Abstract
Rapid, accurate detection of Clostridioides difficile toxin may potentially be predicted by toxin B PCR cycle threshold (tcdB Ct). We investigated the validity of this approach in an inpatient adult population. Patients who tested positive by C. difficile PCR (Cepheid GeneXpert) from December 2016 to October 2020 (n = 368) at a tertiary medical center were included. All stool samples were further tested by rapid glutamate dehydrogenase (GDH)/toxin B EIA and cell cytotoxin neutralization assay (CCNA). Receiver operating characteristic curves were analyzed. The area under the curve for tcdB Ct predicting toxin result by EIA was 0.795 (95% confidence interval (CI) 0.747–0.843) and by CCNA was 0.771 (95% CI 0.720–0.822). The Youden Ct cutoff for CCNA was ≤27.8 cycles (sensitivity 65.0%, specificity 77.2%). For specimens with Ct ≤ 25.0 cycles (n = 115), CCNA toxin was positive in >90%. The negative predictive value of tcdB Ct for CCNA was no greater than 80% regardless of cutoff chosen. In summary, very low Ct values (≤25.0) could have limited value as a rapid indicator of positive toxin status by CCNA in our patient population. A broad distribution of Ct values for toxin-negative and toxin-positive specimens precluded more robust prediction. Additional data are needed before broader application of Ct values from qualitatively designed assays to clinical laboratory reporting.
1. Introduction
Clostridioides difficile is an anaerobic, spore-forming Gram-positive bacillus and one of the most commonly reported pathogens in health care-associated infections [1]. In the context of a perturbed fecal microbiota, C. difficile causes disease via toxin production, leading to intestinal mucosal damage. Major risk factors for disease include prior antibiotic usage, older age, and healthcare exposure. The spectrum of disease ranges from diarrhea to pseudomembranous colitis and toxic megacolon. Both toxins A and B are produced by most pathogenic strains, but toxin B is detected in nearly all cases of C. difficile disease. Diagnosis is based upon the clinical suspicion and detection of toxigenic C. difficile or its toxins in stool [2].
The rapid, accurate diagnosis of C. difficile infection (CDI) is not yet fully optimized, but toxin detection may be considered the strongest correlate with clinical outcomes [3]. Methods to detect toxin B in stool include enzyme immunoassay (EIA), which has variable levels of performance [2,4], and cell culture cytotoxicity neutralization assay (CCNA). The detection of toxins correlates with disease severity [5], and CCNA results have been shown to correlate most closely with CDI compared to EIA-based toxin assays and toxigenic culture [3]. However, as CCNA is a time-consuming, with a manual method that requires up to 72 h for final results, surrogate methods have been put forth to hasten the time to an accurate toxicology result.
It has been demonstrated that the bacterial load of toxigenic C. difficile in stool correlates with the detection of toxins, with higher bacterial loads observed in specimens that test toxin-positive than those that test toxin-negative [6,7]. Several studies have therefore evaluated the cycle threshold (Ct) from real-time PCR amplification of C. difficile tcdB from stool as a potentially rapid predictor of toxin status [6,7,8,9]. In our clinical experience, toxin EIA has performed poorly compared to CCNA [10], and we have not observed an obvious correlation between tcdB Ct and toxin status. It was therefore suspected that the predictive ability of tcdB Ct values may not be broadly applicable to different toxin assays or patient populations. The objective of this study was to investigate the potential use of tcdB Ct values in a hospitalized adult population for predicting toxin status by either toxin EIA or CCNA.
2. Results
2.1. Patient Demographics
Of 370 PCR-positive samples from hospitalized inpatients, 2 were excluded because CCNA was not performed due to lab error. The remaining 368 samples were from 191 (51.9%) male and 177 (48.1%) female patients (Table S1). Mean and median ages were 58.7 and 62.0 years, respectively. Reasons for admission were largely related to patient history of solid organ transplant (n = 64 (17.4%)), hematopoietic stem cell transplant (n = 23 (6.3%)), malignancy (n = 105 (28.5%)), and surgical procedures (n = 97 (20.4%)). Underlying conditions of all patients are summarized in Table 1.

Table 1.
Underlying medical conditions of hospitalized adult patients with positive C. difficile PCR included in this study.
2.2. Summary Statistics
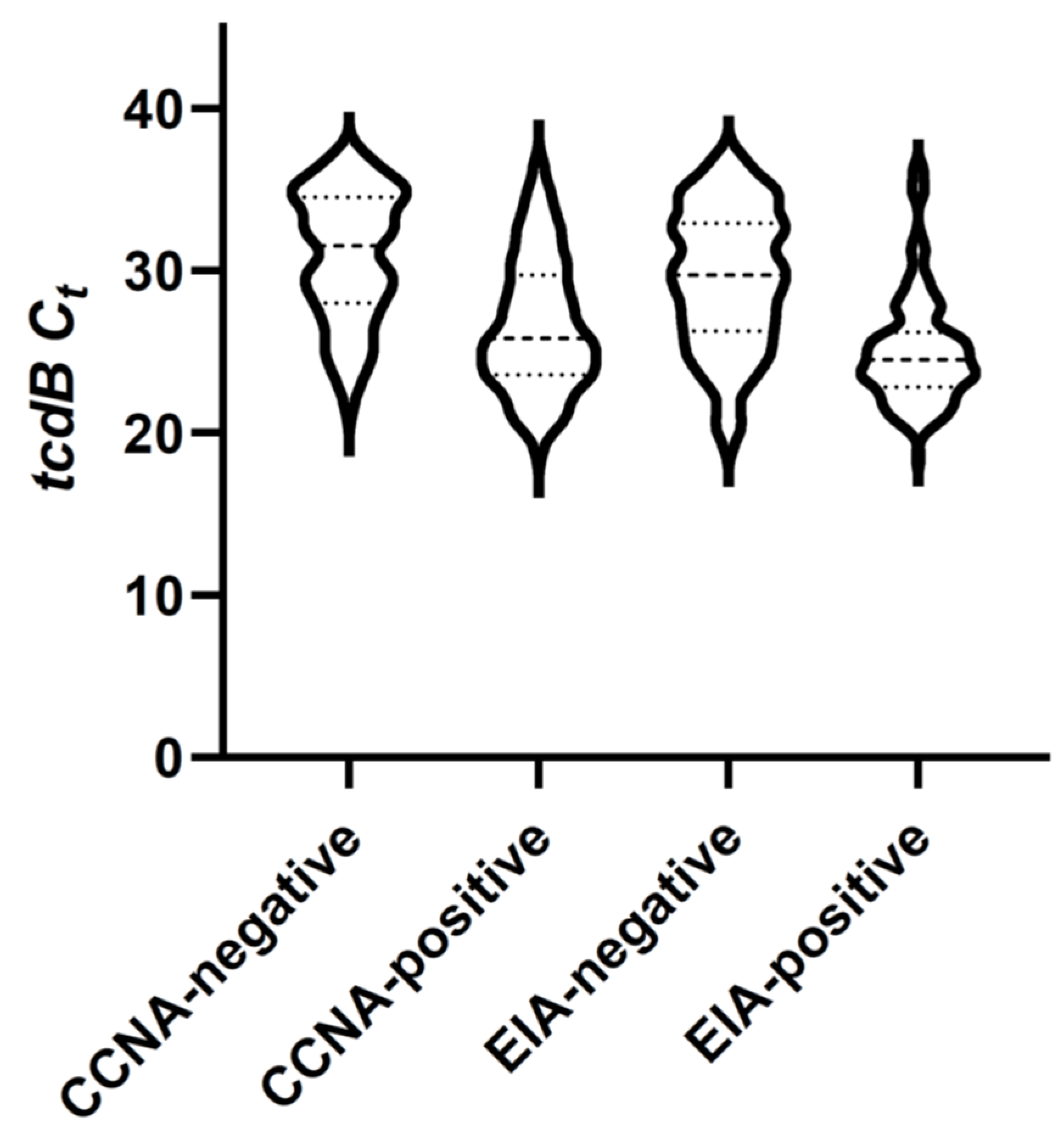
Out of the 368 toxigenic C. difficile PCR-positive specimens, 326 (88.6%) tested positive by GDH EIA, 127 (34.5%) by toxin EIA, and 254 (69.0%) by CCNA. Compared to CCNA as the reference standard, toxin EIA had a sensitivity of 48.4% (123/254; 95% confidence interval (CI) 42.1–54.8%) and specificity of 96.5% (110/114; 95% CI 91.3–99.0%). The tcdB Ct values of the toxin EIA-positive, CCNA-negative specimens ranged from 26.1 to 35.0. Distribution of results demonstrated CCNA toxin-positive specimens to have a more gradual decline in numbers as Ct values increased, compared to toxin EIA-positive samples which demonstrated a denser clustering at lower Ct values (Figure 1).
Figure 1.
Box and violin plot shows distributions of tcdB Ct values according to toxin test results. Minimum, maximum, median (large dashed line), and 25th and 75th percentiles (small dashed lines) are indicated. Observed frequencies of values are represented by width of the plot interval.
2.3. Cycle Threshold Value and GDH, Toxin EIA, and CCNA Results
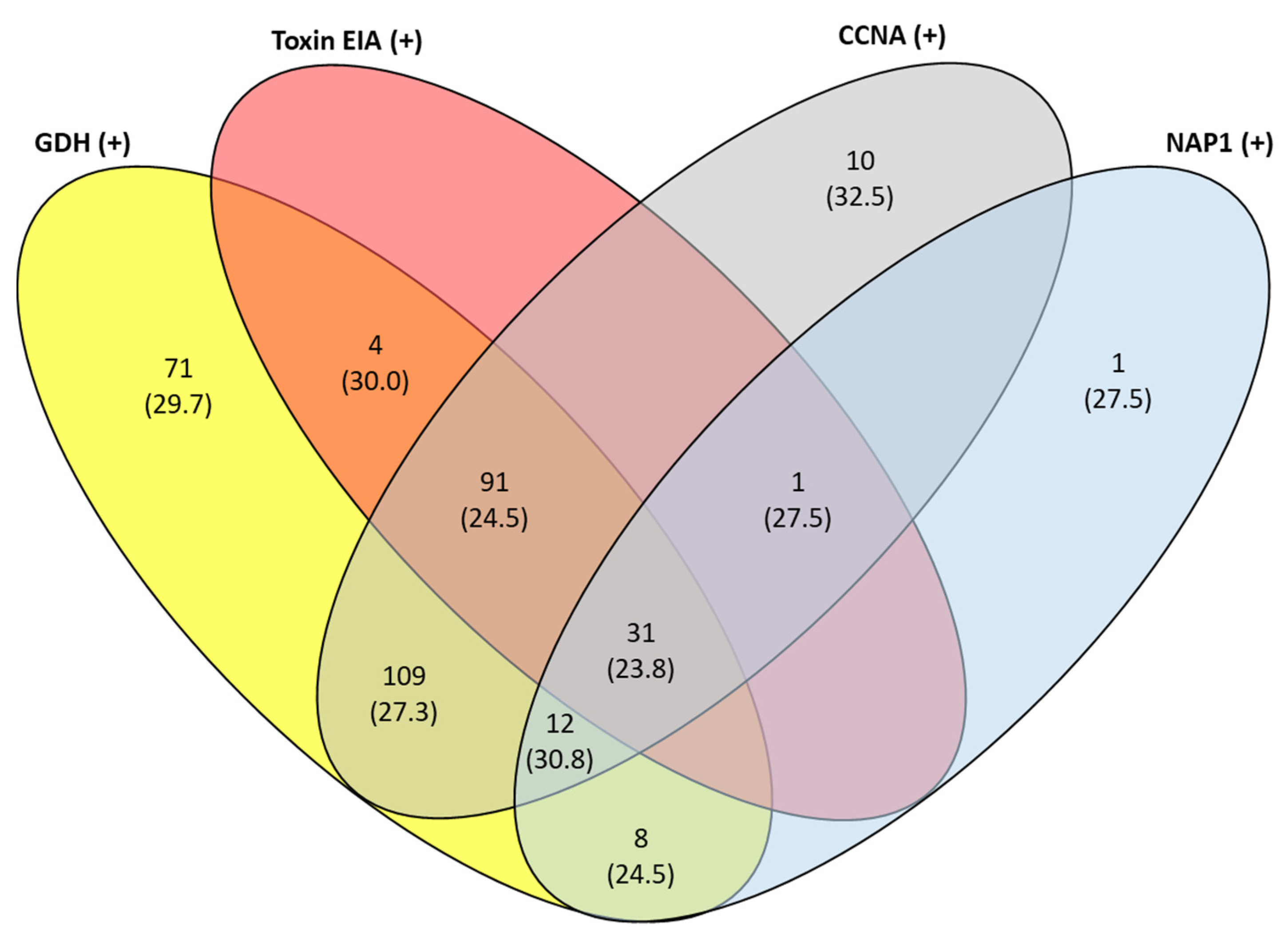
The tcdB Ct values were significantly higher for GDH-negative than GDH-positive samples, toxin EIA-negative than toxin EIA-positive samples, CCNA-negative than CCNA-positive samples, and EIA-positive than CCNA-positive samples. There was no statistically significant difference between NAP1-negative and NAP1-presumptive positive samples (Table 2, Figure 2). However, NAP1-presumptive positive specimens were significantly more frequently EIA-positive (31/53; 58.5%) than NAP1-presumptive negative specimens (95/315; 30.2%) (p = 0.0001); and more frequently CCNA-positive (44/53; 83.0%) than NAP-1 presumptive negative specimens (210/315; 66.7%) (p = 0.016).

Table 2.
Summary statistics of Ct values for tcdB by GDH EIA, toxin EIA, CCNA, and PCR NAP1 results.
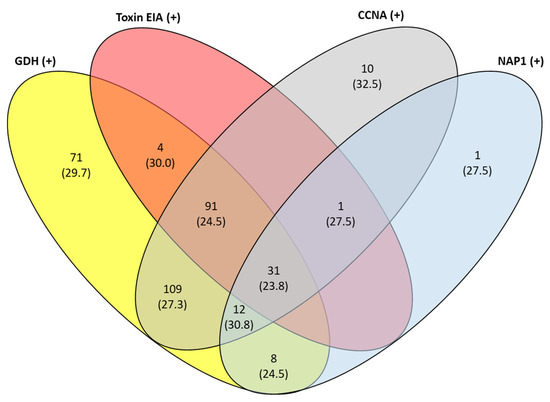
Figure 2.
Venn diagram illustrates the number of specimens with each different test result combination, given as n (median tcdB Ct value). Abbreviations: Ct, threshold cycle; GDH, glutamate dehydrogenase; EIA, enzyme immunoassay; CCNA, cell culture cytotoxicity neutralization assay; NAP1, North American PFGE type 1.
2.4. Use of tcdB Ct Value as an Indicator of Toxin Results
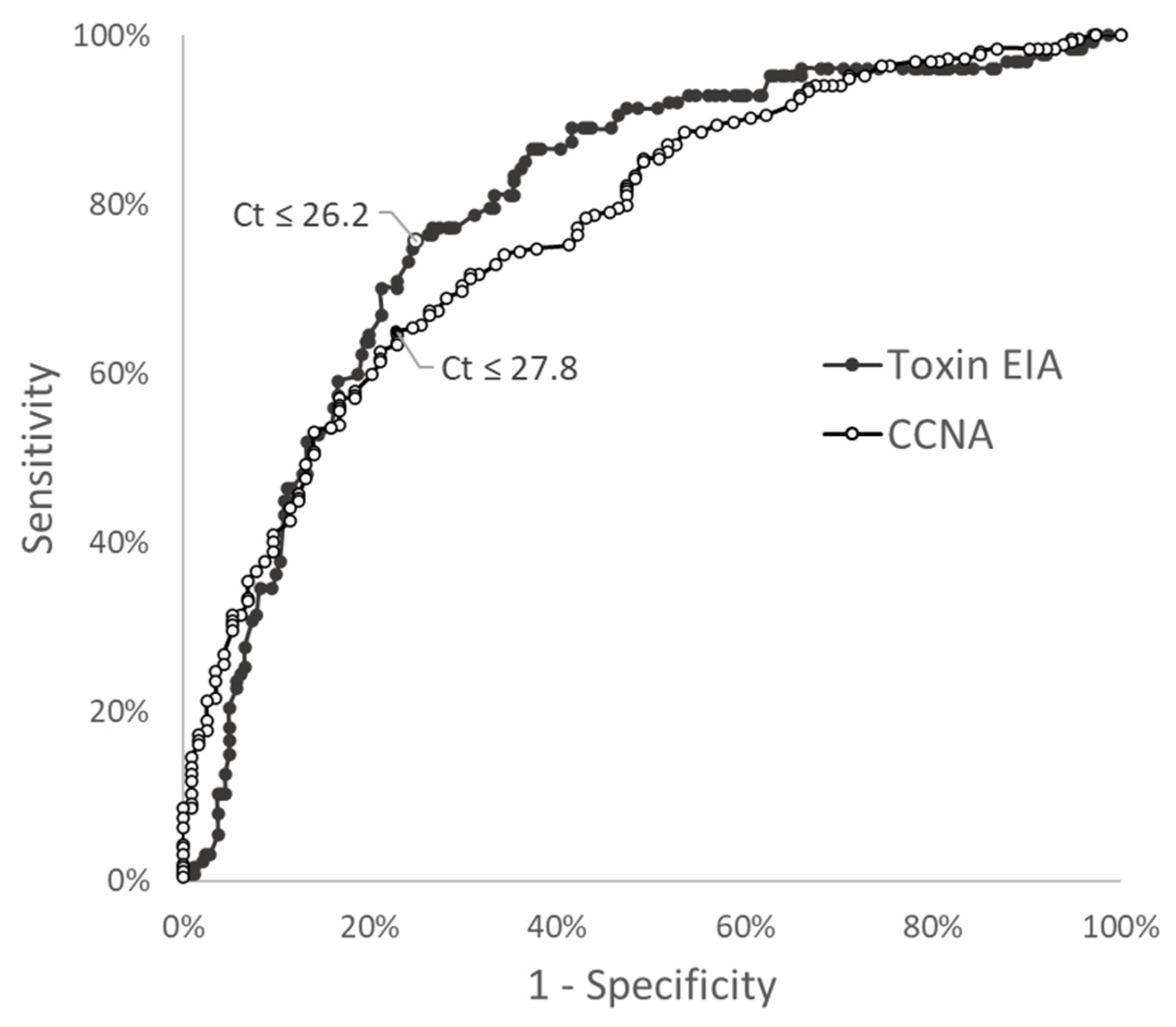
An ROC curve analysis of tcdB Ct values to predict toxin EIA results yielded an AUC of 0.795 (95% CI 0.747–0.843) (Figure 3). The Youden Ct cutoff of ≤26.2 cycles had a sensitivity of 75.6% (95% CI 67.4–82.2%) and specificity of 75.1% (95% CI 69.2–80.1%). The ROC curve for tcdB Ct values to predict CCNA toxin result yielded an AUC of 0.771 (95% CI 0.720–0.822) (Figure 3). The Youden Ct cutoff of ≤27.8 cycles had a sensitivity of 65.0% (95% CI 58.9–70.6%) and specificity of 77.2% (95% CI 68.7–83.9%). To account for the rapid turnaround time and accuracy of toxin EIA-positive results, we performed a subset analysis on toxin EIA-negative specimens, for which CCNA toxin results were potentially more applicable. In toxin EIA-negative specimens, the AUC was 0.677 (95% CI 0.610–0.745).
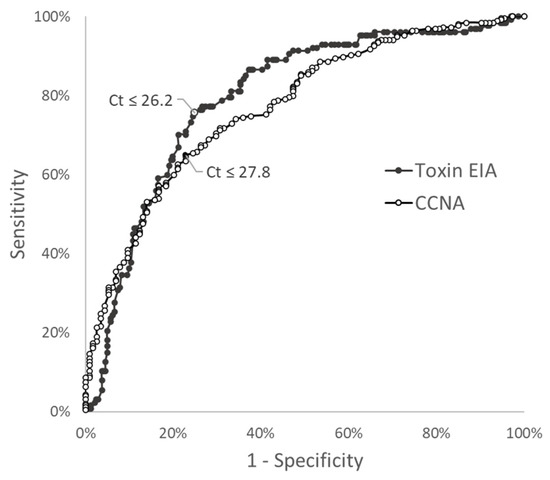
Figure 3.
Receiver operating characteristic (ROC) curve for tcdB Ct value predicting EIA toxin status (AUC = 0.795), or CCNA toxin status (AUC = 0.771). Youden cutoffs are indicated on each curve with their corresponding Ct value cutoffs.
When examining the positive predictive value of tcdB Ct for CCNA toxin results by Ct value, we found that tcdB Ct ≤ 21.3 cycles was the highest cutoff at which positive toxin detection by CCNA could be predicted with 100% accuracy (n = 22). A cutoff of Ct ≤ 25.0 cycles was the highest at which >90.0% (104/115) of such specimens tested positive for toxin by CCNA. No meaningful ≥ Ct cutoff could predict negative CCNA toxin results beyond 80% accuracy. Even at a cutoff of ≥35.4 cycles, 4 of 19 (21.1%) specimens still tested CCNA-positive.
3. Discussion
Our analysis of data from a recent four-year period sought to characterize the predictive value of the tcdB Ct value for C. difficile toxin status in PCR-positive fecal specimens in an adult inpatient population. Our findings could be relevant to institutions considering the use of algorithmic or combination testing for C. difficile by toxin assays and PCR, particularly as we correlated PCR Ct values with CCNA, a reference standard toxin assay [11,12]. The rapid toxin EIA test used here can provide results within minutes, negating much of the benefit of using for Ct value from PCR to predict its results. Conversely, the low sensitivity for C. difficile toxin B by EIA compared to CCNA (48.4% in this study) limits its utility as a rapid toxin assay. Furthermore, use of the tcdB Ct value to predict toxin results obtained by CCNA could be considered more impactful given that CCNA toxin results have been shown to correspond with C. difficile disease severity [2,5], and that tcdB Ct values are obtained at the time of real-time PCR but CCNA requires 1 to 3 days.
In this study, tcdB Ct values yielded similar AUCs for toxin results by EIA and CCNA, and it was shown that using tcdB Ct value as predictor of toxin results yielded suboptimal sensitivity and specificity (~75%) at the optimal cutoffs. Selecting a separate cutoff tcdB Ct value for positive and negative toxin results by CCNA offered some advantages, albeit limited. Although a cutoff of Ct ≤ 25.0 cycles could predict positive CCNA results for a specimen with >90% accuracy, more than half of CCNA-positive specimens actually had Ct numbers >25.0. In our analysis, there no practical tcdB Ct cutoff value was found that reliably corresponded to CCNA-negative results given the wide and even distribution of CCNA-positive specimens across Ct values.
Of note, other studies evaluating the ability of tcdB Ct results to predict toxin status showed better performance than found here. An AUC as high as 0.921 for predicting combined results of toxin testing by EIA and CCNA using the Xpert assay, quantitatively calibrated to tcdB target concentrations, has been demonstrated (7). A sensitivity of 99.0% for rapid EIA toxin detection was attained with a tcdB Ct cutoff of <27.55 (Xpert), although the corresponding specificity was 58.8% [8]. It is noteworthy that in these two aforementioned studies, toxigenic bacterial load clustered tightly according to toxin test result, in contrast to our tcdB Ct results, which were much more broadly distributed. Similar to our study, another study evaluating Xpert PCR results from a 6-year period described significant overlap of Ct values between EIA toxin-positive and -negative specimens [13]. We can only speculate that differences in Ct value distribution seen between studies could have resulted from studies of longer study periods capturing more variation in test operators and assay lot-to-lot differences. Discrepancies in performance characteristics for the same C. difficile toxin and PCR assays have furthermore been observed to occur between different geographic sites and strain types [2,14,15], potentially contributing to our observed results. The low sensitivity of the rapid GDH/toxin combination at our institution is described in other studies, though it contrasts with the performance found by others [10,16,17,18,19], a trend which remained consistent throughout this four-year study period. Our results were similar to those described in a cancer center patient population, in which an AUC of 0.83 was obtained with a Youden cutoff of ≤28.0 cycles (vs. our Youden cutoff of ≤27.8 cycles) for the prediction of CCNA toxin results. Overlapping distributions of Ct values of 25.0–28.0 were also noted between CCNA-negative and CCNA-positive cases in another comparison [20]. Although others have not found adverse outcomes associated with the implementation of reporting tcdB Ct values [21], it is important to note that test performance characteristics may differ by institution.
These studies demonstrate the potential applications of Ct values from the typically qualitative C. difficile PCR. The Xpert assay is generally considered to have excellent sensitivity in organism detection and specificity in ruling out CDI, similar to that of other commercial C. difficle PCR assays [22,23]. It is stressed that such application of Ct values is not FDA-cleared for C. difficile PCR testing, including the commonly used Xpert assay. Test cartridges are inoculated with a swab dipped into the fecal specimen; hence, the starting material is a non-standard, non-quantified amount. Quantitative results could further be subject to variations in operator technique, stool consistency, and DNA recovery, among other factors. To the contrary, one study found that variations in stool input volume had little bearing on the Ct value, and moreover, the coefficient of variation for the tcdB Ct was only 2.8% across four lots of the Xpert assay [8]. In additional support of the potential quantitative use of C. difficile PCR results, Ct values were found to significantly correlate with quantitative culture results for C. difficile in stool [6]. In our retrospective analysis of clinical test results, we did not calibrate Ct against a standard curve to mitigate any lot-to-lot variation over the study period. In order for Ct values for qualitative tests to offer maximal performance as a toxin prediction tool for clinical purposes, we believe the test should be managed in the laboratory as a quantitative, laboratory-developed test. Our study results otherwise advise against use of the Ct result at face value for clinical purposes.
In addition to predicting toxin status, the bacterial load of toxigenic C. difficile in stool has been proposed as a predictor of CDI severity and clinical outcome [9,23,24]. However, the actual value of its prognostic contribution, as compared to the information derived from toxin testing and assessment of clinical risk factors, has been questioned [24]. With different case definitions and specimen inclusion criteria between different studies, optimal cutoffs for tcdB Ct values from the Xpert platform have ranged from <23.5 to <27.55 for predicting poor outcomes for CDI [9,19,24,25,26,27]. Incorporating expert clinical consensus, a more recent study found a threshold of <24.0 cycles on the Xpert assay corresponded with a high probability of CDI [28].
Gene targets of the Xpert C. difficile PCR assay include binary toxin and tcdC deletion for presumptive detection of the NAP1 strain. Outside the epidemic setting, the clinical significance of the NAP1 strain is variable, with some studies noting increased associated CDI severity and mortality but others finding host factors to be more contributory to outcome than strain type [29,30,31]. In either case, NAP1 strains are known to produce higher levels of toxin A and B in vitro and in vivo [31,32]. Similar to others [7,24], this study observed a trend (p = 0.056) towards lower Ct values for presumptive NAP1 strains and higher frequency of toxin positivity by either EIA or CCNA compared to NAP1-negative specimens. These results were from a single center among adult inpatients, and the results may not be generalizable to other patient populations. CCNA testing was performed by a reference laboratory within specimen stability limits, rather than immediately set up for in-house testing, which may have had a minor impact on CCNA results. Another consideration is that only Bristol scale 6 or 7 stools were included for clinical testing to improve appropriate test utilization, although this restriction may have excluded some cases of CDI [33,34]. Because our purpose was to analyze the practical implications of using Ct as a simple indicator of toxin status, wherein the clinical laboratory would operate within its current test algorithm, we did not further stratify patients using clinical severity scores or other clinical variables to improve the predictive power of the tcdB Ct value for CCNA toxin status. This remains an important consideration to be further explored in the future.
In summary, we found that the use of tcdB Ct values from a commonly used C. difficile PCR platform was limited in its ability to predict CCNA toxin status. The difficulty was related to the broad distribution of tcdB Ct values observed in the study period, even among CCNA-positive specimens. Our data were compiled from several years of clinical testing and found that results were not as robust and reliable compared to focused studies occurring over a short period of time or those using calibrated assays.
4. Materials and Methods
4.1. Specimen Inclusion Criteria
In this retrospective analysis, we included the clinical results of all stool samples from hospitalized adult patients that had undergone C. difficile testing by EIA and CCNA (detailed below) after testing positive for C. difficile toxin gene tcdB by real-time PCR (GeneXpert C. difficile/Epi PCR, Cepheid, Sunnyvale, CA, USA), which, at the time of study, was from December 2016 to October 2020. The patients were from a tertiary care center specializing in surgical, transplant, and oncology care (Keck Medical Center, Los Angeles, CA, USA). Per institutional policy, specimens were rejected if not meeting Bristol stool scale type 6 or 7 or if a prior specimen had been tested from the same patient within the past 7-day period.
4.2. Data Collection and C. difficile Test Methods
C. difficile PCR testing was performed upon physician’s request based on clinical suspicion. C. difficile testing is performed promptly upon receipt by the laboratory. For hospitalized patients, standard-of-care testing for specimens positive by C. difficile PCR included immediate testing by a rapid EIA assay for glutamate dehydrogenase (GDH) and toxin B (Cdiff Quick Check, Alere Inc., Waltham, MA, USA), and immediately freezing an aliquot and sending it for CCNA testing at a reference laboratory (ARUP Laboratories, Salt Lake City, UT, USA). C. difficile test results by PCR, EIA, and CCNA, as well as tcdB Ct values and NAP1 results from the Xpert PCR assay, were retrospectively collected for this study. Electronic medical records were reviewed for patient demographics and underlying health conditions.
4.3. Statistical Analysis
Mean ranks of tcdB Ct values between groups were compared using the Mann–Whitney U test. Frequency of categorical variables between groups were compared using two-tailed Fisher’s exact test. Receiver operating characteristic (ROC) curve analysis was performed using Ct values as a marker of toxin positivity by either EIA or CCNA. The area under the curve (AUC) for each toxin test was calculated and compared using the Wilcoxon trapezoidal method. The optimal Ct cutoff value was determined using the Youden maximum index value. Statistical calculations were conducted using GraphPad Prism 9.0.0 (San Diego, CA, USA).
5. Conclusions
The application of tcdB Ct values from C. difficile PCR in a tertiary care, adult inpatient population was suboptimal as a predictive tool to determine C. difficile toxin status by the reference cytotoxin neutralization assay or by enzyme immunoassay. Substantial overlap of tcdB Ct values between toxin-negative and toxin-positive specimens precluded more accurate prediction.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/antibiotics11050576/s1, Table S1: Case summaries and results.
Author Contributions
Conceptualization, R.C.S. and N.N.; methodology, R.C.S.; software, S.L. and Y.L.; formal analysis, S.L. and Y.L.; investigation, S.L. and K.Y.; data curation, K.Y.; writing, R.C.S.; writing—review and editing, N.N.; supervision, R.C.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of University of Southern California (Protocol HS-16-00402, approved July 2016).
Informed Consent Statement
Patient consent was waived due to the study involving no more than minimal risk to subjects and the determination that the waiver would not adversely affect the rights and welfare of subjects.
Data Availability Statement
The data presented in this study are available in the Supplementary Materials.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Magill, S.S.; Edwards, J.R.; Bamberg, W.; Beldavs, Z.G.; Dumyati, G.; Kainer, M.A.; Lynfield, R.; Maloney, M.; McAllister-Hollod, L.; Nadle, J.; et al. Multistate point-prevalence survey of health care-associated infections. N. Engl. J. Med. 2014, 370, 1198–1208. [Google Scholar] [CrossRef] [PubMed]
- Van Prehn, J.; Reigadas, E.; Vogelzang, E.H.; Bouza, E.; Hristea, A.; Guery, B.; Krutova, M.; Norén, T.; Allerberger, F.; Coia, J.; et al. European Society of Clinical Microbiology and Infectious Diseases: 2021 update on the treatment guidance document for Clostridioides difficile infection in adults. Clin. Microbiol. Infect. 2021, 27 (Suppl. S2), S1–S21. [Google Scholar] [CrossRef] [PubMed]
- Planche, T.D.; Davies, K.A.; Coen, P.G.; Finney, J.M.; Monahan, I.M.; Morris, K.A.; O’Connor, L.; Oakley, S.J.; Pope, C.F.; Wren, M.W.; et al. Differences in outcome according to Clostridium difficile testing method: A prospective multicentre diagnostic validation study of C difficile infection. Lancet Infect. Dis. 2013, 13, 936–945. [Google Scholar] [CrossRef]
- Planche, T.; Aghaizu, A.; Holliman, R.; Riley, P.; Poloniecki, J.; Breathnach, A.; Krishna, S. Diagnosis of Clostridium difficile in-fection by toxin detection kits: A systematic review. Lancet Infect. Dis. 2008, 8, 777–784. [Google Scholar] [CrossRef]
- Longtin, Y.; Trottier, S.; Brochu, G.; Paquet-Bolduc, B.; Garenc, C.; Loungnarath, V.; Beaulieu, C.; Goulet, D.; Longtin, J. Impact of the Type of Diagnostic Assay on Clostridium difficile Infection and Complication Rates in a Mandatory Reporting Program. Clin. Infect. Dis. 2012, 56, 67–73. [Google Scholar] [CrossRef]
- Dionne, L.L.; Raymond, F.; Corbeil, J.; Longtin, J.; Gervais, P.; Longtin, Y. Correlation between Clostridium difficile bacterial load, commercial real-time PCR cycle thresholds, and results of diagnostic tests based on enzyme immunoassay and cell culture cytotoxicity assay. J. Clin. Microbiol. 2013, 51, 3624–3630. [Google Scholar] [CrossRef]
- Leslie, J.L.; Cohen, S.H.; Solnick, J.V.; Polage, C.R. Role of fecal Clostridium difficile load in discrepancies between toxin tests and PCR: Is quantitation the next step in C. difficile testing? Eur. J. Clin. Microbiol. Infect. Dis. 2012, 31, 3295–3299. [Google Scholar] [CrossRef]
- Senchyna, F.; Gaur, R.L.; Gombar, S.; Truong, C.Y.; Schroeder, L.F.; Banaei, N. Clostridium difficile PCR Cycle Threshold Predicts Free Toxin. J. Clin. Microbiol. 2017, 55, 2651–2660. [Google Scholar] [CrossRef]
- Kamboj, M.; Brite, J.; McMillen, T.; Robilotti, E.; Herrera, A.; Sepkowitz, K.; Babady, N.E. Potential of real-time PCR threshold cycle (C(T)) to predict presence of free toxin and clinically relevant C. difficile infection (CDI) in patients with cancer. J. Infect. 2018, 76, 369–375. [Google Scholar] [CrossRef]
- Ashraf, Z.; Rahmati, E.; Bender, J.M.; Nanda, N.; She, R.C. GDH and toxin immunoassay for the diagnosis of Clostridioides (Clostridium) difficile infection is not a ‘one size fit all’ screening test. Diagn. Microbiol. Infect. Dis. 2018, 94, 109–112. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Short Summary: Testing for C. difficile and Standardized Infection Ratios, National Healthcare Safety Network. 2019. Available online: https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/Cdiff-testing-sir-508.pdf (accessed on 24 February 2022).
- Bagdasarian, N.; Rao, K.; Malani, P.N. Diagnosis and treatment of Clostridium difficile in adults: A systematic review. JAMA 2015, 313, 398–408. [Google Scholar] [CrossRef] [PubMed]
- Wilmore, S.; Goldenberg, S.D. Potential of real-time PCR threshold cycle (CT) to predict presence of free toxin and clinically relevant C. difficile infection (CDI) in patients with cancer: A reply. J. Infect. 2018, 76, 424–426. [Google Scholar] [CrossRef] [PubMed]
- Tenover, F.C.; Novak-Weekley, S.; Woods, C.W.; Peterson, L.R.; Davis, T.; Schreckenberger, P.; Fang, F.C.; Dascal, A.; Gerding, D.N.; Nomura, J.H.; et al. Impact of Strain Type on Detection of Toxigenic Clostridium difficile: Comparison of Molecular Diagnostic and Enzyme Immunoassay Approaches. J. Clin. Microbiol. 2010, 48, 3719–3724. [Google Scholar] [CrossRef] [PubMed]
- Rizzardi, K.; Åkerlund, T.; Norén, T.; Matussek, A. Impact of ribotype on Clostridioides difficile diagnostics. Eur. J. Clin. Microbiol. 2020, 39, 847–853. [Google Scholar] [CrossRef] [PubMed]
- Quinn, C.D.; Sefers, S.E.; Babiker, W.; He, Y.; Alcabasa, R.; Stratton, C.W.; Carroll, K.C.; Tang, Y.-W.C. Diff Quik Chek Complete Enzyme Immunoassay Provides a Reliable First-Line Method for Detection of Clostridium difficile in Stool Specimens. J. Clin. Microbiol. 2010, 48, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Chung, H.-S.; Lee, M. Evaluation of the performance of C. DIFF QUIK CHEK COMPLETE and its usefulness in a hospital setting with a high prevalence of Clostridium difficile infection. J. Investig. Med. 2017, 65, 88–92. [Google Scholar] [CrossRef]
- Larson, A.M.; Fung, A.M.; Fang, F.C. Evaluation of tcdB Real-Time PCR in a Three-Step Diagnostic Algorithm for Detection of Toxigenic Clostridium difficile. J. Clin. Microbiol. 2010, 48, 124–130. [Google Scholar] [CrossRef]
- Gomez, E.J.; Montgomery, S.; Alby, K.; Robinson, D.P.; Roundtree, S.S.; Blecker-Shelly, D.; Sullivan, K.V. Poor yield of Clostridium difficile testing algorithms using glutamate dehydrogenase antigen and C. difficile toxin enzyme immunoassays in a pediatric population with declining prevalence of clostridium difficile strain BI/NAP1/027. Diagn. Microbiol. Infect. Dis. 2018, 91, 229–232. [Google Scholar] [CrossRef]
- Shah, M.D.; Balada-Llasat, J.-M.; Coe, K.; Reed, E.; Sandlund, J.; Pancholi, P. Evaluation of Cycle Threshold, Toxin Concentration, and Clinical Characteristics of Clostridioides difficile Infection in Patients with Discordant Diagnostic Test Results. J. Clin. Microbiol. 2020, 58, e01681-19. [Google Scholar] [CrossRef]
- Hitchcock, M.M.; Holubar, M.; Hogan, C.A.; Tompkins, L.S.; Banaei, N. Dual Reporting of Clostridioides difficile PCR and Pre-dicted Toxin Result Based on PCR Cycle Threshold Reduces Treatment of Toxin-Negative Patients without Increases in Ad-verse Outcomes. J. Clin. Microbiol. 2019, 57, e01288-19. [Google Scholar] [CrossRef]
- Bai, Y.; Sun, X.; Jin, Y.; Wang, Y.; Li, J. Accuracy of Xpert Clostridium difficile assay for the diagnosis of Clostridium difficile infection: A meta analysis. PLoS ONE 2017, 12, e0185891. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, A.; Pasupuleti, V.; Rolston, D.D.; Jain, A.; Deshpande, N.; Pant, C.; Hernandez, A.V. Diagnostic accuracy of re-al-time polymerase chain reaction in detection of Clostridium difficile in the stool samples of patients with suspected Clostridium difficile Infection: A meta-analysis. Clin. Infect. Dis. 2011, 53, e81–e90. [Google Scholar] [CrossRef] [PubMed]
- Reigadas, E.; Alcalá, L.; Valerio, M.; Marín, M.; Martin, A.; Bouza, E. Toxin B PCR cycle threshold as a predictor of poor out-come of Clostridium difficile infection: A derivation and validation cohort study. J. Antimicrob. Chemother. 2016, 71, 1380–1385. [Google Scholar] [CrossRef]
- De Francesco, M.A.; Lorenzin, G.; Piccinelli, G.; Corbellini, S.; Bonfanti, C.; Caruso, A. Correlation between tcdB gene PCR cycle threshold and severe Clostridium difficile disease. Anaerobe 2019, 59, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Origüen, J.; Orellana, M.Á.; Fernández-Ruiz, M.; Corbella, L.; San Juan, R.; Ruiz-Ruigómez, M.; López-Medrano, F.; Lizasoain, M.; Ruiz-Merlo, T.; Maestro-de la Calle, G.; et al. Toxin B PCR Amplification Cycle Thresh-old Adds Little to Clinical Variables for Predicting Outcomes in Clostridium difficile Infection: A Retrospective Cohort Study. J. Clin. Microbiol. 2019, 57, e01125-18. [Google Scholar] [CrossRef]
- Garvey, M.I.; Bradley, C.W.; Wilkinson, M.A.; Holden, E. Can a toxin gene NAAT be used to predict toxin EIA and the severity of Clostridium difficile infection? Antimicrob. Resist Infect. Control 2017, 6, 127. [Google Scholar] [CrossRef]
- Doolan, C.P.; Louie, T.; Lata, C.; Larios, O.E.; Stokes, W.; Kim, J.; Brown, K.; Beck, P.; Deardon, R.; Pillai, D.R. Latent Class Analysis for the Diagnosis of Clostridioides difficile Infection. Clin. Infect. Dis. 2020, 73, e2673–e2679. [Google Scholar] [CrossRef]
- Scardina, T.; Labuszewski, L.; Pacheco, S.; Adams, W.; Schreckenberger, P.; Johnson, S. Clostridium difficile Infection (CDI) Severity and Outcome among Patients Infected with the NAP1/BI/027 Strain in a Non-Epidemic Setting. Infect. Control Hosp. Epidemiol. 2015, 36, 280–286. [Google Scholar] [CrossRef]
- Katz, K.C.; Golding, G.R.; Choi, K.B.; Pelude, L.; Amaratunga, K.R.; Taljaard, M.; Alexandre, S.; Collet, J.C.; Davis, I.; Du, T.; et al. The evolving epidemiology of Clostridium difficile infection in Canadian hospitals during a postepidemic period (2009–2015). Can. Med Assoc. J. 2018, 190, E758–E765. [Google Scholar] [CrossRef]
- Sirard, S.; Valiquette, L.; Fortier, L.-C. Lack of Association between Clinical Outcome of Clostridium difficile Infections, Strain Type, and Virulence-Associated Phenotypes. J. Clin. Microbiol. 2011, 49, 4040–4046. [Google Scholar] [CrossRef]
- Warny, M.; Pepin, J.; Fang, A.; Killgore, G.; Thompson, A.; Brazier, J.; Frost, E.; McDonald, L.C. Toxin production by an emerging strain of Clostridium difficile associated with outbreaks of severe disease in North America and Europe. Lancet 2005, 366, 1079–1084. [Google Scholar] [CrossRef]
- Kwon, J.H.; Reske, K.A.; Hink, T.; Burnham, C.-A.D.; Dubberke, E.R. Evaluation of Correlation between Pretest Probability for Clostridium difficile Infection and Clostridium difficile Enzyme Immunoassay Results. J. Clin. Microbiol. 2017, 55, 596–605. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Caroff, D.A.; Edelstein, P.H.; Hamilton, K.; Pegues, D.A.; CDC Prevention Epicenters Program. The Bristol Stool Scale and Its Relationship to Clostridium difficile Infection. J. Clin. Microbiol. 2014, 52, 3437–3439. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).