Conventional and Real-Time PCR Targeting blaOXA Genes as Reliable Methods for a Rapid Detection of Carbapenem-Resistant Acinetobacter baumannii Clinical Strains
Abstract
:1. Introduction
2. Results
2.1. Antimicrobial Susceptibility
2.2. Results of the Reference Method of Carbapenemase Genes Detection
2.3. Results Comparison
3. Discussion
4. Conclusions
5. Materials and Methods
5.1. Bacterial Strains and Their Origin
5.2. Antimicrobial Susceptibility
5.3. Carbapenemases and Carbapenemase Genes Detection
5.4. Phenotypic Tests
5.5. Molecular Biology-Based Approach
5.5.1. DNA Template Extraction
5.5.2. Conventional “In House” PCR for the Detection of blaOXA Genes
5.6. Data Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dijkshoorn, L.; Nemec, A.; Seifert, H. An Increasing Threat in Hospitals: Multidrug-Resistant Acinetobacter baumannii. Nat. Rev. Microbiol. 2007, 5, 939–951. [Google Scholar] [CrossRef] [PubMed]
- Protic, D.; Pejovic, A.; Andjelkovic, D.; Djukanovic, N.; Savic, D.; Piperac, P.; Markovic Denic, L.; Zdravkovic, M.; Todorovic, Z. Nosocomial Infections Caused by Acinetobacter baumannii: Are We Losing the Battle? Surg. Infect. 2016, 17, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Antunes, L.C.S.; Visca, P.; Towner, K.J. Acinetobacter Baumannii: Evolution of a Global Pathogen. Pathog. Dis. 2014, 71, 292–301. [Google Scholar] [CrossRef] [Green Version]
- Custovic, A.; Smajlovic, J.; Tihic, N.; Hadzic, S.; Ahmetagic, S.; Hadzagic, H. Epidemiological Monitoring of Nosocomial Infections Caused by Acinetobacter baumannii. Med. Arch. 2014, 68, 402–406. [Google Scholar] [CrossRef] [Green Version]
- Abbott, I.; Cerqueira, G.M.; Bhuiyan, S.; Peleg, A.Y. Carbapenem Resistance in Acinetobacter baumannii: Laboratory Challenges, Mechanistic Insights and Therapeutic Strategies. Expert Rev. Anti-Infect. 2013, 11, 395–409. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.; Joshi, S.G. Carbapenem resistance in Acinetobacter baumannii, and their importance in hospital-acquired infections: A scientific review. J. Appl. Microbiol. 2021, 131, 2715–2738. [Google Scholar] [CrossRef] [PubMed]
- Shin, B.; Park, W. Antibiotic Resistance of Pathogenic Acinetobacter Species and Emerging Combination Therapy. J. Microbiol. 2017, 55, 837–849. [Google Scholar] [CrossRef]
- Ramirez, M.S.; Bonomo, R.A.; Tolmasky, M.E. Carbapenemases: Transforming Acinetobacter baumannii into a Yet More Dangerous Menace. Biomolecules 2020, 10, 720. [Google Scholar] [CrossRef] [PubMed]
- Turton, J.F.; Ward, M.E.; Woodford, N.; Kaufmann, M.E.; Pike, R.; Livermore, D.M.; Pitt, T.L. The Role of ISAba1 in Expression of OXA Carbapenemase Genes in Acinetobacter baumannii. FEMS Microbiol. Lett. 2006, 258, 72–77. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, A.T.; Pham, S.C.; Ly, A.K.; Nguyen, C.V.V.; Vu, T.T.; Ha, T.M. Overexpression of blaOXA-58 Gene Driven by ISAba3 Is Associated with Imipenem Resistance in a Clinical Acinetobacter baumannii Isolate from Vietnam. Biomed. Res. Int. 2020, 2020, 7213429. [Google Scholar] [CrossRef]
- Bedenić, B.; Plečko, V.; Sardelić, S.; Uzunović, S.; Godič Torkar, K. Carbapenemases in Gram-Negative Bacteria: Laboratory Detection and Clinical Significance. BioMed. Res. Int. 2014, 2014, e841951. [Google Scholar] [CrossRef] [PubMed]
- National Institiute for Health and Care Excellence. Eazyplex SuperBug Kits for Detecting Carbapenemaseproducing Organisms. Available online: https://www.nice.org.uk/advice/mib94/resources/eazyplex-superbug-kits-for-detecting-carbapenemaseproducing-organisms-pdf-63499468392133#:~:text=One%20study%20reported%20that%20the,sequencing%20results%20for%20clinical%20isolates (accessed on 18 March 2022).
- Peleg, A.Y.; Seifert, H.; Paterson, D.L. Acinetobacter baumannii: Emergence of a Successful Pathogen. Clin. Microbiol. Rev. 2008, 21, 538–582. [Google Scholar] [CrossRef] [Green Version]
- Cai, Y.; Chai, D.; Wang, R.; Liang, B.; Bai, N. Colistin Resistance of Acinetobacter baumannii: Clinical Reports, Mechanisms and Antimicrobial Strategies. J. Antimicrob. Chemother. 2012, 67, 1607–1615. [Google Scholar] [CrossRef]
- Imperi, F.; Antunes, L.C.S.; Blom, J.; Villa, L.; Iacono, M.; Visca, P.; Carattoli, A. The Genomics of Acinetobacter baumannii: Insights into Genome Plasticity, Antimicrobial Resistance and Pathogenicity. IUBMB Life 2011, 63, 1068–1074. [Google Scholar] [CrossRef]
- Słoczyńska, A.; Wand, M.E.; Tyski, S.; Laudy, A.E. Analysis of BlaCHDL Genes and Insertion Sequences Related to Carbapenem Resistance in Acinetobacter baumannii Clinical Strains Isolated in Warsaw, Poland. Int. J. Mol. Sci. 2021, 22, 2486. [Google Scholar] [CrossRef] [PubMed]
- Anane, Y.A.; Apalata, T.; Vasaikar, S.; Okuthe, G.E.; Songca, S. Molecular Detection of Carbapenemase-Encoding Genes in Multidrug-Resistant Acinetobacter baumannii Clinical Isolates in South Africa. Int. J. Microbiol. 2020, 2020, 7380740. [Google Scholar] [CrossRef]
- Mugnier, P.D.; Poirel, L.; Naas, T.; Nordmann, P. Worldwide Dissemination of the blaOXA-23 Carbapenemase Gene of Acinetobacter baumannii. Emerg. Infect. Dis. 2010, 16, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Dortet, L.; Poirel, L.; Errera, C.; Nordmann, P. CarbAcineto NP Test for Rapid Detection of Carbapenemase-Producing Acinetobacter Spp. J. Clin. Microbiol. 2014, 52, 2359–2364. [Google Scholar] [CrossRef] [Green Version]
- Literacka, E.; Herda, M.; Baraniak, A.; Żabicka, D.; Hryniewicz, W.; Skoczyńska, A.; Gniadkowski, M. of the Carba NP Test for Carbapenemase Detection in Enterobacteriaceae, Pseudomonas Spp. and Acinetobacter Spp., and Its Practical Use in the Routine Work of a National Reference Laboratory for Susceptibility Testing. Eur. J. Clin. Microbiol. Infect. Dis. 2017, 36, 2281–2287. [Google Scholar] [CrossRef]
- Bogiel, T.; Rzepka, M.; Gospodarek-Komkowska, E. An Application of Imipenem Discs or P. Aeruginosa ATCC 27853 Reference Strain Increases Sensitivity of Carbapenem Inactivation Method for Non-Fermenting Gram-Negative Bacteria. Antibiotics 2021, 10, 875. [Google Scholar] [CrossRef]
- Simner, P.J.; Opene, B.N.A.; Chambers, K.K.; Naumann, M.E.; Carroll, K.C.; Tamma, P.D. Carbapenemase Detection among Carbapenem-Resistant Glucose-Nonfermenting Gram-Negative Bacilli. J. Clin. Microbiol. 2017, 55, 2858–2864. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poirel, L.; Naas, T.; Nordmann, P. Diversity, Epidemiology, and Genetics of Class D β-Lactamases. Antimicrob. Agents Chemother. 2010, 54, 24–38. [Google Scholar] [CrossRef] [Green Version]
- Whitley, V.; Kircher, S.; Gill, T.; Hindler, J.A.; O’Rourke, S.; Cooper, C.; Tulpule, A.; Denys, G.A. Multicenter Evaluation of the BD Phoenix CPO Detect Test for Detection and Classification of Carbapenemase-Producing Organisms in Clinical Isolates. J. Clin. Microbiol. 2020, 58, e01752-19. [Google Scholar] [CrossRef] [Green Version]
- Thomson, G.; Turner, D.; Brasso, W.; Kircher, S.; Guillet, T.; Thomson, K. High-Stringency Evaluation of the Automated BD Phoenix CPO Detect and Rapidec Carba NP Tests for Detection and Classification of Carbapenemases. J. Clin. Microbiol. 2017, 55, 3437–3443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mentasti, M.; Prime, K.; Sands, K.; Khan, S.; Wootton, M. Rapid Detection of OXA-23-like, OXA-24-like, and OXA-58-like Carbapenemases from Acinetobacter Species by Real-Time PCR. J. Hosp. Infect. 2020, 105, 741–746. [Google Scholar] [CrossRef]
- EUCAST: Previous Versions of Documents. Available online: https://www.eucast.org/ast_of_bacteria/previous_versions_of_documents/ (accessed on 17 January 2022).
- Literacka, E. Wykrywanie karbapenemaz u pałeczek Enterobacterales, Pseudomonas spp. i Acinetobacter spp. Test CIM. 2019. Available online: https://korld.nil.gov.pl/pdf/CIM%20-%20KORLD_2019.pdf (accessed on 17 January 2022).
- Abrar, S.; Vajeeha, A.; Ul-Ain, N.; Riaz, S. Distribution of CTX-M Group I and Group III β-Lactamases Produced by Escherichia coli and Klebsiella pneumoniae in Lahore, Pakistan. Microb. Pathog. 2017, 103, 8–12. [Google Scholar] [CrossRef]
- Woodford, N.; Ellington, M.J.; Coelho, J.M.; Turton, J.F.; Ward, M.E.; Brown, S.; Amyes, S.G.B.; Livermore, D.M. Multiplex PCR for Genes Encoding Prevalent OXA Carbapenemases in Acinetobacter Spp. Int. J. Antimicrob. Agents 2006, 27, 351–353. [Google Scholar] [CrossRef]



| Antimicrobial | Resistant Strains (n = 58) Number (%) |
|---|---|
| Imipenem | 58 (100%) |
| Meropenem | 58 (100%) |
| Gentamicin | 43 (74.1%) |
| Amikacin | 55 (94.8%) |
| Tobramycin | 56 (96.6%) |
| Ciprofloxacin | 58 (100%) |
| Levofloxacin | 58 (100%) |
| Trimethoprim/sulfamethoxazole | 57 (98.3%) |
| Colistin | 5 (8.6%) |
| No. of Isolates Positive for a Particular Class of Beta-Lactamases/Strains Number (%) | |
|---|---|
| Assay | Class D carbapenemase |
| CPO | 53/58 (91.4%) |
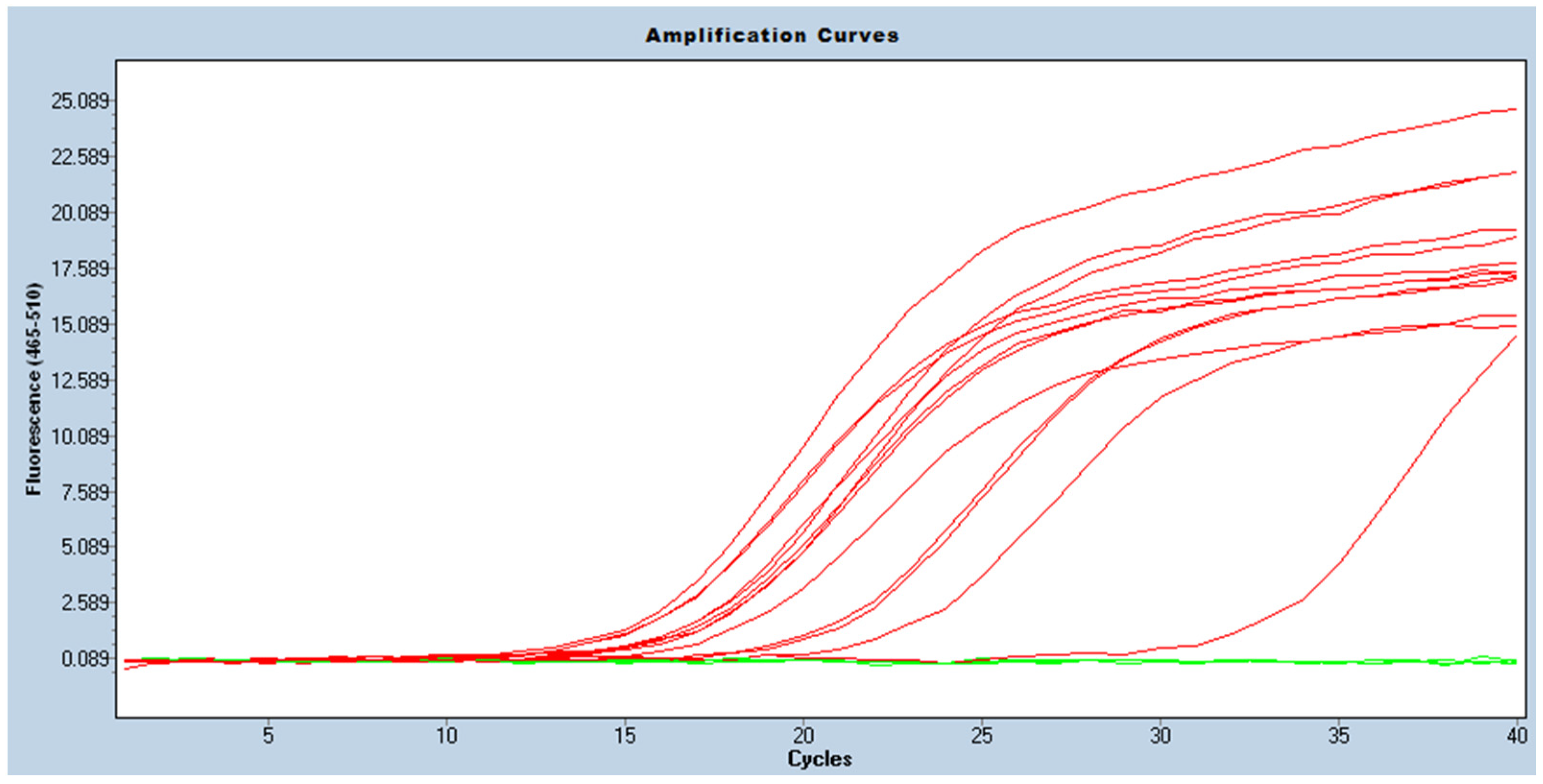
| Real-time PCR | 58/58 (100%) |
| Conventional PCR | 58/58 (100%) |
| Assay | No. of Positive Results of Carbapenemase Detection/Strains Number (%) |
|---|---|
| CarbAcineto NP | 38/58 (65.5%) * |
| CIM | 58/58 (100%) |
| CPO | 58/58 (100%) |
| Real-time PCR | 58/58 (100%) |
| Conventional PCR | 58/58 (100%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Depka, D.; Mikucka, A.; Bogiel, T.; Rzepka, M.; Zawadka, P.; Gospodarek-Komkowska, E. Conventional and Real-Time PCR Targeting blaOXA Genes as Reliable Methods for a Rapid Detection of Carbapenem-Resistant Acinetobacter baumannii Clinical Strains. Antibiotics 2022, 11, 455. https://doi.org/10.3390/antibiotics11040455
Depka D, Mikucka A, Bogiel T, Rzepka M, Zawadka P, Gospodarek-Komkowska E. Conventional and Real-Time PCR Targeting blaOXA Genes as Reliable Methods for a Rapid Detection of Carbapenem-Resistant Acinetobacter baumannii Clinical Strains. Antibiotics. 2022; 11(4):455. https://doi.org/10.3390/antibiotics11040455
Chicago/Turabian StyleDepka, Dagmara, Agnieszka Mikucka, Tomasz Bogiel, Mateusz Rzepka, Patryk Zawadka, and Eugenia Gospodarek-Komkowska. 2022. "Conventional and Real-Time PCR Targeting blaOXA Genes as Reliable Methods for a Rapid Detection of Carbapenem-Resistant Acinetobacter baumannii Clinical Strains" Antibiotics 11, no. 4: 455. https://doi.org/10.3390/antibiotics11040455
APA StyleDepka, D., Mikucka, A., Bogiel, T., Rzepka, M., Zawadka, P., & Gospodarek-Komkowska, E. (2022). Conventional and Real-Time PCR Targeting blaOXA Genes as Reliable Methods for a Rapid Detection of Carbapenem-Resistant Acinetobacter baumannii Clinical Strains. Antibiotics, 11(4), 455. https://doi.org/10.3390/antibiotics11040455







