High Carriage Rate of the Multiple Resistant Plasmids Harboring Quinolone Resistance Genes in Enterobacter spp. Isolated from Healthy Individuals
Abstract
:1. Introduction
2. Results
2.1. Bacterial Isolates
2.2. Antimicrobial Susceptibility Analysis
2.3. Prevalence of PMQR Genes
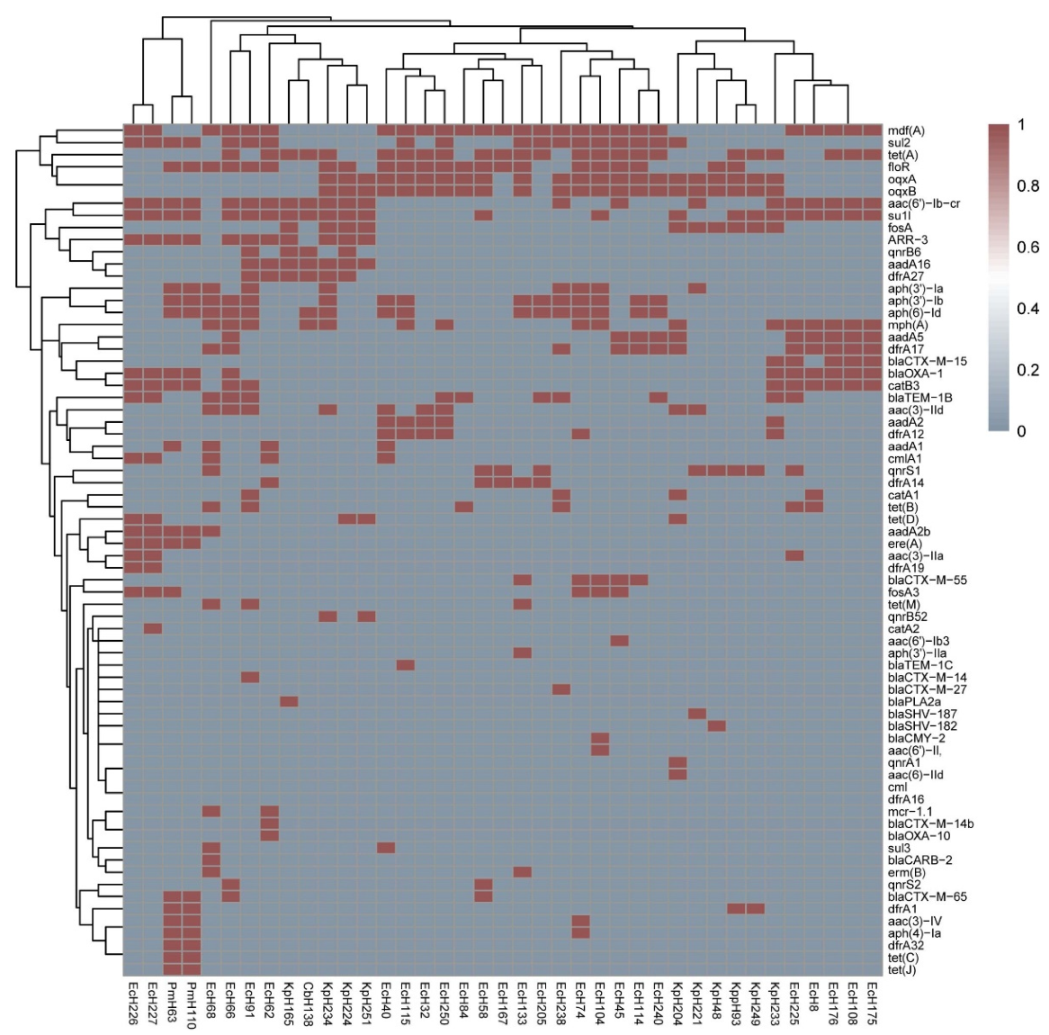
2.4. Other Acquired Resistance Genes Exist and Coexist in the Isolates
2.5. Drug Resistance Caused by Gene Mutations
2.6. Consistency Rates between the Drug Resistance Genes and Drug Resistance Phenotypes
3. Discussion
4. Materials and Methods
4.1. Samples and Bacterial Strains
4.2. PMQR Gene Amplification
4.3. Antimicrobial Susceptibility Testing
4.4. Genome and Plasmid Sequencing
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liu, X.M. International perspectives on food safety and regulations—A need for harmonized regulations: Perspectives in China. J. Sci. Food Agric. 2014, 94, 1928–1931. [Google Scholar] [CrossRef] [PubMed]
- Tang, Q.; Song, P.; Li, J.; Kong, F.; Sun, L.; Xu, L. Control of antibiotic resistance in China must not be delayed: The current state of resistance and policy suggestions for the government, medical facilities, and patients. Biosci. Trends 2016, 10, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Q.Q.; Ying, G.G.; Pan, C.G.; Liu, Y.S.; Zhao, J.L. Comprehensive evaluation of antibiotics emission and fate in the river basins of China: Source analysis, multimedia modeling, and linkage to bacterial resistance. Environ. Sci. Technol. 2015, 49, 6772–6782. [Google Scholar] [CrossRef]
- Anna, F.; Sergi, M.; Ernest, G.; Jordi, V. Mechanism of action of and resistance to quinolones. Microb. Biotechnol. 2009, 2, 40–61. [Google Scholar]
- Rodríguez-Martínez, J.M.; Machuca, J.; Cano, M.E.; Calvo, J.; Martinez-Martinez, L.; Pascual, A. Plasmid-mediated quinolone resistance: Two decades on. Drug Resist. Updates 2016, 29, 13–29. [Google Scholar] [CrossRef] [PubMed]
- Jacoby, G.A.; Strahilevitz, J.; Hooper, D.C. Plasmid-Mediated Quinolone Resistance. Microbiol. Spectr. 2014, 2, 475–503. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martà nez-Martà nez, L.; Pascual, A.; Jacoby, G.A. Quinolone resistance from a transferable plasmid. Lancet 1998, 351, 797–799. [Google Scholar] [CrossRef]
- Ruiz, J.; Pons, M.J.; Gomes, C. Transferable mechanisms of quinolone resistance. Int. J. Antimicrob. Agents 2012, 40, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhang, W.; Pan, W.; Yin, J.; Pan, Z.; Gao, S.; Jiao, X. Prevalence of qnr, aac(6′)-Ib-cr, qepA, and oqxAB in Escherichia coli isolates from humans, animals, and the environment. Antimicrob. Agents Chemother. 2012, 56, 3423–3427. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, X.; Li, J.; Zhang, Y.; Yan, H.; Wang, Y.; Shi, L.; Zhou, L. Detection of plasmid-mediated quinolone resistance determinants and qnrS expression in Enterobacteriaceae clinical isolates. J. Infect. Dev. Ctries. 2014, 8, 1625–1629. [Google Scholar] [CrossRef] [Green Version]
- Zhao, L.; Zhang, J.; Zheng, B.; Wei, Z.; Shen, P.; Li, S.; Li, L.; Xiao, Y. Molecular epidemiology and genetic diversity of fluoroquinolone-resistant Escherichia coli isolates from patients with community-onset infections in 30 Chinese county hospitals. J. Clin. Microbiol. 2015, 53, 766–770. [Google Scholar] [CrossRef] [Green Version]
- Li, P.; Liu, D.; Zhang, X.; Tuo, H.; Lei, C.; Xie, X.; Gu, J.; Zhang, A. Characterization of Plasmid-Mediated Quinolone Resistance in Gram-Negative Bacterial Strains from Animals and Humans in China. Microb. Drug Resist. 2019, 25, 1050–1056. [Google Scholar] [CrossRef]
- Jones-Dias, D.; Manageiro, V.; Francisco, A.P.; Martins, A.P.; Domingues, G.; Louro, D.; Ferreira, E.; Canica, M. Assessing the molecular basis of transferable quinolone resistance in Escherichia coli and Salmonella spp. from food-producing animals and food products. Vet. Microbiol. 2013, 167, 523–531. [Google Scholar] [CrossRef]
- Albrechtova, K.; Papousek, I.; De Nys, H.; Pauly, M.; Anoh, E.; Mossoun, A.; Dolejska, M.; Masarikova, M.; Metzger, S.; Couacy-Hymann, E.; et al. Low Rates of Antimicrobial-Resistant Enterobacteriaceae in Wildlife in Tai National Park, Cote d’Ivoire, Surrounded by Villages with High Prevalence of Multiresistant ESBL-Producing Escherichia coli in People and Domestic Animals. PLoS ONE 2014, 9, e113548. [Google Scholar] [CrossRef]
- Gibson, J.S.; Cobbold, R.N.; Heisig, P.; Sidjabat, H.E.; Kyaw-Tanner, M.T.; Trott, D.J. Identification of Qnr and AAC(6′)-1b-cr plasmid-mediated fluoroquinolone resistance determinants in multidrug-resistant Enterobacter spp. isolated from extraintestinal infections in companion animals. Vet. Microbiol. 2010, 143, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Shen, C.; Zheng, X.B.; Liu, Y.; Ahmed, M.A.E.; Zhao, Z.H.; Liao, K.; Shi, Y.L.; Guo, X.; Zhong, R.X.; et al. Plasmid-mediated colistin resistance gene mcr-1 in Escherichia coli and Klebsiella pneumoniae isolated from market retail fruits in Guangzhou, China. Infect. Drug Resist. 2019, 12, 385–389. [Google Scholar] [CrossRef] [Green Version]
- Nayme, K.; Barguigua, A.; Bouchrif, B.; Diawara, I.; El Otmani, F.; Elmdaghri, N.; Zerouali, K.; Timinouni, M. Occurrence of extended-spectrum beta-lactamase, AmpC and virulence genes in Escherichia coli isolates from vegetable salads in Morocco. Br. Food J. 2017, 119, 1633–1647. [Google Scholar] [CrossRef]
- Li, J.; Wang, T.; Shao, B.; Shen, J.Z.; Wang, S.C.; Wu, Y.N. Plasmid-Mediated Quinolone Resistance Genes and Antibiotic Residues in Wastewater and Soil Adjacent to Swine Feedlots: Potential Transfer to Agricultural Lands. Environ. Health Perspect. 2012, 120, 1144–1149. [Google Scholar] [CrossRef] [PubMed]
- Vaz-Moreira, I.; Varela, A.R.; Pereira, T.V.; Fochat, R.C.; Manaia, C.M. Multidrug Resistance in Quinolone-Resistant Gram-Negative Bacteria Isolated from Hospital Effluent and the Municipal Wastewater Treatment Plant. Microb. Drug Resist. 2016, 22, 155–163. [Google Scholar] [CrossRef]
- Daniela, F.; Kayode, F.; Aurora, G.-F.; Laura, V.; Alessandra, C. Plasmid-mediated quinolone resistance and β-lactamases in Escherichia coli from healthy animals from Nigeria. J. Antimicrob. Chemother. 2011, 66, 1269–1272. [Google Scholar]
- Veldman, K.; Kant, A.; Dierikx, C.; van Essen-Zandbergen, A.; Wit, B.; Mevius, D. Enterobacteriaceae resistant to third-generation cephalosporins and quinolones in fresh culinary herbs imported from Southeast Asia. Int. J. Food Microbiol. 2014, 177, 72–77. [Google Scholar] [CrossRef]
- Kim, J.; Park, K.Y.; Park, H.K.; Hwang, H.S.; Seo, M.R.; Kim, B.; Cho, Y.; Rho, M.; Pai, H. High fecal carriage of bla(CTX-M), bla(CMY-2), and plasmid-mediated quinolone resistance genes among healthy Korean people in a metagenomic analysis. Sci. Rep. 2021, 11, 5874. [Google Scholar] [CrossRef]
- Yang, T.; Zeng, Z.; Rao, L.; Chen, X.; He, D.; Lv, L.; Wang, J.; Zeng, L.; Feng, M.; Liu, J.H. The association between occurrence of plasmid-mediated quinolone resistance and ciprofloxacin resistance in Escherichia coli isolates of different origins. Vet. Microbiol. 2014, 170, 89–96. [Google Scholar] [CrossRef]
- Liu, Y.; Li, X.Y.; Wan, L.G.; Jiang, W.Y.; Yang, J.H.; Li, F.Q. Virulence and transferability of resistance determinants in a novel Klebsiella pneumoniae sequence type 1137 in China. Microb. Drug Resist. 2014, 20, 150–155. [Google Scholar] [CrossRef]
- Mirzaii, M.; Jamshidi, S.; Zamanzadeh, M.; Marashifard, M.; Hosseini, S.A.A.M.; Haeili, M.; Jahanbin, F.; Mansouri, F.; Darban-Sarokhalil, D.; Khoramrooz, S.S. Determination of gyrA and parC mutations and prevalence of plasmid-mediated quinolone resistance genes in Escherichia coli and Klebsiella pneumoniae isolated from patients with urinary tract infection in Iran. J. Glob. Antimicrob. Resist. 2018, 13, 197–200. [Google Scholar] [CrossRef]
- Pasom, W.; Chanawong, A.; Lulitanond, A.; Wilailuckana, C.; Kenprom, S.; Puang-Ngern, P. Plasmid-Mediated Quinolone Resistance Genes, aac (6)-Ib-cr, qnrS, qnrB, and qnrA, in Urinary Isolates of Escherichia coli and Klebsiella pneumoniae at a Teaching Hospital, Thailand. Jpn. J. Infect. Dis. 2013, 66, 428–432. [Google Scholar] [CrossRef] [Green Version]
- Karah, N.; Poirel, L.; Bengtsson, S.; Sundqvist, M.; Kahlmeter, G.; Nordmann, P.; Sundsfjord, A. Plasmid-mediated quinolone resistance determinants qnr and aac(6′)-Ib-cr in Escherichia coli and Klebsiella spp. from Norway and Sweden. Diagn. Microbiol. Infect. Dis. 2010, 66, 425–431. [Google Scholar] [CrossRef]
- Ni, Q.; Tian, Y.; Zhang, L.; Jiang, C.; Dong, D.; Li, Z.; Mao, E.; Peng, Y. Prevalence and quinolone resistance of fecal carriage of extended-spectrum β-lactamase-producing Escherichia coli in 6 communities and 2 physical examination center populations in Shanghai, China. Diagn. Microbiol. Infect. Dis. 2016, 86, 428–433. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.; Wu, H.; Zhai, Y.; He, Z.; Sun, H.; Cai, T.; He, D.; Liu, J.; Wang, S.; Pan, Y.; et al. Prevalence and molecular characterization of oqxAB in clinical Escherichia coli isolates from companion animals and humans in Henan Province, China. Antimicrob. Resist. Infect. Control 2018, 7, 18. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhi, C.P.; Chen, X.J.; Guo, Z.W.; Liu, W.L.; Luo, J.; Huang, X.Y.; Zeng, L.; Huang, J.W.; Xia, Y.B.; et al. Characterization of oqxAB in Escherichia coli Isolates from Animals, Retail Meat, and Human Patients in Guangzhou, China. Front. Microbiol. 2017, 8, 1982. [Google Scholar] [CrossRef] [Green Version]
- Cheng, L.; Cao, X.-L.; Zhang, Z.-F.; Ning, M.-z.; Xu, X.-J.; Zhou, W.; Chen, J.-H.; Zhang, J.-H.; Shen, H.; Zhang, K. Clonal dissemination of KPC-2 producing Klebsiella pneumoniae ST11 clone with high prevalence of oqxAB and rmtB in a tertiary hospital in China: Results from a 3-year period. Ann. Clin. Microbiol. Antimicrob. 2016, 15, 1. [Google Scholar] [CrossRef] [Green Version]
- Azargun, R.; Barhaghi, M.H.S.; Kafil, H.S.; Oskouee, M.A.; Sadeghi, V.; Memar, M.Y.; Ghotaslou, R. Frequency of DNA gyrase and topoisomerase IV mutations and plasmid-mediated quinolone resistance genes among Escherichia coli and Klebsiella pneumoniae isolated from urinary tract infections in Azerbaijan, Iran. J. Glob. Antimicrob. Resist. 2019, 17, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Bi, W.; Liu, H.; Dunstan, R.A.; Li, B.; Torres, V.V.L.; Cao, J.; Chen, L.; Wilksch, J.J.; Strugnell, R.A.; Lithgow, T.; et al. Extensively Drug-Resistant Klebsiella pneumoniae Causing Nosocomial Bloodstream Infections in China: Molecular Investigation of Antibiotic Resistance Determinants, Informing Therapy, and Clinical Outcomes. Front. Microbiol. 2017, 8, 1230. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Zhang, K.; Chen, W.; Chen, J.; Zheng, J.; Liu, C.; Cheng, L.; Zhou, W.; Shen, H.; Cao, X. Epidemiological characteristics of carbapenem-resistant Enterobacteriaceae collected from 17 hospitals in Nanjing district of China. Antimicrob. Resist. Infect. Control 2020, 9, 15. [Google Scholar] [CrossRef] [Green Version]
- Ruiz, E.; Sáenz, Y.; Zarazaga, M.; Rocha-Gracia, R.; Martínez-Martínez, L.; Arlet, G.; Torres, C. qnr, aac(6′)-Ib-cr and qepA genes in Escherichia coli and Klebsiella spp.: Genetic environments and plasmid and chromosomal location. J. Antimicrob. Chemother. 2012, 67, 886–897. [Google Scholar] [CrossRef]
- Rodríguez-Martínez, J.M.; Díaz de Alba, P.; Briales, A.; Machuca, J.; Lossa, M.; Fernández-Cuenca, F.; Rodríguez Baño, J.; Martínez-Martínez, L. Contribution of OqxAB efflux pumps to quinolone resistance in extended-spectrum-β-lactamase-producing Klebsiella pneumoniae. J. Antimicrob. Chemother. 2013, 68, 68–73. [Google Scholar] [CrossRef] [Green Version]
- Lu, X.; Hu, Y.; Luo, M.; Zhou, H.; Wang, X.; Du, Y.; Li, Z.; Xu, J.; Zhu, B.; Xu, X.; et al. MCR-1.6, a New MCR Variant Carried by an IncP Plasmid in a Colistin-Resistant Salmonella enterica Serovar Typhimurium Isolate from a Healthy Individual. Antimicrob. Agents Chemother. 2017, 61, e02632-16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, Y.; Yang, X.; Li, J.; Lv, N.; Liu, F.; Wu, J.; Lin, I.Y.; Wu, N.; Weimer, B.C.; Gao, G.F.; et al. The Bacterial Mobile Resistome Transfer Network Connecting the Animal and Human Microbiomes. Appl. Environ. Microbiol. 2016, 82, 6672–6681. [Google Scholar] [CrossRef] [Green Version]
- Todorovic, D.; Velhner, M.; Milanov, D.; Vidanovic, D.; Suvajdzic, L.; Stojanov, I.; Krnjaic, D. Characterization of tetracycline resistance of salmonella enterica subspecies enterica serovar infantis isolated from poultry in the northern part of serbia. Acta Vet.-Beogr. 2015, 65, 548–556. [Google Scholar] [CrossRef] [Green Version]
- Deiss, R.G.; Bolaris, M.; Wang, A.; Filler, S.G. Cryptococcus gattii Meningitis Complicated by Listeria monocytogenes Infection. Emerg. Infect. Dis. 2016, 22, 1669. [Google Scholar] [CrossRef] [Green Version]
- Wick, R.R.; Judd, L.M.; Gorrie, C.L.; Holt, K.E. Unicycler: Resolving bacterial genome assemblies from short and long sequencing reads. PLoS Comput. Biol. 2017, 13, e1005595. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Bacterial Strains | No. of Isolates with Detected PMQR Gene a | |||||||
|---|---|---|---|---|---|---|---|---|
| qnr | aac | oqxA+ oqxB | qnr+ oqxA+ oqxB | qnr+ aac | oqxA+ oqxB+ aac | aac+ qnr+ oqxA+ oqxB | Total in Every Species, n (%) | |
| E. coli (n = 112) | 3 (2.7) | 7 (6.3) | 11 (9.8) | 1 (0.9) | 3 (2.7) | 1 (0.89) | 0 (0.0) | 26 (23.2) |
| K. pneumoniae (n = 10) | 0 (0.0) | 0 (0.0) | 1 (10) | 4 (40) | 1 (10) | 1 (10) | 3 (30) | 10 (100) |
| P. mirabilis (n = 2) | 0 (0.0) | 2 (100) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (100) |
| C. braakii (n = 1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (100) | 0 (0.0) | 0 (0.0) | 1 (100) |
| Total (125) | 3 (2.4) | 9 (7.2) | 12 (9.6) | 5 (4.0) | 5 (4.0) | 2 (1.6) | 3 (2.4) | 39 (31.2) |
| Strains | Incompatibility Group plasMINds and the Carrying Resistant Genes | Resistant Genes on Chromosome | Point Mutations of DNA Topoisomerase IV and Gyrase | MDR Phenotype |
|---|---|---|---|---|
| K. pneumoniae | ||||
| H93 | IncR: qnrS; sul1; tet(A); dfrA1 IncX1: floR | OqxA, oqxB; fosA | - | CIP, LVX, NOR, MXF, TET, CHL, SXT |
| H165 | IncN:aac(6′)-Ib-cr, qnrB6; sul1; aadA16; tet(A); dfrA27; ARR-3 IncHI2A: - | blaPLA2a; fosA | - | CIP, LVX, NOR, MXF, TET, SXT |
| H204 | IncHI1B:qnrA; aac(3)-IId, aadA5; catA1; mph(A); sul1, sul2, tet(D); dfrA17 IncHI2A: - | OqxA, oqxB; blaSHV-110, blaSHV-81;fosA | - | CIP, GEN, LVX, MXF, NOR, MIN, CHL, FD, TET, SXT |
| H221 | IncFIB: aac(3)-IId, aph(3′)-Ia IncHI2A: - IncFIB: - | OqxA, oqxB; blaSHV-187; fosA | - | CIP, LVX, NOR, MXF, MIN, TET, CHL, GEN, FD, SXT |
| H224 | IncR: aac(6′)-Ib-cr, qnrB6; aadA16; floR; sul1; tet(D); ARR-3; dfrA27 | OqxA, oqxB; fosA | - | CIP, LVX, NOR, MXF, SAM, TET, MIN, CHL, SXT |
| H233 | IncFIB: aac(6′)-Ib-cr; blaCTX-M-15, blaOXA-1, blaTEM-1B; aadA2; catB3; mph(A); sul1; tet(A); dfrA12 | OqxA, oqxB; fosA | - | CIP, NOR, MXF, LVX, SAM, ATM, CFZ, CAZ, AXO, CXM, TET, TOB, SXT |
| H234 | IncR: aac(6′)-Ib-cr, qnrB52; aac(3)-IId, aadA16, aph(3″)-Ib, aph(3′)-Ia, aph(6)-Id; floR; mph(A); sul; tet(A); dfrA27; ARR-3 IncFIB: - | oqxA, oqxB; fosA | - | CIP, LVX, NOR, MXF, TET, CHL, GEN, FD, SXT |
| H249 | IncR: qnrS1; sul1; tet(A); dfrA1 IncHI2A: - IncL/M(pOXA-48): - | oqxA, oqxB; fosA | - | CIP, LVX, MXF, NOR, FOX, CXM, TET, MIN, CHL, FD, SXT |
| H251 | IncR: aac(6′)-Ib-cr, qnrB91, aadA16; floR; sul1; tet(D); dfrA27; ARR-3 IncFIB: - IncHI1B: - | oqxA, oqxB; fosA | - | CIP, LVX, NOR, MXF, MIN, TET, CHL, FD, SXT |
| E. coli | ||||
| H8 | IncFII:aac(6′)-Ib-cr; blaOXA-1; aadA5; catA1, catB3; mph(A); sul1; tet(B); dfrA17 IncB: - IncO: - IncK: - IncZ: - | mdf(A) | parC; gyrA; parE | CIP, LVX, NOR, MXF, SAM, TET, TOB, SXT |
| H32 | IncFIB: oqxA, oqxB; aac(3)-IId, aadA2; floR; dfrA12; tet(A) IncFII(29): - | mdf(A) | gyrA; parC | CHL, CIP, LVX, MXF, NOR, TET, GEN, TOB |
| H40 | IncFIB: oqxA, oqxB; aac(3)-IId, aadA, aadA2, aph(3″)-Ib, aph(6)-Id; cmlA1, floR; sul3; tet(A); dfrA12 | mdf(A) | gyrA; parE; parC | CHL, CIP, GEN, FD, MXF, LVX, NOR, TET, TOB, SXT |
| H45 | IncFII: aac(6′)-Ib-cr, oqxA, oqxB; blaCTX-M-55; aac(6′)-Ib3, aadA5; floR; sul2; tet(A); dfrA17; fosA3 | mdf(A) | gyrA; parC | CHL, CIP, MXF, LVX, NOR, ATM, CFZ, AXO, CXM, TET, TOB, FOS, SXT |
| H58 | IncFIB: qnrS13; dfrA14; tet(A); floR IncHI2: oqxA, oqxB, qnrS2; blaCTX-M-65; sul1; tet(A) | mdf(A) | gyrA; parC | CIP, LVX, NOR, MXF, ATM, AXO, CFZ, CXM, TE, CHL |
| H62 | p0111: blaOXA-10; aadA1; tet(A); dfrA14; sul2; floR, cmlA1; ARR-2 IncI1: aac(6′)-Ib-cr; blaCTX-M-14b; aadA16; sul; floR; dfrA27; ARR-3 IncI2: mcr-1.1 IncFIB: - IncFII: - Col(MG828): - | mdf(A) | parE; parC; gyrA | CIP, LVX, MXF, NOR, SAM, CFZ, FEP, AXO, CXM, TET, CHL, TOB, SXT, COL |
| H66 | IncFIB: blaTEM-1B; aadA5, aac(3)-IId, aph(3″)-Ib, aph(6)-Id; mph(A); sul2, sul1; tet(A) IncHI1A: - IncHI1B: - IncX9: - | aac(6′)-Ib-cr, qnrS2; blaCTX-M-65, blaOXA-1; floR, catB3; mdf(A); ARR-3 | parC; gyrA | CIP, LVX, MXF, NOR, SAM, ATM, CFZ, AXO, CXM, TET, CHL, GEN, TOB, SXT |
| H68 | IncN: blaCARB-2; aac(3)-IId, aadA1, aadA2b, aph(3′)-Ia; sul3; tet(M); cmlA1, floR; dfrA17 IncFII: qnrS1; blaTEM-1B; floR; mph(A), erm(B) IncX1: aph(3″)-Ib, aph(6)-Id; tet(B) IncX4: mcr-1.1 | mdf(A) | parC; gyrA | CIP, NOR, MXF, LVX, SAM, CHL, MIN, TET, GEN, TOB, SXT, COL |
| H74 | IncFIB:oqxA, oqxB; aph(3′)-Ia, aph(4)-Ia, aac(3)-IV, aph(3″)-Ib, aph(3′)-Ia, aph(6)-Id; mph(A); sul2; tet(A); dfrA12; floR IncFII: blaCTX-M-55; fosA3 | - | gyrA; parC | CIP, LVX, NOR, MXF, SAM, ATM, FEP, CFZ, AXO, CXM, TET, CHL, GEN, TOB, FOS |
| H84 | IncR: oqxA, oqxB; blaTEM-1B; floR | mdf(A) | parC; gyrA | CIP, LVX, NOR, MXF, TET, CHL |
| H91 | IncFIA-IncHI1B-IncQ1: qnrB6, aac(6′)-Ib-cr; aph(3′)-Ia, aac(3)-IId, aadA16, aph(3″)-Ib, aph(6)-Id; sul2; tet(B), tet(M); dfrA27; ARR-3 IncI1: floR IncX1: - Col440II: - | blaTEM-1B; mdf(A), mph(A) | gyrA; parE; parC | CIP, LVX, MXF, NOR, SAM, CFZ, SCP, AXO, CXM, MIN, TET, CHL, GEN, TOB, SXT |
| H104 | IncA/C2: oqxA, oqxB; blaCMY-2; sul1, sul2; aac(6′)-Il, aph(6)-Id, aph(3″)-Ib, aph(3′)-Ia; mph(A); tet(A) IncFII/IncN: blaCTX-M-55 Col156: - | mdf(A) | gyrA; parC | CIP, LVX, NOR, MXF, AMC, SAM, ATM, FEP, CFZ, FOX, SCP, CAZ, AXO, CXM, TET, CHL, TOB, FOS, SXT |
| H108 | IncFIA: aac(6′)-Ib-cr; blaOXA-1, blaCTX-M-15; aadA5; catB3; mph(A); sul1; tet(A); dfrA17 Col440II: - | mdf(A) | parE; gyrA; parC | CIP, LVX, NOR, MXF, FEP, SAM, ATM, CFZ, SCP, CAZ, AXO, CXM, TET, TOB, SXT |
| H114 | IncFIB: oqxA, oqxB; blaCTX-M-55; aadA5, aph(3″)-Ib, aph(6)-Id; sul2; tet(A); dfrA17; floR | mdf(A) | gyrA; parC | CIP, LVX, NOR, MXF, ATM, CFZ, FEP, CAZ, AXO, CXM, TET, CHL, SXT |
| H115 | IncN: oqxA, oqxB; blaTEM-1C; aadA2, aph(3″)-Ib, aph(6)-Id; floR; mph(A); sul2; tet(A); dfrA12 Col440I: - | mdf(A) | gyrA; parC | CIP, LVX, NOR, MXF, TET, CHL, SXT |
| H133 | IncFII-IncN: oqxA, oqxB; blaCTX-M-55; aph(3″)-Ib, aph(3′)-IIa, aph(6)-Id; floR; sul2; tet(A); dfrA14 Col(MG828): - | - | parC; gyrA | CIP, LVX, NOR, MXF, ATM, CFZ, FEP, CAZ, AXO, CXM, TET, CHL, FD, SXT |
| H167 | IncFIB: qnrS1; floR; tet(A); dfrA14 | mdf(A) | gyrA; parC | CIP, LVX, NOR, MXF, TET, CHL |
| H175 | IncFIA: aadA5; mph(A); sul1; tet(A); dfrA17 | aac(6′)-Ib-cr; blaCTX-M-15, blaOXA-1; catB3; aac(3)-IIa; mdf(A) | parC; gyrA; parE | CIP, LVX, NOR, MXF, ATM, CFZ, FEP, CAZ, AXO, CXM, TET, GEN, TOB, SXT |
| H176 | IncFIA: aadA5; mph(A); sul; tet(A); dfrA17 IncFII: - | aac(6′)-Ib-cr;blaCTX-M-15, blaOXA-1; catB3; aac(3)-IIa; mdf(A) | gyrA; parE; parC | CIP, LVX, NOR, MXF, ATM, CFZ, FEP, CAZ, AXO, CXM, TET, GEN, TOB, SXT |
| H205 | IncFIC: qnrS; blaTEM-1B; aph(3″)-Ib, aph(6)-Id; sul; tet(A); dfrA14 | mdf(A) | parE; gyrA; parC | CIP, LVX, NOR, MXF, SAM, CFZ, FOX, AXO, CXM, TET, SXT |
| H225 | IncFIA: aac(6′)-Ib-cr; blaCTX-M-15, blaOXA-1; aadA5, aac(3)-IIa; catB3; sul; dfrA17; mph(A) IncN:qnrS1; blaTEM-1B; mph(A) IncL/M: - | mdf(A); tet(B) | gyrA; parC; parE | CIP, LVX, NOR, MXF, SAM, ATM, CFZ, FEP, CAZ, AXO, CXM, TET, GEN, TOB, SCP |
| H226 | RepA: aac(6′)-Ib-cr; blaOXA-1, blaTEM-1B; aac(3)-IIa, aadA2b; catA2, catB3, cmlA; ere(A); sul1, sul2; tet(D); dfrA19; fosA3; ARR-3 IncX1: - | mdf(A) | gyrA; parC | CIP, LVX, NOR, MXF, SAM, TET, CHL, GEN, TOB, SXT |
| H227 | RepA: aac(6′)-Ib-cr; blaOXA-1, blaTEM-1B; aac(3)-IIa, aadA2b; catA2, catB3, cmlA; ere(A); tet(D); sul1, sul2; dfrA19; fosA3; ARR-3 IncX1: - | mdf(A) | gyrA; parC | CIP, LVX, NOR, MXF, SAM, TET, CHL, GEN, TOB, SXT |
| H238 | IncQ1:oqxA, oqxB; blaTEM-1B, blaCTX-M-27; aph(3″)-Ib, aph(3′)-Ia, aph(6)-Id; catA1; sul2; tet(B); dfrA17 IncFIB: - | - | gyrA; parC | CIP, LVX, NOR, MXF, ATM, CFZ, FEP, AXO, CXM, CHL, TET, SXT |
| H240 | IncQ1: - | oqxA, oqxB; blaTEM-1B; aadA5, aph(3″)-Ib, aph(6)-Id; tet(A); mdf(A); sul2; dfrA17 | gyrA; parC | CIP, LVX, NOR, MXF, SAM, TET, FD, SXT |
| H250 | IncFIB: oqxA, oqxB; blaTEM-1B; aac(3)-IId, aadA2; mph(A), tet(A); dfrA12 IncI1: floR; sul2 | mdf(A) | parC; gyrA; parE | CIP, LVX, NOR, MXF, NOR, CHL, TET, GE, TOB, FD, SXT |
| C. braakii | ||||
| H138 | IncR:qnrB6, aac(6′)-Ib-cr; aadA16, aph(6)-Id; mph(A); sul1; tet(A); dfrA27; ARR-3; floR | - | - | CIP, LVX, MFX, NOR, AMC, CFZ, FOX, TET, CHL, SXT |
| Drug Resistance a | K. pneumoniae | E. coli |
|---|---|---|
| CIP | 100% | 100% |
| NOR | 0% | \ |
| FEP | 40% | 69.20% |
| FOX | 90% | 100.00% |
| CAZ | 50% | 65.40% |
| AXO | 30% | \ |
| AMC | 90% | \ |
| TZP | 90% | 53.80% |
| ATM | 50% | \ |
| TET | 70% | 100% |
| TGC | 60% | 100% |
| MIN | 30% | \ |
| CHL | 90% | 76.90% |
| AK | 50% | 53.80% |
| GEN | 100% | 100% |
| TOB | 40% | 100% |
| ETP | 100% | 100% |
| IMI | 100% | 100% |
| MEC | 100% | 100% |
| FOS | 10% | 92.30% |
| SXT | 90% | 88.40% |
| COL | \ | 100% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Long, Y.; Lu, X.; Ni, X.; Liu, J.; Wang, M.; Li, X.; Li, Z.; Zhou, H.; Li, Z.; Wu, K.; et al. High Carriage Rate of the Multiple Resistant Plasmids Harboring Quinolone Resistance Genes in Enterobacter spp. Isolated from Healthy Individuals. Antibiotics 2022, 11, 15. https://doi.org/10.3390/antibiotics11010015
Long Y, Lu X, Ni X, Liu J, Wang M, Li X, Li Z, Zhou H, Li Z, Wu K, et al. High Carriage Rate of the Multiple Resistant Plasmids Harboring Quinolone Resistance Genes in Enterobacter spp. Isolated from Healthy Individuals. Antibiotics. 2022; 11(1):15. https://doi.org/10.3390/antibiotics11010015
Chicago/Turabian StyleLong, Yongyan, Xin Lu, Xiansheng Ni, Jiaqi Liu, Mengyu Wang, Xu Li, Zhe Li, Haijian Zhou, Zhenpeng Li, Kui Wu, and et al. 2022. "High Carriage Rate of the Multiple Resistant Plasmids Harboring Quinolone Resistance Genes in Enterobacter spp. Isolated from Healthy Individuals" Antibiotics 11, no. 1: 15. https://doi.org/10.3390/antibiotics11010015





