Development of New Antimicrobial Oleanonic Acid Polyamine Conjugates
Abstract
:1. Introduction
2. Experimental Section
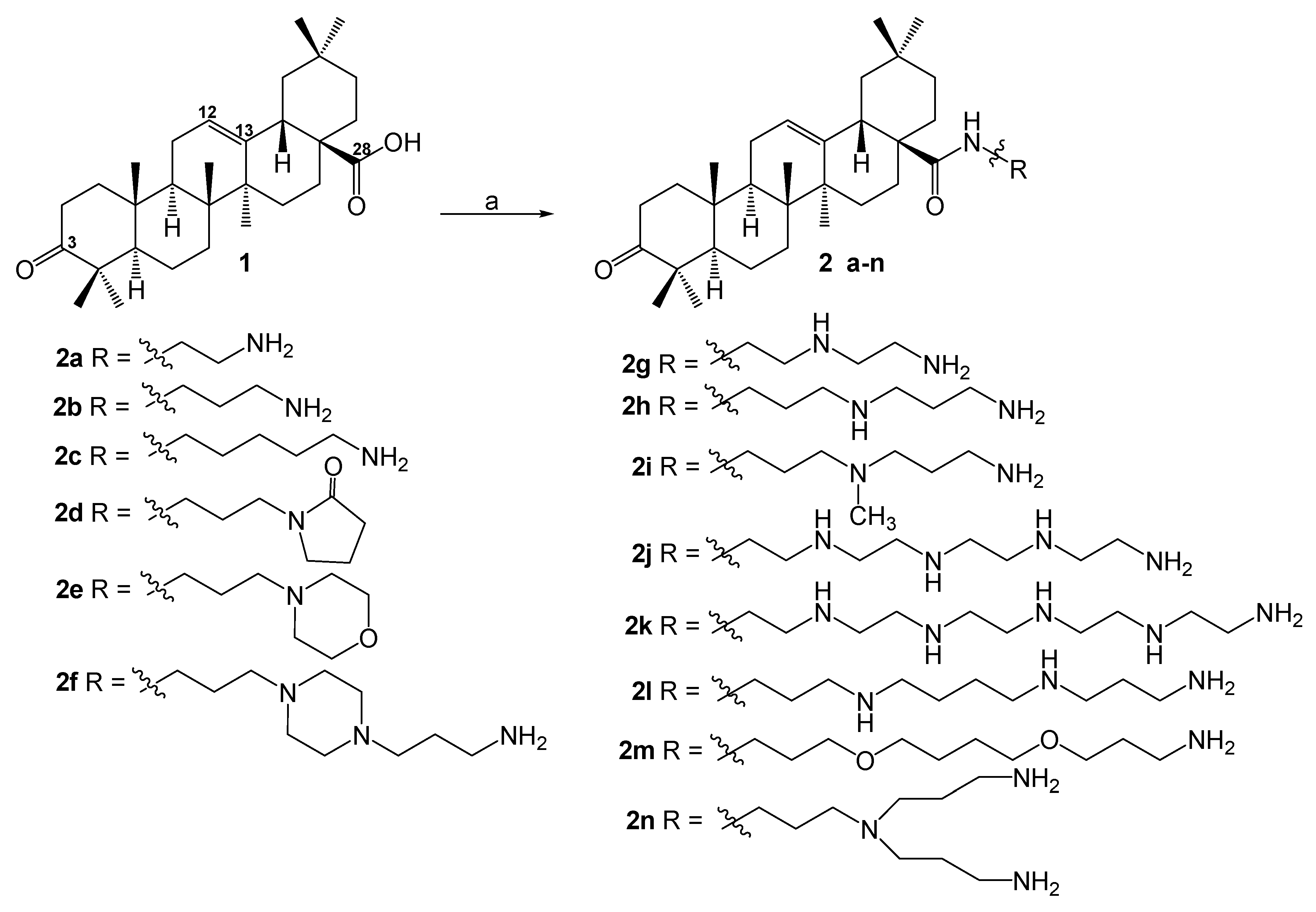
2.1. Synthesis of Amide Derivatives 2a–2n, and 7a–7c
2.2. General Procedure for the Synthesis of Compounds 3, 4
2.3. Synthesis of Compound 6
2.4. Bacterial Strains
2.5. In Vitro Antibacterial Screening
2.6. Antibiotic Susceptibility Testing
2.7. Determination of MICs of Doxycycline or Erythromycine in the Presence of Synergizing Compounds
2.8. Outer Membrane Permeation Assay
3. Results
3.1. Chemistry
3.2. Antibacterial Activities
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cassini, A.; Hogberg, L.D.; Plachouras, D.; Quattrocchi, A.; Hoxha, A.; Simonsen, G.S.; Colomb-Cotinat, M.; Kretzschmar, M.E.; Devleesschauwer, B.; Cecchini, M.; et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European economic area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019, 19, 56–66. [Google Scholar] [CrossRef] [Green Version]
- Douafer, H.; Andrieu, V.; Phanstiel, O.; Brunel, J.M. Antibiotics adjuvants: Make antibiotics great again! J. Med. Chem. 2019, 62, 8665–8681. [Google Scholar] [CrossRef]
- Liu, Y.; Li, R.; Xiao, X.; Wang, Z. Antibiotic adjuvants: An alternative approach to overcome multi-drug resistant Gram-negative bacteria. Crit. Rev. Microbiol. 2019, 45, 301–314. [Google Scholar] [CrossRef] [PubMed]
- Moloney, M.G. Natural products as a source for novel antibiotics. Trends Pharm. Sci. 2016, 37, 689–701. [Google Scholar] [CrossRef] [PubMed]
- Che, C.T.; Zhang, H. Plant natural products for human health. Int. J. Mol. Sci. 2019, 20, 830. [Google Scholar] [CrossRef] [Green Version]
- Saleem, M.; Nazir, M.; Shaiq, A.M.; Hussain, H.; Lee, Y.S.; Riaz, N.; Jabbara, A. Antimicrobial natural products: An update on future antibiotic drug candidates. Nat. Prod. Rep. 2010, 27, 238–254. [Google Scholar] [CrossRef] [PubMed]
- Osbourn, A.E.; Lanzotti, V. Plant-Derived Natural Products; Springer: Dordrecht, The Netherlands, 2009; pp. 361–384. [Google Scholar]
- Subramani, R.; Narayanasamy, M.; Feussner, K.D. Plant-derived antimicrobials to fight against multi-drug resistant human pathogens. 3 Biotech 2017, 7, 172. [Google Scholar] [CrossRef] [PubMed]
- Mushtaq, S.; Abbasi, B.H.; Uzair, B.; Abbasi, R. Natural products as reservoirs of novel therapeutic agents. EXCLI J. 2018, 17, 420–451. [Google Scholar]
- Wang, Y.Y.; Yang, Y.X.; Zhe, H.; He, Z.X.; Zhou, S.F. Bardoxolone methyl (CDDO-Me) as a therapeutic agent: An update on its pharmacokinetic and pharmacodynamic properties. Drug Des. Dev. Ther. 2014, 8, 2075–2088. [Google Scholar]
- Wozniak, L.; Skapska, S.; Marszalek, K. Ursolic acid—A pentacyclic triterpenoid with a wide spectrum of pharmacological activities. Molecules 2015, 20, 20614–20641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cappiello, F.; Loffredo, M.R.; Del Plato, C.; Cammarone, S.; Casciaro, B.; Quaglio, D.; Mangoni, M.L.; Botta, B.; Ghirga, F. The revaluation of plant-derived terpenes to fight antibiotic-resistant infections. Antibiotics 2020, 9, 325. [Google Scholar] [CrossRef]
- Catteau, L.; Zhu, L.; Van Bambeke, F.; Quetin-Leclercq, J. Natural and hemi-synthetic pentacyclic triterpenes as antimicrobials and resistance modifying agents against Staphylococcus aureus: A review. Phytochem. Rev. 2018, 17, 1129–1163. [Google Scholar] [CrossRef]
- Chung, P.Y. Novel targets of pentacyclic triterpenoids in Staphylococcus aureus: A systematic review. Phytomedicine 2020, 73, 152933. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.M.; Chen, H.T.; Wu, Z.Y.; Jhan, Y.L.; Shyu, S.L.; Chou, S.H. Antibacterial and synergistic activity of pentacyclic triterpenoids isolated from Alstonia scholaris. Molecules 2016, 21, 139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurek, A.; Nadkowska, P.; Pliszka, S.; Wolska, K.I. Modulation of antibiotic resistance in bacterial pathogen by oleanolic acid and ursolic acid. Phytomedicine 2012, 19, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Kononova, L.I.; Filatova, L.B.; Eroshenko, D.V.; Korobov, V.P. Suppression of development of vancomycin-resistant Staphylococcus epidermidis by low-molecular-weight cationic peptides of the antibiotic family. Microbiology 2017, 86, 571–578. [Google Scholar] [CrossRef]
- Brunel, J.M.; Négrel, S. Synthesis and biological activities of naturally functionalized polyamines: An overview. Curr. Med. Chem. 2021, 28, 3406–3448. [Google Scholar]
- Bildziukevich, U.; Vida, N.; Rárová, L.; Kolář, M.; Šaman, D.; Havlíček, L.; Drašar, P.; Wimmer, Z. Polyamine derivatives of betulinic acid and b-sitosterol: A comparative investigation. Steroids 2015, 100, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Spivak, A.Y.; Khalitova, R.R.; Nedopekina, D.A.; Gubaidullin, R.R. Antimicrobial properties of amine- and guanidine-functionalized derivatives of betulinic, ursolic and oleanolic acids: Synthesis and structure/activity evaluation. Steroids 2020, 154, 108530–1085512. [Google Scholar] [CrossRef] [PubMed]
- Bildziukevich, U.; Malík, M.; Özdemir, Z.; Rárová, L.; Janovská, L.; Šlouf, M.; Šaman, D.; Šarek, J.; Wimmer, Z. Spermine amides of selected triterpenoid acids: Dynamic supramolecular systems formation influences cytotoxicity of the drugs. J. Mater. Chem. B 2020, 8, 484–491. [Google Scholar] [CrossRef] [PubMed]
- Özdemir, Z.; Šaman, D.; Bertula, K.; Lahtinen, M.; Bednárová, L.; Pazderková, M.; Rárová, L.; Nonappa; Wimmer, Z. Rapid self-healing and thixotropic organogelation of amphiphilic oleanolic acid–spermine conjugates. Langmuir 2021, 37, 2693–2706. [Google Scholar] [CrossRef]
- Kazakova, O.B.; Giniyatullina, G.V.; Mustafin, A.G.; Babkov, D.A.; Sokolova, E.V.; Spasov, A.A. Evaluation of cytotoxicity and α-glucosidase inhibitory activity of amide and polyamino-derivatives of lupane triterpenoids. Molecules 2020, 25, 4833. [Google Scholar] [CrossRef]
- Kazakova, O.; Rubanik, L.; Smirnova, I.; Poleschuk, N.; Petrova, A.; Kapustsina, Y.; Baikova, I.; Tret’yakova, E.; Khusnutdinova, E. Synthesis and in vitro activity of oleanolic acid derivatives against Chlamydia trachomatis and Staphylococcus aureus. Med. Chem. Res. 2021, 30, 1408–1418. [Google Scholar] [CrossRef]
- Song, Y.L.; Zhang, P.B.; Tong, R.J.; Li, L.; Meng, Y.Q. Design and synthesis of VEGFR-2 inhibitors based on oleanolic acid moiety. J. Asian Nat. Prod. Res. 2021, 23, 176–188. [Google Scholar] [CrossRef] [PubMed]
- Kazakova, O.B.; Brunel, J.M.; Khusnutdinova, E.F.; Negrel, S.; Giniyatullina, G.V.; Lopatina, T.V.; Petrova, A.V. A-Ring-modified triterpenoids and their spermidine–aldimines with strong antibacterial activity. Molbank 2019, 2019, M1078. [Google Scholar] [CrossRef] [Green Version]
- Khusnutdinova, E.F.; Petrova, A.V.; Lobov, A.N.; Kukovinets, O.S.; Baev, D.S.; Kazakova, O.B. Synthesis of C17-[5-methyl-1,3]-oxazoles by N- propargylation of triterpenic acids and evaluation of their cytotoxic activity. Nat. Prod. Res. 2020, 35, 3850–3858. [Google Scholar] [CrossRef] [PubMed]
- Members of the Antibiogram Committee. Comité de l’Antibiogramme de la Société Française de Microbiologie. Int. J. Antimicrob. Agents 2003, 21, 364–391. [Google Scholar]
- Clinical and Laboratory Standards Institute. Development of In Vitro Susceptibility Testing Criteria and Quality Control Parameters, 5th ed.; National Committee for Clinical Laboratory Standards: Wayne, PA, USA, 2018; p. M23. [Google Scholar]
- Tolstikova, T.G.; Sorokina, I.V.; Tolstikov, G.A.; Tolstikov, A.G.; Flekhter, O.B. Biological activity and pharmacological prospects of lupane terpenoids: II. Semisynthetic lupane derivatives. Russ. J. Bioorg. Chem. 2006, 32, 261–276. [Google Scholar] [CrossRef]
- Brunel, J.M.; Salmi, C.; Letourneux, Y. Efficient peptide coupling method of conjugated carboxylic acids with methyl ester amino acids hydrochloride. Application to the synthesis of Fa-Met, an important enzymatic substrate. Tetrahedron Lett. 2005, 46, 217–220. [Google Scholar] [CrossRef]
- Salmi, C.; Letourneux, Y.; Brunel, J. Efficient diastereoselective titanium (IV) reductive amination of ketones. Lett. Org. Chem. 2006, 3, 384–389. [Google Scholar] [CrossRef]
- Salmi, C.; Letourneux, Y.; Brunel, J. Efficient synthesis of various secondary amines through a titanium (IV)isopropoxide- mediated reductive amination of ketones. Lett. Org. Chem. 2006, 3, 396–401. [Google Scholar] [CrossRef] [Green Version]
- Csuk, R.; Sczepek, R.; Siewert, B.; Nitsche, C. Cytotoxic betulin-derived hydroxypropargylamines trigger apoptosis. Bioorg. Med. Chem. 2013, 21, 425–435. [Google Scholar] [CrossRef] [PubMed]
- Blanchet, M.; Borselli, D.; Rodallec, A.; Peiretti, F.; Vidal, N.; Bolla, J.M.; Digiorgio, C.; Morrison, K.R.; Wuest, W.M.; Brunel, J.M. Claramines: A new class of broad-spectrum antimicrobial agents with bimodal activity. Chem. Med. Chem. 2018, 13, 1018–1027. [Google Scholar] [CrossRef] [PubMed]
- Lieutaud, A.; Guinoiseau, E.; Lorenzi, V.; Giuliani, M.; Lome, V.; Brunel, J.; Luciani, A.; Casanova, J.; Berti, L.; Bolla, J. Inhibitors of antibiotic effux by AcrAB-TolC in Enterobacter aerogenes. Anti-Infect. Agents 2013, 11, 168–178. [Google Scholar] [CrossRef]
- Borselli, D.; Brunel, J.M.; Gorgé, O.; Bolla, J.M. Polyamino-isoprenyl derivatives as antibiotic adjuvants and motility inhibitors for Bordetella bronchiseptica porcine pulmonary infection treatment. Front. Microbiol. 2019, 10, 1771. [Google Scholar] [CrossRef] [Green Version]
- Dong, J.; Wang, N.-N.; Yao, Z.-J.; Zhang, L.; Cheng, Y.; Ouyang, D.; Lu, A.-P.; Cao, D.-S. ADMETlab: A platform for systematic ADMET evaluation based on a comprehensively collected ADMET database. J. Cheminform. 2018, 10, 29. [Google Scholar] [CrossRef]
- Xiong, G.; Wu, Z.; Yi, J.; Fu, L.; Yang, Z.; Hsieh, C.; Yin, M.; Zeng, X.; Wu, C.; Lu, A.; et al. ADMETlab 2.0: An integrated online platform for accurate and comprehensive predictions of ADMET properties. Nucleic Acids Res. 2021, 49, 5–14. [Google Scholar] [CrossRef]
- Yang, H.; Lou, C.; Sun, L.; Li, J.; Cai, Y.; Wang, Z.; Li, W.; Liu, G.; Tang, Y. AdmetSAR 2.0: Web-service for prediction and optimization of chemical ADMET properties. Bioinformatics 2019, 35, 1067–1069. [Google Scholar] [CrossRef]
- Daina, A.; Michielin, O.; Zoete, V. SwissADME: A free web tool to evaluate pharmacokinetics, drug-likeness, and medicinal chemistry friendliness of small molecules. Sci. Rep. 2017, 7, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Lavigne, J.P.; Brunel, J.M.; Chevalier, J.; Pages, J.M. Squalamine, an original chemosensitizer to combat antibiotic-resistant Gram-negative bacteria. J. Antimicrob. Chemother. 2010, 65, 799–801. [Google Scholar] [CrossRef]
- Teuber, M. Action of polymyxin B on bacterial membranes. III: Differential inhibition of cellular functions in Salmonella typhimurium. Arch. Microbiol. 1974, 100, 131–144. [Google Scholar] [CrossRef]
- Vaara, M.; Vaara, T. Polycations sensitize enteric bacteria to antibiotics. Antimicrob. Agents Chemother. 1983, 24, 107–113. [Google Scholar] [CrossRef] [Green Version]
- Daugelavicius, R.; Bakiene, E.; Bamford, D.H. Stages of polymyxin B interaction with the Escherichia coli cell envelope. Antimicrob. Agents Chemother. 2000, 44, 2969–2978. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, L.; Dhillon, P.; Yan, H.; Farmer, S.; Hancock, R.E. Interactions of bacterial cationic peptide antibiotics with outer and cytoplasmic membranes of Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 2000, 44, 3317–3321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, S.; Walters, G.; Parg, R.; Dutcher, J.R. Nanomechanical response of bacterial cells to cationic antimicrobial peptides. Soft Matter. 2014, 10, 1806–1815. [Google Scholar] [CrossRef] [PubMed]
- Fessey, R.E.; Austin, R.P.; Barton, P.; Davis, A.M.; Wenlock, M.C. The Role of Plasma Protein Binding in Drug Discovery. In Pharmacokinetic Profiling in Drug Research; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2006; pp. 119–141. ISBN 978-3-906390-46-8. [Google Scholar]
- Kerns, E.H.; Di, L. Chapter 14—Plasma Protein Binding. In Drug-Like Properties: Concepts, Structure Design and Methods; Kerns, E.H., Di, L., Eds.; Academic Press: Cambridge, MA, USA, 2008; pp. 187–196. ISBN 978-0-12-369520-8. [Google Scholar]
- Luo, G.; Guenthner, T.; Gan, L.-S.; Humphreys, W.G. CYP3A4 Induction by Xenobiotics: Biochemistry, Experimental Methods and Impact on Drug Discovery and Development. Curr. Drug Metab. 2004, 5, 483–505. [Google Scholar] [CrossRef]
- Walker, M.A. Improvement in aqueous solubility achieved via small molecular changes. Bioorg. Med. Chem. Lett. 2017, 27, 5100–5108. [Google Scholar] [CrossRef] [PubMed]
- Broccatelli, F.; Aliagas, I.; Zheng, H. Why decreasing lipophilicity alone is often not a reliable strategy for extending IV half-life. ACS Med. Chem. Lett. 2018, 9, 522–527. [Google Scholar] [CrossRef] [PubMed]


| Compound | Minimum Inhibitory Concentration a (µM) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Gram-Negative Bacteria b | Gram-Positive Bacteria c | |||||||||
| PA ATCC 27853 | PA CIP 100720 | EC ATCC 28922 | EC CIP 54.8 | SE | EA289 | SA ATCC 25923 | SA CIP 76.25 | SF sp. | BC sp. | |
| 2a | >200 | >200 | 200 | 200 | 50 | 200 | 6.25 | 12.5 | 25 | 12.5 |
| 2b | >200 | >200 | 200 | >200 | 200 | 200 | 12.5 | 25 | 12.5 | 12.5 |
| 2c | >200 | >200 | 100 | >200 | 100 | 100 | 12.5 | 25 | 6.25 | 12.5 |
| 2d | >200 | >200 | >200 | >200 | NT | NT | >200 | >200 | 200 | NT |
| 2e | >200 | >200 | >200 | >200 | >200 | >200 | >200 | >200 | >200 | >200 |
| 2f | 50 | 200 | 50 | 200 | 25 | 25 | 12.5 | 25 | 12.5 | 12.5 |
| 2g | 50 | 100 | 25 | 50 | 25 | 50 | 12.5 | 12.5 | 12.5 | 12.5 |
| 2h | 50 | 100 | 25 | 50 | 12.5 | 25 | 12.5 | 25 | 12.5 | 12.5 |
| 2i | 25 | 100 | 25 | 50 | 12.5 | 12.5 | 6.25 | 12.5 | 6.25 | 6.25 |
| 2j | 200 | >200 | 50 | 50 | 25 | 25 | 12.5 | NT | 12.5 | 12.5 |
| 2k | >200 | >200 | >200 | >200 | NT | NT | >200 | >200 | >200 | NT |
| 2l | >200 | >200 | 25 | 50 | NT | NT | 3.125 | 6.25 | 200 | NT |
| 2m | >200 | >200 | >200 | >200 | NT | NT | 100 | NT | 50 | NT |
| 2n | 200 | >200 | 100 | 100 | NT | NT | 100 | NT | 200 | NT |
| 3 | >200 | >200 | >200 | >200 | NT | NT | >200 | NT | >200 | NT |
| 4 | >200 | >200 | >200 | >200 | >200 | >200 | >200 | >200 | >200 | >200 |
| 5 | >200 | >200 | >200 | >200 | NT | NT | >200 | >200 | >200 | NT |
| 6 | 12.5 | 25 | 6.25 | 12.5 | 12.5 | 25 | 12.5 | NT | 6.25 | NT |
| 7a | 200 | >200 | 100 | 200 | 25 | 50 | 25 | 50 | 100 | 25 |
| 7b | >200 | >200 | 100 | 100 | 50 | 100 | 50 | 100 | 50 | 25 |
| 7c | 100 | >200 | 25 | 50 | 12.5 | 25 | 12.5 | 25 | NT | 25 |
| Cpd/Strains | 2a | 2b | 2c | 2d | 2e | 2f | 2g | 2h | 2i | 2j | 2k | 2l | 2m | 2n | 3 | 4 | 5 | 6 | 7a | 7b | 7c | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MIC (µg/mL) c | P. aeruginosa ATCC 27853 a | 200 | 200 | 200 | >200 | >200 | 100 | 25 | 50 | 25 | 100 | >200 | 100 | >200 | 200 | >200 | >200 | >200 | 6.25 | 200 | 200 | 100 |
| E. coli ATCC 28922 b | 100 | 200 | 200 | >200 | >200 | 100 | 50 | 25 | 25 | 25 | >200 | 50 | >200 | 50 | >200 | >200 | >200 | 3.125 | 50 | 200 | 12.5 | |
| Category | Property | Predicted Values | Consensus Value 1 | |||
|---|---|---|---|---|---|---|
| ADMET 1ab [38] | ADMET Lab 2.0 [39] | Admet SAR [40] | SwissADME [41] | |||
| Physicochemical | Water solubility (l g mol/L) | −5.77 | −4.65 | −3.19 | −7.99 | −5.40 |
| LogP | 7 | 5.285 | 7 | 6.18 | 6.37 | |
| Absorption | Intestinal absorption (human, %) | + | + | + | Low | + |
| Human oral bioavailability | + | + | + | + | ||
| P-glycoprotein substrate | - | - | + | - | - | |
| P-glycoprotein I inhibitor | + | - | + | + | ||
| Distribution | VD (human, L/kg) | 0.836 | 0.876 | 0.856 | ||
| Plasma protein binding (%) | 81.68 | 59.69 | 100 | 90.84 | ||
| BBB permeability | + | - | + | - | - | |
| Metabolism | CYP1A2 inhibitior | - | - | - | - | - |
| CYP2C19 inhibitior | - | - | - | - | - | |
| CYP2C9 inhibitior | - | - | - | - | - | |
| CYP2D6 inhibitior | - | + | - | - | - | |
| CYP2D6 substrate | - | + | - | - | ||
| CYP3A4 inhibitior | - | + | - | - | - | |
| CYP3A4 substrate | + | + | + | + | ||
| Excretion | Total clearance (mL/min/kg) | 1.24 | 5.47 | 3.36 | ||
| T1/2 (h) | 1.93 | 0.175 | 1.05 | |||
| Toxicity | AMES toxicity | - | - | - | - | |
| hERG I inhibitor | - | - | - | |||
| hERG II inhibitor | - | - | - | |||
| Acute oral toxicity (LD50, mg/kg) | 279.17 | 368.13 | 323.65 | |||
| Hepatotoxicity | - | - | - | - | ||
| Skin sensitization | - | - | - | |||
| Carcinogenicity | - | - | - | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khusnutdinova, E.F.; Sinou, V.; Babkov, D.A.; Kazakova, O.; Brunel, J.M. Development of New Antimicrobial Oleanonic Acid Polyamine Conjugates. Antibiotics 2022, 11, 94. https://doi.org/10.3390/antibiotics11010094
Khusnutdinova EF, Sinou V, Babkov DA, Kazakova O, Brunel JM. Development of New Antimicrobial Oleanonic Acid Polyamine Conjugates. Antibiotics. 2022; 11(1):94. https://doi.org/10.3390/antibiotics11010094
Chicago/Turabian StyleKhusnutdinova, Elmira F., Véronique Sinou, Denis A. Babkov, Oxana Kazakova, and Jean Michel Brunel. 2022. "Development of New Antimicrobial Oleanonic Acid Polyamine Conjugates" Antibiotics 11, no. 1: 94. https://doi.org/10.3390/antibiotics11010094
APA StyleKhusnutdinova, E. F., Sinou, V., Babkov, D. A., Kazakova, O., & Brunel, J. M. (2022). Development of New Antimicrobial Oleanonic Acid Polyamine Conjugates. Antibiotics, 11(1), 94. https://doi.org/10.3390/antibiotics11010094









