Antibiotic Use and Resistance Knowledge Assessment of Personnel on Chicken Farms with High Levels of Antimicrobial Resistance: A Cross-Sectional Survey in Ica, Peru
Abstract
:1. Introduction
2. Results
3. Discussion
4. Material and Methods
4.1. Farmworker Cross-Sectional Survey
4.2. Study Farms
4.3. Chicken Samples
4.4. Bacterial Culture and Antibiotic Susceptibility Testing
4.5. DNA Extraction
4.6. Detection of blaCTX-M Gene
4.7. Data Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Statistics|Food and Agriculture Organization of the United Nations. Available online: http://www.fao.org/statistics/en (accessed on 11 May 2020).
- Alkhalf, A.; Alhaj, M.; Al-Homidan, I. Influence of probiotic supplementation on blood parameters and growth performance in broiler chickens. Saudi J. Biol. Sci. 2010, 17, 219–225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evans, M.C.; Wegener, H.C. Antimicrobial growth promoters and Salmonella spp., Campylobacter spp. in poultry and swine, Denmark. Emerg. Infect. Dis. 2003, 9, 489–492. [Google Scholar] [CrossRef] [PubMed]
- Woolhouse, M.; Ward, M.; Van Bunnik, B.; Farrar, J. Antimicrobial resistance in humans, livestock and the wider environment. Philos. Trans. R. Soc. B Biol. Sci. 2015, 370. [Google Scholar] [CrossRef] [PubMed]
- Hashempour-Baltork, F.; Hosseini, H.; Shojaee-Aliabadi, S.; Torbati, M.; Alizadeh, A.M.; Alizadeh, M. Drug resistance and the prevention strategies in food borne bacteria: An update review. Adv. Pharm. Bull. 2019, 9, 335–347. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.M.; Stegger, M.; Aziz, M.; Johnson, T.J.; Waits, K.; Nordstrom, L.; Gauld, L.; Weaver, B.; Rolland, D.; Statham, S.; et al. Escherichia coli ST131-H22 as a foodborne uropathogen. MBio 2018, 9, e00470-18. [Google Scholar] [CrossRef] [Green Version]
- Davis, G.S.; Waits, K.; Nordstrom, L.; Grande, H.; Weaver, B.; Papp, K.; Horwinski, J.; Koch, B.; Hungate, B.A.; Liu, C.M.; et al. Antibiotic-resistant Escherichia coli from retail poultry meat with different antibiotic use claims. BMC Microbiol. 2018, 18, 174. [Google Scholar] [CrossRef]
- Ho, B.T.; Dong, T.G.; Mekalanos, J.J. A view to a kill: The bacterial type VI secretion system. Cell Host Microbe 2014, 15, 9–21. [Google Scholar] [CrossRef] [Green Version]
- Abdi, R.D.; Mengstie, F.; Beyi, A.F.; Beyene, T.; Waktole, H.; Mammo, B.; Ayana, D.; Abunna, F. Determination of the sources and antimicrobial resistance patterns of Salmonella isolated from the poultry industry in Southern Ethiopia. BMC Infect. Dis. 2017, 17, 352. [Google Scholar] [CrossRef]
- Sun, J.; Liao, X.P.; D’Souza, A.W.; Boolchandani, M.; Li, S.H.; Cheng, K.; Luis Martínez, J.; Li, L.; Feng, Y.J.; Fang, L.X.; et al. Environmental remodeling of human gut microbiota and antibiotic resistome in livestock farms. Nat. Commun. 2020, 11, 1427. [Google Scholar] [CrossRef] [Green Version]
- Neyra, R.C.; Vegosen, L.; Davis, M.F.; Price, L.; Silbergeld, E.K. Antimicrobial-resistant bacteria: An unrecognized work-related risk in food animal production. Saf. Health Work 2012, 3, 85–91. [Google Scholar] [CrossRef] [Green Version]
- Oluwasile, B.; Agbaje, M.; Ojo, O.; Dipeolu, M. Antibiotic usage pattern in selected poultry farms in Ogun state. Sokoto J. Vet. Sci. 2014, 12, 45. [Google Scholar] [CrossRef] [Green Version]
- Boamah, V.E.; Odoi, H.; Dalsgaard, A. Practices and Factors Influencing the Use of Antibiotics in Selected Poultry Farms in Ghana. J. Antimicrob. Agents 2016, 2, 120. [Google Scholar] [CrossRef]
- Awogbemi, J.; Adeye, M.; Olugbenga, A.E. A Survey of Antimicrobial Agents Usage in Poultry Farms and Antibiotic Resistance in Escherichia Coli and Staphylococci Isolates from the Poultry in Ile-Ife, Nigeria. J. Infect. Dis. Epidemiol. 2018, 4, 4–11. [Google Scholar] [CrossRef] [Green Version]
- Ozturk, Y.; Celik, S.; Sahin, E.; Acik, M.N.; Cetinkaya, B. Assessment of farmers’ knowledge, attitudes and practices on antibiotics and antimicrobial resistance. Animals 2019, 9, 653. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Mustapha, A.I.; Adetunji, V.O.; Heikinheimo, A. Risk perceptions of antibiotic usage and resistance: A cross-sectional survey of poultry farmers in Kwara State, Nigeria. Antibiotics 2020, 9, 378. [Google Scholar] [CrossRef]
- Caudell, M.A.; Dorado-Garcia, A.; Eckford, S.; Creese, C.; Byarugaba, D.K.; Afakye, K.; Chansa-Kabali, T.; Fasina, F.O.; Kabali, E.; Kiambi, S.; et al. Towards a bottom-up understanding of antimicrobial use and resistance on the farm: A knowledge, attitudes, and practices survey across livestock systems in five African countries. PLoS ONE 2020, 15, e0220274. [Google Scholar] [CrossRef] [Green Version]
- Bâtie, C.; Kassie, D.; Randravatsilavo, D.N.R.M.; Baril, L.; Waret Szkuta, A.; Goutard, F.L. Perception of Drug Vendors and Pig and Poultry Farmers of Imerintsiatosika, in Madagascar, Toward Risks Related to Antibiotic Usage: A Q-Method Approach. Front. Vet. Sci. 2020, 7, 490. [Google Scholar] [CrossRef]
- Kalam, M.A.; Alim, M.A.; Shano, S.; Nayem, M.R.K.; Badsha, M.R.; Al Mamun, M.A.; Hoque, A.; Tanzin, A.Z.; Khan, S.A.; Islam, A.; et al. Knowledge, attitude, and practices on antimicrobial use and antimicrobial resistance among commercial poultry farmers in Bangladesh. Antibiotics 2021, 10, 784. [Google Scholar] [CrossRef]
- Prigitano, A.; Romanò, L.; Auxilia, F.; Castaldi, S.; Tortorano, A.M. Antibiotic resistance: Italian awareness survey 2016. J. Infect. Public Health 2018, 11, 30–34. [Google Scholar] [CrossRef]
- Chukwu, E.E.; Oladele, D.A.; Awoderu, O.B.; Afocha, E.E.; Lawal, R.G.; Abdus-Salam, I.; Ogunsola, F.T.; Audu, R.A. A national survey of public awareness of antimicrobial resistance in Nigeria. Antimicrob. Resist. Infect. Control 2020, 9, 72. [Google Scholar] [CrossRef]
- Effah, C.Y.; Amoah, A.N.; Liu, H.; Agboyibor, C.; Miao, L.; Wang, J.; Wu, Y. A population-base survey on knowledge, attitude and awareness of the general public on antibiotic use and resistance. Antimicrob. Resist. Infect. Control 2020, 9, 105. [Google Scholar] [CrossRef] [PubMed]
- Michaelidou, M.; Karageorgos, S.A.; Tsioutis, C. Antibiotic use and antibiotic resistance: Public awareness survey in the republic of cyprus. Antibiotics 2020, 9, 759. [Google Scholar] [CrossRef] [PubMed]
- Sastry, S.; Doi, Y. Fosfomycin: Resurgence of an old companion. J. Infect. Chemother. 2016, 22, 273–280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. Global Action Plan on Antimicrobial Resistance; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- MINSA Plan Nacional para Enfrentar la Resistencia a los Antimicrobianos 2017–2021. Available online: http://www.digemid.minsa.gob.pe/UpLoad/UpLoaded/PDF/Acceso/URM/GestionURMTrabSalud/ReunionTecnica/VIII/Dia2/Antimicrobianos/PlanNacionalATM-2017-2021.pdf (accessed on 11 May 2020).
- Usui, M.; Ozawa, S.; Onozato, H.; Kuge, R.; Obata, Y.; Uemae, T.; Ngoc, T.; Heriyanto, A.; Chalemchaikit, T.; Makita, K.; et al. Antimicrobial Susceptibility of Indicator Bacteria Isolated from Chickens in Southeast Asian Countries (Vietnam, Indonesia and Thailand). J. Vet. Med. Sci. 2014, 76, 685–692. [Google Scholar] [CrossRef] [Green Version]
- Van Boeckel, T.P.; Pires, J.; Silvester, R.; Zhao, C.; Song, J.; Criscuolo, N.G.; Gilbert, M.; Bonhoeffer, S.; Laxminarayan, R. Global trends in antimicrobial resistance in animals in low- and middle-income countries. Science 2019, 365. [Google Scholar] [CrossRef] [Green Version]
- Murray, M.; Salvatierra, G.; Dávila-Barclay, A.; Ayzanoa, B.; Castillo-Vilcahuaman, C.; Huang, M.; Pajuelo, M.J.; Lescano, A.G.; Cabrera, L.; Calderón, M.; et al. Market Chickens as a Source of Antibiotic-Resistant Escherichia coli in a Peri-Urban Community in Lima, Peru. Front. Microbiol. 2021, 12, 635871. [Google Scholar] [CrossRef]
- Nadimpalli, M.; Vuthy, Y.; de Lauzanne, A.; Fabre, L.; Criscuolo, A.; Gouali, M.; Huynh, B.T.; Naas, T.; Phe, T.; Borand, L.; et al. Meat and fish as sources of extended-spectrum β-Lactamase– producing Escherichia coli, Cambodia. Emerg. Infect. Dis. 2019, 25, 126–131. [Google Scholar] [CrossRef] [Green Version]
- Day, M.J.; Hopkins, K.L.; Wareham, D.W.; Toleman, M.A.; Elviss, N.; Randall, L.; Teale, C.; Cleary, P.; Wiuff, C.; Doumith, M.; et al. Extended-spectrum β-lactamase-producing Escherichia coli in human-derived and foodchain-derived samples from England, Wales, and Scotland: An epidemiological surveillance and typing study. Lancet Infect. Dis. 2019, 19, 1325–1335. [Google Scholar] [CrossRef] [Green Version]
- Doi, Y.; Iovleva, A.; Bonomo, R.A. The ecology of extended-spectrum b-lactamases (ESBLs) in the developed world. J. Travel Med. 2017, 24, S45–S50. [Google Scholar] [CrossRef]
- WHO. Antibiotic Resistance: Multi-Country Public Awareness Survey; WHO Press: Geneve, Switzerland, 2015; pp. 1–51. [Google Scholar]
- Sørensen, K.; Pelikan, J.M.; Röthlin, F.; Ganahl, K.; Slonska, Z.; Doyle, G.; Fullam, J.; Kondilis, B.; Agrafiotis, D.; Uiters, E.; et al. Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. [Google Scholar] [CrossRef] [Green Version]
- Sadiq, M.B.; Syed-Hussain, S.S.; Ramanoon, S.Z.; Saharee, A.A.; Ahmad, N.I.; Noraziah, M.Z.; Khalid, S.F.; Naseeha, D.S.; Syahirah, A.A.; Mansor, R. Knowledge, attitude and perception regarding antimicrobial resistance and usage among ruminant farmers in Selangor, Malaysia. Prev. Vet. Med. 2018, 156, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Singer, R.S.; Patterson, S.K.; Meier, A.E.; Gibson, J.K.; Lee, H.L.; Maddox, C.W. Relationship between phenotypic and genotypic florfenicol resistance in Escherichia coli. Antimicrob. Agents Chemother. 2004, 48, 4047–4049. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salm, F.; Ernsting, C.; Kuhlmey, A.; Kanzler, M.; Gastmeier, P.; Gellert, P. Antibiotic use, knowledge and health literacy among the general population in Berlin, Germany and its surrounding rural areas. PLoS ONE 2018, 13, e0193336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marshall, B.M.; Levy, S.B. Food Animals and Antimicrobials: Impacts on Human Health. Clin. Microbiol. Rev. 2011, 24, 718–733. [Google Scholar] [CrossRef] [Green Version]
- Gupta, K.; Bhadelia, N. Management of urinary tract infections from multidrug-resistant organisms. Infect. Dis. Clin. N. Am. 2014, 28, 49–59. [Google Scholar] [CrossRef]
- Maciorowski, K.G.; Herrera, P.; Jones, F.T.; Pillai, S.D.; Ricke, S.C. Effects on poultry and livestock of feed contamination with bacteria and fungi. Anim. Feed Sci. Technol. 2007, 133, 109–136. [Google Scholar] [CrossRef]
- Skóra, J.; Matusiak, K.; Wojewódzki, P.; Nowak, A.; Sulyok, M.; Ligocka, A.; Okrasa, M.; Hermann, J.; Gutarowska, B. Evaluation of microbiological and chemical contaminants in poultry farms. Int. J. Environ. Res. Public Health 2016, 13, 192. [Google Scholar] [CrossRef]
- Pearson, A.D.; Greenwood, M.; Healing, T.D.; Rollins, D.; Shahamat, M.; Donaldson, J.; Colwell, R.R. Colonization of broiler chickens by waterborne Campylobacter jejuni. Appl. Environ. Microbiol. 1993, 59, 987–996. [Google Scholar] [CrossRef] [Green Version]
- Dhanarani, T.S.; Shankar, C.; Park, J.; Dexilin, M.; Kumar, R.R.; Thamaraiselvi, K. Study on acquisition of bacterial antibiotic resistance determinants in poultry litter. Poult. Sci. 2009, 88, 1381–1387. [Google Scholar] [CrossRef]
- D’Andrea, M.M.; Arena, F.; Pallecchi, L.; Rossolini, G.M. CTX-M-type β-lactamases: A successful story of antibiotic resistance. Int. J. Med. Microbiol. 2013, 303, 305–317. [Google Scholar] [CrossRef]
- Vermeulen, B.; De Backer, P.; Remon, J.P. Drug administration to poultry. Adv. Drug Deliv. Rev. 2002, 54, 795–803. [Google Scholar] [CrossRef]
- Diario Oficial del Bicentenario. Resolución Directoral No 0091-2019-MINAGRI-SENASA-DIAIA; Diario El Peruano: Lima, Peru, 2019. [Google Scholar]
- Cardinal, M.K.; Kipper, M.; Andretta, I.; Machado Leal Ribeiro, A. Withdrawal of antibiotic growth promoters from broiler diets: Performance indexes and economic impact. Poult. Sci. 2019, 98, 6659–6667. [Google Scholar] [CrossRef] [PubMed]
- Nadimpalli, M.; Delarocque-Astagneau, E.; Love, D.C.; Price, L.B.; Huynh, B.-T.; Collard, J.-M.; Lay, K.S.; Borand, L.; Ndir, A.; Walsh, T.R.; et al. Combating Global Antibiotic Resistance: Emerging One Health Concerns in Lower-and Middle-Income Countries. Clin. Infect. Dis. 2018, 66, 963–969. [Google Scholar] [CrossRef] [PubMed]
- Al Masud, A.; Rousham, E.K.; Islam, M.A.; Alam, M.U.; Rahman, M.; Al Mamun, A.; Sarker, S.; Asaduzzaman, M.; Unicomb, L. Drivers of Antibiotic Use in Poultry Production in Bangladesh: Dependencies and Dynamics of a Patron-Client Relationship. Front. Vet. Sci. 2020, 7, 78. [Google Scholar] [CrossRef]
- Redding, L.E.; Brooks, C.; Georgakakos, C.B.; Habing, G.; Rosenkrantz, L.; Dahlstrom, M.; Plummer, P.J. Addressing Individual Values to Impact Prudent Antimicrobial Prescribing in Animal Agriculture. Front. Vet. Sci. 2020, 7, 297. [Google Scholar] [CrossRef]
- Elmi, S.A.; Simons, D.; Elton, L.; Haider, N.; Hamid, M.M.A.; Shuaib, Y.A.; Khan, M.A.; Othman, I.; Kock, R.; Osman, A.Y. Identification of risk factors associated with resistant escherichia coli isolates from poultry farms in the east coast of peninsular malaysia: A cross sectional study. Antibiotics 2021, 10, 117. [Google Scholar] [CrossRef]
- Wongsuvan, G.; Wuthiekanun, V.; Hinjoy, S.; Day, N.P.J.; Limmathurotsakul, D. Antibiotic use in poultry: A survey of eight farms in Thailand. Bull. World Health Organ. 2018, 96, 94–100. [Google Scholar] [CrossRef]
- Jiang, W.; Paudel, S.K.; Amarasekara, N.R.; Zhang, Y.; Etienne, X.; Jones, L.; Li, K.W.; Hansen, F.; Jaczynski, J.; Shen, C. Survey of small local produce growers’ perception of antibiotic resistance issues at farmers markets. Food Control 2021, 125, 107997. [Google Scholar] [CrossRef]
- Chereau, F.; Opatowski, L.; Tourdjman, M.; Vong, S. Risk assessment for antibiotic resistance in South East Asia. BMJ 2017, 358, 2–8. [Google Scholar] [CrossRef] [Green Version]
- Braykov, N.P.; Eisenberg, J.N.S.; Grossman, M.; Zhang, L.; Vasco, K.; Cevallos, W.; Muñoz, D.; Acevedo, A.; Moser, K.A.; Marrs, C.F.; et al. Antibiotic Resistance in Animal and Environmental Samples Associated with Small-Scale Poultry Farming in Northwestern Ecuador. mSphere 2016, 1, e00021-15. [Google Scholar] [CrossRef] [Green Version]
- Moser, A.I.; Kuenzli, E.; Campos-Madueno, E.I.; Büdel, T.; Rattanavong, S.; Vongsouvath, M.; Hatz, C.; Endimiani, A. Antimicrobial-Resistant Escherichia coli Strains and Their Plasmids in People, Poultry, and Chicken Meat in Laos. Front. Microbiol. 2021, 12, 2106. [Google Scholar] [CrossRef] [PubMed]
- FAO Animal Production and Health Division. Poultry Sector Country Review: India; FAO Animal Production and Health Division: Rome, Italy, 2008. [Google Scholar]
- CLSI. M100: Performance Standards for Antimicrobial Susceptibility Testing, 28th ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2018. [Google Scholar]
- European Committee on Antimicrobial Susceptibility Testing. Breakpoint Tables for Interpretation of MICs and Zone Diameters Version 7.1; European Committee on Antimicrobial Susceptibility Testing: Växjö, Sweden, 2017. [Google Scholar]
- Dashti, A.A.; Jadaon, M.M.; Abdulsamad, A.M.; Dashti, H.M. Heat Treatment of Bacteria: A Simple Method of DNA Extraction for Molecular Techniques. Kuwait Med. J. 2009, 41, 117–122. [Google Scholar]
- Edelstein, M.; Pimkin, M.; Palagin, I.; Edelstein, I.; Stratchounski, L. Prevalence and Molecular Epidemiology of CTX-M Extended-Spectrum β-Lactamase-Producing Escherichia coli and Klebsiella pneumoniae in Russian Hospitals. Antimicrob. Agents Chemother. 2003, 47, 3724–3732. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [Green Version]


| Results | n (%) | |
|---|---|---|
| Q1. When did you last take antibiotics? | ||
| In the last month | 33 (61.0) | |
| In the last 6 months | 19 (35.2) | |
| In the last year | 1 (1.9) | |
| More than a year ago | 1 (1.9) | |
| Q2. On that occasion, did you get the antibiotics (or a prescription for them) from a doctor or nurse? | ||
| Yes | 23 (42.6) | |
| Q3. On that occasion, where did you get the antibiotics? | ||
| Medical store or pharmacy | 36 (66.7) | |
| I had them saved up from a previous time | 18 (33.3) | |
| Q4. When do you think you should stop taking antibiotics once you’ve begun treatment? | ||
| When you feel better | 11 (20.4) | |
| When you’ve taken all of the antibiotics as directed | 42 (77.8) | |
| Don’t know | 1 (1.9) | |
| Q5. “It’s okay to use antibiotics that were given to a friend or family member, as long as they were used to treat the same illness” (TRUE) | ||
| Yes | 37 (68.5) | |
| Q6. “It’s okay to buy the same antibiotics, or request these from a doctor, if you’re sick and they helped you get better when you had the same symptoms before” (TRUE) | ||
| Yes | 25 (46.3) | |
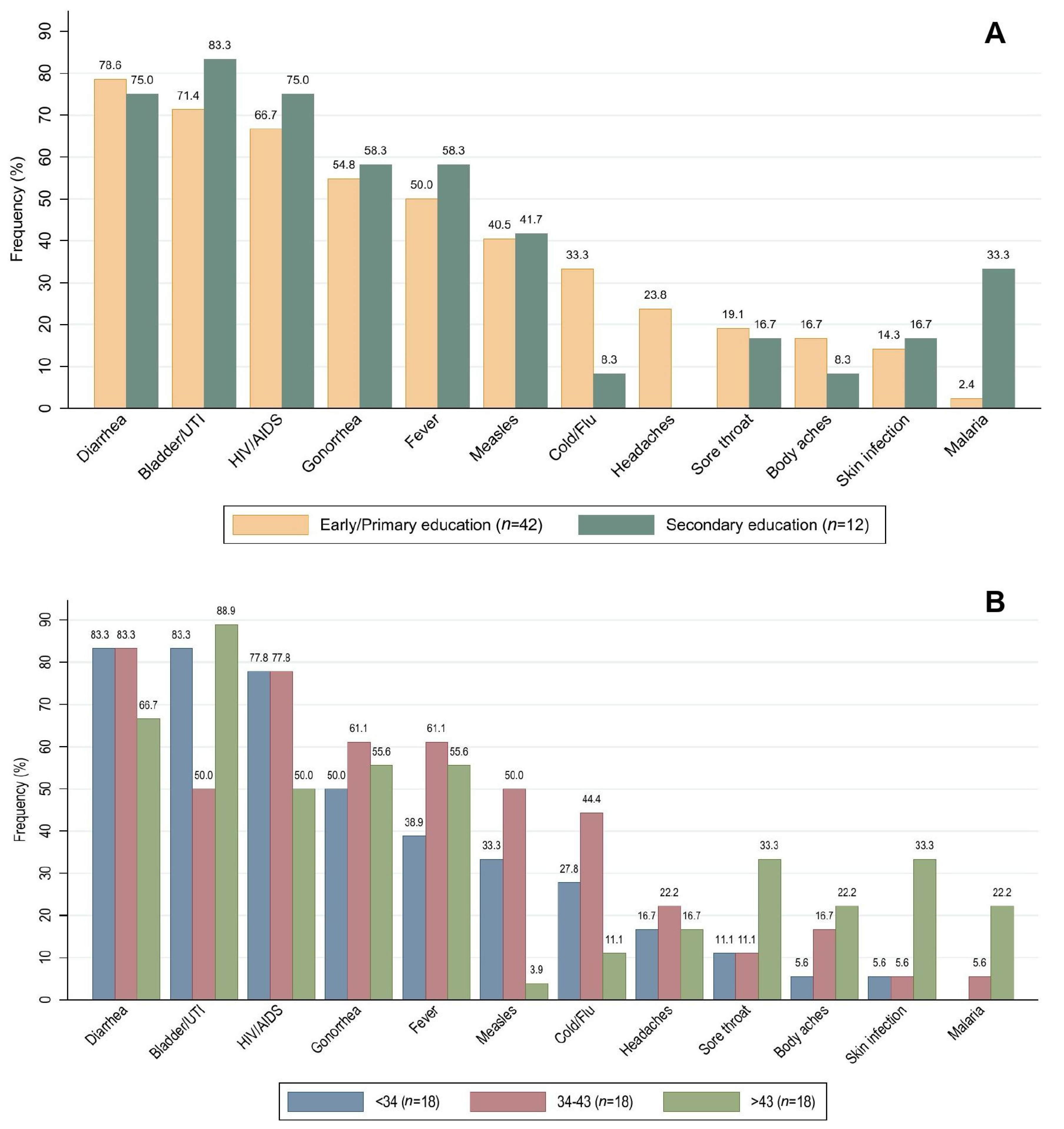
| Q7. Do you think these conditions can be treated with antibiotics? | ||
| Diarrhoea | 42 (77.8) | |
| Bladder infection or urinary tract infection | 40 (74.1) | |
| HIV/AIDS | 37 (68.5) | |
| Gonorrhoea | 30 (55.6) | |
| Fever | 28 (51.9) | |
| Measles | 22 (40.7) | |
| Cold and flu | 15 (27.8) | |
| Sore throat | 10 (18.5) | |
| Headaches | 10 (18.5) | |
| Skin or wound infection | 8 (14.8) | |
| Body aches | 8 (14.8) | |
| Malaria | 5 (9.3) | |
| Q8. Have you ever heard of any of the following terms? | ||
| Antibiotic resistance | 45 (83.3) | |
| Superbugs | 11 (20.4) | |
| Antimicrobial resistance | 37 (68.5) | |
| AMR | 5 (9.3) | |
| Drug resistance | 38 (70.4) | |
| Antibiotic-resistant bacteria | 18 (33.3) | |
| Q9. Do you agree that the following actions would help address the problem of antibiotic resistance? (Yes) | ||
| People should use antibiotics only when they are prescribed by a doctor or nurse | 48 (88.9) | |
| Farmers should give fewer antibiotics to food-producing animals | 23 (42.6) | |
| People should not keep antibiotics and use them later for other illnesses | 33 (61.1) | |
| Parents should make sure all of their children’s vaccinations are up-to-date | 21 (38.9) | |
| People should wash their hands regularly | 13 (24.1) | |
| Doctors should only prescribe antibiotics when they are needed | 50 (92.6) | |
| Governments should reward the development of new antibiotics | 18 (33.3) | |
| Pharmaceutical companies should develop new antibiotics | 22 (40.7) | |
| Characteristics | Total | Antibiotics Consumed during the Previous Month | p-Value * | |
|---|---|---|---|---|
| Yes (n = 33) | No (n = 21) | |||
| Age (tertiles) | ||||
| <34 | 18 (33.3) | 8 (24.2) | 10 (47.6) | 0.296 |
| 34–43 | 18 (33.3) | 13 (39.4) | 5 (23.8) | |
| >43 | 18 (33.3) | 12 (36.4) | 6 (28.6) | |
| Education level | ||||
| Early/Primary | 42 (77.8) | 26 (78.8) | 16 (76.2) | 1.000 |
| Secondary | 12 (22.2) | 7 (21.2) | 5 (23.8) | |
| Results | Total (n = 107) | Farm A (n = 32) | Farm B (n = 37) | Farm C (n = 38) | p-Value * |
|---|---|---|---|---|---|
| MDR | |||||
| Yes | 96 (89.7) | 28 (87.5) | 36 (97.3) | 32 (94.2) | 0.147 |
| ESBL | |||||
| Yes | 77 (71.9) | 20 (62.5) | 33 (89.2) | 24 (63.2) | 0.012 |
| Amphenicols | |||||
| Chloramphenicol | 72 (67.3) | 22 (68.8) | 21 (56.8) | 29 (76.3) | 0.200 |
| Tetracyclines | |||||
| Tetracycline | 86 (80.4) | 27 (84.4) | 23 (62.2) | 36 (94.7) | 0.002 |
| Sulfonamides | |||||
| Trimethoprim/sulfamethoxazole | 102 (95.3) | 31 (96.9) | 37 (100.0) | 34 (89.5) | 0.078 |
| Aminoglycosides | |||||
| Gentamicin | 64 (59.8) | 23 (71.9) | 21 (56.8) | 20 (52.6) | 0.246 |
| Macrolides | |||||
| Azithromycin | 2 (1.9) | 0 (0.0) | 1 (2.7) | 1 (2.6) | 1.000 |
| Penicillins | |||||
| Amoxicillin | 93 (86.9) | 29 (90.6) | 35 (94.6) | 29 (76.3) | 0.067 |
| Cephalosporins | |||||
| Cefalotin | 84 (78.5) | 21 (65.6) | 35 (94.6) | 28 (73.7) | 0.007 |
| Cefepime | 12 (11.2) | 4 (12.5) | 5 (13.5) | 3 (7.9) | 0.742 |
| Carbapenems | |||||
| Meropenem | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | N.A. |
| Quinolones | |||||
| Nalidixic Acid | 91 (85.1) | 26 (81.3) | 36 (97.3) | 29 (76.3) | 0.021 |
| Ciprofloxacin | 72 (67.3) | 15 (46.9) | 32 (86.5) | 25 (65.8) | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dávalos-Almeyda, M.; Guerrero, A.; Medina, G.; Dávila-Barclay, A.; Salvatierra, G.; Calderón, M.; Gilman, R.H.; Tsukayama, P. Antibiotic Use and Resistance Knowledge Assessment of Personnel on Chicken Farms with High Levels of Antimicrobial Resistance: A Cross-Sectional Survey in Ica, Peru. Antibiotics 2022, 11, 190. https://doi.org/10.3390/antibiotics11020190
Dávalos-Almeyda M, Guerrero A, Medina G, Dávila-Barclay A, Salvatierra G, Calderón M, Gilman RH, Tsukayama P. Antibiotic Use and Resistance Knowledge Assessment of Personnel on Chicken Farms with High Levels of Antimicrobial Resistance: A Cross-Sectional Survey in Ica, Peru. Antibiotics. 2022; 11(2):190. https://doi.org/10.3390/antibiotics11020190
Chicago/Turabian StyleDávalos-Almeyda, María, Agustín Guerrero, Germán Medina, Alejandra Dávila-Barclay, Guillermo Salvatierra, Maritza Calderón, Robert H. Gilman, and Pablo Tsukayama. 2022. "Antibiotic Use and Resistance Knowledge Assessment of Personnel on Chicken Farms with High Levels of Antimicrobial Resistance: A Cross-Sectional Survey in Ica, Peru" Antibiotics 11, no. 2: 190. https://doi.org/10.3390/antibiotics11020190







