Antimicrobial Activity of Polyphenols and Natural Polyphenolic Extracts on Clinical Isolates
Abstract
:1. Introduction
2. Antibacterial Activity of Polyphenol Extracts in Clinical Isolates
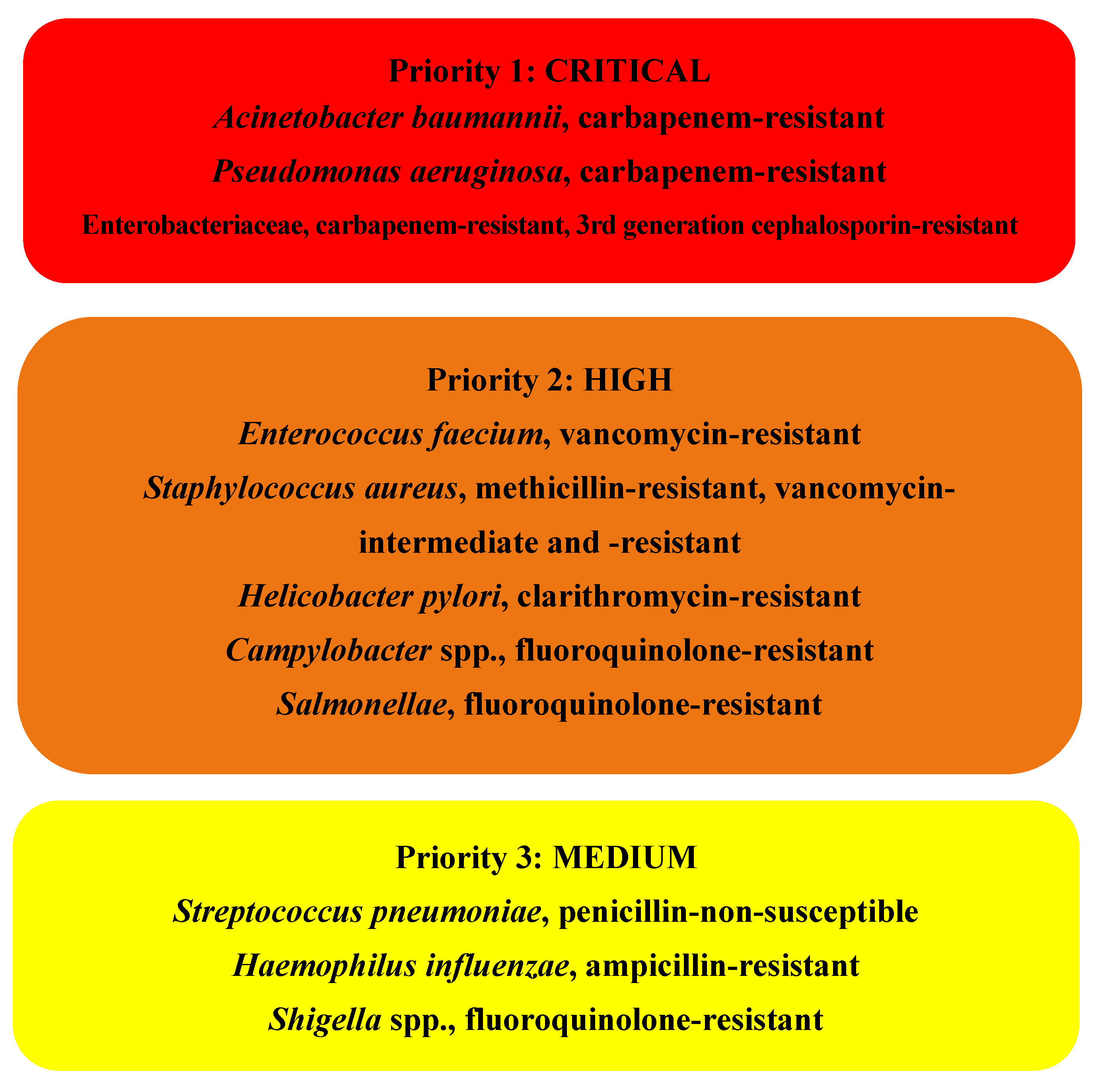
2.1. Bacteria Belonging to Priority 1: Critical
2.1.1. Acinetobacter baumannii
2.1.2. Pseudomonas aeruginosa
2.1.3. Enterobacteriaceae
- -
- K. pneumoniae: extracts of Acacia nilotica, Cinnamum zeylanicum and Syzygium aromaticum [26], tea polyphenols (catechins, EGCG, ECG (epigallocatechin) GCG (epicatechin gallate), EC (epicatechin) [27], extracts of C. longa [25], extracts of Prosopis laevigata and Opuntia ficus-indica [28], extracts of Lawsonia inermis (Klebsiella spp.) [29] and extracts obtained from leaves and inflorescences of different species of A. retroflexus vegetative organs [23];
- -
- E. coli: extracts of A. nilotica, C. zeylanicum and S. aromaticum [26], extracts of C. longa [25], extracts of P. laevigata, O. ficus-indica and Gutierrezia microcephala [28], extracts of L. inermis [29], extracts of Punica granatum [30] and extracts obtained from leaves and inflorescences of different species of A. retroflexus vegetative organs [23];
- -
- -
- -
2.2. Bacteria Belonging to Priority 2: High
2.2.1. Staphylococcus aureus
2.2.2. Helicobacter pylori
2.3. Bacteria out of the Who Classification
| Botanical Extract | Phenolic Compounds | Microorganisms | Clinical Samples | Synergism with Antibiotics | Ref. |
|---|---|---|---|---|---|
| S. baicalensis R. rugosa T. chebula | Norwogonin, ellagic acid chebulagic acid, chebulinic acid, corilagin and terchebulin | A. baumannii (3 MDR strains) | 1 blood, 2 respiratory | Ampicillin/sulbactam, azithromycin, cefepime, colistin, imipenem, levofloxacin, minocycline, rifampin, tobramycin, trimethoprim/sulfamethoxazole | [20] |
| - | Epicatechin, theaflavin | A. baumannii S. maltophilia | Sputum | [21] | |
| P. cuspidatum | S. aureus (3 strains) A. baumannii (3 strains) P. aeruginosa (4 strains) | blood and sputum | Erytromycin, gentamicin, tetracycline, spectinomycin, piperacillin, G kanamycin, amikacin, clindamycin, ampicillin, cephalosporinin, trimethoprim/sulfamethoxazole, amoxillin | [22] | |
| A. retroflexus | Not determined (literature: rich in polyphenols) * | S. aureus B. subtilis P. aeruginosa E. coli K. pneumoniae A. baumannii | Trimetoprim-sulphamethoxazole, piperacillin-tazobactam, ticarcillin-clavulanic acid, piperacillin, ceftriaxone, cefotaxime, cephalexin, penicillin, cefaclor, chloramphenicol, ciprofloxacin, kanamycin, colistin, vancomycin | [23] | |
| Epigallocatechin gallate | P. aeruginosa (15 MDR strains) | Aztreonam, cefotaxime | [24] | ||
| C. longa L. (Zingiberaceae) | Tannins, flavonoids | E. coli P. aeruginosa K. pneumoniae Proteus sp. Salmonella sp. Bacillus sp. | [25] | ||
| A. nilotica C. zeylanicum S. aromaticum | Not defined | K. pneumoniae E. coli | [26] | ||
| S. secundiflora S. ambigua P. laevigata O. ficus-indica M. vulgare S. drummondi N. bivalve G. microcephala | Tannins, flavonoids | K. pneumoniae E. faecalis E. coli S. maltophilia S. aureus | [28] | ||
| L. inermis | Tannins and other polyphenols | E. coli S. typhi Klebsiella spp. S. sonnei B. subtilis S. aureus S. epidermidis | [29] | ||
| P. granatum. | Pomegranate juice: anthocyanins (delphinidin, cyanidin glucosides), hydrolysable tannins (gallotannins), ellagitannins and gallagyl esters, hydroxybenzoic and hydroxycinnamic acids. Promegranate peel: bis-HHDP-hexoside (pedunculagin I), punicalin, ellagic acid (hexose, pentose and deoxyhexose derivatives) | S.aureus E.coli | Pharyngeal sample, sputum | [30] | |
| T. alternifolia | Flavonoids | S. aureus (11 MRSA strains, 4 VRSA strains) | Skin infections | [31] | |
| - | Flavonols:morin, quercetin, kaempferol Flavanols and derivatives: (−)-epigallocatechin gallate, (+)-catechin acyl derivates, epicatechin gallate 3-O-decyl-(+)-catechin, (+)-catechin Phenolic acids and derivatives:protocatechuic acid, ethyl ester, caffeic acid | S. aureus | [32] | ||
| C. salviifolius C. paradisi P. granatum C. salviifolius C. paradisi P. granatum | C. salviifolius: (epi)gallocatechin and its dimer pedunculagin I coumaroylquinic acid prodelphinidin B2-3′-O-gallate, punicalagin I and II, caffeoyl-hexose, myricetin hexoside, tergallic-C-glucoside, myricetin 3-arabinoside I and II, quercetin glucoside, ellagic acid-7-xiloside I and II, kaempferol diglycoside P. granatum: HHDP glucoside isomers, galloyl glucosa, punicalin, pedunculagin I, punicalagin isomers I, II and III, punigluconin, quercetin glucoside, ellagic acid rhamnoside, ellagic acid * gallic acid punicalagin, quercetin-3-glucuronide, myricetin, naringenin, ellagic acid | S. aureus (100 strains, 50 MRSA) S. aureus (100 strains, 50 MRSA) | [33] | ||
| M. indica L. | Pentagalloylglucopyranose, methyl gallate and gallic acid The same isolated phenolic principles | S. aureus (19 strains MRSA) | Penicillin | [34] | |
| P. vera L. | Hydroxybenzoic acids (gallic acid, protocatechuic acid), flavan-3-ols (+-catechin), flavonols (isoquercetin) * | S. aureus (44 strains, 9 MRSA) | Skin and surgical infections | [35] | |
| P. vera L. | Hydroxybenzoic acids: gallic acid, protocathecuic acid, hydroxybenzoic acid, vanillic acid Hydroxycinnamic acids: chlorogenic acid, caffeic acid, cumaric acid Flavanones: eryodictiol, eryodictiol-7-O-glucoside, naringenin, naringin Flavonols: kaempferol-3-O-rutinoside, quercetin, quercetin-3-O-rutinoside, quercetin-3-O-glucoside Flavones: amentoflavone, luteolin, apigenin Isoflavones: daidzein, genistein Flavanols: epicatechin, catechin * | Staphylococcus: (31 strains) S. aureus (23, 21 MRSA) S. epidermidis (2) S. lugdunensis (2) S. hominis (1) S. xylosus (1) Staphylococcus (1 not identified) | Orthopedic infections: 16 knee prosthesis or surgical wounds, 7 hip prosthesis, and other orthopedic sites | [36] | |
| 19 Chinese medicinal plants: D. capitata | Polyphenols | S. aureus (9 MRSA strains) | [37] | ||
| V. vinifera V. rotundifolia | Ellagic acid, myricetin, quercetin, resveratrol | H. pylori | [38] | ||
| - | Epigallocatechin-3-gallate | S. maltophilia (40 strains) | 19 respiratory samples, 8 bloodstream infections, 7 catheter tips, 3 wounds, 2 drain fluids and 1 ileal biopsy | [39] |
| Botanical Extract | Phenolic Compounds | Microorganisms | Ref. |
|---|---|---|---|
| A. retroflexus | Not determined (literature: rich in polyphenols) * | C. famata, C. utilis, C. albicans, S. cerevisiae | [23] |
| A. nilotica, C. zeylanicum S. aromaticum | Not defined | C. albicans | [26] |
| D. longan | Gallic acid, ellagic acid, corilagin * Reference compounds of the same polyphenols | Candida species, C. neoformans and some dermatophytes, C. albicans (9 strains), C.neoformans (4 strains), filamentous fungi (T. rubrum, T. mentagrophytes, M. gypseum, M. canis, E. floccosum, P. boydii, P. siamensis, P. pinophilum, P. marneffei, A. nidulans, A. niger and A. fumigatus) | [40] |
| Resveratrol | C. albicans (30 strains) Fluconazole resistant strains of C. albicans ** (3 strains) | [41] |
3. Antifungal Activity on Clinical Isolates
- -
- Ellagic acid exhibited the best antifungal activity, followed by corilagin and gallic acid, respectively.
- -
- The three polyphenolic compounds (gallic acid, ellagic acid, and corilagin) were active against Candida species and C. neoformans;
- -
- Ellagic acid and longan seed extracts inhibited the growth of C. albicans and C. neoformans (with longan seed extract being more effective than pure ellagic acid). Ellagic acid showed better activity against Candida parapsilosis and C. neoformans than against Candida krusei and some C. albicans clinical strains;
- -
- Gallic acid exhibited better antifungal activity against C. parapsilosis and most C. albicans strains than against C. krusei and C. neoformans;
- -
- Corilagin demonstrated a low effect against both Candida sp. and C. neoformans;
- -
- Regarding dermatophytes, ellagic acid demonstrated weak antifungal activity against T. rubrum, M. gypseum and E. floccosum. Gallic acid and corilagin could not inhibit the growth of these dermatophytes.
- -
- Longan seed extract demonstrated the best antifungal activity, while pulp and whole fruit extracts showed no effects;
- -
- Longan seed extract (Baidam) was more active against C. parapsilosis than against C. albicans, C. neoformans and C. krusei, while longan seed extract (Edor) showed worse antifungal activity against C. parapsilosis, C. krusei and C. neoformans than Baidam. Edor did not show better antifungal activity than Baidam against C. albicans. Higher amounts of gallic acid and ellagic acid in Baidam seed extract could be related to its higher inhibitory activity on C. krusei, C. parapsilosis and C. neoformans than Edor seed extract;
- -
- Regarding dermatophytes, longan seed extract exhibited a weak antifungal effect on the tested species of dermatophytes, including T. rubrum, M. gypseum and E. floccosum;
- -
- None of the tested longan extracts showed antifungal activity against the filamentous fungi tested: A. niger, A. nidulans, A. fumigatus, P. marneffei, P. siamensis, P. pinophilum, T. mentagrophytes, T. rubrum, M. gypseum, M. canis, and P. boydii [40].
4. Concluding Remarks
Author Contributions
Funding
Conflicts of Interest
References
- Agencia Española de Medicamentos y Productos Sanitarios (AEMPS). Nota Informativa 11/2010 Los Líderes Mundiales Reunidos en la Asamblea General de las Naciones Unidas se Comprometen a Adoptar una Estrategia Contra la Resistencia a los Antibióticos. Available online: https://www.aemps.gob.es/informa/notasInformativas/laAEMPS/2016/docs/NI-AEMPS_11-2016-reunion-ONU-antibioticos.pdf?x89163 (accessed on 5 November 2021).
- AEMPS. Plan Nacional Frente a la Resistencia a los Antibióticos 2019–2021. Available online: http://www.resistenciaantibioticos.es/es/system/files/field/files/pran_2019-2021_0.pdf?file=1&type=node&id=497&force=0 (accessed on 5 November 2021).
- Écoantibio 2: Plan National de Réduction des Risques D’antibiorésistance en Médecine Vétérinaire (2017–2022). Available online: https://agriculture.gouv.fr/le-plan-ecoantibio-2-2017-2022. (accessed on 9 November 2021).
- DART 2020 Fighting Antibiotic Resistance for the Good of both Humans and Animals. Available online: https://www.bmel.de/SharedDocs/Downloads/EN/Publications/DART2020.pdf;jsessionid=C332D8B25955F30CC57A8BDFF94EB91D.live852?__blob=publicationFile&v=3 (accessed on 9 November 2021).
- Swiss Antibiotic Resistance Report 2020. Available online: https://www.star.admin.ch/star/en/home.html (accessed on 9 November 2021).
- WHO Publishes List of Bacteria for Which New Antibiotics Are Urgently Needed. Available online: https://www.who.int/news/item/27-02-2017-who-publishes-list-of-bacteria-for-which-new-antibiotics-are-urgently-needed (accessed on 5 November 2021).
- Asokan, G.V.; Ramadhan, T.; Ahmed, E.; Sanad, H. WHO global priority pathogens list: A bibliometric analysis of medline-pubmed for knowledge mobilization to infection prevention and control practices in Bahrain. Oman Med. J. 2019, 34, 184–193. [Google Scholar] [CrossRef]
- Rice, L.B. Federal funding for the study of antimicrobial resistance in nosocomial pathogens: No ESKAPE. J. Infect. Dis. 2008, 197, 1079–1081. [Google Scholar] [CrossRef] [PubMed]
- Mulani, M.S.; Kamble, E.E.; Kumkar, S.N.; Tawre, M.S.; Pardesi, K.R. Emerging strategies to combat ESKAPE pathogens in the era of antimicrobial resistance: A review. Front. Microbiol. 2019, 10, 539. [Google Scholar] [CrossRef] [PubMed]
- Daglia, M. Polyphenols as antimicrobial agents. Curr. Opin. Biotechnol. 2012, 23, 174–181. [Google Scholar] [CrossRef]
- Fraga, C.G.; Croft, K.D.; Kennedy, D.O.; Tomás-Barberán, F.A. The effects of polyphenols and other bioactives on human health. Food Funct. 2019, 10, 514–528. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Efenberger-Szmechtyk, M.; Nowak, A.; Czyzowska, A. Plant extracts rich in polyphenols: Antibacterial agents and natural preservatives for meat and meat products. Crit. Rev. Food Sci. Nutr. 2021, 61, 149–178. [Google Scholar] [CrossRef]
- Olszewska, M.A.; Gędas, A.; Simões, M. Antimicrobial polyphenol-rich extracts: Applications and limitations in the food industry. Food Res. Int. 2020, 134, 109214. [Google Scholar] [CrossRef]
- Skroza, D.; Šimat, V.; Smole Možina, S.; Katalinić, V.; Boban, N.; Generalić Mekinić, I. Interactions of resveratrol with other phenolics and activity against food-borne pathogens. Food Sci. Nutr. 2019, 7, 2312–2318. [Google Scholar] [CrossRef] [Green Version]
- Bouarab Chibane, L.; Degraeve, P.; Ferhout, H.; Bouajila, J.; Oulahal, N. Plant antimicrobial polyphenols as potential natural food preservatives. J. Sci. Food Agric. 2019, 99, 1457–1474. [Google Scholar] [CrossRef] [Green Version]
- Gutiérrez-del-Río, I.; Fernández, J.; Lombó, F. Plant nutraceuticals as antimicrobial agents in food preservation: Terpenoids, polyphenols and thiols. Int. J. Antimicrob. Agents 2018, 52, 309–315. [Google Scholar] [CrossRef]
- Rama, J.L.R.; Mallo, N.; Biddau, M.; Fernandes, F.; de Miguel, T.; Sheiner, L.; Choupina, A.; Lores, M. Exploring the powerful phytoarsenal of white grape marc against bacteria and parasites causing significant diseases. Environ. Sci. Pollut. Res. Int. 2021, 28, 24270–24278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Álvarez-Martínez, F.J.; Barrajón-Catalán, E.; Encinar, J.A.; Rodríguez-Díaz, J.C.; Micol, V. Antimicrobial Capacity of Plant Polyphenols against Gram-positive Bacteria: A Comprehensive Review. Curr. Med. Chem. 2020, 27, 2576–2606. [Google Scholar] [CrossRef] [PubMed]
- Gato, E.; Rosalowska, A.; Martínez-Guitián, M.; Lores, M.; Bou, G.; Pérez, A. Anti-adhesive activity of a Vaccinium corymbosum polyphenolic extract targeting intestinal colonization by Klebsiella pneumoniae. Biomed. Pharmacother. 2020, 132, 110885. [Google Scholar] [CrossRef] [PubMed]
- Miyasaki, Y.; Rabenstein, J.D.; Rhea, J.; Crouch, M.L.; Mocek, U.M.; Kittell, P.E.; Morgan, M.A.; Nichols, W.S.; van Benschoten, M.M.; Hardy, W.D.; et al. Isolation and Characterization of Antimicrobial Compounds in Plant Extracts against Multidrug-Resistant Acinetobacter baumannii. PLoS ONE 2013, 8, e61594. [Google Scholar] [CrossRef] [Green Version]
- Betts, J.W.; Kelly, S.M.; Haswell, S.J. Antibacterial effects of theaflavin and synergy with epicatechin against clinical isolates of Acinetobacter baumannii and Stenotrophomonas maltophilia. Int. J. Antimicrob. Agents 2011, 38, 421–425. [Google Scholar] [CrossRef] [Green Version]
- Su, P.W.; Yang, C.H.; Yang, J.F.; Su, P.Y.; Chuang, L.Y. Antibacterial activities and antibacterial mechanism of polygonum cuspidatum extracts against nosocomial drug-resistant pathogens. Molecules 2015, 20, 11119–11130. [Google Scholar] [CrossRef] [Green Version]
- Marinaş, I.C.; Chifiriuc, C.; Oprea, E.; Lazăr, V. Antimicrobial and antioxidant activities of alcoholic extracts obtained from vegetative organs of A. retroflexus. Roum. Arch. Microbiol. Immunol. 2014, 73, 35–42. [Google Scholar]
- Betts, J.W.; Hornsey, M.; Higgins, P.G.; Lucassen, K.; Wille, J.; Salguero, F.J.; Seifert, H.; la Ragione, R.M. Restoring the activity of the antibiotic aztreonam using the polyphenol epigallocatechin gallate (EGCG) against multidrug-resistant clinical isolates of Pseudomonas aeruginosa. J. Med. Microbiol. 2019, 68, 1552–1559. [Google Scholar] [CrossRef]
- Álvarez, N.M.; Ortíz, A.A.; Martínez, O.C. In Vitro antibacterial activity of Curcuma longa (Zingiberaceae) against nosocomial bacteria in Montería, Colombia. Rev. Biol. Trop. 2016, 64, 1201–1208. [Google Scholar] [CrossRef]
- Khan, R.; Islam, B.; Akram, M.; Shakil, S.; Ahmad, A.; Ali, S.M.; Siddiqui, M.; Khan, A.U. Antimicrobial activity of five herbal extracts against Multi Drug Resistant (MDR) strains of bacteria and fungus of clinical origin. Molecules 2009, 14, 586–597. [Google Scholar] [CrossRef]
- Zhang, N.; Liu, W.; Qian, K. In-Vitro antibacterial effect of tea polyphenols combined with common antibiotics on multidrug-resistant Klebsiella pneumoniae. Minerva Med. 2020, 111, 536–543. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, E.; Rivas Morales, C.; Castillo, S.; Leos-Rivas, C.; García-Becerra, L.; Ortiz Martínez, D.M. Antibacterial and Antibiofilm Activity of Methanolic Plant Extracts against Nosocomial Microorganisms. Evid. Based Complement. Alternat. Med. 2016, 2016, 1572697. [Google Scholar] [CrossRef] [Green Version]
- Gull, I.; Sohail, M.; Aslam, M.S.; Athar, M.A. Phytochemical, toxicological and antimicrobial evaluation of lawsonia inermis extracts against clinical isolates of pathogenic bacteria. Ann. Clin. Microbiol. Antimicrob. 2013, 12, 36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pagliarulo, C.; de Vito, V.; Picariello, G.; Colicchio, R.; Pastore, G.; Salvatore, P.; Volpe, M.G. Inhibitory effect of pomegranate (Punica granatum L.) polyphenol extracts on the bacterial growth and survival of clinical isolates of pathogenic Staphylococcus aureus and Escherichia coli. Food Chem. 2016, 190, 824–831. [Google Scholar] [CrossRef] [PubMed]
- Marathe, N.P.; Rasane, M.H.; Kumar, H.; Patwardhan, A.A.; Shouche, Y.S.; Diwanay, S.S. In Vitro antibacterial activity of Tabernaemontana alternifolia (Roxb) stem bark aqueous extracts against clinical isolates of methicillin resistant Staphylococcus aureus. Ann. Clin. Microbiol. Antimicrob. 2013, 12, 26. [Google Scholar] [CrossRef] [Green Version]
- Miklasińska-Majdanik, M.; Kępa, M.; Wojtyczka, R.D.; Idzik, D.; Wąsik, T.J. Phenolic Compounds Diminish Antibiotic Resistance of Staphylococcus Aureus Clinical Strains. Int. J. Environ. Res. Public Health 2018, 15, 2321. [Google Scholar] [CrossRef] [Green Version]
- Álvarez-Martínez, F.J.; Rodríguez, J.C.; Borrás-Rocher, F.; Barrajón-Catalán, E.; Micol, V. The antimicrobial capacity of Cistus salviifolius and Punica granatum plant extracts against clinical pathogens is related to their polyphenolic composition. Sci. Rep. 2021, 11, 588. [Google Scholar] [CrossRef]
- Jiamboonsri, P.; Pithayanukul, P.; Bavovada, R.; Chomnawang, M.T. The inhibitory potential of thai mango seed kernel extract against methicillin-resistant staphylococcus aureus. Molecules 2011, 16, 6255–6270. [Google Scholar] [CrossRef] [Green Version]
- Bisignano, C.; Filocamo, A.; Faulks, R.M.; Mandalari, G. In Vitro antimicrobial activity of pistachio (Pistacia vera L.) polyphenols. FEMS Microbiol. Lett. 2013, 341, 62–67. [Google Scholar] [CrossRef] [Green Version]
- La Camera, E.; Bisignano, C.; Crisafi, G.; Smeriglio, A.; Denaro, M.; Trombetta, D.; Mandalari, G. Biochemical Characterization of Clinical Strains of Staphylococcus spp. and Their Sensitivity to Polyphenols-Rich Extracts from Pistachio (Pistacia vera L.). Pathogens 2018, 7, 82. [Google Scholar] [CrossRef] [Green Version]
- Zuo, G.Y.; Wang, G.C.; Zhao, Y.B.; Xu, G.L.; Hao, X.Y.; Han, J.; Zhao, Q. Screening of Chinese medicinal plants for inhibition against clinical isolates of methicillin-resistant Staphylococcus aureus (MRSA). J. Ethnopharmacol. 2008, 120, 287–290. [Google Scholar] [CrossRef]
- Brown, J.C.; Huang, G.; Haley-Zitlin, V.; Jiang, X. Antibacterial effects of grape extracts on helicobacter pylori. Appl. Environ. Microbiol. 2009, 75, 848–852. [Google Scholar] [CrossRef] [Green Version]
- Gordon, N.C.; Wareham, D.W. Antimicrobial activity of the green tea polyphenol (-)-epigallocatechin-3-gallate (EGCG) against clinical isolates of Stenotrophomonas maltophilia. Int. J. Antimicrob. Agents 2010, 36, 129–131. [Google Scholar] [CrossRef]
- Rangkadilok, N.; Tongchusak, S.; Boonhok, R.; Chaiyaroj, S.C.; Junyaprasert, V.B.; Buajeeb, W.; Akanimanee, J.; Raksasuk, T.; Suddhasthira, T.; Satayavivad, J. In Vitro antifungal activities of longan (Dimocarpus longan Lour.) seed extract. Fitoterapia 2012, 83, 545–553. [Google Scholar] [CrossRef]
- Wang, J.; Zhang, X.; Gao, L.; Wang, L.; Song, F.; Zhang, L.; Wan, Y. The synergistic antifungal activity of resveratrol with azoles against Candida albicans. Lett. Appl. Microbiol. 2021, 72, 688–697. [Google Scholar] [CrossRef]
| Number and Layout of Carbon Atoms | Polyphenol Class or Family (Polyphenol subclass) | Reviewed Polyphenols |
|---|---|---|
| C6–C1 | Benzoic acids | Gallic acid |
| Methyl gallate | ||
| Protocathecuic acid | ||
| Protocatechuic acid ethyl ester | ||
| Hydroxybenzoic acid | ||
| Vanillic acid | ||
| C6–C3 | Cinnamic acids | Chlorogenic acid |
| Caffeic acid | ||
| Coumaric acid | ||
| Coumaroylquinic acid | ||
| Caffeoyl-hexose | ||
| Coumarins | ||
| C6–C2–C6 | Stilbenes | Resveratrol |
| Piceid | ||
| C6–C3–C6 | Flavonoids | |
| Flavonols | Quercetin | |
| Quercetin-3-O-rutinoside | ||
| Quercetin-3-O-glucoside | ||
| Myricetin | ||
| Kaempferol | ||
| Kaempferol diglycoside | ||
| Kaempferol-3-O-rutinoside | ||
| Morin | ||
| Flavones | Apigenin | |
| Luteolin | ||
| Amentoflavone | ||
| Norwogonin | ||
| Flavan-3-ols | Catechin | |
| Epicatechin | ||
| Epicatechin gallate | ||
| Epigallocatechin-3-gallate | ||
| 3-O-decyl-(+)-catechin | ||
| Catechin acyl derivates | ||
| Prodelphinidin B2-3′-O-gallate | ||
| Theaflavin | ||
| Flavonoids (cont.) | ||
| Flavanones | Naringenin | |
| Naringin | ||
| Eryodictiol | ||
| Eryodictiol-7-O-glucoside | ||
| Isoflavones | Daidzein | |
| Genistein | ||
| Anthocyanidins | Delphinidin glucosides | |
| Cyaniding glucosides | ||
| (C6–C1)n | Hydrolysable tannins | |
| Building blocks | Ellagic acid | |
| Pentagalloylglucopyranose | ||
| Hexahydroxydiphenic acid (HHDP) | ||
| Ellagitannins | Corilagin | |
| Chebulinic acid | ||
| Chebulagic acid | ||
| Terchebulin | ||
| Punicalin | ||
| Pedunculagin I | ||
| Punicalagin I, II and III | ||
| Punigluconin | ||
| Dehydrated tergallic-c-glucoside | ||
| HHDP glucoside isomers | ||
| Gallotannins | Galloyl glucose | |
| Gallagyl esters | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manso, T.; Lores, M.; de Miguel, T. Antimicrobial Activity of Polyphenols and Natural Polyphenolic Extracts on Clinical Isolates. Antibiotics 2022, 11, 46. https://doi.org/10.3390/antibiotics11010046
Manso T, Lores M, de Miguel T. Antimicrobial Activity of Polyphenols and Natural Polyphenolic Extracts on Clinical Isolates. Antibiotics. 2022; 11(1):46. https://doi.org/10.3390/antibiotics11010046
Chicago/Turabian StyleManso, Tamara, Marta Lores, and Trinidad de Miguel. 2022. "Antimicrobial Activity of Polyphenols and Natural Polyphenolic Extracts on Clinical Isolates" Antibiotics 11, no. 1: 46. https://doi.org/10.3390/antibiotics11010046
APA StyleManso, T., Lores, M., & de Miguel, T. (2022). Antimicrobial Activity of Polyphenols and Natural Polyphenolic Extracts on Clinical Isolates. Antibiotics, 11(1), 46. https://doi.org/10.3390/antibiotics11010046