An Antisense yycF RNA Modulates Biofilm Organization of Methicillin-Resistant Staphylococcus aureus and Pathogenicity in a Rat Model of Osteomyelitis
Abstract
:1. Introduction
2. Results
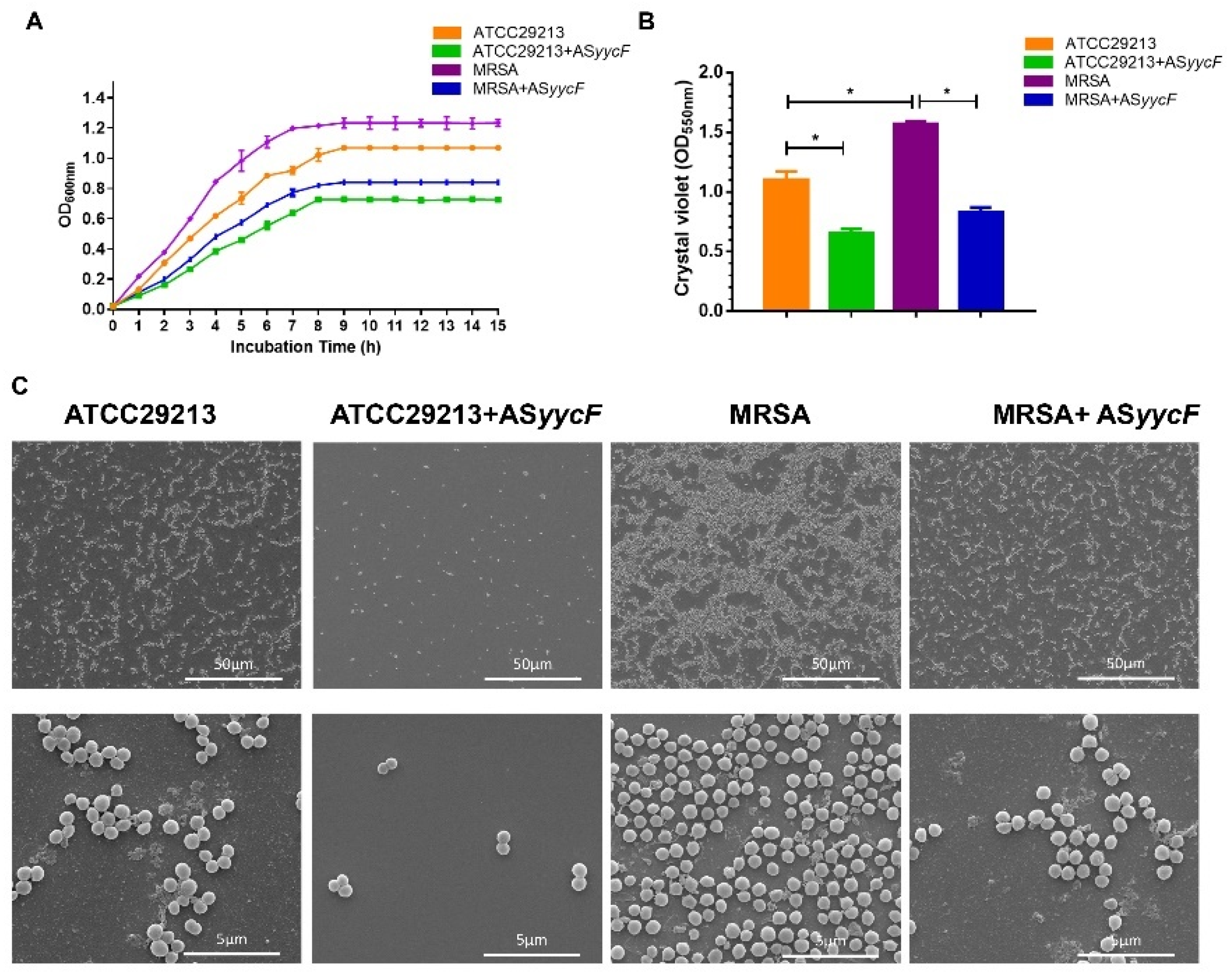
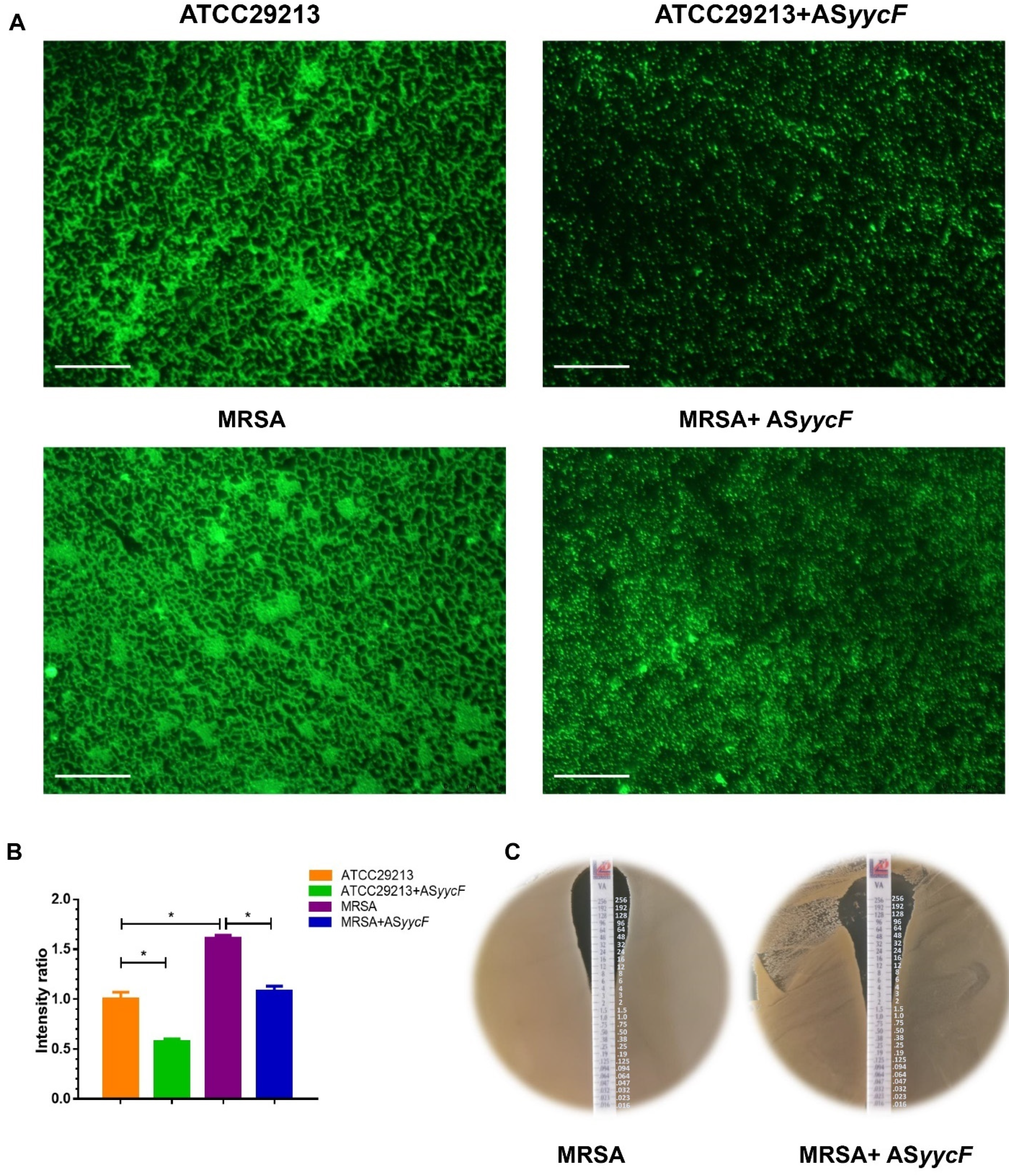
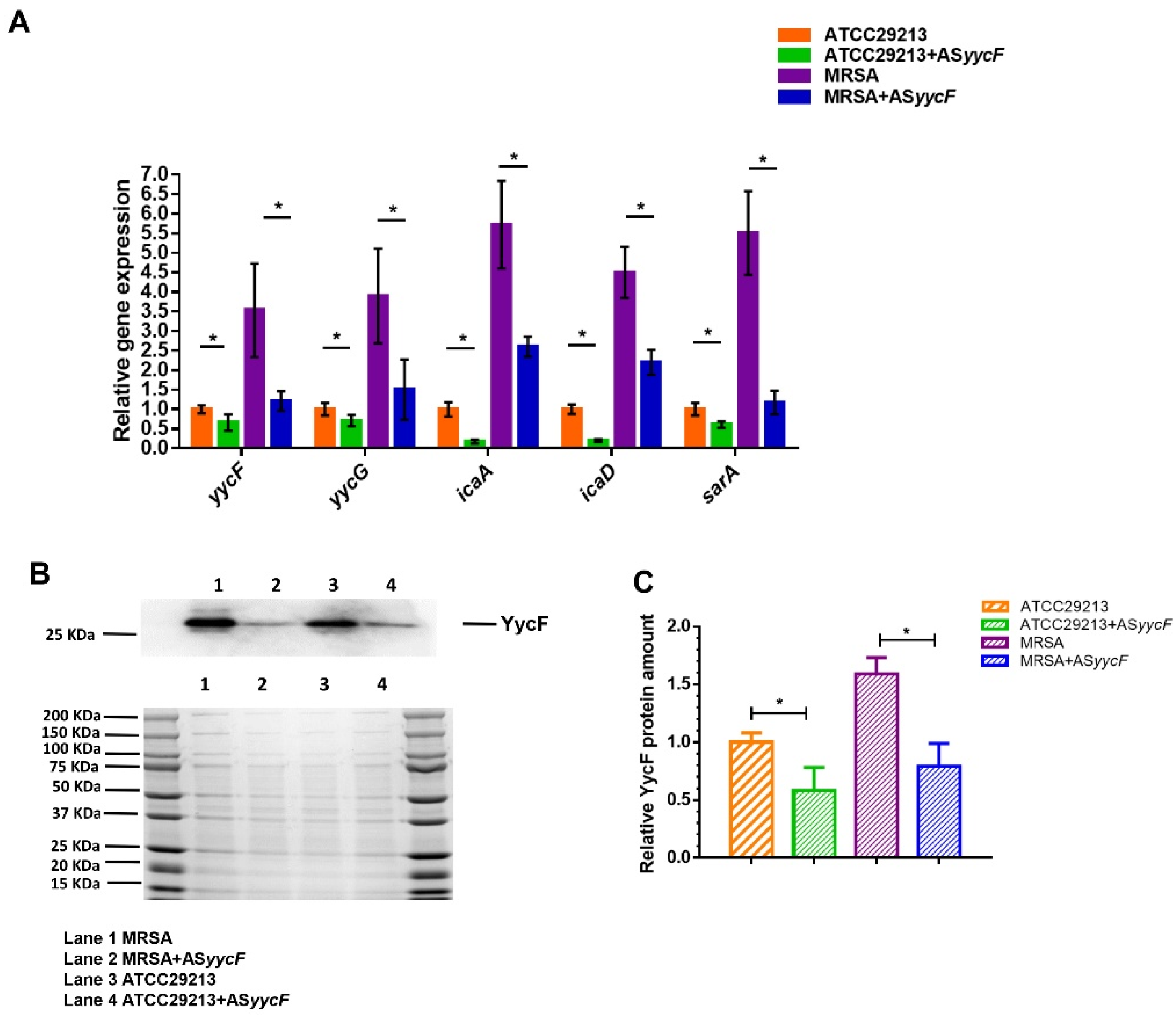
2.1. ASyycF Modulated Bacterial Growth and Biofilm Organization
2.2. Effect of Biofilm Formation on Antibiotic Sensitivity
2.3. ASyycF Inhibited MRSA Invasion in a Rat Tibial Infection Model
3. Discussion
4. Materials and Methods
4.1. Bacterial Growth Conditions
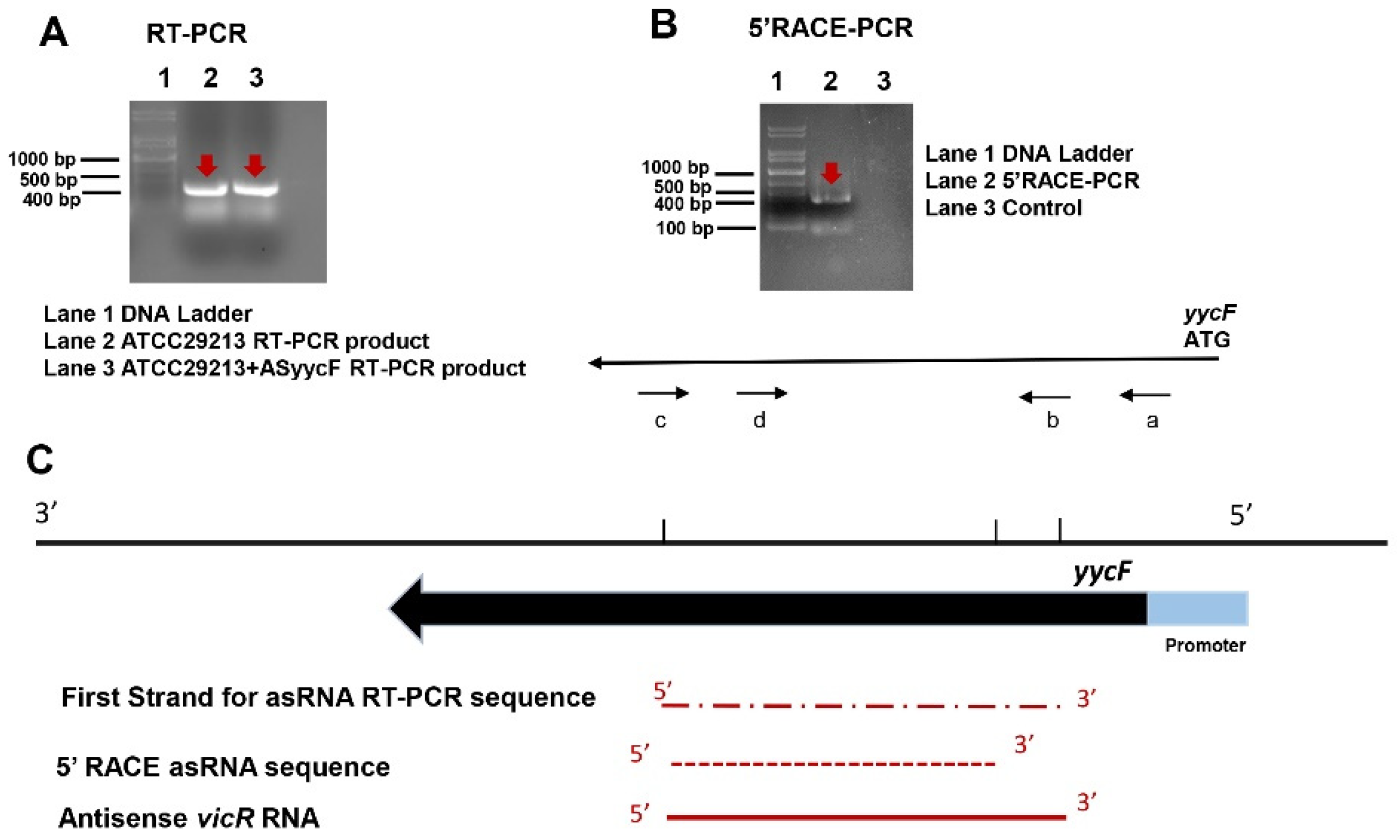
4.2. 5′-Rapid Amplification of cDNA Ends (5′-RACE) Assay for Antisense yycF
4.3. ASyycF Mutant Construction
4.4. Detection of Bacterial Growth and Biofilm Assessment
4.5. Identification of MIC Values
4.6. cDNA Reverse Transcription for RT-PCR Assays
4.7. Protein Extraction and Western Blotting
4.8. Osteomyelitis in an In Vivo Rat Model
4.9. Histological Evaluation and Fluorescent In Situ Hybridization Examination
4.10. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wu, S.; Liu, Y.; Zhang, H.; Lei, L. A new transformation method with nanographene oxides of antisense carrying yycG RNA improved antibacterial properties on methicillin-resistant Staphylococcus aureus biofilm. J. Vet. Med. Sci. 2019, 81, 1540–1546. [Google Scholar] [CrossRef] [Green Version]
- Algammal, A.M.; Hetta, H.F.; Elkelish, A.; Alkhalifah, D.H.H.; Hozzein, W.N.; Batiha, G.E.-S.; El Nahhas, N.; Mabrok, M.A. Methicillin-Resistant Staphylococcus aureus (MRSA): One Health Perspective Approach to the Bacterium Epidemiology, Virulence Factors, Antibiotic-Resistance, and Zoonotic Impact. Infect. Drug Resist. 2020, 13, 3255–3265. [Google Scholar] [CrossRef]
- Yu, K.; Song, L.; Kang, H.P.; Kwon, H.-K.; Back, J.; Lee, F.Y. Recalcitrant methicillin-resistant Staphylococcus aureus infection of bone cells: Intracellular penetration and control strategies. Bone Jt. Res. 2020, 9, 49–59. [Google Scholar] [CrossRef]
- Jayakumar, J.; Kumar, V.A.; Biswas, L.; Biswas, R. Therapeutic applications of lysostaphin against Staphylococcus aureus. J. Appl. Microbiol. 2020. [Google Scholar] [CrossRef]
- Gajdács, M. The Continuing Threat of Methicillin-Resistant Staphylococcus aureus. Antibiotics 2019, 8, 52. [Google Scholar] [CrossRef] [Green Version]
- Wu, S.; Huang, F.; Zhang, H.; Lei, L. Staphylococcus aureus biofilm organization modulated by YycFG two-component regulatory pathway. J. Orthop. Surg. Res. 2019, 14, 10. [Google Scholar] [CrossRef] [PubMed]
- Mosselhy, D.A.; Assad, M.; Sironen, T.; Elbahri, M. Nanotheranostics: A Possible Solution for Drug-Resistant Staphylococcus aureus and their Biofilms? Nanomaterials 2021, 11, 82. [Google Scholar] [CrossRef]
- Da Costa, D.; Exbrayat-Héritier, C.; Rambaud, B.; Megy, S.; Terreux, R.; Verrier, B.; Primard, C. Surface charge modulation of rifampicin-loaded PLA nanoparticles to improve antibiotic delivery in Staphylococcus aureus biofilms. J. Nanobiotechnol. 2021, 19, 12. [Google Scholar] [CrossRef]
- Nguyen, H.T.T.; Nguyen, T.H.; Otto, M. The staphylococcal exopolysaccharide PIA—Biosynthesis and role in biofilm for-mation, colonization, and infection. Comput. Struct. Biotechnol. J. 2020, 18, 3324–3334. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Liu, Y.; Lei, L.; Zhang, H. Antisense yycG Regulation of Antibiotic Sensitivity of Methicillin-Resistant Staphylococcus aureus in Chronic Osteomyelitis. Surg. Infect. (Larchmt) 2019, 20, 472–479. [Google Scholar] [CrossRef]
- Tierney, A.R.; Rather, P.N. Roles of two-component regulatory systems in antibiotic resistance. Future Microbiol. 2019, 14, 533–552. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Lin, K.; Liu, Y.; Zhang, H.; Lei, L. Two-component signaling pathways modulate drug resistance of Staphylococcus aureus (Review). Biomed. Rep. 2020, 13, 5. [Google Scholar]
- Rapun-Araiz, B.; Haag, A.F.; De Cesare, V.; Gil, C.; Dorado-Morales, P.; Penades, J.R.; Lasa, I. Systematic Reconstruction of the Complete Two-Component Sensorial Network in Staphylococcus aureus. mSystems 2020, 5, e00511–e00520. [Google Scholar] [CrossRef]
- Villanueva, M.; García, B.; Valle, J.; Rapún, B.; de Los Mozos, I.R.; Solano, C.; Martí, M.; Penadés, J.R.; Toledo-Arana, A.; Lasa, I. Sensory deprivation in Staphylococcus aureus. Nat. Commun. 2018, 9, 523. [Google Scholar] [CrossRef]
- Wu, S.; Liu, Y.; Lei, L.; Zhang, H. Endogenous antisense walR RNA modulates biofilm organization and pathogenicity of Enterococcus faecalis. Exp. Ther. Med 2020, 21, 69. [Google Scholar]
- Lei, L.; Stipp, R.N.; Chen, T.; Wu, S.Z.; Hu, T.; Duncan, M.J. Activity of Streptococcus mutans VicR Is Modulated by An-tisense RNA. J. Dent. Res. 2018, 97, 1477–1484. [Google Scholar] [CrossRef] [PubMed]
- Lakhundi, S.; Zhang, K. Methicillin-Resistant Staphylococcus aureus: Molecular Characterization, Evolution, and Epide-miology. Clin. Microbiol. Rev. 2018, 31, e00018–e00020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gould, I. Costs of hospital-acquired methicillin-resistant Staphylococcus aureus (MRSA) and its control. Int. J. Antimicrob. Agents 2006, 28, 379–384. [Google Scholar] [CrossRef]
- Suresh, M.K.; Biswas, R.; Biswas, L. An update on recent developments in the prevention and treatment of Staphylococcus aureus biofilms. Int. J. Med. Microbiol. 2019, 309, 1–12. [Google Scholar] [CrossRef]
- Wu, S.; Liu, Y.; Lei, L.; Zhang, H. Nanographene oxides carrying antisense walR RNA regulates the Enterococcus faecalis biofilm formation and its susceptibility to chlorhexidine. Lett. Appl. Microbiol. 2020, 71, 451–458. [Google Scholar] [CrossRef]
- Uruén, C.; Chopo-Escuin, G.; Tommassen, J.; Mainar-Jaime, R.C.; Arenas, J. Biofilms as Promoters of Bacterial Antibiotic Resistance and Tolerance. Antibiotics 2020, 10, 3. [Google Scholar] [CrossRef]
- Ceri, H.; Olson, M.E.; Stremick, C.; Read, R.R.; Morck, D.; Buret, A. The Calgary Biofilm Device: New Technology for Rapid Determination of Antibiotic Susceptibilities of Bacterial Biofilms. J. Clin. Microbiol. 1999, 37, 1771–1776. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodvold, K.A.; McConeghy, K.W. Methicillin-Resistant Staphylococcus aureus Therapy: Past, Present, and Future. Clin. Infect. Dis. 2013, 58, S20–S27. [Google Scholar] [CrossRef]
- Figueiredo, A.M.S.; Ferreira, F.A.; Beltrame, C.O.; Côrtes, M.F. The role of biofilms in persistent infections and factors in-volved in ica-independent biofilm development and gene regulation in Staphylococcus aureus. Crit. Rev. Microbiol. 2017, 43, 602–620. [Google Scholar] [CrossRef]
- Jamal, M.; Ahmad, W.; Andleeb, S.; Jalil, F.; Imran, M.; Nawaz, M.A.; Hussain, T.; Ali, M.; Rafiq, M.; Kamil, M.A. Bacterial biofilm and associated infections. J. Chin. Med. Assoc. 2018, 81, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Tande, A.J.; Osmon, D.R.; Greenwood-Quaintance, K.E.; Mabry, T.M.; Hanssen, A.D.; Patel, R. Clinical Characteristics and Outcomes of Prosthetic Joint Infection Caused by Small Colony Variant Staphylococci. mBio 2014, 5, e01910–e01914. [Google Scholar] [CrossRef] [Green Version]
- Wu, S.; Liu, Y.; Lei, L.; Zhang, H. Virulence of methicillin-resistant Staphylococcus aureus modulated by the YycFG two-component pathway in a rat model of osteomyelitis. J. Orthop. Surg. Res. 2019, 14, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Wu, S.; Liu, Y.; Zhang, H.; Lei, L. The Pathogenicity and Transcriptome Analysis of Methicillin-Resistant Staphylococcus aureus in Response to Water Extract of Galla chinensis. Evid.-Based Complement. Altern. Med. 2019, 2019, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Aktas, G. Efficacy of vancomycin in combination with various antimicrobial agents against clinical methicillin resistant Staphylococcus aureus strains. Pak. J. Med. Sci. 2020, 37, 151–156. [Google Scholar] [CrossRef]

| Primers | Sequence 5′-3′ (Forward/Reverse) | Reference |
|---|---|---|
| RT-qPCR | ||
| icaA | 5′-GATTATGTAATGTGCTTGGA-3′/ 5′-ACTACTGCTGCGTTAATAAT-3′ | [6] |
| yycF | 5′-TGGCGAAAGAAGACATCA-3′/ 5′-AACCCGTTACAAATCCTG-3′ | [6] |
| yycG | 5′-CGGGGCGTTCAAAAGACTTT-3′/ 5′-TCTGAACCTTTGAACACACGT-3′ | [6] |
| sarA | 5′-AGATGGCCCTTCTTCAAATG-3′/ 5′-CCGCAATAATTCTTGTGACG-3′ | This study |
| icaD | 5′-ATGGTCAAGCCCAGACAGAG-3′/ 5′-CGTGTTTTCAACATTTAATGCAA-3′ | [6] |
| 16S rRNA | 5′-GTAGGTGGCAAGCGTTATCC-3′/ 5′-CGCACATCAGCGTCAACA-3′ | [6] |
| AS yycF detection | ||
| First strand synthesis SAPCR | 5′-CGTATTATTAGATATCATGTTACCTGGTCG-3′ | This study |
| AS yycF detection SAAS | 5′-GTTCACGTGTCATTACTTGTCCCATATG-3′ | This study |
| 5′RACE | ||
| 5′RACE adapter | 5′-GCUGAUGGCGAUGAAUGAAC ACUGCGUUUGCUGGCUUUGAUGAAA-3′ | First Choice RLM–RACE (RNA ligase-mediated rapid amplification of cDNA ends), Thermo Scientific |
| 5′ RACE outer primer (c) | 5′-GCTGATGGCGATGAATGAACACTG-3′ | First Choice RLM–RACE, Thermo Scientific |
| 5′ RACE inner primer (d) | 5′-CGCGGATCCGAACACTGCGTTTGCTG GCTTTGATG-3′ | First Choice RLM–RACE, Thermo Scientific |
| Gene specific outer primer (a) | 5′-GGCGAAGATATTGAATTAACACATCGTG-3′ | This study |
| Gene specific inner primer (b) | 5′-CATATGGGACAAGTAATGACACGTGAAC-3′ | This study |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, S.; Liu, Y.; Lei, L.; Zhang, H. An Antisense yycF RNA Modulates Biofilm Organization of Methicillin-Resistant Staphylococcus aureus and Pathogenicity in a Rat Model of Osteomyelitis. Antibiotics 2021, 10, 603. https://doi.org/10.3390/antibiotics10050603
Wu S, Liu Y, Lei L, Zhang H. An Antisense yycF RNA Modulates Biofilm Organization of Methicillin-Resistant Staphylococcus aureus and Pathogenicity in a Rat Model of Osteomyelitis. Antibiotics. 2021; 10(5):603. https://doi.org/10.3390/antibiotics10050603
Chicago/Turabian StyleWu, Shizhou, Yunjie Liu, Lei Lei, and Hui Zhang. 2021. "An Antisense yycF RNA Modulates Biofilm Organization of Methicillin-Resistant Staphylococcus aureus and Pathogenicity in a Rat Model of Osteomyelitis" Antibiotics 10, no. 5: 603. https://doi.org/10.3390/antibiotics10050603





