy, M.P. Organizing Pneumonia and Pulmonary Eosinophilic Infiltration Associated with Daptomycin. Ann. Pharm. 2007, 41, 696–701. [Google Scholar] [CrossRef]
- Lal, Y.; Assimacopoulos, A.P. Two cases of daptomycin-induced eosinophilic pneumonia and chronic pneumonitis. Clin. Infect. Dis. 2010, 50, 737–740. [Google Scholar] [CrossRef] [PubMed]
- Miller, B.A.; Gray, A.; LeBlanc, T.W.; Sexton, D.J.; Martin, A.R.; Slama, T.G. Acute Eosinophilic Pneumonia Secondary to Daptomycin: A Report of Three Cases. Clin. Infect. Dis. 2010, 50, e63–e68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bartal, C.; Sagy, I.; Barski, L. Drug-induced eosinophilic pneumonia. Medicine 2018, 97, e9688. [Google Scholar] [CrossRef] [PubMed]
- Saleh-Mghir, A.; Muller-Serieys, C.; Dinh, A.; Massias, L.; Crémieux, A.-C. Adjunctive Rifampin Is Crucial to Optimizing Daptomycin Efficacy against Rabbit Prosthetic Joint Infection Due to Methicillin-Resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 2011, 55, 4589–4593. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- John, A.-K.; Baldoni, D.; Haschke, M.; Rentsch, K.; Schaerli, P.; Zimmerli, W.; Trampuz, A. Efficacy of Daptomycin in Implant-Associated Infection Due to Methicillin-Resistant Staphylococcus aureus: Importance of Combination with Rifampin. Antimicrob. Agents Chemother. 2009, 53, 2719–2724. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Durante-Mangoni, E.; Andini, R.; Parrella, A.; Mattucci, I.; Cavezza, G.; Senese, A.; Trojaniello, C.; Caprioli, R.; Diana, M.V.; Utili, R. Safety of treatment with high-dose daptomycin in 102 patients with infective endocarditis. Int. J. Antimicrob. Agents 2016, 48, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Roux, S.; Valour, F.; Karsenty, J.; Gagnieu, M.-C.; Perpoint, T.; Lustig, S.; Ader, F.; Martha, B.; Laurent, F.; Chidiac, C.; et al. Daptomycin > 6 mg/kg/day as salvage therapy in patients with complex bone and joint infection: Cohort study in a regional reference center. BMC Infect. Dis. 2016, 16, 83. [Google Scholar] [CrossRef] [Green Version]
- Hirai, J.; Hagihara, M.; Haranaga, S.; Kinjo, T.; Hashioka, H.; Kato, H.; Sakanashi, D.; Yamagishi, Y.; Mikamo, H.; Fujita, J. Eosinophilic pneumonia caused by daptomycin: Six cases from two institutions and a review of the literature. J. Infect. Chemother. 2017, 23, 245–249. [Google Scholar] [CrossRef]
- Uppal, P.; LaPlante, K.L.; Gaitanis, M.M.; Jankowich, M.D.; Ward, K.E. Daptomycin-induced eosinophilic pneumonia-a systematic review. Antimicrob. Resist. Infect. Control 2016, 5, 55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higashi, Y.; Nakamura, S.; Tsuji, Y.; Ogami, C.; Matsumoto, K.; Kawago, K.; Tokui, K.; Hayashi, R.; Sakamaki, I.; Yamamoto, Y. Daptomycin-induced eosinophilic pneumonia and a review of the published literature. Intern. Med. 2018, 57, 253–258. [Google Scholar] [CrossRef] [Green Version]
- Nickerson, M.; Bhargava, A.; Kale-Pradhan, P. Daptomycin-associated eosinophilic pneumonia with rechallenge: A case report. Int. J. Clin. Pharm. 2017, 55, 521–524. [Google Scholar] [CrossRef] [PubMed]
- Phillips, J.; Cardile, A.P.; Patterson, T.F.; Lewis, J.S. Daptomycin-induced acute eosinophilic pneumonia: Analysis of the current data and illustrative case reports. Scand. J. Infect. Dis. 2013, 45, 804–808. [Google Scholar] [CrossRef] [PubMed]
| Cases with DEP n = 11 | Cases without DEP n = 218 | HR (95% CI) | p-Value | |
|---|---|---|---|---|
| Age (median, IQR) | 77.4 (71.3–85.5) | 69.7 (55.6–78.1) | 1.06 (1.01–1.12) | 0.042 |
| <70 years | 1 | |||
| ≥70 years | 10 (91) | 108 (50) | 10.19 (1.28–80.93) | 0.028 |
| Female | 5 (45) | 104 (48) | 0.91 (0.27–3.08) | 0.884 |
| Comorbidities | ||||
| Charlson score (median, IQR) | 5 (4–7) | 4 (2–5) | 1.31 (1.03–1.67) | 0.031 |
| Chronic heart disease | 3 (30) | 27 (12) | 2.65 (0.66–10.62) | 0.168 |
| Chronic pulmonary disease | 3 (30) | 20 (9) | 3.71 (0.91–15.12) | 0.067 |
| Chronic kidney disease | 2 (20) | 56 (26) | 0.64 (0.13–3.07) | 0.579 |
| Analytical data (baseline) | ||||
| Creatinine (µmol/L) | 62 (49–70) | 72 (57–105) | 0.98 (0.960–1.005) | 0.134 |
| Leucocytes (×109 cells/L) | 10.1 (7.3–11) | 9.4 (7.2–12.3) | 0.965 (0.829–1.122) | 0.640 |
| Eosinophils (cells/µL; median, IQR) | 130 (30–230) | 100 (30–240) | 0.99 (0.996–1.003) | 0.709 |
| Analytical data (end of treatment) | ||||
| 2Creatine kinase (mkat/L) | 0.68 (0.31–0.89) | 0.87 (0.54–1.85) | 0.81 (0.498–1.316) | 0.395 |
| C-reactive protein (mg/L) | 223 (120–315) | 36 (17–83) | 1.01 (1.007–1.018) | <0.001 |
| Leucocytes (×109 cells/L) | 12.9 (9.5–15.4) | 7.8 (6–9.8) | 1.14 (1.035–1.258) | 0.008 |
| Eosinophils (cells/µL) | 650 (520–1410) | 220 (100–400) | 1.01 (1.002–1.004) | <0.001 |
| Daptomycin therapy | ||||
| Daily dose (mg; median, IQR) | 700 (700–700) | 700 (600–800) | 1 (0.99–1.01) | 0.719 |
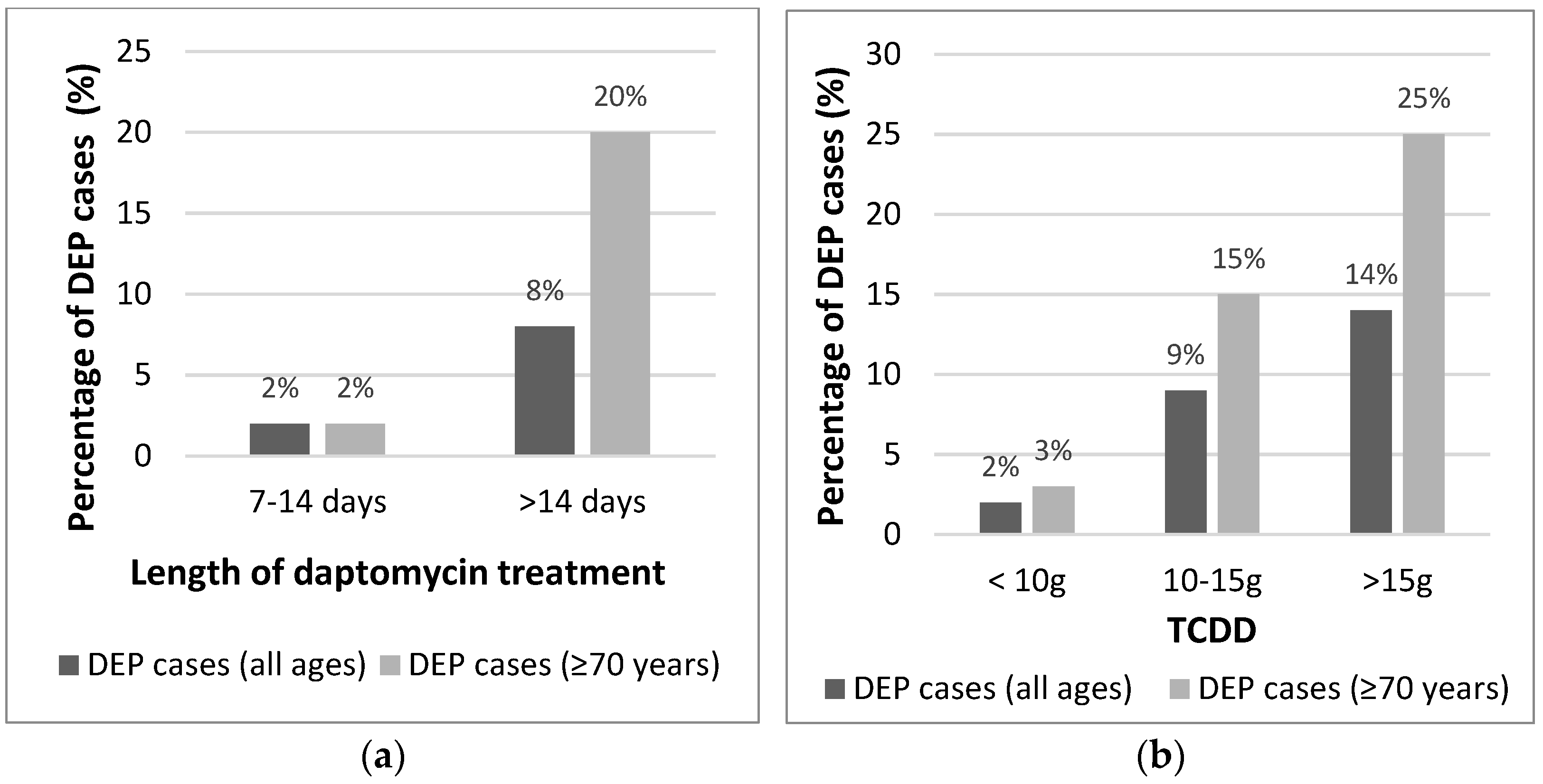
| Length (days; median, IQR) | 19 (12–25) | 7 (4–15) | 1.08 (1.03–1.14) | 0.005 |
| ≤14 days | 3 (27) | 162 (74) | 1 | |
| >14 days | 8 (73) | 56 (26) | 7.71 (1.98–30.09) | 0.003 |
| 1TCDD (g; median, IQR) | 13.2 (8.4–17.5) | 5.1 (2.4–11.2) | 1.11 (1.03–1.19) | 0.004 |
| <10 g | 3 (27) | 155 (71) | 1 | |
| 10–15 g | 4 (36) | 39 (18) | 5.30 (1.14–24.66) | 0.034 |
| >15 g | 4 (36) | 24 (11) | 8.61 (1.81–40.87) | 0.007 |
| Repeated exposure | 2 (20) | 23 (10) | 1.88 (0.38–9.26) | 0.435 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soldevila-Boixader, L.; Villanueva, B.; Ulldemolins, M.; Benavent, E.; Padulles, A.; Ribera, A.; Borras, I.; Ariza, J.; Murillo, O. Risk Factors of Daptomycin-Induced Eosinophilic Pneumonia in a Population with Osteoarticular Infection. Antibiotics 2021, 10, 446. https://doi.org/10.3390/antibiotics10040446
Soldevila-Boixader L, Villanueva B, Ulldemolins M, Benavent E, Padulles A, Ribera A, Borras I, Ariza J, Murillo O. Risk Factors of Daptomycin-Induced Eosinophilic Pneumonia in a Population with Osteoarticular Infection. Antibiotics. 2021; 10(4):446. https://doi.org/10.3390/antibiotics10040446
Chicago/Turabian StyleSoldevila-Boixader, Laura, Bernat Villanueva, Marta Ulldemolins, Eva Benavent, Ariadna Padulles, Alba Ribera, Irene Borras, Javier Ariza, and Oscar Murillo. 2021. "Risk Factors of Daptomycin-Induced Eosinophilic Pneumonia in a Population with Osteoarticular Infection" Antibiotics 10, no. 4: 446. https://doi.org/10.3390/antibiotics10040446
APA StyleSoldevila-Boixader, L., Villanueva, B., Ulldemolins, M., Benavent, E., Padulles, A., Ribera, A., Borras, I., Ariza, J., & Murillo, O. (2021). Risk Factors of Daptomycin-Induced Eosinophilic Pneumonia in a Population with Osteoarticular Infection. Antibiotics, 10(4), 446. https://doi.org/10.3390/antibiotics10040446







