Dispensing Antibiotics without Prescription at Community Pharmacies and Accredited Drug Dispensing Outlets in Tanzania: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Method
2.1. Study Design
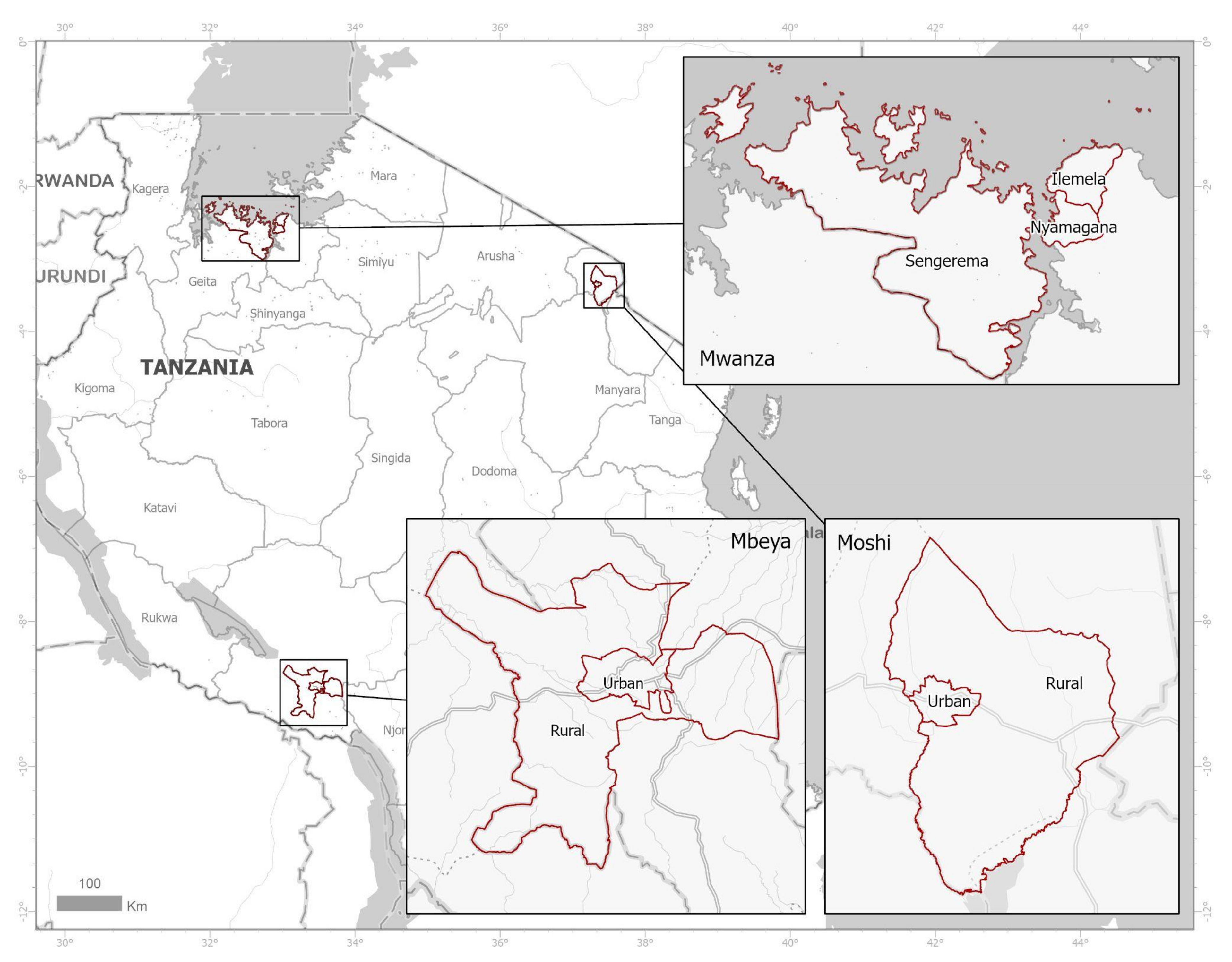
2.2. Study Areas and Sampling
2.3. Data Collection
2.4. Data Analysis
2.5. Ethical Considerations
3. Results
3.1. Community Pharmacies and ADDOs in Mwanza, Mbeya and Kilimanjaro
3.2. Stocking, Dispensing and Price of Amoxicillin in Mwanza, Mbeya and Kilimanjaro
3.3. Other Antibiotics Dispensed without Prescription
3.4. Differences between ADDOs and Pharmacies Regarding Dispenisng Practices
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Antimicrobial Resistance Global Report on Surveillance: 2014 Summary; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Klein, E.Y.; Van Boeckel, T.P.; Martinez, E.; Pant, S.; Gandra, S.; Levin, S.A.; Goossens, H.; Laxminarayan, R. Global increase and geographic convergence in antibiotic consumption between 2000 and 2015. Proc. Natl. Acad. Sci. USA 2018, 115, E3463–E3470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mbwasi, R.; Mapunjo, S.; Wittenauer, R.; Valimba, R.; Msovela, K.; Werth, B.J.; Khea, A.M.; Nkiligi, E.A.; Lusaya, E.; Stergachis, A.; et al. National Consumption of Antimicrobials in Tanzania: 2017–2019. Front. Pharmacol. 2020, 11, 585553. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Antimicrobial Consumption: Annual Epidemiological Report for 2017; ECDC: Stockholm, Sweden, 2018. [Google Scholar]
- Seni, J.; Mapunjo, S.G.; Wittenauer, R.; Valimba, R.; Stergachis, A.; Werth, B.J.; Saitoti, S.; Mhadu, N.H.; Lusaya, E.; Konduri, N. Antimicrobial use across six referral hospitals in Tanzania: A point prevalence survey. BMJ Open 2020, 10, e042819. [Google Scholar] [CrossRef]
- WHO. Global Antimicrobial Resistance Surveillance System (GLASS) Report: Early Implementation 2016–2017; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- Miller, R.; Goodman, C. Performance of retail pharmacies in low- and middle-income Asian settings: A systematic review. Health Policy Plan. 2016, 31, 940–953. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sudhinaraset, M.; Ingram, M.; Lofthouse, H.K.; Montagu, D. What is the role of informal healthcare providers in developing countries? A systematic review. PLoS ONE 2013, 8, e54978. [Google Scholar]
- Olenja, J. Editorial Health seeking behaviour in context. East Afr. Med. J. 2003, 80, 61–62. [Google Scholar] [CrossRef] [Green Version]
- Ocan, M.; Obuku, E.A.; Bwanga, F.; Akena, D.; Richard, S.; Ogwal-Okeng, J.; Obua, C. Household antimicrobial self-medication: A systematic review and meta-analysis of the burden, risk factors and outcomes in developing countries. BMC Public Health 2015, 15, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Salim, A.M.; Elgizoli, B. Exploring the reasons why pharmacists dispense antibiotics without prescriptions in Khartoum state, Sudan. Int. J. Pharm. Pract. 2017, 25, 59–65. [Google Scholar] [CrossRef]
- Goodman, C.; Kachur, S.P.; Abdulla, S.; Bloland, P.; Mills, A. Drug shop regulation and malaria treatment in Tanzania—Why do shops break the rules, and does it matter? Health Policy Plan. 2007, 22, 393–403. [Google Scholar] [CrossRef] [Green Version]
- Eliakimu, E. Antimicrobial stewardship in Tanzania. Int. J. Health Gov. 2016, 21, 150–164. [Google Scholar] [CrossRef]
- Rutta, E.; Senauer, K.; Johnson, K.; Adeya, G.; Mbwasi, R.; Liana, J.; Kimatta, S.; Sigonda, M.; Alphonce, E. Creating a New Class of Pharmaceutical Services Provider for Underserved Areas: The Tanzania Accredited Drug Dispensing Outlet Experience. Prog. Community Health Partnersh. Res. Educ. Action 2009, 3, 145–153. [Google Scholar] [CrossRef] [PubMed]
- MOH. Standard Treatment Guidelines & National Essential Medications List: Mainland, Tanzania. 2021. Available online: http://www.tzdpg.or.tz/fileadmin/documents/dpg_internal/dpg_working_groups_clusters/cluster_2/health/Key_Sector_Documents/Tanzania_Key_Health_Documents/STANDARD_TREATMENT_GUIDELINES__CORRECT_FINAL_USE_THIS-1.pdf (accessed on 22 August 2021).
- Rutta, E.; Liana, J.; Embrey, M.; Johnson, K.J.; Kimatta, S.; Valimba, R.; Lieber, R.; Shekalaghe, E.; Sillo, H. Accrediting retail drug shops to strengthen Tanzania’s public health system: An ADDO case study. J. Pharm. Policy Pract. 2015, 8, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Embrey, M.; Mbwasi, R.; Shekalaghe, E.; Liana, J.; Kimatta, S.; Ignace, G.; Dillip, A.; Hafner, T. National Health Insurance Fund’s relationship to retail drug outlets: A Tanzania case study. J. Pharm. Policy Pract. 2021, 14, 1–12. [Google Scholar] [CrossRef]
- Chalker, J.C.; Vialle-Valentin, C.; Liana, J.; Mbwasi, R.; Semali, I.A.; Kihiyo, B.; Shekalaghe, E.; Dillip, A.; Kimatta, S.; Valimba, R.; et al. What roles do accredited drug dispensing outlets in Tanzania play in facilitating access to antimicrobials? Results of a multi-method analysis. Antimicrob. Resist. Infect. Control. 2015, 4, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simba, D.; Kakoko, D.; Semali, I.; Kessy, A.; Embrey, M. Household Knowledge of Antimicrobials and Antimicrobial Resistance in the Wake of an Accredited Drug Dispensing Outlet (ADDO) Program Rollout in Tanzania. PLoS ONE 2016, 11, e0163246. [Google Scholar] [CrossRef] [Green Version]
- Poyongo, B.P.; Sangeda, R.Z. Pharmacists’ Knowledge, Attitude and Practice Regarding the Dispensing of Antibiotics without Prescription in Tanzania: An Explorative Cross-Sectional Study. Pharmacy 2020, 8, 238. [Google Scholar] [CrossRef]
- Hall, J.W.; Bouchard, J.; Bookstaver, P.B.; Haldeman, M.S.; Kishimbo, P.; Mbwanji, G.; Mwakyula, I.; Mwasomola, D.; Seddon, M.; Shaffer, M.; et al. The Mbeya Antimicrobial Stewardship Team: Implementing Antimicrobial Stewardship at a Zonal-Level Hospital in Southern Tanzania. Pharmacy 2020, 8, 107. [Google Scholar] [CrossRef] [PubMed]
- Mboya, E.A.; Sanga, L.A.; Ngocho, J.S. Irrational use of antibiotics in the Moshi Municipality Northern Tanzania: A cross sectional study. Pan Afr. Med. J. 2018, 31, 165. [Google Scholar] [CrossRef] [PubMed]
- Viberg, N.; Kalala, W.; Mujinja, P.; Tomson, G.; Lundborg, C.S. “Practical knowledge” and perceptions of antibiotics and antibiotic resistance among drugsellers in Tanzanian private drugstores. BMC Infect. Dis. 2010, 10, 270–279. [Google Scholar] [CrossRef] [Green Version]
- Horumpende, P.G.; Sonda, T.B.; Van Zwetselaar, M.; Antony, M.L.; Tenu, F.F.; Mwanziva, C.E.; Shao, E.R.; Mshana, S.E.; Mmbaga, B.T.; Chilongola, J. Prescription and non-prescription antibiotic dispensing practices in part I and part II pharmacies in Moshi Municipality, Kilimanjaro Region in Tanzania: A simulated clients approach. PLoS ONE 2018, 13, e0207465. [Google Scholar] [CrossRef] [Green Version]
- Samwel, T. Knowledge of Malaria Symptoms, Antimalarial Drugs Stocked and Dispensing Practises in Acredited Drug Dispensing Outlets; Muhimbili University of Health and Allied Sciences: Morogoro, Tanzania, 2013. [Google Scholar]
- Wafula, F.N.; Miriti, E.M.; Goodman, C.A. Examining characteristics, knowledge and regulatory practices of specialized drug shops in Sub-Saharan Africa: A systematic review of the literature. BMC Health Serv. Res. 2012, 12, 223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nga, D.T.T.; Chuc, N.T.K.; Hoa, N.P.; Nguyen, N.T.T.; Loan, H.T.; Toan, T.K.; Phuc, H.D.; Horby, P.; Van Yen, N.; Van Kinh, N.; et al. Antibiotic sales in rural and urban pharmacies in northern Vietnam: An observational study. BMC Pharmacol. Toxicol. 2014, 15, 6. [Google Scholar] [CrossRef] [Green Version]
- Asiimwe, B.B.; Kiiru, J.; Mshana, S.E.; Neema, S.; Keenan, K.; Kesby, M.; Mwanga, J.R.; Sloan, D.J.; Mmbaga, B.T.; Smith, V.A.; et al. Protocol for an interdisciplinary cross-sectional study investigating the social, biological and community-level drivers of antimicrobial resistance (AMR): Holistic Approach to Unravel Antibacterial Resistance in East Africa (HATUA). BMJ Open 2021, 11, e041418. [Google Scholar] [CrossRef]
- Watson, M.C.; Norris, P.; Granas, A.G. A systematic review of the use of simulated patients and pharmacy practice research. Int. J. Pharm. Pract. 2006, 14, 83–93. [Google Scholar] [CrossRef]
- Aanensen, D.M.; Huntley, D.M.; Menegazzo, M.; Powell, C.I.; Spratt, B.G. EpiCollect+: Linking smartphones to web applications for complex data collection projects. F1000Research 2014, 3, 199. [Google Scholar] [CrossRef] [PubMed]
- Auta, A.; Hadi, M.A.; Oga, E.; Adewuyi, E.O.; Abdu-Aguye, S.; Adeloye, D.; Strickland-Hodge, B.; Morgan, D.J. Global access to antibiotics without prescription in community pharmacies: A systematic review and meta-analysis. J. Infect. 2019, 78, 8–18. [Google Scholar] [CrossRef]
- Yadesa, T.M.; Zeberga, G. Assessment of good dispensing practice among drug stores in Mizan Aman Town, South West Ethiopia. Pharm. Lett. 2018, 10, 9–20. [Google Scholar]
- Saleem, Z.; Hassali, M.A.; Godman, B.; Fatima, M.; Ahmad, Z.; Sajid, A.; Rehman, I.U.; Nadeem, M.U.; Javaid, Z.; Malik, M.; et al. Sale of WHO AWaRe groups antibiotics without a prescription in Pakistan: A simulated client study. J. Pharm. Policy Pract. 2020, 13, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Chang, J.; Liu, X.; Zhai, P.; Hu, S.; Li, P.; Hayat, K.; Kabba, J.A.; Feng, Z.; Yang, C.; et al. Dispensing Antibiotics without a Prescription for Acute Cough Associated with Common Cold at Community Pharmacies in Shenyang, Northeastern China: A Cross-Sectional Study. Antibiotics 2020, 9, 163. [Google Scholar] [CrossRef] [Green Version]
- Chang, J.; Xu, S.; Zhu, S.; Li, Z.; Yu, J.; Zhang, Y.; Zu, J.; Fang, Y.; Ross-Degnan, D. Assessment of non-prescription antibiotic dispensing at community pharmacies in China with simulated clients: A mixed cross-sectional and longitudinal study. Lancet Infect. Dis. 2019, 19, 1345–1354. [Google Scholar] [CrossRef]



| Study Region/District | Population (Average House Size) | Number of Drug Shops | Outlet Density per Population (Region) | Outlet Density per Population (District) | ||
|---|---|---|---|---|---|---|
| ADDO | PHARMACY | Total | ||||
| Mwanza | 2205.3 | |||||
| Urban | 706453 (4.8) | 324 | 110 | 434 | 1600.3 | |
| Rural | 663,034 (6.0) | 184 | 3 | 187 | 3489.7 | |
| Mbeya | 2271.7 | |||||
| Urban | 385,279 (4.2) | 142 | 31 | 173 | 1888.6 | |
| Rural | 305,319 (4.1) | 120 | 11 | 131 | 2150.1 | |
| Kilimanjaro | 2593.7 | |||||
| Urban | 184,292 (4.0) | 97 | 23 | 120 | 1288.8 | |
| Rural | 466,737 (4.2) | 110 | 2 | 112 | 4094.2 | |
| Seller Response when Directly Asked to Sell a Half Course of Amoxicillin | Mwanza (n = 612) | Mbeya (n = 304) | Kilimanjaro (n = 232) | TOTAL (n = 1148) | Chi-Square and p Value |
|---|---|---|---|---|---|
| Did not sell amoxicillin a | 47 (7.7) | 3 (1.0) | 7 (3.0) | 57 (4.9) | Pearson chi2(2) = 21.267, Pr = 0.000 |
| Sold half course without questions | 509 (83.2) | 276 (90.8) | 216 (93.1) | 1001 (87.2) | Pearson chi2(2) = 19.652 Pr =0.000 |
| Sold half course but advised full course | 45 (7.4) | 22 (7.2) | 6 (2.6) | 73 (6.4) | Pearson chi2, 6.9546 Pr = 0.031 |
| Would only sell a full course | 11 (1.8) | 3 (1.0) | 3 (1.3) | 17 (1.5) | Fisher’s exact = 0.554 |
| Quality of interaction by item | |||||
| Asked about prescription | 9 (1.5) | 2 (0.7) | 3 (1.3) | 14 (1.2) | Fisher’s exact = 0.631 |
| Asked to describe symptoms | 54 (8.8) | 16 (5.3) | 13 (5.6) | 83 (7.22) | Pearson chi2(2) = 5.851 Pr = 0.054 |
| Asked about taking other medications | 10 (1.6) | 4 (1.3) | 3 (1.3) | 17 (1.5) | Fisher’s exact = 1.000 |
| Suggested no need of antibiotics | 5 (0.8) | 1 (0.3) | 3 (1.3) | 9 (0.8) | Fisher’s exact = 0.492 |
| Suggested to see a doctor | 11 (1.8) | 0 | 9 (3.9) | 20 (1.7) | Fisher’s exact = 0.001 |
| Provided instruction to buy a full course | 49 (8.0) | 19 (6.3) | 6 (2.6) | 74 (6.4) | Pearson chi2(2) = 9.0799 Pr = 0.011 |
| Provided instruction to finish a full course | 47 (7.7) | 20 (6.9) | 6 (2.6) | 73 (6.4) | Pearson chi2(2) = 7.721 Pr = 0.021 |
| Quality of interaction additive score | |||||
| 0 - no question asked or advice given | 522 (85.3) | 275 (90.5) | 216 (93.1) | 1013 (88.2) | Pearson chi2 = 11.851Pr = 0.003 |
| 1 question or piece of advice | 35 (5.7) | 6 (1.9) | 4 (1.7) | 45 (3.9) | |
| 2 questions or pieces of advice | 28 (4.6) | 14 (4.6) | 9 (3.9) | 51 (4.4) | |
| 3 questions or pieces of advice | 18 (2.9) | 8 (2.6) | 0 | 26 (2.3) | |
| 4 questions or pieces of advice | 6 (0.9) | 1 (0.3) | 0 | 7 (0.6) | |
| 5 questions or pieces of advice | 2 (0.3) | 0 | 0 | 2 (0.2) | |
| 6 questions or pieces of advice | 1 (0.2) | 0 | 0 | 1 (0.1) | |
| 7 questions or pieces of advice | 0 | 0 | 3 (1.3) | 3 (0.3) | |
| Total with a score between 1–7 | 90 (14.7) | 29 (9.5) | 16 (6.9) | 135 (11.7) |
| Mwanza (n = 26) | Mbeya (n = 13) | Kilimanjaro (n = 1) |
|---|---|---|
| Ampicloxacillin (9) | Ampicloxacillin (1) | Trimethoprim/sulfamethoxazole (1) |
| Ampicillin (3) | Ampicloxacillin and Phenoxymethylpenicillin (1) | |
| Metronidazole (2) | Azithromycin and Metronidazole (1) | |
| Azithromycin (2) | Cephalexin (1) | |
| Ciprofloxacin (5) | Ciprofloxacin (4) | |
| Doxycycline (1) | Doxycycline and Metronidazole (1) | |
| Trimethoprim/sulfamethoxazole (3) | Nitrofurantoin and Azithromycin (1) | |
| Doxycycline and Azithromycin (1) | PenV (1) | |
| Trimethoprim/sulfamethoxazole (1) | ||
| Trimethoprim/sulfamethoxazole (1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ndaki, P.M.; Mushi, M.F.; Mwanga, J.R.; Konje, E.T.; Ntinginya, N.E.; Mmbaga, B.T.; Keenan, K.; Sabiiti, W.; Kesby, M.; Benitez-Paez, F.; et al. Dispensing Antibiotics without Prescription at Community Pharmacies and Accredited Drug Dispensing Outlets in Tanzania: A Cross-Sectional Study. Antibiotics 2021, 10, 1025. https://doi.org/10.3390/antibiotics10081025
Ndaki PM, Mushi MF, Mwanga JR, Konje ET, Ntinginya NE, Mmbaga BT, Keenan K, Sabiiti W, Kesby M, Benitez-Paez F, et al. Dispensing Antibiotics without Prescription at Community Pharmacies and Accredited Drug Dispensing Outlets in Tanzania: A Cross-Sectional Study. Antibiotics. 2021; 10(8):1025. https://doi.org/10.3390/antibiotics10081025
Chicago/Turabian StyleNdaki, Pendo M., Martha F. Mushi, Joseph R. Mwanga, Eveline T. Konje, Nyanda E. Ntinginya, Blandina T. Mmbaga, Katherine Keenan, Wilber Sabiiti, Mike Kesby, Fernando Benitez-Paez, and et al. 2021. "Dispensing Antibiotics without Prescription at Community Pharmacies and Accredited Drug Dispensing Outlets in Tanzania: A Cross-Sectional Study" Antibiotics 10, no. 8: 1025. https://doi.org/10.3390/antibiotics10081025
APA StyleNdaki, P. M., Mushi, M. F., Mwanga, J. R., Konje, E. T., Ntinginya, N. E., Mmbaga, B. T., Keenan, K., Sabiiti, W., Kesby, M., Benitez-Paez, F., Sandeman, A., Holden, M. T. G., Mshana, S. E., & HATUA Consortium. (2021). Dispensing Antibiotics without Prescription at Community Pharmacies and Accredited Drug Dispensing Outlets in Tanzania: A Cross-Sectional Study. Antibiotics, 10(8), 1025. https://doi.org/10.3390/antibiotics10081025






