Isavuconazole in the Treatment of Aspergillus fumigatus Fracture-Related Infection: Case Report and Literature Review
Abstract
:1. Introduction
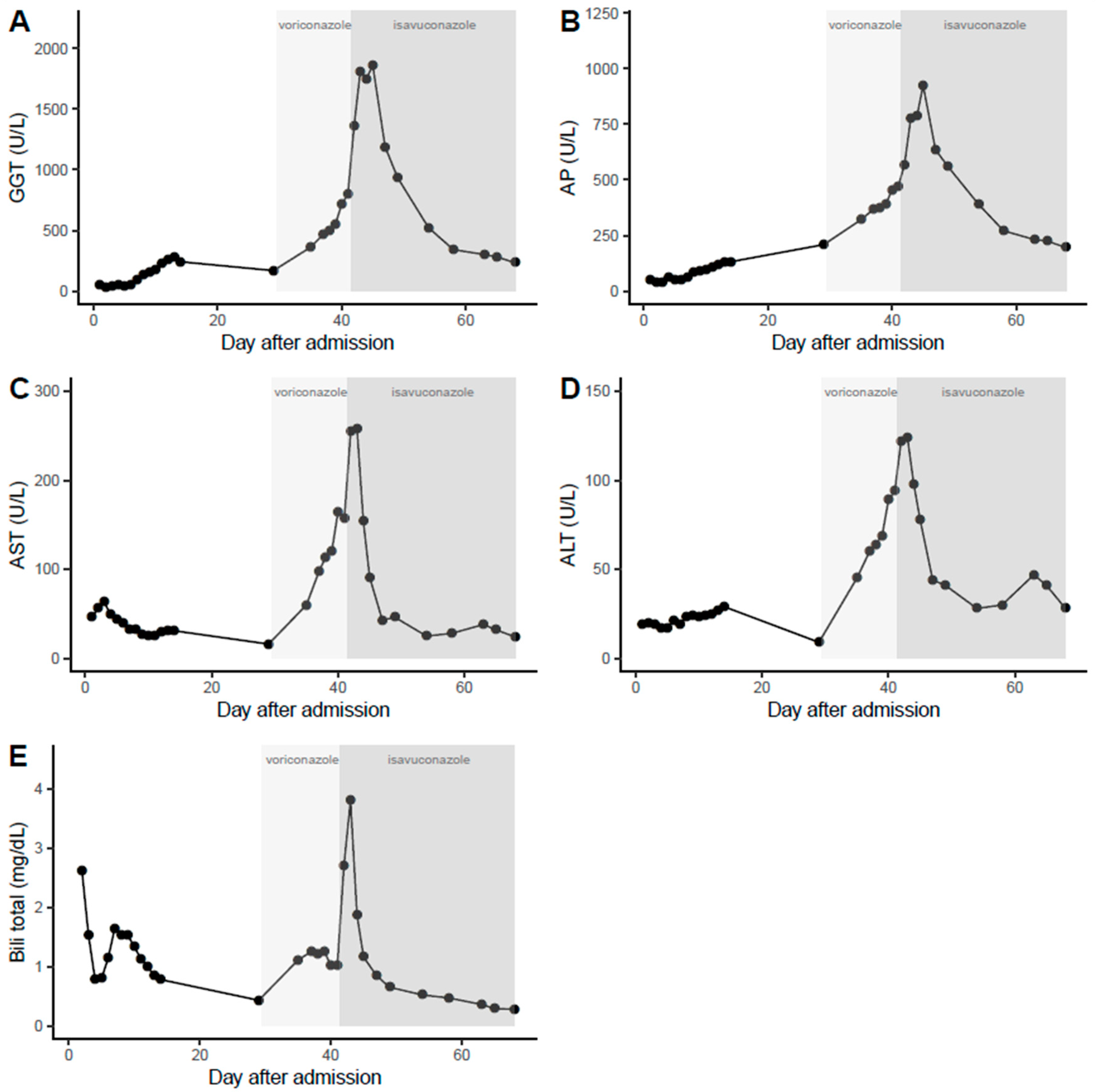
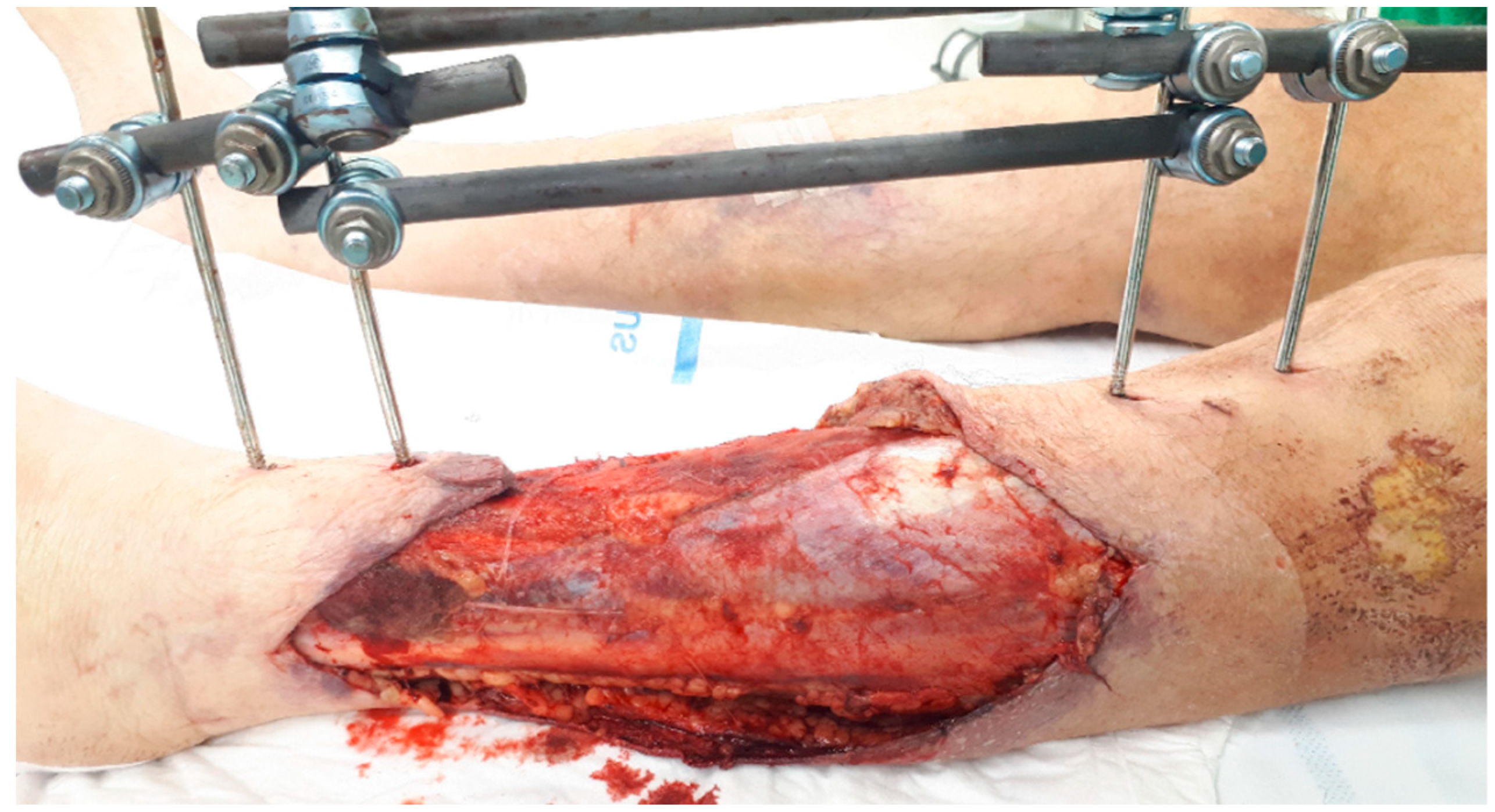
2. Case Report
3. Methods Literature Review
3.1. Antifungal Treatment of Aspergillus Osteomyelitis
3.2. Antifungal Bone Penetration
4. Results Literature Review
4.1. Antifungal Treatment of Aspergillus Osteomyelitis
4.2. Antifungal Bone Penetration
4.2.1. Triazoles
Itraconazole
Voriconazole
Posaconazole
Isavuconazole
4.2.2. Echinocandins
4.2.3. Polyenes
4.2.4. 5-Fluorocytosine
5. Discussion
5.1. Antifungal Treatment of Aspergillus Osteomyelitis
5.2. Antifungal Bone Penetration
5.3. Expert Opinion
6. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix B
Appendix C
| Reference (Year) | Age, Sex | Infection Location | Infection Mechanism | Host Factors | A. Species | Surgical Treatment | AFT | Posology | Rationale Switch | Duration | TDM | Outcome | FU Clinical Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fracture-related infection | |||||||||||||
| Rodríguez-Hernández (2001) [3] | 30,F | Parietal bone (R) | DI: fracture after cranial trauma | None | A. fumigatus | SD | AmB IV | 1 mg/kg q24 h | NA | 27 wk | Y | IC | 2 yr after FRI diagnosis |
| → Itr PO | 200 mg q12 h | NS | |||||||||||
| Mouas (2005) [4] | 46,M | Metacarpal bone (R) | DI: fracture after trauma | None | A. terreus | SD | Vor PO | 150–200 mg q12 h | NA | 93 d | N | IF | 9 yr after trauma |
| 43,M a | Femur, fibula (L) | DI: fracture after trauma | None | A. fumigatus | SD, external fixation, knee arthrodesis | Itr | 400 mg q24 h | NA | ±35 wk | Y | IF | 14 mo after trauma | |
| → L-AmB IV | 3 mg/kg q24 h | TF | |||||||||||
| → Vor PO | 200 mg q12 h (d1: LD) | TF | |||||||||||
| Garazzino (2008) [5] | 69,M | Tibia (L) | DI: chronic infection after trauma (30 yr before) | DM | A. flavus | SD | Vor IV,PO | 4 mg/kg q12 h (d1: LD) | NA | 7 mo | N | IF | ≥4 mo after AFT initiation |
| Dabkana (2015) [6] | 26,F | Tibia, patella, femur (R) | DI: femur fracture after trauma | None | NS | Sequestrectomy, amputation, hip disarticulation | Tioconazole | NS | NA | NS | N | IC | NS |
| Takagi (2019) [7] | 74,M | T11-T12 vertebrae | DI: fractures of T12, L1 vertebrae, rib 10–12 (L) after trauma | None | A. terreus | Partial laminectomy, spinal fusion | Vor IV,PO | 600 mg/d | NA | 5 mo | N | IC | 2 yr after surgery |
| Sternal/rib osteomyelitis | |||||||||||||
| Allen (2002) [44] | 67,F | Sternum | C/H: IPA (8 yr before) | None | A. fumigatus | None | L-AmB IV | 1 mg/kg q24 h | NA | 10 wk | N | D ** | 8 mo after AFT cessation |
| → Itr PO | 200 mg q12 h | TA | |||||||||||
| Vandecasteele (2002) [23] | 74,F b | Sternum | DI: CABG | None | A. flavus | SD | Itr PO | 200 mg q12 h | NA | 128 d | Y | IC | ≥128 d after AFT initiation |
| 76,M c | Sternum | DI: CABG | None | A. flavus | Curettage | Itr PO | 200 mg q12 h | NA | 87 d | Y | IC | ≥87 d after AFT initiation | |
| 69,F d | Sternum | DI: CABG | IS | A. flavus | Multiple SDs, marsupiali-zation of abscess | Itr PO | 200 mg q12 h | NA | 100 d | Y | IC | ≥100 d after AFT initiation | |
| 75,F e | Sternum | DI: CABG | None | A. flavus | Multiple curettages | Itr PO | 200 mg q12 h | NA | 122 d | Y | IC | ≥122 d after AFT initiation | |
| 75,F f | Sternum | DI: CABG | IS | A. flavus | Curettage | Itr PO | 200 mg q12 h | NA | 11 d | Y | D * | 55 d after OM diagnosis | |
| Elahi (2005) [45] | 62,M | Sternum, rib 6–10 (R) | DI: repeated CABG | DM | A. fumigatus | Multiple SDs, partial resection of sternum & ribs 6–8 | Itr PO | 200 mg/d | NA | 6 mo | N | IC | 12 mo after surgery |
| Mouas (2005) [4] | 31,Mg | Rib (R) (NS) | C/H: IPA | HIV | A. fumigatus | None | AmB IV | 1 mg/kg q24–96 h | NA | ±17 mo | Y | D ** | ±21 mo after OM diagnosis |
| → AmB IV | 1 mg/kg q72–96 h | NS | |||||||||||
| +5-FC | NS | ||||||||||||
| → Itr | 400 mg q24 h | TF | |||||||||||
| → AmB IV | NS | TF | |||||||||||
| → Vor PO | 100–200 mg q12 h | TF | |||||||||||
| 55,M | Sternum | NS | SOT | A. fumigatus | NS | AmB IV | NS | NA | ≥17 d | N | IC | ≥17 d after Vor initiation | |
| +Itr | NS | ||||||||||||
| → Vor PO | NS | NS | |||||||||||
| Soto-Hurtado (2005) [46] | 65,M | Lower ribs (L) (NS) | C/H: pulmonary aspergillomas | None | U | Thoracotomy | AmB IV | NS | NA | NS | N | D * | Few days after AFT initiation |
| Natesan (2007) [47] | 29,F | Sternum | DI: pericardiectomy | SOT, DM | A. terreus | SD | Itr PO | 200 mg q24 h | NA | ±2–4 mo | N | IF | ±6 mo after pericard-iectomy |
| → L-AmB IV | 150 mg q24 h | NS | |||||||||||
| → Caf IV | 50 mg q24 h (d1: LD) | R | |||||||||||
| → Vor | 200 mg q24 h | NS | |||||||||||
| Verghese (2008) [48] | 70,M | Rib 7 (L) | DI: CABG | DM | A. flavus | Partial rib excision, abscess drainage | Vor | 200–400 mg q12 h | NA | 5 mo | N | IC | NS |
| Horn (2009) [49] | 62,F | Rib (NS) | NS | None | A. fumigatus | Surgery type NS | Vor | NS | NA | 16 d | N | IF | 71 d after OM diagnosis |
| 63,M | Sternum | DI: aortic valve replacement | None | A. fumigatus | Surgery type NS | Flu | NS | NA | 10 d | N | D | 33 d after OM diagnosis | |
| 48,F | Sternum | DI: aortic valve replacement | None | A. fumigatus | Surgery type NS | Vor | NS | NA | 26 d | N | IF | 26 d after OM diagnosis | |
| Puri (2011) [50] | 52,M | Rib (NS) (R) | C/H: suspicion of IPA | None | U | Partial resection of sternum, 4 ribs & lung lobe, chest wall reconstruction | AmB IV | NS | NA | NS | N | NS | NS |
| Asare (2013) [24] | 69,M | Sternum | DI: CABG, aortic valve replacement | None | A. fumigatus | Sternectomy, multiple SDs | Vor IV,PO | 300 mg q12 h (d1: LD) | NA | NS | Y | IC | NS |
| Landaburu (2019) [51] | 61,F | Rib 10,12 (R) | DI: pulmonary segmentectomy | IS | A. flavus | None | Vor IV,PO | 200 mg q12 h | NA | 8 mo | N | IC | 8 mo after AFT initiation |
| Assaf (2020) [25] | 65,M | Sternum | DI: heart Tx, re-opening of sternotomy | SOT | A. fumigatus | Wire removal, abscess drainage | Vor IV,PO | 4 mg q12 h (d1: LD) | NA | 12 mo | Y | IF | ≥10 mo after Isa initiation |
| → L-AmB IV | 3 mg/kg q24 h | TA | |||||||||||
| → Isa | 200 mg q24 h (d1,2: LD) | TA | |||||||||||
| Doub (2020) [26] | 37,M | Rib 10 (R) | U | None | A. fumigatus | Multiple SDs, removal of rib graft, decortication, chest wall reconstruction | Vor IV,PO | 4 mg/kg (d1: LD) | NA | 9 mo | Y | IF | 9 mo after AFT cessation |
| Pos PO | 300–400 mg q24 h | TA | |||||||||||
| Routray (2020) [27] | 65,F | Sternum | DI: CABG | DM | A. fumigatus | Partial sternectomy, abscess drainage, multiple SDs | Mcf IV | 100 mg q24 h | NA | ±7 mo | Y | IC | ≥2 wk after AFT reinitiation |
| +Vor IV,PO | 200 mg q12 h | ||||||||||||
| → Vor PO | 200–400 mg q12 h | NS | |||||||||||
| → Isa PO | 372 mg q24 h (d1,2: LD) | AD, TA | |||||||||||
| → L-AmB IV | 400 mg q24 h | AD, TA | ±9.5 mo (re-initiation 6 mo after Isa discont-inuation) | ||||||||||
| +Vor IV | 400 mg q12 h | ||||||||||||
| +Mcf IV | 100 mg q24 h | ||||||||||||
| → Vor IV,PO | 200–400 mg q12 h | TA | |||||||||||
| +Mcf IV | 100 mg q24 h | ||||||||||||
| → Vor PO | 200 mg q12 h | NS | |||||||||||
| Osteomyelitis of the extremities | |||||||||||||
| Kaneko (2002) [52] | 57,F | Femur (R) | U | SOT | A. fumigatus | None | AmB IV | 0.7 mg/kg q24 h | NA | 13 mo | N | IC | ±1 yr after OM diagnosis |
| +5-FC | 120 mg/kg q24 h | ||||||||||||
| → Itr | 200 mg/d | NS | |||||||||||
| Lodge (2004) [28] | 64,M | Calcaneal bone (R) | C/H: IPA | SOT | A. fumigatus | SD, partial calcanectomy | Itr PO | 200 mg q12 h | NA | ±13 mo | Y | IF | 12 mo after AFT cessation |
| +ABLC IV | 5 mg/kg q24 h | ||||||||||||
| +AmB INH | 25 mg/wk | ||||||||||||
| → ABLC IV | 5 mg/kg q24 h | ST | |||||||||||
| +AmB INH | 25 mg/wk | ||||||||||||
| → Pos PO | 400 mg q12 h | TA, TF | |||||||||||
| NB: prior AFT (AmB INH ± Itr) for IPA | |||||||||||||
| Brodsky (2005) [53] | 40,M | 5th distal phalanx (R) | DI: paronychia after toenail clipping | HM | A. versicolor | SD, partial resection of phalanx | ABLC IV | NS | NA | ±6 wk | N | D ** | 2 mo after AFT cessation |
| → Itr PO | NS | NS | |||||||||||
| NB: prior empiric AFT (Flu + AmB IV) | |||||||||||||
| Denes (2007) [19] | 83,F | Femur, tibia (L) | DI: knee arthritis after CS infiltration | None | A. fumigatus | SD, amputation | Vor IV,PO | 4 mg/kg q12 h (d1: LD) | NA | <1 wk | Y | D * | Few days after amputation |
| Hodiamont (2009) [54] | 18,M | Cuneiform bones (R) | NS | ID | A. fumigatus | SD | Vor IV | 4 mg/kg q12 h | NA | ±13.5 mo | N | IF | ±13.5 mo after AFT initiation |
| → Caf IV | 70 mg q24 h | RS | |||||||||||
| → Pos PO | 400 mg q12 h | NS | |||||||||||
| NB: Itr prophylaxis started at age of 7 yr and restarted after Pos cessation | |||||||||||||
| Horn (2009) [49] | 60,F | Scapula (R) | C/H: IPA | SOT | A. fumigatus | None | Vor | NS | NA | 69 d | N | D | 74 d after OM diagnosis |
| → Pos | NS | NS | |||||||||||
| +Mcf IV | NS | ||||||||||||
| Karia (2011) [55] | 79,F | Femur | U | HM | A. fumigatus | None | Vor IV | NS | NA | 4 wk | N | IC | 4 wk after AFT initiation |
| +AmB IV | NS | ||||||||||||
| Hall (2012) [56] | 72,F | Proximal humerus (R) | DI: prior shoulder arthroscopy | DM | A. fumigatus | SD, reverse shoulder arthroplasty | Vor PO | 200 mg q12 h | NA | 16 mo | N | IF | 2 yr after OM diagnosis |
| +AmB cement spacer | 300 mg | ±6–12 wk | |||||||||||
| Hébert-Seropian (2020) [57] | 52,M | Scapula (L) | C/H: IPA | SOT, GVHD | A. fumigatus | Multiple SDs & drainages | Vor IV,PO | NS | NA | ±22 mo | N | IC | 2 yr after 2nd surgery |
| Vertebral osteomyelitis | |||||||||||||
| van Ooij (2000) [58] | 56,F | T12-L1 | NS | HM | A. fumigatus | SD, laminectomy, spinal stabilization | AmB IV | Total dose: 3000 mg | NA | ≥2.5 mo | N | IC | ≥5 yr after OM diagnosis |
| → Itr PO | NS | NS | |||||||||||
| Frazier (2001) [59] | 52,M | T7-T8,L1-L3 | C/H: A. endocarditis | IS | A. fumigatus | None | AmB IV | Total dose: 2000 mg | NA | NS | N | D * | 33 d after surgery |
| 62,M | L2-L3 | U | IS | A. fumigatus | Corpectomy, spinal stabilization | AmB IV | Total dose: 1100 mg | NA | NS | N | IF | ≥18 mo after OM diagnosis | |
| Govender (2001) [60] | 54,M | L4 | U | None | A. fumigatus | Decompression, spinal stabilization | AmB IV | 0.25–0.7 mg/kg q24 h | NA | 6–9 wk | N | IF | ≥2 yr after OM diagnosis |
| +5-FC PO | 200–400 mg/kg q24 h | ||||||||||||
| 29,F | T1 | U | None | A. fumigatus | Decompression, spinal stabilization | AmB IV | 0.25–0.7 mg/kg q24 h | NA | 6–9 wk | N | IF | ≥2 yr after OM diagnosis | |
| +5-FC PO | 200–400 mg/kg q24 h | ||||||||||||
| 18,F | T7 | U | None | A. fumigatus | Decompression, spinal stabilization | AmB IV | 0.25–0.7 mg/kg q24 h | NA | 6–9 wk | N | IF | ≥2 yr after OM diagnosis | |
| +5-FC PO | 200–400 mg/kg q24 h | ||||||||||||
| 33,M | T1 | U | None | A. fumigatus | Decompression, spinal stabilization | AmB IV | NS | NA | 6–9 wk | N | IF | ≥2 yr after OM diagnosis | |
| +5-FC PO | |||||||||||||
| → Flu | 400 mg/d | TA | |||||||||||
| Chi (2003) [61] | 63,M | C2-C5 | U | DM | A. flavus | Laminectomy | Itr PO | 200 mg q8–12 h | NA | 2 wk | N | D * | 2 wk after surgery |
| → AmB IV | 25 mg q24 h | NS | |||||||||||
| Salvalaggio (2003) [62] | 46,M | L3 | U | SOT, DM | A. fumigatus | SD, discectomy | AmB IV | 1 mg/kg q24 h | NA | 16 wk | N | IF | ≥18 mo after Tx |
| → AmB IV | 1 mg/kg q24 h | TF | |||||||||||
| +5-FC | 6 g q24 h | ||||||||||||
| → AmB IV | 1 mg/kg q24 h | NS | |||||||||||
| → Caf IV | 50 mg q24 h | TA | |||||||||||
| Stratov (2003) [63] | 52,M | L2,L4 | U | None | A. fumigatus | Partial vertebrectomy, discectomy | D-AmB IV | 1 mg/kg q24 h | NA | ±6.5 mo | N | IC | ≥15 mo after AFT cessation |
| → L-AmB IV | 4–7.5 mg/kg q24 h | TA, TF | |||||||||||
| → Vor IV,PO | 200–280 mg q12 h | TF | |||||||||||
| Vaishya (2003) [64] | 35,F | D11 | U | None | NS | Corpectomy, spinal stabilization | AmB IV | NS | NA | ±6 wk | N | D ** | 2 mo after surgery |
| → AmB IV | NS | NS | |||||||||||
| +Itr PO | 200 mg q12 h | ||||||||||||
| Kim (2004) [112] | 68,M | T1-T3 | C/H: suspicion of IPA | None | NS | Laminectomy, abscess drainage | Itr | 400 mg/d | NA | 27 d | N | D * | ≥5 wk after surgery |
| Salloum (2004) [65] | 48,M | T6-T7, rib 9–10 (L) | H: IV drug use | None | A. fumigatus | Rib resection, abscess drainage, chest wall excision | Itr PO | 200 mg q12 h | NA | 18 mo | N | IF | 18 mo after AFT initiation |
| Santos (2004) [66] | 59,F | T11-T12 | U | HM | A. fumigatus | Arthrodesis, partial vertebrectomy | Itr | 200 mg q12 h | NA | 9 mo | N | IC | NS |
| → Itr | 200 mg q12 h | NS | |||||||||||
| +L-AmB IV | 3 mg/kg q24 h | ||||||||||||
| → Itr | 200 mg q12 h | NS | |||||||||||
| Nusair (2005) [67] | 49,F | T8-T9 | NS | None | A. fumigatus | SD, corpectomy, discectomy, arthrodesis | Vor IV,PO | 200 mg q12 h | NA | 6 mo | N | IF | ±2 mo after surgery |
| Myhre (2006) [68] | 57,M | L2-L5 | DI: posterior spinal fusion | None | A. fumigatus | SD | Vor | NS | NA | NS | N | IC | NS |
| Dayan (2007) [69] | 78,F | T12-L1 | NS | IS | A. fumigatus | Spinal stabilization & realignment | Vor | NS | NA | NS | N | D ** | 2 wk after surgery |
| Andaluz (2008) [70] | 65,M | T1-T6 | C/H: IPA 3 yr before | None | A. fumigatus | None | Vor PO | 400 mg/d | NA | ≥5.5 mo | N | IC | ≥4 mo after OM diagnosis |
| → Caf IV | 50 mg q24 h (d1: LD) | NS | |||||||||||
| → D-AmB IV | 1 mg/kg q24 h | TF | |||||||||||
| → L-AmB IV | NS | TA | |||||||||||
| → Pos PO | 800 mg/d | TF | |||||||||||
| Horn (2009) [49] | 58,M | T7-T8 | NS | SOT | A. fumigatus | None | Vor | NS | NA | ≥84 d | N | NIF | 84 d after OM diagnosis |
| +Caf IV | NS | ||||||||||||
| → Vor | NS | NS | |||||||||||
| 44,F | T8-T9 | NS | None | A. fumigatus | Surgery type NS | Vor | NS | NA | ≥84 d | N | NIF | 84 d after OM diagnosis | |
| 46,F | T8-T9 | U | None | A. flavus | Surgery type NS | Vor | NS | NA | ≥84 d | N | NIF | 90 d after OM diagnosis | |
| 48,F | T4 | NS | None | A. fumigatus | Surgery type NS | L-AmB IV | NS | NA | ≥84 d | N | NIF | 84 d after OM diagnosis | |
| → Vor | NS | NS | |||||||||||
| Tew (2009) [71] | 50,M | T2-T8 | U | DM | A. fumigatus | Laminectomy, costovertebral joint excision, abscess drainage | Vor IV | 4 mg/kg q12 h (d1: LD) | NA | ±2 wk | N | D * | 2 wk after surgery |
| Vor PO | 200 mg q12 h | ||||||||||||
| Nandeesh (2010) [72] | 66,F | L2-S1 | U | DM | U | SD, anterior decompression, spinal stabilization | Vor | NS | NA | NS | N | IC | NS |
| Batra (2011) [73] | 45,M | L3-L5 | U | None | A. fumigatus | SD, laminectomy | Itr PO | 200 mg q12 h | NA | 3 mo | N | IC | FU: 36 mo |
| Studemeister (2011) [15] | 52,F | L2-L3,L4-L5 | C/H: pulmonary aspergillomas | None | A. fumigatus | SD, laminectomy, discectomy, internal fixation | Vor IV | 4 mg/kg q12 h | NA | 6 mo | Y | IF | 2 mo after initial surgery |
| Vor PO | 150–200 mg q12 h | ||||||||||||
| Zhu (2011) [74] | 46,M | L4-L5 | C/H: IPA | SOT | A. flavus | SD, spinal stabilization | Vor IV,PO | NS | NA | 15 mo | N | IC | 12 mo after AFT cessation |
| → ABCD IV | NS | NS | |||||||||||
| → Itr IV | 200 mg q12–24 h | TA | |||||||||||
| → Itr IV,PO alternately | 200 mg q12–24 h | NS | |||||||||||
| → Itr PO | 200 mg q24 h | NS | |||||||||||
| NB: prior AFT (Mcf + ABCD + Vor) for IPA | |||||||||||||
| Sethi (2012) [75] | 25,M | L4-L5 | U | None | U | Surgical decompression, interbody fusion | Itr | 200 mg q12 h | NA | 3 mo | N | IC | FU: 1 yr |
| 19,M | D10-D11 | U | None | U | Corpectomy, spinal fusion | Itr | 200 mg q12 h | NA | 2 mo (ITT) | N | IC | No FU | |
| Jiang (2013) [76] | 40,F | T1-T3 | U | None | A. nidulans | SD, laminectomy | Vor IV | 4 mg/kg q12 h (d1: LD) | NA | ±1,5 mo | N | IC | 1 yr after AFT cessation |
| Vor IV | 4 mg/kg q12 h (d1: LD) | AD | ±6 mo (re-initiation after cessation) | ||||||||||
| → Vor PO | 200 mg q12 h | NS | |||||||||||
| Nicolle (2013) [77] | 65,M | C2-C3 | C/H: prior otogenic skull base OM | DM | A. flavus | None (prior mastoidectomy) | Vor | NS | NA | 12 mo | N | IC | 12 mo after AFT initiation |
| McCaslin (2015) [78] | 19,F | T12-L1 | NS | HM | NS | Laminectomy, abscess drainage | Vor IV | 4 mg/kg q12 h (d1: LD) | NA | NS | N | D * | NS |
| Yoon (2015) [79] | 53,M | L2-L3 | U | None | NS | Laminectomy, corpectomy, spinal fusion | AmB IV | 0.35 mg/kg q24 h | NA | 30 d | N | IC | 7 mo after discharge |
| Li (2016) [80] | 53,M | L2-L3,L5 | C/H: suspicion of IPA | None | U | Multiple SDs & drainages, decompression, spinal stabilization | Vor IV,PO | 4 mg/kg q12 h (d1: LD) | NA | ≥3 mo | N | IC | ≥3 mo after AFT initiation |
| Ono (2018) [81] | 70,F | T4-T5 | C/H: IPA | HM | A. fumigatus | None | L-AmB IV | 2.5 mg/kg q24 h | NA | 14 d | N | D * | 14 d after admission |
| → L-AmB IV | 4 mg/kg q24 h | NS | |||||||||||
| +Mcf IV | 200 mg q24 h | ||||||||||||
| → Vor IV | 4 mg/kg q12 h (d1: LD) | NS | |||||||||||
| Shweikeh (2018) [82] | 58,F | L4-S1 | DI: multiple spinal surgeries, epidural injections | IS | NS | None | Vor IV | NS | NA | 3 mo (ITT) | N | IC | NS |
| +Mcf IV | NS | ||||||||||||
| Yang (2019) [83] | 51,M | T5-T10 | C/H: fungal infection (NS) | None | A. fumigatus | Laminectomy | AmB IV | 60 mg q24 h | NA | NS | N | D * | NS |
| Karaisz (2020) [84] | 64,F | Lumbar spine | NS | SOT | A. fumigatus | None | AmB IV | NS | NA | ±2 mo | N | D * | ±2 mo after AFT initiation |
| → Isa | NS | NS | |||||||||||
| +anidulafungin | NS | ||||||||||||
| Senosain-Leon (2020) [85] | 29,M | T4-T6 | C/H: IPA | HIV | NS | None | D-AmB | NS | NA | 2 d | N | D * | 2 d after D-AmB initiation |
| NB: prior AFT (Itr PO) for IPA | |||||||||||||
| Spondylodiscitis | |||||||||||||
| Grandière-Perez (2000) [29] | 40,M | L3-L4 | C/H: IPA | HM | A. terreus | NS | None | NA | NA | NA | Y | D ** | 6 mo after spondylo-discitis diagnosis |
| NB: prior treatment for IPA: AmB IV → Itr | 2 mg/kg q24 h → 800 mg/d | NA | ≥1 mo | ||||||||||
| Park (2000) [86] | 37,M | L3- -S1 | U | HM | A. terreus | SD, spinal fusion | AmB IV | Total dose: 2000 mg | NA | NS | N | IF | NS |
| Tang (2000) [87] | 43,M | L2-L3, L4-L5 | U | SOT | A. flavus | None (NB: Girdlestone procedure for A. coxarthritis) | L-AmB IV | 5 mg/kg q24 h | NA | ≥15 wk | N | IC | 1 yr after Tx |
| → Itr | 400 mg/d | NS | |||||||||||
| van Ooij (2000) [58] | 45,M | T4-T5 | C/H: pulmonary aspergillomas | HM | NS | SD, spinal stabilization | AmB IV | Total dose: 3800 mg | NA | ±6.5 mo | N | IC | 3 yr after surgery |
| → Itr PO | NS | NS | |||||||||||
| NB: prior AFT (AmB) for pulmonary aspergillomas | |||||||||||||
| 69,M | T12-L1 | C/H: suspicion of IPA | HM | A. fumigatus | SD, spinal stabilization | AmB IV | Total dose: 2070 mg | NA | ≥6 wk | N | D ** | 4 mo after surgery | |
| +5-FC IV | NS | ||||||||||||
| → Itr | 400 mg/d | NS | |||||||||||
| NB: prior AFT (AmB + Itr) for suspicion of IPA | |||||||||||||
| 39,F | L4-L5 | C/H: IPA | HM | A. fumigatus | SD, spinal stabilization | AmB IV | NS | NA | ≥4 mo | N | D ** | 4 mo after surgery | |
| → Itr PO | 400 mg/d | NS | |||||||||||
| → Experi-mental AFT | NS | TF | |||||||||||
| → AmB IV | NS | TF | |||||||||||
| Beckers (2002) [88] | 72,F | T11-T12 | C/H: IPA | None | NS | Vertebrectomy | AmB IV | NS | NA | NS | N | D ** | NS |
| → Itr | NS | TA | |||||||||||
| NB: prior AFT (Itr) for IPA | |||||||||||||
| Takagi (2002) [30] | 51,M | L1-L2 | U | HM | NS | None | AmB IV | 50 mg q24 h | NA | ≥40 d | Y | IC | NS |
| +Itr | 200 mg/d | ||||||||||||
| → Itr PO | 200–900 mg/d | TA | |||||||||||
| NB: prior AFT (AmB + Itr) for suspected fungal infection | |||||||||||||
| Lenzi (2004) [89] | 50,F | L4-L5 | DI: spinal surgery | None | A. fumigatus | SD | Itr | NS | NA | NS | N | IC | 3 mo after surgery |
| Park (2004) [90] | 59,F | L2-L4 | U | SOT | NS | Surgical decompression | AmB IV | NS | NA | NS | N | D * | ≥60 d after diagnosis |
| Mouas (2005) [4] | 76,M | C5-T2 | U | None | A. fumigatus | None | D-AmB IV | Total dose: 1200 mg | NA | ≥14 mo | N | IF | ±2.5–3 yr after diagnosis |
| → Vor IV,PO | ≥150 mg q12 h | NS | |||||||||||
| NB: prior empiric AFT (Itr) | |||||||||||||
| 62,M | NS | NS | None | A. fumigatus | NS | AmB IV | NS | NA | ≥84 d | N | NIF | ≥84 d after Vor initiation | |
| +5-FC | NS | ||||||||||||
| → Vor IV,PO | NS | NS | |||||||||||
| 53,F | Lumbar spine | NS | SOT | A. versicolor | NS | AmB IV | NS | NA | ≥197 d | N | NIF | ≥197 d after Vor initiation | |
| → Itr | NS | NS | |||||||||||
| → Vor PO | NS | NS | |||||||||||
| 45,M | L3-L4 | U | None | A. terreus | NS | Vor PO | NS | NS | 127 d | N | IC | ≥127 d after Vor initiation | |
| 39,M | L4-L5 | U | HM | A. fumigatus | NS | AmB IV | NS | NA | ≥47 d | N | IC | ≥47 d after Vor initiation | |
| → Itr | NS | NS | |||||||||||
| → Vor PO | NS | NS | |||||||||||
| 69,M | Lumbar spine | NS | DM | A. fumigatus | NS | AmB IV | NS | NA | ≥6 d | N | IC | ≥6 d after Vor initiation | |
| → Vor IV | NS | NS | |||||||||||
| Kolbe (2007) [91] | 51,F | L4-L5 (+menin-geal involve-ment) | DI: discography, epidural steroid injections | None | A. fumigatus | None | Caf IV | NS | NA | NS | N | D * | 4–5 mo after spondylo-discitis diagnosis |
| +Vor | NS | ||||||||||||
| → Long-term AF (NS) | NS | NS | |||||||||||
| Wéclawiak (2007) [92] | 18,M | T12-L1 | U | SOT | A. fumigatus | None | Vor | 200–400 mg/d | NA | 4 mo | N | IC | 4 mo after AFT initiation |
| Gerlach (2009) [93] | 25,M | L2-L3 | C/H: IPA | SOT | A. fumigatus | SD, spinal stabilization | Vor | NS | NA | ≥2 mo | N | IC | 15 mo after surgery |
| → Vor | NS | TF | |||||||||||
| +Caf IV | 50 mg q24 h | ||||||||||||
| +L-AmB IV | 5 mg/kg q24 h | ||||||||||||
| Oh (2009) [94] | 46,M | L3-L5, C4-C5, D2-D4, D6-D7, D10-D11 | C/H: pulmonary aspergillomas | SOT | NS | Decompression, interbody fusion | AmB IV | 50 mg q24 h | NA | ±15.5 mo | N | IC | ±3 yr after admission |
| → Itr | 100 mg q12 h | TF | |||||||||||
| → Vor | 200 mg q12 h | TF | |||||||||||
| Ersoy (2011) [95] | 46,M | T8-T9, L2-L3 | C/H: IPA | SOT | A. fumigatus | Corpus resection, discectomy, abscess drainage | Vor | 200 mg/d | NA | 107 d | N | IC | ≥18 mo after diagnosis |
| NB: prior AFT (Caf) for IPA | |||||||||||||
| Li (2012) [96] | 44,M | L4-L5, L5-S1 | U | SOT, DM | A. flavus | SD, decompression, spinal fusion | Vor IV | 4 mg/kg q12 h (d1: LD) | NA | NS | N | IC | ≥20 wk after AFT initiation |
| → Vor PO | 200 mg q12 h | ||||||||||||
| Raj (2013) [97] | 45,F | L5-S1 | NS | DM | A. fumigatus | Laminectomy, abscess drainage | Itr PO | 200 mg q12 h | NA | 3 mo | N | IC | 9 mo after surgery |
| Shashidhar (2014) [98] | 33,F | L2-L3 | DI: spinal anesthesia | None | A. fumigatus | SD, discectomy, spinal fusion | Vor IV,PO | 200 mg q12 h | NA | 12 wk | N | IC | FU: 1 yr |
| Comacle (2015) [31] | 20,M | T7-T12 | DI: motorbike accident (3 yr before) | None | A. niger | SD, spinal arthrodesis | Vor IV | 4 mg/kg q12 h (d1: LD) | NA | ≥2 mo | Y | IC | 4 mo after AFT initiation |
| → Vor PO | 200–400 mg q12 h | ||||||||||||
| → Caf IV | 50 mg q24 h (d1: LD) | TA | |||||||||||
| → Vor PO | NS | NS | |||||||||||
| +Caf IV | 50 mg q24 h | ||||||||||||
| → Vor PO | NS | NS | |||||||||||
| Dai (2020) [99] | 67,M | T3-T5 | C/H: IPA | None | A. fumigatus | None | Vor | 200 mg q12 h | NA | 20 wk | N | IC | FU: 20 mo |
| 68,M | T12-L2 | NS | IS | A. fumigatus | SD, laminectomy, decompression, instrumentation | Vor | 200 mg q12 h | NA | 16 wk | N | IC | FU: 24 mo | |
| 50,F | L3-L4 | NS | None | A. fumigatus | SD, laminectomy, instrumentation | Vor | 200 mg q12 h | NA | 18 wk | N | IC | FU: 24 mo | |
| 48,M | L4-L | U/DI: minimally invasive spinal surgery | None | A. fumigatus | SD, laminectomy, instrumentation | Vor | 200 mg q12 h | NA | 16 wk | N | IC | FU: 15 mo | |
| 43,M | L4-L5 | U/DI: spinal surgery | None | A. niger | SD, laminectomy, decompression, instrumentation | Vor | 200 mg q12 h | NA | 22 wk | N | IC | FU: 20 mo | |
| 66,M | L2-L3 | U/DI: spinal surgery | None | NS | SD, laminectomy, instrumentation | Vor | 200 mg q12 h | NA | 20 wk | N | IC | FU: 18 mo | |
| Fan (2020) [100] | 49,M | T12-L1, L2-L3 | NS | None | A. flavus | Percutaneous transforaminal endoscopic discectomy | Itr PO | 150 mg q12 h | NA | 13 mo | N | IC | 9 mo after surgery |
| +intervertebral Itr injections | NS | ||||||||||||
| Perna (2021) [12] | 76,M | L2-L3 | U | HM | A. fumigatus | None | L-AmB IV | NS | NA | 7 mo | N | IF | 7 mo after AFT initiation |
| → Vor PO | NS | NS | |||||||||||
References
- Depypere, M.; Morgenstern, M.; Kuehl, R.; Senneville, E.; Moriarty, T.F.; Obremskey, W.T.; Zimmerli, W.; Trampuz, A.; Lagrou, K.; Metsemakers, W.-J. Pathogenesis and management of fracture-related infection. Clin. Microbiol. Infect. 2019, 26, 572–578. [Google Scholar] [CrossRef] [PubMed]
- Metsemakers, W.-J.; Onsea, J.; Neutjens, E.; Steffens, E.; Schuermans, A.; McNally, M.; Nijs, S. Prevention of fracture-related infection: A multidisciplinary care package. Int. Orthop. 2017, 41, 2457–2469. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodriguez-Hernandez, M.; Jiménez-Mejías, M.E.; Montero, J.; Regordan, C.; Ferreras, G. Aspergillus fumigatus Cranial Infection After Accidental Traumatism. Eur. J. Clin. Microbiol. 2001, 20, 655–656. [Google Scholar] [CrossRef] [PubMed]
- Mouas, H.; Lutsar, I.; Dupont, B.; Fain, O.; Herbrecht, R.; Lescure, F.; Lortholary, O. The Voriconazole/Bone Invasive Aspergillosis Study Group Voriconazole for Invasive Bone Aspergillosis: A Worldwide Experience of 20 Cases. Clin. Infect. Dis. 2005, 40, 1141–1147. [Google Scholar] [CrossRef]
- Garazzino, S.; Maiello, A.; DE Rosa, F.G.; Aprato, A.; Di Perri, G. Post-Traumatic Osteomyelitis Due to Aspergillus flavus Successfully Treated with Voriconazole: A Case Report. J. Chemother. 2008, 20, 524–526. [Google Scholar] [CrossRef]
- Dabkana, T.; Mayun, A.; Pindiga, U.; Nggada, H. Aspergillosis of the bone. Ann. Afr. Med. 2015, 14, 62–64. [Google Scholar] [CrossRef]
- Takagi, Y.; Yamada, H.; Ebara, H.; Hayashi, H.; Kidani, S.; Okamoto, S.; Nakamura, Y.; Kitano, Y.; Kagechika, K.; Demura, S.; et al. Aspergillus terreus spondylodiscitis following an abdominal stab wound: A case report. J. Med Case Rep. 2019, 13, 1–6. [Google Scholar] [CrossRef] [Green Version]
- De Meo, D.; Cera, G.; Ceccarelli, G.; Castagna, V.; Aronica, R.; Pieracci, E.M.; Persiani, P.; Villani, C. Candida fracture-related infection: A systematic review. J. Bone Jt. Infect. 2021, 6, 321–328. [Google Scholar] [CrossRef]
- Gamaletsou, M.N.; Rammaert, B.; Bueno, M.A.; Moriyama, B.; Sipsas, N.V.; Kontoyiannis, D.P.; Roilides, E.; Zeller, V.; Prinapori, R.; Taj-Aldeen, S.J.; et al. Aspergillus osteomyelitis: Epidemiology, clinical manifestations, management, and outcome. J. Infect. 2013, 68, 478–493. [Google Scholar] [CrossRef] [Green Version]
- Gabrielli, E.; Fothergill, A.W.; Brescini, L.; Sutton, D.A.; Marchionni, E.; Orsetti, E.; Staffolani, S.; Castelli, P.; Gesuita, R.; Barchiesi, F. Osteomyelitis caused by Aspergillus species: A review of 310 reported cases. Clin. Microbiol. Infect. 2014, 20, 559–565. [Google Scholar] [CrossRef] [Green Version]
- Koehler, P.; Tacke, D.; Cornely, O.A. Aspergillosis of bones and joints—A review from 2002 until today. Mycoses 2013, 57, 323–335. [Google Scholar] [CrossRef] [PubMed]
- Perna, A.; Ricciardi, L.; Fantoni, M.; Taccari, F.; Torelli, R.; Santagada, D.A.; Fumo, C.; Tamburrelli, F.C.; Proietti, L. Spontaneous Vertebral Aspergillosis, the State of Art: A Systematic Literature Review. Neurospine 2021, 18, 23–33. [Google Scholar] [CrossRef]
- Patterson, T.F.; Thompson, G.R.; Denning, D.; Fishman, J.A.; Hadley, S.; Herbrecht, R.; Kontoyiannis, D.P.; Marr, K.A.; Morrison, V.A.; Nguyen, M.H.; et al. Executive Summary: Practice Guidelines for the Diagnosis and Management of Aspergillosis: 2016 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2016, 63, 433–442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kirby, A.; Hassan, I.; Burnie, J. Recommendations for managing Aspergillus osteomyelitis and joint infections based on a review of the literature. J. Infect. 2006, 52, 405–414. [Google Scholar] [CrossRef] [PubMed]
- Studemeister, A.; Stevens, D.A. Aspergillus Vertebral Osteomyelitis in Immunocompetent Hosts: Role of Triazole Antifungal Therapy. Clin. Infect. Dis. 2011, 52, e1–e6. [Google Scholar] [CrossRef]
- Metsemakers, W.; Morgenstern, M.; McNally, M.; Moriarty, F.; McFadyen, I.; Scarborough, M.; Athanasou, N.; Ochsner, P.; Kuehl, R.; Raschke, M.; et al. Fracture-related infection: A consensus on definition from an international expert group. Injury 2017, 49, 505–510. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dudareva, M.; Barrett, L.; Morgenstern, M.; Atkins, B.; Brent, A.; McNally, M. Providing an Evidence Base for Tissue Sampling and Culture Interpretation in Suspected Fracture-Related Infection. J. Bone Jt. Surg. 2021, 103, 977–983. [Google Scholar] [CrossRef]
- Ashbee, H.R.; Barnes, R.A.; Johnson, E.M.; Richardson, M.; Gorton, R.; Hope, W. Therapeutic drug monitoring (TDM) of antifungal agents: Guidelines from the British Society for Medical Mycology. J. Antimicrob. Chemother. 2013, 69, 1162–1176. [Google Scholar] [CrossRef] [Green Version]
- Denes, E.; Boumediene, A.; Durox, H.; Oksman, A.; Saint-Marcoux, F.; Darde, M.-L.; Gaulier, J.-M. Voriconazole concentrations in synovial fluid and bone tissues. J. Antimicrob. Chemother. 2007, 59, 818–819. [Google Scholar] [CrossRef]
- Maertens, J.A.; Raad, I.I.; Marr, K.A.; Patterson, T.; Kontoyiannis, D.P.; Cornely, O.; Bow, E.J.; Rahav, G.; Neofytos, D.; Aoun, M.; et al. Isavuconazole versus voriconazole for primary treatment of invasive mould disease caused by Aspergillus and other filamentous fungi (SECURE): A phase 3, randomised-controlled, non-inferiority trial. Lancet 2015, 387, 760–769. [Google Scholar] [CrossRef]
- Marty, F.M.; Ostrosky-Zeichner, L.; Cornely, O.A.; Mullane, K.M.; Perfect, J.R.; Thompson, G.R.; Alangaden, G.J.; Brown, J.M.; Fredricks, D.N.; Heinz, W.J.; et al. Isavuconazole treatment for mucormycosis: A single-arm open-label trial and case-control analysis. Lancet Infect. Dis. 2016, 16, 828–837. [Google Scholar] [CrossRef]
- Furfaro, E.; Signori, A.; Di Grazia, C.; Dominietto, A.; Raiola, A.M.; Aquino, S.; Ghiggi, C.; Ghiso, A.; Ungaro, R.; Angelucci, E.; et al. Serial monitoring of isavuconazole blood levels during prolonged antifungal therapy. J. Antimicrob. Chemother. 2019, 74, 2341–2346. [Google Scholar] [CrossRef]
- Vandecasteele, S.J.; Boelaert, J.R.; Verrelst, P.; Graulus, E.; Gordts, B.Z. Diagnosis and Treatment of Aspergillus flavus Sternal Wound Infections after Cardiac Surgery. Clin. Infect. Dis. 2002, 35, 887–890. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asare, K.A.; Jahng, M.; Pincus, J.L.; Massie, L.; Lee, S.A. Sternal osteomyelitis caused by Aspergillus fumigatus following cardiac surgery: Case and review. Med. Mycol. Case Rep. 2012, 2, 4–6. [Google Scholar] [CrossRef]
- Assaf, A.; Faure, E.; Sermet, K.; Loridant, S.; Leroy, J.; Goeminne, C.; Dozier, A.; Chopin, M.; Panaget, S.; Faure, K.; et al. Successful treatment of Aspergillus fumigatus sternal osteomyelitis with isavuconazole in a heart transplant recipient. Transpl. Infect. Dis. 2020, 22, e13313. [Google Scholar] [CrossRef] [PubMed]
- Doub, J.B.; Mathur, P. Duration of posaconazole therapy for Aspergillus fumigatus osteomyelitis dictated by serial monitoring of 1,3-beta-D glucan. Infection 2020, 48, 959–963. [Google Scholar] [CrossRef] [PubMed]
- Routray, C.; Nwaigwe, C. Sternal osteomyelitis secondary to Aspergillus fumigatus after cardiothoracic surgery. Med. Mycol. Case Rep. 2020, 28, 16–19. [Google Scholar] [CrossRef] [PubMed]
- Lodge, B.A.; Ashley, E.D.; Steele, M.P.; Perfect, J.R. Aspergillus fumigatus Empyema, Arthritis, and Calcaneal Osteomyelitis in a Lung Transplant Patient Successfully Treated with Posaconazole. J. Clin. Microbiol. 2004, 42, 1376–1378. [Google Scholar] [CrossRef] [Green Version]
- Grandière-Perez, L.; Asfar, P.; Chennebault, J.M.; Foussard, C.; Penn, P.; Degasne, I. Spondylodiscitis due to Aspergillus terreus during an efficient treatment against invasive pulmonary aspergillosis. Intensiv. Care Med. 2000, 26, 1010–1011. [Google Scholar] [CrossRef]
- Takagi, K.; Yoshida, A.; Yamauchi, T.; Yamashita, T.; Iwasaki, H.; Tsutani, H.; Maezawa, Y.; Baba, H.; Ueda, T. Successful treatment of Aspergillus spondylodiscitis with high-dose itraconazole in a patient with acute myelogenous leukemia. Leukemia 2001, 15, 1670–1671. [Google Scholar] [CrossRef] [Green Version]
- Comacle, P.; Le Govic, Y.; Hoche-Delchet, C.; Sandrini, J.; Aguilar, C.; Bouyer, B.; Blanchi, S.; Penn, P. Spondylodiscitis Due to Aspergillus terreus in an Immunocompetent Host: Case Report and Literature Review. Mycopathologia 2016, 181, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Bellmann, R.; Smuszkiewicz, P. Pharmacokinetics of antifungal drugs: Practical implications for optimized treatment of patients. Infection 2017, 45, 737–779. [Google Scholar] [CrossRef] [PubMed]
- Felton, T.; Troke, P.F.; Hope, W.W.; Simonsen, K.A.; Anderson-Berry, A.L.; Delair, S.F.; Dele Davies, H. Tissue Penetration of Antifungal Agents. Clin. Microbiol. Rev. 2014, 27, 68–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stover, K.R.; Cleary, J.D. Antifungal Penetration and Distribution into Organs and Tissue. Curr. Fungal Infect. Rep. 2020, 14, 279–288. [Google Scholar] [CrossRef]
- Schmitt-Hoffmann, A.-H.; Kato, K.; Townsend, R.; Potchoiba, M.J.; Hope, W.W.; Andes, D.; Spickermann, J.; Schneidkraut, M.J. Tissue Distribution and Elimination of Isavuconazole following Single and Repeat Oral-Dose Administration of Isavuconazonium Sulfate to Rats. Antimicrob. Agents Chemother. 2017, 61, e01292-17. [Google Scholar] [CrossRef] [Green Version]
- Ripp, S.L.; Aram, J.A.; Bowman, C.J.; Chmielewski, G.; Conte, U.; Cross, D.M.; Gao, H.; Lewis, E.M.; Lin, J.; Liu, P.; et al. Tissue Distribution of Anidulafungin in Neonatal Rats. Birth Defects Res. Part B Dev. Reprod. Toxicol. 2012, 95, 89–94. [Google Scholar] [CrossRef]
- Lawrence, R.M.; Hoeprich, P.D.; Jagdis, F.A.; Monji, N.; Huston, A.C.; Schaffner, C.P.; Domagala, J.M. Distribution of doubly radiolabelled amphotericin B methyl ester and amphotericin B in the non-human primate, Macaca mulatta. J. Antimicrob. Chemother. 1980, 6, 241–249. [Google Scholar] [CrossRef]
- Groll, A.H.; Mickiene, D.; Piscitelli, S.C.; Walsh, T.J. Distribution of Lipid Formulations of Amphotericin B into Bone Marrow and Fat Tissue in Rabbits. Antimicrob. Agents Chemother. 2000, 44, 408–410. [Google Scholar] [CrossRef] [Green Version]
- Adler-Moore, J.P.; Proffitt, R.T.; Olson, J.A.; Jensen, G.M. Tissue pharmacokinetics and pharmacodynamics of AmBisome® (L-AmBis) in uninfected and infected animals and their effects on dosing regimens. J. Liposome Res. 2017, 27, 195–209. [Google Scholar] [CrossRef]
- Fielding, R.; Singer, A.W.; Wang, L.H.; Babbar, S.; Guo, L.S. Relationship of pharmacokinetics and drug distribution in tissue to increased safety of amphotericin B colloidal dispersion in dogs. Antimicrob. Agents Chemother. 1992, 36, 299–307. [Google Scholar] [CrossRef] [Green Version]
- Conaughty, J.M.; Khurana, S.; Banovac, K.; Martinez, O.V.; Eismont, F.J. Antifungal Penetration into Normal Rabbit Nucleus Pulposus. Spine 2004, 29, E289–E293. [Google Scholar] [CrossRef] [PubMed]
- Visser, G.W.; Boele, S.; Knops, G.H.; Herscheid, J.D.; Hoekstra, A. Synthesis and biodistribution of [18F]-5-fluorocytosine. Nucl. Med. Commun. 1985, 6, 455–459. [Google Scholar] [CrossRef]
- Polak, A. Pharmacokinetics of amphotericin B and flucytosine. Postgrad. Med. J. 1979, 55, 667–670. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allen, D.; Ng, S.; Beaton, K.; Taussig, D. Sternal osteomyelitis caused by Aspergillus fumigatus in a patient with previously treated Hodgkin’s disease. J. Clin. Pathol. 2002, 55, 616–618. [Google Scholar] [CrossRef] [Green Version]
- Elahi, M.M.; Mitra, A.; Spears, J.; McClurken, J.B. Recalcitrant Chest Wall Aspergillus Fumigatus Osteomyelitis After Coronary Artery Bypass Grafting: Successful Radical Surgical and Medical Management. Ann. Thorac. Surg. 2005, 79, 1057–1059. [Google Scholar] [CrossRef] [PubMed]
- Soto-Hurtado, E.J.; Marín-Gámez, E.; Segura-Domínguez, N.; Jiménez-Oñate, F. Pleural Aspergillosis with Bronchopleurocutaneous Fistula and Costal Bone Destruction: A Case Report. Lung 2005, 183, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Natesan, S.; Abraham, G.; Mathew, M.; Lalitha, M.; Srinivasan, C. Secondary sternal Aspergillus osteomyelitis in a diabetic hemodialysis patient with previous allograft rejection. Hemodial. Int. 2007, 11, 403–405. [Google Scholar] [CrossRef] [PubMed]
- Verghese, S.; Chellamma, T.; Cherian, K.M. Osteomyelitis of the rib caused by Aspergillus flavus following cardiac surgery. Mycoses 2009, 52, 91–93. [Google Scholar] [CrossRef]
- Horn, D.; Sae-Tia, S.; Neofytos, D. Aspergillus osteomyelitis: Review of 12 cases identified by the Prospective Antifungal Therapy Alliance registry. Diagn. Microbiol. Infect. Dis. 2009, 63, 384–387. [Google Scholar] [CrossRef]
- Puri, V.; Johnson, S.M.; Munfakh, N.A. Fungal Osteomyelitis Masquerading as a Chest Wall Tumor. Ann. Thorac. Surg. 2011, 91, 304. [Google Scholar] [CrossRef]
- Landaburu, M.F.; Daneri, G.L.; Ploszaj, F.; Kruss, M.; Vinante, A.; Veciño, C.H.; Mujica, M.T. Osteomyelitis of the rib cage by Aspergillus flavus. Rev. Iberoam. Micol. 2019, 36, 86–89. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, J.; Sugawara, Y.; Makuuchi, M. Aspergillus osteomyelitis after liver transplantation. Liver Transplant. 2002, 8, 1073–1075. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brodsky, J.W.; Seidenfeld, S.M.; Brooks, B.; Shabat, S. Aspergillus Osteomyelitis and Lymphangitis in Immunocompromised Patient After Toenail Clipping. Foot Ankle Int. 2005, 26, 576–578. [Google Scholar] [CrossRef] [PubMed]
- Hodiamont, C.J.; Dolman, K.M.; Berge, I.J.M.T.; Melchers, W.J.G.; Verweij, P.E.; Pajkrt, D. Multiple-azole-resistant Aspergillus fumigatus osteomyelitis in a patient with chronic granulomatous disease successfully treated with long-term oral posaconazole and surgery. Med. Mycol. 2009, 47, 217–220. [Google Scholar] [CrossRef] [Green Version]
- Karia, S.; Jeyapalan, K.; Kennedy, B. Aspergillus fumigatus osteomyelitis in a patient receiving alemtuzumab for B-cell chronic lymphocytic leukaemia. Br. J. Haematol. 2011, 153, 147. [Google Scholar] [CrossRef]
- Hall, G.L.; Villanueva-Siles, E.; Borzykowski, R.M.; Gruson, K.I.; Dorfman, H.D.; Geller, D.S. Aspergillus osteomyelitis of the proximal humerus: A case report. Skelet. Radiol. 2012, 41, 1021–1025. [Google Scholar] [CrossRef]
- Hébert-Seropian, S.; Pelet, S. Aspergillus Osteomyelitis of the Scapula. JBJS Case Connect. 2020, 10, e0343. [Google Scholar] [CrossRef]
- Van Ooij, A.; Beckers, J.M.H.; Herpers, M.J.H.M.; Walenkamp, G.H.I.M. Surgical treatment of Aspergillus spondylodiscitis. Eur. Spine J. 2000, 9, 75–79. [Google Scholar] [CrossRef] [Green Version]
- Frazier, D.D.; Campbell, D.R.; Garvey, T.A.; Wiesel, S.; Bohlman, H.H.; Eismont, F.J. Fungal infections of the spine. Report of eleven patients with long-term follow-up. J. Bone Jt. Surg. Am. 2001, 83, 560–565. [Google Scholar] [CrossRef]
- Govender, S.; Kumar, K. Aspergillus spondylitis in immunocompetent patients. Int. Orthop. 2001, 25, 74–76. [Google Scholar] [CrossRef] [Green Version]
- Chi, C.Y.; Fung, C.P.; Liu, C.Y. Aspergillus flavus epidural abscess and osteomyelitis in a diabetic patient. J. Microbiol. Immunol. Infect. 2003, 36, 145–148. [Google Scholar] [PubMed]
- Salvalaggio, P.; Bassetti, M.; Lorber, M.; Micheletto, G.; Friedman, A.; Andriole, V.; Basadonna, G. Aspergillus vertebral osteomyelitis after simultaneous kidney-pancreas transplantation. Transpl. Infect. Dis. 2003, 5, 187–190. [Google Scholar] [CrossRef] [PubMed]
- Stratov, I.; Korman, T.; Johnson, P.D.R. Management of Aspergillus Osteomyelitis: Report of Failure of Liposomal Amphotericin B and Response to Voriconazole in an Immunocompetent Host and Literature Review. Eur. J. Clin. Microbiol. 2003, 22, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Vaishya, S.; Sharma, M.S. Spinal Aspergillus vertebral osteomyelitis with extradural abscess: Case report and review of literature. Surg. Neurol. 2004, 61, 551–555. [Google Scholar] [CrossRef] [PubMed]
- Salloum, A.; Rao, S.; Havasi, A.; Miljkovic, G.; Amoateng-Adjepong, Y. Aspergillus rib and vertebral osteomyelitis in a former intravenous drug user. Am. J. Med. 2004, 116, 208–209. [Google Scholar] [CrossRef] [PubMed]
- Santos, A.B.; Llamas, P.; Gadea, I.; Román, A.; Subirá, D.; Prieto, E.; Tomás, J.F. Aspergillus fumigatus: A rare cause of vertebral osteomyelitis. Haematologica 2004, 89, Ecr10. [Google Scholar]
- Nusair, A.; Smith, P.W. Aspergillus vertebral osteomyelitis in a immunocompetent host treated with voriconazole. Infect. Dis. Clin. Pract. 2007, 15, 122–124. [Google Scholar] [CrossRef]
- Myhre, A.P.; Jarosz, T.J.; Hunter, J.C.; Richardson, M.L. Postoperative Bone Graft Displacement: An Unusual Sign of Infection Following Posterior Spinal Fusion. Radiol. Case Rep. 2006, 1, 21–23. [Google Scholar] [CrossRef] [Green Version]
- Dayan, L.; Sprecher, H.; Hananni, A.; Rosenbaum, H.; Milloul, V.; Oren, I. Aspergillus vertebral osteomyelitis in chronic leukocyte leukemia patient diagnosed by a novel panfungal polymerase chain reaction method. Spine J. 2007, 7, 615–617. [Google Scholar] [CrossRef]
- Andaluz, N.; Zuccarello, M. Multidrug-resistant, progressive, invasive diffuse spinal aspergillosis: Case report and review of the literature. J. Neurosurg. Sci. 2008, 52, 49–53. [Google Scholar]
- Tew, C.W.; Han, F.C.; Jureen, R.; Tey, B.H. Aspergillus vertebral osteomyelitis and epidural abscess. Singap. Med. J. 2009, 50, e151–e154. [Google Scholar]
- Nandeesh, B.; Kini, U.; Alexander, B.; Bn, N. Vertebral osteomyelitis with a rare etiology diagnosed by fine-needle aspiration cytology. Diagn. Cytopathol. 2009, 38, 360–363. [Google Scholar] [CrossRef] [PubMed]
- Batra, P.; Shah, N. Recalcitrant osteomyelitis following tooth extraction in a case of malignant osteopetrosis. Int. Dent. J. 2004, 54, 418–423. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.-P.; Chen, X.-S.; Wu, J.-Q.; Yang, F.-F.; Weng, X.-H. Aspergillus vertebral osteomyelitis and ureteral obstruction after liver transplantation. Transpl. Infect. Dis. 2011, 13, 192–199. [Google Scholar] [CrossRef]
- Sethi, S.; Kalra, K.L.; Siraj, F.; Chopra, P. Aspergillus vertebral osteomyelitis in immunocompetent patients. Indian J. Orthop. 2012, 46, 246–250. [Google Scholar] [CrossRef]
- Jiang, Z.; Wang, Y.; Jiang, Y.; Xu, Y.; Meng, B. Vertebral osteomyelitis and epidural abscess due to Aspergillus nidulans resulting in spinal cord compression: Case report and literature review. J. Int. Med. Res. 2013, 41, 502–510. [Google Scholar] [CrossRef] [PubMed]
- Nicolle, A.; de la Blanchardière, A.; Bonhomme, J.; Hamon, M.; Leclercq, R.; Hitier, M. Aspergillus vertebral osteomyelitis in immunocompetent subjects: Case report and review of the literature. Infection 2013, 41, 833–840. [Google Scholar] [CrossRef]
- McCaslin, A.F.; Lall, R.R.; Wong, A.P.; Lall, R.R.; Sugrue, P.A.; Koski, T.R. Thoracic spinal cord intramedullary Aspergillus invasion and abscess. J. Clin. Neurosci. 2015, 22, 404–406. [Google Scholar] [CrossRef]
- Yoon, K.-W.; Kim, Y.-J. Lumbar Aspergillus osteomyelitis mimicking pyogenic osteomyelitis in an immunocompetent adult. Br. J. Neurosurg. 2014, 29, 277–279. [Google Scholar] [CrossRef]
- Li, Y.; Cen, Y.; Luo, Y.; Zhu, Z.; Min, S.; Chen, X. Aspergillus Vertebral Osteomyelitis Complicating Pulmonary Granuloma in an Immunocompetent Adult. Med. Princ. Pr. 2015, 25, 394–396. [Google Scholar] [CrossRef]
- Ono, R.; Sato, S.; Okada, S.; Kanbe, E.; Tanaka, E.; Tamai, Y. Invasive Pulmonary Aspergillosis in the Epidural Space in a Patient with Acute Myelogenous Leukemia with Myelodysplasia-related Changes: A Case Study and Literature Review of Vertebral Aspergillosis in Japan. Intern. Med. 2018, 57, 3205–3212. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shweikeh, F.; Zyck, S.; Sweiss, F.; Sangtani, A.; Shweikeh, M.; Issa, H.; Steinmetz, M.P.; Markarian, G.Z. Aspergillus spinal epidural abscess: Case presentation and review of the literature. Spinal Cord Ser. Cases 2018, 4, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, H.; Shah, A.A.; Nelson, S.B.; Schwab, J.H. Fungal spinal epidural abscess: A case series of nine patients. Spine J. 2019, 19, 516–522. [Google Scholar] [CrossRef] [PubMed]
- Karaisz, F.; Upadhyay, N.; Xie, C.; Aburjania, N.; Maley, W.R.; Civan, J.M.; Sass, D.A. S2505 Aspergillus Fumigatus Vertebral Osteomyelitis with Intracardiac and Renal Aspergillomas in a Liver Transplant Recipient: A Clinical Vignette. Am. J. Gastroenterol. 2020, 115, S1322. [Google Scholar] [CrossRef]
- Senosain-Leon, V.; Hidalgo-Benites, A.; Montenegro, J.A.; D’Angelo-Piaggio, L.; Beas, R. Invasive pulmonary aspergillosis with Aspergillus vertebral osteomyelitis in an HIV-infected adult: A case report. Int. J. STD AIDS 2019, 30, 1140–1142. [Google Scholar] [CrossRef]
- Park, K.U.; Lee, H.S.; Kim, C.J.; Kim, E.C. Fungal discitis due to Aspergillus terreusin a patient with acute lymphoblastic leukemia. J. Korean Med. Sci. 2000, 15, 704–707. [Google Scholar] [CrossRef] [Green Version]
- Tang, T.J.; Janssen, H.L.A.; Van Der Vlies, C.H.; De Man, R.A.; Metselaar, H.J.; Tilanus, H.W.; De Marie, S. Aspergillus osteomyelitis after liver transplantation. Eur. J. Gastroenterol. Hepatol. 2000, 12, 123–126. [Google Scholar] [CrossRef]
- Beckers, E.A.; van Schijndel, R.J.S. Aspergillus spondylodiskitis in a patient with chronic obstructive pulmonary disease. Eur. J. Intern. Med. 2002, 13, 139–142. [Google Scholar] [CrossRef]
- Lenzi, J.; Agrillo, A.; Santoro, A.; Marotta, N.; Cantore, G.P. Postoperative spondylodiscitis from Aspergillus fumigatus in immunocompetent subjects. J. Neurosurg. Sci. 2004, 48, 81–85. [Google Scholar]
- Park, S.; Kang, M.; Whang, E.; Han, S.; Kim, H. A case of fungal sepsis due to Aspergillus spondylitis followed by cytomegalovirus infection in a renal transplant recipient. Transplant. Proc. 2004, 36, 2154–2155. [Google Scholar] [CrossRef]
- Kolbe, A.B.L.; Mckinney, A.; Kendi, A.T.K.; Misselt, D. Aspergillus meningitis and discitis from low-back procedures in an immunocompetent patient. Acta Radiol. 2007, 48, 687–689. [Google Scholar] [CrossRef] [PubMed]
- Wéclawiak, H.; Garrouste, C.; Kamar, N.; Linas, M.-D.; Tall, P.; Dambrin, C.; Durand, D.; Rostaing, L. Aspergillus fumigatus-Related Spondylodiscitis in a Heart Transplant Patient Successfully Treated With Voriconazole. Transplant. Proc. 2007, 39, 2627–2628. [Google Scholar] [CrossRef] [PubMed]
- Gerlach, U.A.; Kohler, S.; Sauer, I.M.; Joerres, D.; Kandziora, F.; Neuhaus, P.; Pratschke, J.; Pascher, A. Aspergillus spondylodiscitis after multivisceral transplantation. Ann. Transplant. 2009, 14, 52–57. [Google Scholar] [PubMed]
- Oh, I.-S.; Seo, J.-Y.; Ha, K.-Y.; Kim, Y.-C. Treatment for Multiple Aspergillus Spondylitis Including a Hip Joint. Asian Spine J. 2009, 3, 106–112. [Google Scholar] [CrossRef] [Green Version]
- Ersoy, A.; Dizdar, O.S.; Koc, A.O.; Akalin, H.; Ener, B. Aspergillus fumigatus spondylodiskitis in renal transplant patient: Voriconazole experience. Exp. Clin. Transplant. 2011, 9, 265–269. [Google Scholar] [PubMed]
- Li, X.F.; Liu, Z.D.; Xia, Q.; Dai, L.Y.; Zhong, G.B.; Chen, B. Primary Aspergillus spondylodiscitis in a liver transplant recipient. Chin. Med. J. 2012, 125, 2772–2774. [Google Scholar] [PubMed]
- Raj, K.A.; Srinivasamurthy, B.C.; Sinduja, M.G.I.; Nagarajan, K. A rare case of spontaneous Aspergillus spondylodiscitis with epidural abscess in a 45-year-old immunocompetent female. J. Craniovertebral Junction Spine 2013, 4, 82–84. [Google Scholar] [CrossRef]
- Shashidhar, N.; Tripathy, S.K.; Balasubramanian, S.; Dhanakodi, N.; Venkataramaiah, S. Aspergillus Spondylodiscitis in an Immunocompetent Patient following Spinal Anesthesia. Orthop. Surg. 2014, 6, 72–77. [Google Scholar] [CrossRef]
- Dai, G.; Wang, T.; Yin, C.; Sun, Y.; Xu, D.; Wang, Z.; Luan, L.; Hou, J.; Li, S. Aspergillus spondylitis: Case series and literature review. BMC Musculoskelet. Disord. 2020, 21, 572. [Google Scholar] [CrossRef]
- Fan, Y.; Xie, T.; Pang, Y.; Zhu, L.; Zhou, S. Percutaneous transforaminal endoscopic discectomy for the treatment of lateral recess stenosis secondary occurred the discal fungus infection. BMC Musculoskelet. Disord. 2020, 21, 175. [Google Scholar] [CrossRef]
- Herbrecht, R.; Denning, D.; Patterson, T.F.; Bennett, J.E.; Greene, R.E.; Oestmann, J.-W.; Kern, W.V.; Marr, K.A.; Ribaud, P.; Lortholary, O.; et al. Voriconazole versus Amphotericin B for Primary Therapy of Invasive Aspergillosis. N. Engl. J. Med. 2002, 347, 408–415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Donnelly, J.P.; Chen, S.C.; Kauffman, C.A.; Steinbach, W.J.; Baddley, J.W.; Verweij, P.E.; Clancy, C.J.; Wingard, J.R.; Lockhart, S.R.; Groll, A.H.; et al. Revision and Update of the Consensus Definitions of Invasive Fungal Disease from the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin. Infect. Dis. 2020, 71, 1367–1376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McNally, M.; Sousa, R.; Wouthuyzen-Bakker, M.; Chen, A.F.; Soriano, A.; Vogely, H.C.; Clauss, M.; Higuera, C.A.; Trebše, R. The EBJIS definition of periprosthetic joint infection. Bone Jt. J. 2021, 103-B, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Zalavras, C.G.; Aerden, L.; Declercq, P.; Belmans, A.; Metsemakers, W.-J. Ninety-Day Follow-up Is Inadequate for Diagnosis of Fracture-related Infections in Patients with Open Fractures. Clin. Orthop. Relat. Res. 2021, 480, 139–146. [Google Scholar] [CrossRef]
- Metsemakers, W.-J.; On behalf of the Fracture-Related Infection (FRI) group; Morgenstern, M.; Senneville, E.; Borens, O.; Govaert, G.A.M.; Onsea, J.; Depypere, M.; Richards, R.G.; Trampuz, A.; et al. General treatment principles for fracture-related infection: Recommendations from an international expert group. Arch. Orthop. Trauma. Surg. 2019, 140, 1013–1027. [Google Scholar] [CrossRef] [Green Version]
- Heykants, J.; Michiels, M.; Meuldermans, W.; Monbaliu, J.; Lavrijsen, K.; Van Peer, A.; Levron, J.C.; Woestenborghs, R.; Cauwenbergh, G. The pharmacokinetics of itraconazole in animals and man: An overview Recent Trends in the Discovery. Dev. Eval. Antifung. Agents 1987, 223–249. [Google Scholar]
- Sendi, P.; Zimmerli, W. Antimicrobial treatment concepts for orthopaedic device-related infection. Clin. Microbiol. Infect. 2012, 18, 1176–1184. [Google Scholar] [CrossRef] [Green Version]
- Landersdorfer, C.B.; Bulitta, J.B.; Kinzig, M.; Holzgrabe, U.; Sorgel, F. Penetration of antibacterials into bone: Pharmacokinetic, pharmacodynamic and bioanalytical considerations. Clin. Pharmacokinet. 2009, 48, 89–124. [Google Scholar] [CrossRef]
- Navarro, A.S. Relevance of antibacterial distribution: The particular case of bone penetration. Clin. Pharmacokinet. 2009, 48, 129–130. [Google Scholar] [CrossRef]
- Schauwvlieghe, A.F.A.D.; Buil, J.B.; Verweij, P.; Hoek, R.A.S.; Cornelissen, J.J.; Blijlevens, N.M.; Henriet, S.S.V.; Rijnders, B.; Brüggemann, R.J.M. High-dose posaconazole for azole-resistant aspergillosis and other difficult-to-treat mould infections. Mycoses 2019, 63, 122–130. [Google Scholar] [CrossRef]
- Seidel, D.; Duran Graeff, L.A.; Vehreschild, M.; Wisplinghoff, H.; Ziegler, M.; Vehreschild, J.J.; Liss, B.; Hamprecht, A.; Kohler, P.; Racil, Z.; et al. FungiScope: Global emerging fungal infection registry. Mycoses 2017, 60, 508–516. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Kim, S.B.; Yi, H.J.; Chung, W.S. Thoracic interdural Aspergillus abscess causing rapid fatal spondylitis in the presence of posterior mediastinitis. J. Korean Neurosurg. Soc. 2005, 37, 146–149. [Google Scholar]


| Reference (Year) | Age, Sex | Infection Location | Infection Mechanism | Host Factors | A. Species | Surgical Treatment | AFT | Posology | Rationale Switch | Duration | TDM | Clinical Outcome | FU Clinical Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rodríguez-Hernández (2001) [3] | 30,F | Parietal bone (R) | DI: fracture after cranial trauma | None | A. fumigatus | SD | AmB IV | 1 mg/kg q24 h | NA | 27 wk | Y | IC | 2 yr after FRI diagnosis |
| → Itr PO | 200 mg q12 h | NS | |||||||||||
| Mouas (2005) [4] | 46,M | Metacarpal bone (R) | DI: fracture after trauma | None | A. terreus | SD | Vor PO | 150–200 mg q12 h | NA | 93 d | N | IF | 9 yr after trauma |
| Mouas (2005) [4] | 43,M | Femur, fibula (L) | DI: fracture after trauma | None | A. fumigatus | SD, external fixation, knee arthrodesis | Itr | 400 mg q24 h | NA | ±35 wk | Y | IF | 14 mo after trauma |
| → L-AmB IV | 3 mg/kg q24 h | TF | |||||||||||
| → Vor PO | 200 mg q12 h (d1: 400 mg q12 h) | TF | |||||||||||
| Garazzino (2008) [5] | 69,M | Tibia (L) | DI: chronic infection after trauma (30 yr before) | DM | A. flavus | SD | Vor IV,PO | 4 mg/kg q12 h (d1: 6 mg/kg q12 h) | NA | 7 mo | N | IF | ≥4 mo after AFT initiation |
| Dabkana (2015) [6] | 26,F | Tibia, patella, femur (R) | DI: femur fracture after trauma | None | NS | Sequestrectomy, amputation, hip disarticulation | Tioconazole | NS | NA | NS | N | IC | NS |
| Takagi (2019) [7] | 74,M | T11-T12 vertebrae | DI: fractures of T12, L1, rib 10–12 (L) after trauma | None | A. terreus | Partial laminectomy, spinal fusion | Vor IV,PO | 600 mg/d | NA | 5 mo | N | IC | 2 yr after surgery |
| Reference (Year) | Antifungal Drug | Posology | Duration of AFT at Sampling Time | Time after Last Dose (Hours) | Plasma Concentration (mg/L) |
|---|---|---|---|---|---|
| Fracture-related infection | |||||
| Rodríguez-Hernández (2001) [3] | Itr PO | 200 mg q12 h | NS | NS | 2.26–2.29 |
| Mouas (2005) a [4] | Itr | 400 mg q24 h | NS | NS | Within applied therapeutic range (NS) |
| Sternal/rib osteomyelitis | |||||
| Vandecasteele (2002) b–f [23] | Itr PO | 200 mg q12 h | NS | ±12 | Within therapeutic range (0.791–8.066) |
| Mouas (2005) g [4] | Itr | 400 mg q24 h | NS | NS | Within applied therapeutic range (NS) |
| Asare (2013) [24] | Vor IV,PO | 300 mg q12 h (d1: 500 mg q12 h) | 3 d | NS | 5 |
| Assaf (2020) [25] | Vor IV,PO | 4 mg q12 h (d1: 6 mg/kg q12 h) | ≥7 d to ≤2 mo | NS | 2.2–2.4 |
| Isa | 200 mg q24 h (d1,2: 200 mg q8 h) | 5 d | NS | 3.2 | |
| Doub (2020) [26] | Pos PO | 300 mg q24 h | 2 wk | ±24 | 0.9 |
| 400 mg q24 h | 6 wk h | ±24 | 2.1 | ||
| Routray (2020) [27] | Vor IV,PO | 200 mg q12 h | ±4 wk | NS | Undetectable |
| Vor PO | 400 mg q12 h | ±8 wk h | NS | Undetectable | |
| Osteomyelitis of the lower extremities | |||||
| Lodge (2004) [28] | Itr PO | 200 mg q12 h | ±15 d | NS | Undetectable |
| Denes (2007) [19] | Vor IV,PO | 4 mg/kg q12 h (d1: 6 mg/kg q12 h) | 1 d | ±12 | 2.41 |
| 2 d | ±12 | 4.09 | |||
| NB: cortical and medullar bone concentrations on day 6: 1.9 μg/g and 20.3 μg/g | |||||
| Vertebral osteomyelitis | |||||
| Studemeister (2011) [15] | Vor IV | 4 mg/kg q12 h | NS | ±12 | 2.4 |
| Vor PO | 200 mg q12 h | ≥6 wk | ±12 | 3.3 | |
| 150 mg q12 h | NS | ±12 | 2.3 | ||
| Spondylodiscitis | |||||
| Grandière-Perez (2000) [29] | Itr | 800 mg/d | NS | NS | Mean concentration: 3 |
| Takagi (2002) [30] | Itr PO | 900 mg/d | 19 d | NS | Itr + hydroxy-Itr: 5.9 |
| 200 mg/d | 26 d i | NS | Itr + hydroxy-Itr: 13 | ||
| Comacle (2015) [31] | Vor IV | 4 mg q12 h (d1: 6 mg/kg q12 h) | 10 d | NS | 0.7 j |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mertens, B.; Van Daele, R.; Depypere, M.; Lagrou, K.; Debaveye, Y.; Wauters, J.; Nijs, S.; Metsemakers, W.-J.; Spriet, I. Isavuconazole in the Treatment of Aspergillus fumigatus Fracture-Related Infection: Case Report and Literature Review. Antibiotics 2022, 11, 344. https://doi.org/10.3390/antibiotics11030344
Mertens B, Van Daele R, Depypere M, Lagrou K, Debaveye Y, Wauters J, Nijs S, Metsemakers W-J, Spriet I. Isavuconazole in the Treatment of Aspergillus fumigatus Fracture-Related Infection: Case Report and Literature Review. Antibiotics. 2022; 11(3):344. https://doi.org/10.3390/antibiotics11030344
Chicago/Turabian StyleMertens, Beatrijs, Ruth Van Daele, Melissa Depypere, Katrien Lagrou, Yves Debaveye, Joost Wauters, Stefaan Nijs, Willem-Jan Metsemakers, and Isabel Spriet. 2022. "Isavuconazole in the Treatment of Aspergillus fumigatus Fracture-Related Infection: Case Report and Literature Review" Antibiotics 11, no. 3: 344. https://doi.org/10.3390/antibiotics11030344
APA StyleMertens, B., Van Daele, R., Depypere, M., Lagrou, K., Debaveye, Y., Wauters, J., Nijs, S., Metsemakers, W.-J., & Spriet, I. (2022). Isavuconazole in the Treatment of Aspergillus fumigatus Fracture-Related Infection: Case Report and Literature Review. Antibiotics, 11(3), 344. https://doi.org/10.3390/antibiotics11030344








