Prevalence of Antimicrobial Resistance (AMR) Salmonella spp. and Escherichia coli Isolated from Broilers in the East Coast of Peninsular Malaysia
Abstract
:1. Introduction
2. Results
2.1. Prevalence of Salmonella spp. and E. coli in Broiler Farms in Kelantan, Terengganu, and Pahang
2.2. Salmonella and E. coli Susceptibility towards Antimicrobial Tested
2.2.1. Overall Salmonella and E. coli Susceptibility towards Antimicrobial Tested
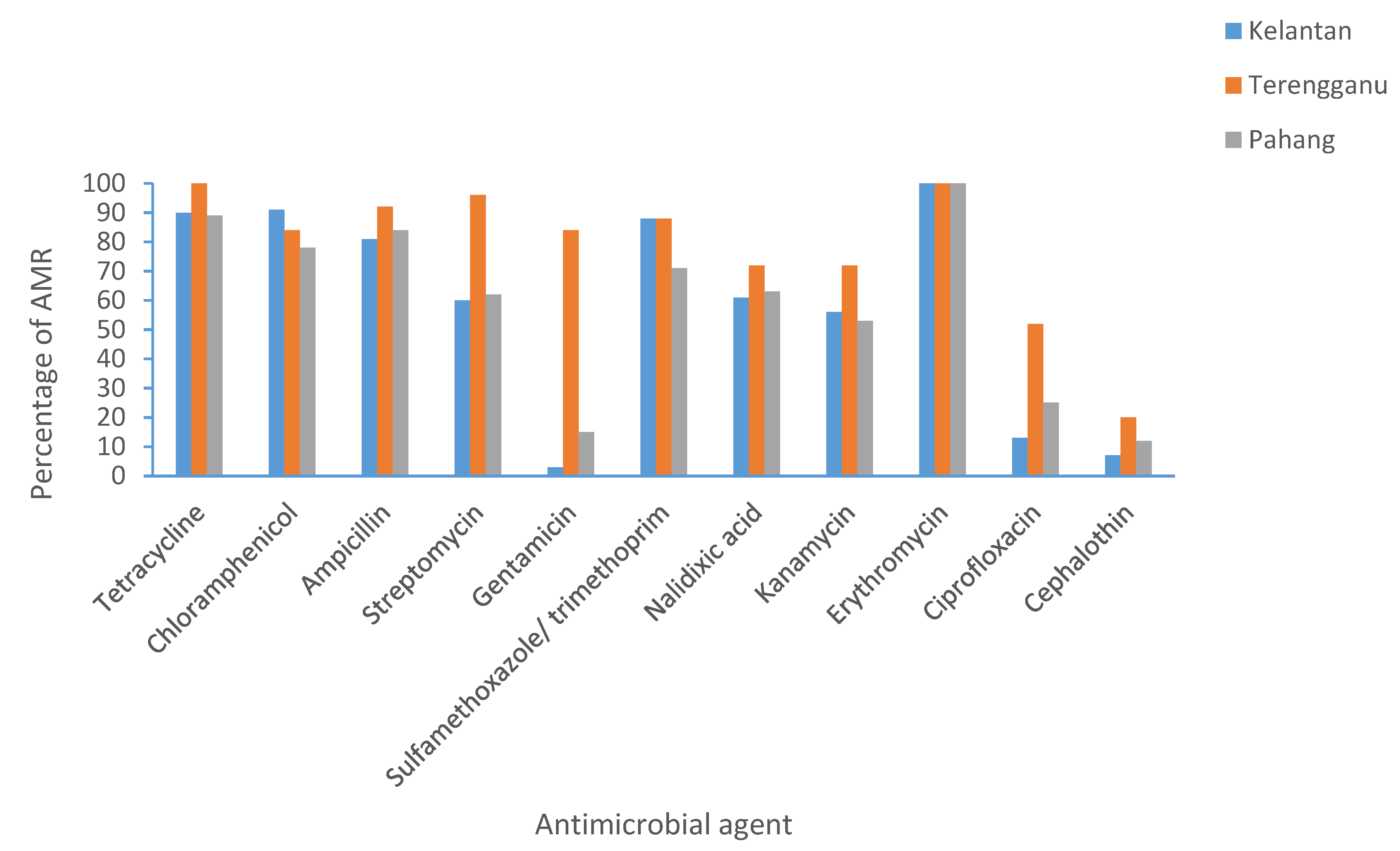
2.2.2. Distribution of Antimicrobial Resistance in Kelantan, Terengganu, and Pahang
2.2.3. Salmonella spp. and E. coli MDR Profile and Multiple Antimicrobial Resistance (MAR) Index
3. Discussion
4. Materials and Methods
4.1. Ethical Statement
4.2. Sampling Method and Sample Size Determination
4.3. Bacteria Isolation and Identification
4.4. Antimicrobial Sensitivity Test
4.5. Determination of Multiple Antimicrobial Resistance (MAR) Indexes
4.6. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Amna, N.; Mohammad, A.; Rosali, M.H. The Development and Future Direction of Malaysia’s Livestock Industry. FFTC-Agricultural Policy Platform (FFTC-AP) 2020. Available online: https://ap.fftc.org.tw/article/960 (accessed on 13 April 2021).
- Orissa International. Poultry Sector in South East Asia Iowa Economic Development Authority; Orissa International Pte. Ltd.: Singapore, 2017; Volume 1, pp. 4–9. [Google Scholar]
- Abu Daud, N.H.B.; Htin, N.N.; Abba, Y.; Paan, F.H.; Kyaw, T.; Khaing, A.T.; Jesse, F.F.A.; Mohammed, K.; Adamu, L.; Tijjani, A. An Outbreak of Colibacillosis in a Broiler Farm. J. Vet. Adv. 2014, 4, 646–651. [Google Scholar]
- Chuah, L.O.; Shamila Syuhada, A.K.; Mohamad Suhaimi, I.; Farah Hanim, T.; Rusul, G. Data on antibiogram and resistance genes harboured by Salmonella strains and their Pulsed-field gel electrophoresis clusters. Data Br. 2018, 17, 698–702. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.-M.; Lin, T.L.; Wu, C.C. Antimicrobial Susceptibility and Resistance of Chicken Escherichia coli, Salmonella spp., and Pasteurella multocida Isolates. Avian Dis. 2009, 53, 89–93. [Google Scholar] [CrossRef]
- Antunes, P.; Mourão, J.; Campos, J.; Peixe, L. Salmonellosis: The role of poultry meat. Clin. Microbiol. Infect. 2016, 22, 110–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mouttotou, N.; Ahmad, S.; Kamran, Z.; Koutoulis, K.V. Prevalence, Risks and Antibiotic Resistance of Salmonella in in Poultry Poultry Production Salmonella Production Chain. In Current Topics in Salmonella and Salmonellosis; IntechOpen: London, UK, 2016. [Google Scholar] [CrossRef]
- Nero, L.A. Highly Prevalent Multidrug-Resistant Salmonella from Chicken and Pork Meat at Retail Markets. Front. Microbiol. 2018, 9, 1–9. [Google Scholar]
- Bula-Rudas, F.J. Salmonella Infections in Childhood. Adv. Pediatr. 2015, 62, 29–58. [Google Scholar] [CrossRef]
- Kuang, X.; Hao, H.; Dai, M.; Wang, Y.; Ahmed, J.; Liu, Z.; Zonghui, Y. Serotypes and antimicrobial susceptibility of Salmonella spp. isolated from farm animals in China. Front. Microbiol. 2015, 6, 602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bin Kim, Y.; Young Yoon, M.; Su Ha, J.; Won Seo, K.; Bi Noh, E.; Son, S.H.; Lee, Y.J. Molecular characterisation of avian pathogenic Escherichia coli from broiler chickens with colibacillosis. Poult. Sci. 2020, 99, 1088–1095. [Google Scholar]
- Kabir, S.M.L. Avian Colibacillosis and Salmonellosis: A Closer Look at Epidemiology, Pathogenesis, Diagnosis, Control and Public Health Concerns. Int. J. Environ. Res. Public Health 2010, 7, 89–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fancher, C.A.; Zhang, L.; Kiess, A.S.; Adhikari, P.A.; Dinh, T.T.N.; Sukumaran, A.T. Avian pathogenic Escherichia coli and clostridium perfringens: Challenges in no antibiotics ever broiler production and potential solutions. Microorganisms 2020, 8, 1533. [Google Scholar] [CrossRef] [PubMed]
- Ricke, S.C.; Rothrock, M.J. Gastrointestinal microbiomes of broilers and layer hens in alternative production systems. Poult. Sci. 2020, 99, 660–669. [Google Scholar] [CrossRef]
- Yang, S.C.; Lin, C.H.; Aljuffali, I.A.; Fang, J.Y. Current pathogenic Escherichia coli food-borne outbreak cases and therapy development. Arch. Microbiol. 2017, 199, 811–825. [Google Scholar] [CrossRef] [PubMed]
- Koutsianos, D.; Gantelet, H.; Franzo, G.; Lecoupeur, M.; Thibault, E.; Cecchinato, M.; Koutoulis, K.C. An assessment of the level of protection against colibacillosis conferred by several autogenous and/or commercial vaccination programs in conventional pullets upon experimental challenge. Vet. Sci. 2020, 7, 80. [Google Scholar] [CrossRef]
- Teillant, A.; Laxminarayan, R. Economics of Antibiotic Use in USA. Swine and Poultry Production. Choices 2015, 30, 1–11. [Google Scholar]
- Van den Bogaard, E.A.; Stobberingh, E.E. Antibiotic Usage in Animals. Drugs 1999, 58, 589–607. [Google Scholar] [CrossRef]
- O’Neill, J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. Review on Antimicrobial Resistance; Wellcome Trust: London, UK, 2016; pp. 10–16. [Google Scholar]
- Alreshidi, M.N.; Neela, M.A.; Alsharari, V.; Hamat, A.S.; Alsalamah, R.A.; Atshan, A.A.; Alzoghaibi, S.S.; Shamsudin, O. Molecular typing and antibiotic resistance patterns of methicillin-resistant Staphylococcus aureus isolates from clinical samples in Malaysia: An update. Trop. Biomed. 2017, 34, 1–6. [Google Scholar]
- Nhung, N.T.; Chansiripornchai, N.; Carrique-Mas, J.J. Antimicrobial Resistance in Bacterial Poultry Pathogens: A Review. Front. Vet. Sci. 2017, 4, 126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Geidam, Y.; Zakaria, Z.; Aziz, S.A.; Bejo, S.K.; Abu, J.; Omar, S. High Prevalence of Multi-drug Resistant Bacteria in Selected Poultry Farms in Selangor, Malaysia. Asian J. Anim. Vet. Adv. 2012, 7, 891–897. [Google Scholar] [CrossRef]
- Jajere, S.M.; Hassan, L.; Aziz, S.A.; Zakaria, Z.; Abu, J.; Nordin, F.; Faiz, N.M. Salmonella in native ‘village’ chickens Gallus domesticus Prevalence and risk factors from farms in South-Central Peninsular Malaysi. Poult. Sci. 2015. [Google Scholar] [CrossRef]
- Gonçalves-Tenório, A.; Nunes Silva, B.; Rodrigues, V.; Cadavez, V.; Gonzales-Barron, U. Prevalence of pathogens in poultry meat: A meta-analysis of European published surveys. Foods 2018, 7, 69. [Google Scholar] [CrossRef] [Green Version]
- Islam, J.; Ahmed, T.; Hasan, K. Isolation and identification of Salmonella spp. from broiler and their antibiogram study in Sylhet, Bangladesh. J. Appl. Biol. Biotechnol. 2017, 4, 46–51. [Google Scholar]
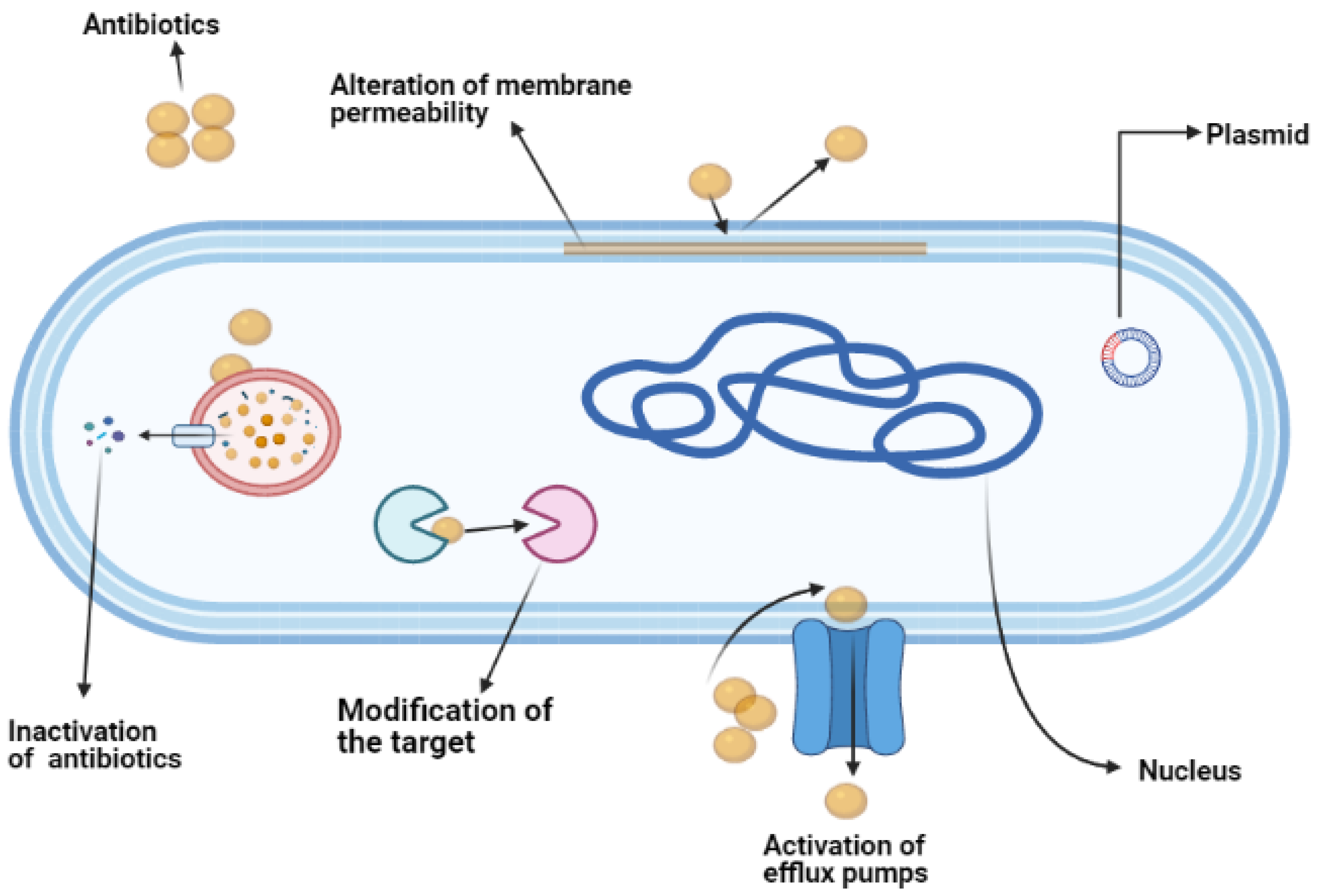
- McManus, M.C. Mechanisms of bacterial resistance to antimicrobial agents. Am. J. Health Syst. Pharm. 1997, 54, 1420–1433. [Google Scholar] [CrossRef] [PubMed]
- Reygaert, W.C. An overview of the antimicrobial resistance mechanisms of bacteria. AIMS Microbiol. 2018, 4, 482–501. [Google Scholar] [CrossRef]
- Tenover, F.C. Mechanisms of antimicrobial resistance in bacteria. Am. J. Infect. Control 2006, 34, S3–S10. [Google Scholar] [CrossRef]
- Thrusfield, M.V. Sample size determination. In Veterinary Epidemiology; Wiley-Blackwell: Hoboken, NJ, USA, 2007. [Google Scholar]
- Ajijur, M.; Rahman, M.M.; Amin, R.; Begum, I.A.; Fries, R.; Husna, A.; Khairalla, A.S.; Badruzzaman, A.T.M.; Zowalaty, M.E.E.; Lampang, K.N.; et al. Susceptibility and Multidrug Resistance Patterns of Escherichia coli Isolated from Cloacal Swabs of Live Broiler Chickens in Bangladesh. Pathogens 2019, 8, 118. [Google Scholar]
- CLSI. Clinical and Laboratory Standards Institute: Performance Standards for Antimicrobial Susceptibility Testing Supplement M100S; CLSI: Junction, MD, USA, 2016. [Google Scholar]
- Christopher, A.F.; Hora, S.; Ali, Z. Investigation of plasmid profile, antibiotic susceptibility pattern multiple antibiotic resistance index calculation of Escherichia coli isolates obtained from different human clinical specimens at tertiary care hospital in Bareilly-India. Ann. Trop. Med. Public Health 2013, 6, 285–289. [Google Scholar] [CrossRef]
- Akande, E.B.; Abodunrin, T.F.; Oladejo, B.O.; Oladunmoye, M.K. Antibiogram and plasmid profiling of resistance bacteria isolated from the blood of Hepatitis C Virus positive individuals. J. Microbiol. Exp. 2019, 7, 156–165. [Google Scholar]


| State/Locality | No. of Samples | Prevalence of Salmonella spp. | Prevalence of E. coli |
|---|---|---|---|
| Kelantan | |||
| Machang | 40 | 0% | 50% |
| Bachok | 40 | 15% | 45% |
| Tumpat | 40 | 12.5% | 62.5% |
| Pasir Mas | 40 | 7.5% | 37.5% |
| Jeli | 40 | 0% | 55% |
| Total | 200 | 7% | 50% |
| Terengganu | |||
| Marang | 30 | 0% | 33.3% |
| Hulu Terengganu | 30 | 13.3% | 63.3% |
| Total | 60 | 6.5% | 48.3% |
| Pahang | |||
| Kuantan | 32 | 0% | 65.6% |
| Pekan | 32 | 0% | 59.4% |
| Maran | 30 | 13.3% | 33.3% |
| Temerloh | 30 | 10% | 66.6% |
| Total | 120 | 5.8% | 58.0% |
| Overall | 384 | 6.5% | 51.8% |
| Pathogens/Antimicrobials | Susceptible (%) | Intermediate (%) | Resistant (%) | |||
|---|---|---|---|---|---|---|
| Salmonella | E. coli | Salmonella | E. coli | Salmonella | E. coli | |
| Tetracycline | 38 | 5.3 | 0 | 0 | 62 | 94.6 |
| Chloramphenicol | 23.8 | 14.8 | 0 | 0.5 | 76.2 | 84.5 |
| Ampicillin | 52.3 | 12 | 0 | 0.5 | 47.7 | 87.5 |
| Streptomycin | 76.1 | 31 | 4.7 | 3 | 19 | 66 |
| Gentamicin | 100 | 75.6 | 0 | 4.2 | 0 | 20.2 |
| Sulfamethoxazole/trimethoprim | 57.1 | 16 | 0 | 0.5 | 42.9 | 83.3 |
| Nalidixic acid | 90.4 | 39.3 | 0 | 0 | 9.6 | 60.7 |
| Kanamycin | 71.4 | 43 | 0 | 0 | 28.6 | 57 |
| Erythromycin | 0 | 0 | 0 | 0 | 100 | 100 |
| Ciprofloxacin | 95.2 | 72 | 0 | 4.2 | 4.8 | 23.8 |
| Cephalothin | 100 | 87 | 0 | 2 | 0 | 11 |
| Colistin sulphate | 100 | 100 | 0 | 0 | 0 | 0 |
| No of Antimicrobials | Salmonella | E. coli | ||||
|---|---|---|---|---|---|---|
| MDR Profile | % of Isolates | MAR Index | MDR Profile | % of Isolates | MAR Index | |
| 12 | N/A | N/A | N/A | N/A | N/A | N/A |
| 11 | N/A | N/A | N/A | TE-C-AMP-S-CN-SXT-NA-K-E-CIP-CL | 1.2 | 0.9 |
| 10 | N/A | N/A | N/A | TE-C-AMP-S-CN-SXT-NA-K-E-CIP, TE-C-S-CN-SXT-NA-K-E-CIP-CL, TE-C-AMP-S-CN-NA-K-E-CIP-CL | 5.9 | 0.8 |
| 9 | N/A | N/A | N/A | TE-C-AMP-S-CN-SXT-NA-K-E TE-C-AMP-S-SXT-NA-K-E-CIP TE-C-AMP-S-SXT-K-E-CIP-CL TE-C-AMP-S-NA-K-E-CIP-CL C-AMP-S-CN-SXT-NA-K-E-CIP TE-C-AMP-S-CN-SXT-NA-E-CIP | 10.7 | 0.7 |
| 8 | TE-C-AMP-S-SXT-K-E-CIP | 4.8 | 0.7 | TE-C-AMP-S-CN-SXT-E-CL TE-C-AMP-S-SXT-NA-K-E TE-C-AMP-S-SXT-NA-K-E TE-C-AMP-S-CN-SXT-K-E TE-C-AMP-S-CN-SXT-K-E TE-C-AMP-S-NA-K-E-CIP TE-C-AMP-S-CN-NA-K-E TE-AMP-S-CN-SXT-NA-K-E | 21.4 | 0.6 |
| 7 | TE-C-S-SXT-NA-K-E | 4.8 | 0.6 | TE-C-AMP-S-SXT-NA-E TE-C-AMP-SXT-NA-K-E TE-AMP-S-SXT-NA-K-E TE–C-S-SXT-NA-K-E TE-AMP-S-SXT-NA-K-E TE-C-AMP-CN-SXT-K-E TE-C-AMP-S-SXT-K-E TE-C-SXT-NA-K-E-CIP TE-C-AMP-SXT-NA-E-CIP TE-C-AMP-NA-E-CIP-CL | 20.2 | 0.5 |
| 6 | TE-C-AMP-S-SXT-E | 4.8 | 0.5 | TE-C-AMP-SXT-K-E TE-C-AMP-S-SXT-E TE-C-SXT-NA-E-CIP TE-C-AMP-SXT-NA-E TE-AMP-SXT-NA-K-E TE-C-AMP-NA-E-CIP TE-S-CN-SXT-K-E | 17.2 | 0.5 |
| 5 | S-SXT-NA-K-E TE-C-AMP-K-E | 14.2 | 0.4 | TE-C-AMP-SXT-E TE–C-S-SXT-E TE-C-AMP-K-E AMP-NA-E-CIP-CL TE-AMP-SXT-NA-E TE-AMP-SXT-K-E TE-AMP-S-SXT-E TE-AMP-NA-E-CIP C-AMP-SXT-K-E TE-AMP-S-NA-E | 12.5 | 0.4 |
| 4 | TE-C-AMP-E TE-C-SXT-E C-AMP-K-E C-AMP-SXT-E | 42.8 | 0.3 | TE-S-SXT-E TE-C-AM-E C-AMP-SXT-E TE-AMP-SXT-E TE-AMP-E-CL AMP-K-E-CL TE-C-SXT-E | 6.5 | 0.3 |
| 3 | SXT-C-E TE-C-E | 9.5 | 0.2 | TE-AMP-E S-NA-E TE-C-E | 3.5 | 0.2 |
| 2 | N/A | N/A | N/A | AMP-E | 0.5 | 0.1 |
| 1 | E | 19 | 0.08 | N/A | 0 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ibrahim, S.; Wei Hoong, L.; Lai Siong, Y.; Mustapha, Z.; C. W. Zalati, C.W.S.; Aklilu, E.; Mohamad, M.; Kamaruzzaman, N.F. Prevalence of Antimicrobial Resistance (AMR) Salmonella spp. and Escherichia coli Isolated from Broilers in the East Coast of Peninsular Malaysia. Antibiotics 2021, 10, 579. https://doi.org/10.3390/antibiotics10050579
Ibrahim S, Wei Hoong L, Lai Siong Y, Mustapha Z, C. W. Zalati CWS, Aklilu E, Mohamad M, Kamaruzzaman NF. Prevalence of Antimicrobial Resistance (AMR) Salmonella spp. and Escherichia coli Isolated from Broilers in the East Coast of Peninsular Malaysia. Antibiotics. 2021; 10(5):579. https://doi.org/10.3390/antibiotics10050579
Chicago/Turabian StyleIbrahim, Shamsaldeen, Loh Wei Hoong, Yip Lai Siong, Zaharuddin Mustapha, C. W. Salma C. W. Zalati, Erkihun Aklilu, Maizan Mohamad, and Nor Fadhilah Kamaruzzaman. 2021. "Prevalence of Antimicrobial Resistance (AMR) Salmonella spp. and Escherichia coli Isolated from Broilers in the East Coast of Peninsular Malaysia" Antibiotics 10, no. 5: 579. https://doi.org/10.3390/antibiotics10050579
APA StyleIbrahim, S., Wei Hoong, L., Lai Siong, Y., Mustapha, Z., C. W. Zalati, C. W. S., Aklilu, E., Mohamad, M., & Kamaruzzaman, N. F. (2021). Prevalence of Antimicrobial Resistance (AMR) Salmonella spp. and Escherichia coli Isolated from Broilers in the East Coast of Peninsular Malaysia. Antibiotics, 10(5), 579. https://doi.org/10.3390/antibiotics10050579






