Search for Indexes to Evaluate Trends in Antibiotic Use in the Sub-Prefectural Regions Using the National Database of Health Insurance Claims and Specific Health Checkups of Japan
Abstract
:1. Introduction
2. Methods and Materials
2.1. Study Design
| Classification *1 | Secondary Medical Area | Populations *2 | Number of Hospitals *3 | Number of Clinics *3 |
|---|---|---|---|---|
| Big city | Kyoto-Otokuni | 1,555,461 | 106 | 1717 |
| Small city-1 | Yamashiro-kita | 433,858 | 23 | 303 |
| Small city-2 | Chutan | 190,822 | 17 | 162 |
| Small city-3 | Nantan | 132,537 | 10 | 101 |
| Small city-4 | Yamashiro-minami | 123,789 | 3 | 92 |
| Small city-5 | Tango | 94,142 | 6 | 76 |
2.2. Data Source
2.3. Calculation of AMU Based on NDB and Evaluation for Trends of AMU
2.4. Statistical Analysis and Ethical Considerations
3. Result
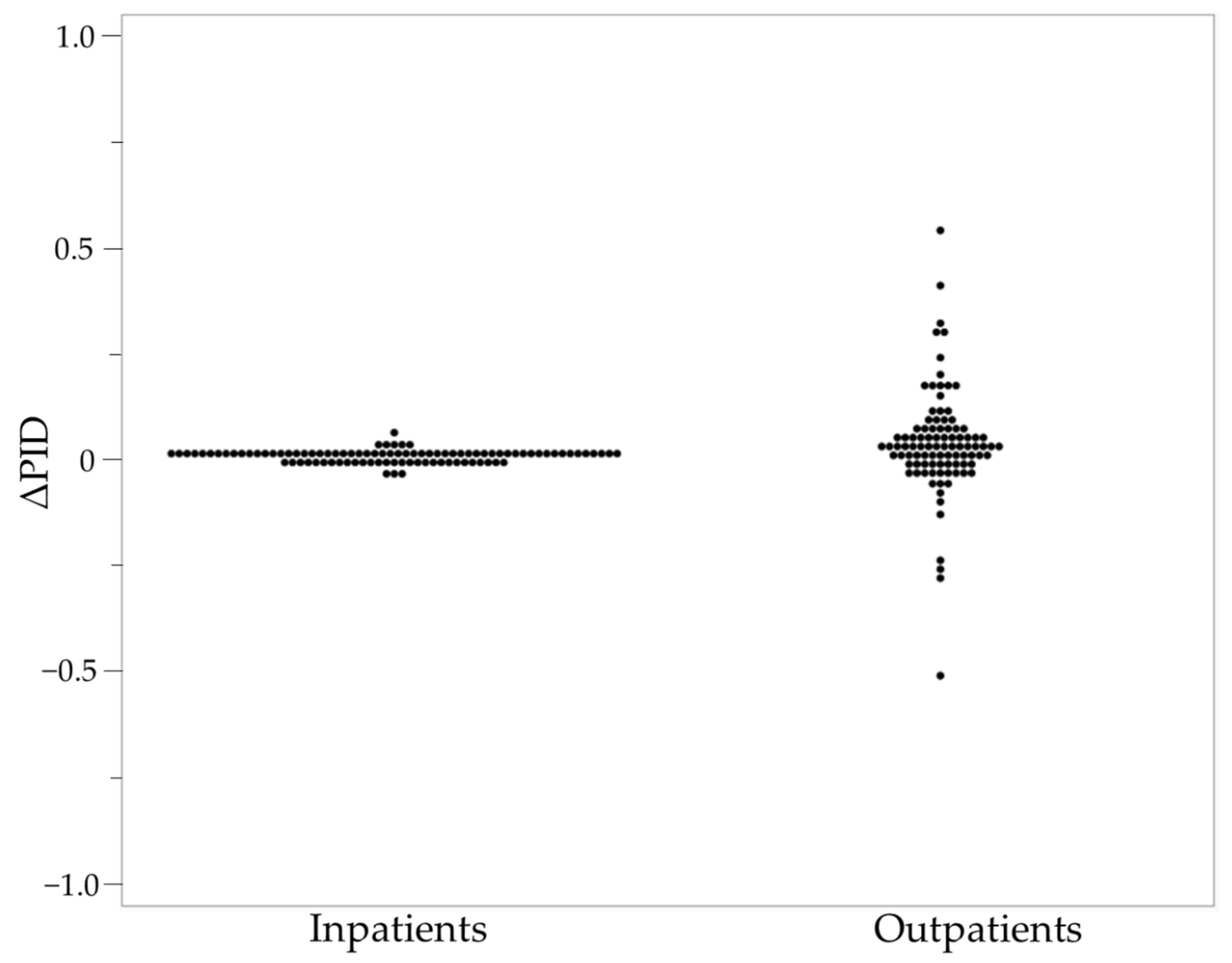
3.1. Trends of AMUs in Secondary Medical Areas in the Kyoto Prefecture from 2013 to 2016
3.2. Relationship between Published Values in Japan or the Kyoto Prefecture and AMU Trends in Each Secondary Medical Area in the Kyoto Prefecture
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bush, K.; Courvalin, P.; Dantas, G.; Davies, J.; Eisenstein, B.; Huovinen, P.; Jacoby, G.A.; Kishony, R.; Kreiswirth, B.N.; Kutter, E.; et al. Tackling antibiotic resistance. Nat. Rev. Microbiol. 2011, 9, 894–896. [Google Scholar] [CrossRef] [PubMed]
- Review on Antimicrobial Resistance, Tackling Drug-Resistant Infections Globally: Final Report and Recommendations (May 2016). Available online: https://amr-review.org/sites/default/files/160518_Final%20paper_with%20cover.pdf (accessed on 24 July 2021).
- WHO. Global Action Plan on Antimicrobial Resistance. Available online: https://apps.who.int/iris/bitstream/handle/10665/193736/9789241509763_eng.pdf?sequence=1 (accessed on 7 October 2021).
- Ministry of Health. Labour and Welfare, National Action Plan on Antimicrobial Resistance (AMR) 2016–2020. Available online: https://www.mhlw.go.jp/file/06-Seisakujouhou-10900000-Kenkoukyoku/0000138942.pdf (accessed on 24 July 2021).
- Bell, B.G.; Schellevis, F.; Stobberingh, E.; Goossens, H.; Pringle, M. A systematic review and meta-analysis of the effects of antibiotic consumption on antibiotic resistance. BMC Infect. Dis. 2014, 14, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- AMR Clinical Reference Center. Surveillance of Antibiotic Use by Prefecture and Age Category, Based on Data from the NDB (published on 19 October 2020), Graph 1. Antibiotic use2013–2019(National). Available online: http://amrcrc.ncgm.go.jp/surveillance/010/1_NDB_stats_202010.pdf (accessed on 25 January 2021). (In Japanese).
- Kusama, Y.; Ishikane, M.; Tanaka, C.; Kimura, Y.; Yumura, E.; Hayakawa, K.; Ohmagari, N. Regional Variation of Antimicrobial Use in Japan from 2013–2016, as Estimated by the Sales Data. Jpn. J. Infect. Dis. 2019, 72, 326–329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsutsui, A.; Yahara, K.; Shibayama, K. Trends and patterns of national antimicrobial consumption in Japan from 2004 to 2016. J. Infect. Cfemother. 2018, 24, 414–421. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, H.; Saito, M.; Sato, J.; Goda, K.; Mitsutake, N.; Kitsuregawa, M.; Nagai, R.; Hatakeyama, S. Indications and classes of outpatient antibiotic prescriptions in Japan: A descriptive study using the national database of electronic health insurance claims, 2012–2015. Int. J. Infect. Dis. 2020, 91, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamasaki, D.; Tanabe, M.; Muraki, Y.; Kato, G.; Ohmagari, N.; Yagi, T. The first report of Japanese antimicrobial use measured by national database based on health insurance claims data (2011–2013): Comparison with sales data, and trend analysis stratified by antimicrobial category and age group. Infection 2018, 46, 207–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ministry of Health. Labour and Welfare, Status of Secondary Medical Areas. Available online: https://www.mhlw.go.jp/file/05-Shingikai-10801000-Iseikyoku-Soumuka/0000058300.pdf (accessed on 20 December 2021). (In Japanese)
- Barlam, T.F.; Cosgrove, S.E.; Abbo, L.M.; MacDougall, C.; Schuetz, A.N.; Septimus, E.J.; Srinivasan, A.; Dellit, T.H.; Falck-Ytter, Y.T.; Fishman, N.O.; et al. Implementing an antibiotic stewardship program: Guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin. Infect. Dis. 2016, 62, 51–77. [Google Scholar] [CrossRef] [PubMed]
- Mita, Y.; Inose, R.; Goto, R.; Kusama, Y.; Koizumi, R.; Yamasaki, D.; Ishikane, M.; Tanabe, M.; Ohmagari, N.; Muraki, Y. An alternative index for evaluating AMU and anti-methicillin-resistant Staphylococcus aureus agent use: A study based on the National Database of Health Insurance Claims and Specific Health Checkups data of Japan. J. Infect. Chemother. 2021, 27, 972–976. [Google Scholar] [CrossRef] [PubMed]
- Statistics Bureau of Japan. I Daytime Population. Available online: https://www.stat.go.jp/english/data/kokusei/2000/jutsu1/00/01.html (accessed on 6 January 2022).
- Koizumi, R.; Kusama, Y.; Muraki, Y.; Ishikane, M.; Yamasaki, D.; Tanabe, M.; Ohmagari, N. Effect of population inflow and outflow between rural and urban areas on regional antimicrobial use surveillance. PLoS ONE 2021, 16, e0248338. [Google Scholar] [CrossRef] [PubMed]
- Council of Local Authorities for International Relations. Local Government in Japan 2016 (2019 Revised Edition). Available online: https://www.soumu.go.jp/main_content/000770124.pdf (accessed on 1 January 2021).
- WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC classification and DDD assignment|2022. Available online: https://www.whocc.no/filearchive/publications/2022_guidelines_web.pdf (accessed on 23 December 2021).
- National Statistics Center. Portal Site of Official Statistics of Japan. Available online: https://www.e-stat.go.jp/en (accessed on 24 July 2021).
- AMR Clinical Reference Center. Surveillance of Antibiotics Use by Prefecture and Age Group Based on the National Database of Health Insurance Claims and Specific Health Checkups (NDB) (published on 30 October 2018). Available online: https://view.officeapps.live.com/op/view.aspx?src=https%3A%2F%2Famrcrc.ncgm.go.jp%2Fsurveillance%2F010%2FNDB_Oral181030.xlsx&wdOrigin=BROWSELINK (accessed on 1 March 2022). (In Japanese).
- Uda, A.; Shigemura, K.; Kitagawa, K.; Osawa, K.; Kusuki, M.; Yan, Y.; Yano, I.; Miyara, T. Effect of Antimicrobial Stewardship on Oral Quinolone Use and Resistance Patterns over 8 Years (2013–2020). Antibiotics 2021, 10, 1426. [Google Scholar] [CrossRef] [PubMed]
- Uda, A.; Kimura, T.; Nishimura, S.; Ebisawa, K.; Ohji, G.; Kusuki, M.; Yahata, M.; Izuta, R.; Sakaue, T.; Nakamura, T.; et al. Efficacy of educational intervention on reducing the inappropriate use of oral third-generation cephalosporins. Infection 2019, 47, 1037–1045. [Google Scholar] [CrossRef] [PubMed]
- Honda, H.; Murakami, S.; Tagashira, Y.; Uenoyama, Y.; Goto, K.; Takamatsu, A.; Hasegawa, S.; Tokuda, Y. Efficacy of a Postprescription Review of Broad-Spectrum Antimicrobial Agents With Feedback: A 4-Year Experience of Antimicrobial Stewardship at a Tertiary Care Center. Open Forum. Infect. Dis. 2018, 5, ofy314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ministry of Health. Labour and Welfare, About the Individual Revise Item. Available online: https://www.mhlw.go.jp/file/05-Shingikai-12404000-Hokenkyoku-Iryouka/0000193708.pdf (accessed on 17 February 2022). (In Japanese)
- Uda, K.; Kinoshita, N.; Morisaki, N.; Kasai, M.; Horikoshi, Y.; Miyairi, I. Targets for Optimizing Oral Antibiotic Prescriptions for Pediatric Outpatients in Japan. Jpn. J. Infect. Dis. 2019, 72, 149–159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Her Majesty’s Government. UK 5-Year Action Plan for Antimicrobial Resistance 2019 to 2024. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/784894/UK_AMR_5_year_national_action_plan.pdf (accessed on 17 February 2022).
- Hicks, L.A.; Bartoces, M.G.; Roberts, R.M.; Suda, K.J.; Hunkler, R.J.; Taylor, T.H., Jr.; Schrag, S.J. US Outpatient Antibiotic Prescribing Variation According to Geography, Patient Population, and Provider Specialty in 2011. Clin. Infect. Dis. 2015, 60, 1308–1316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Augustin, J.; Mangiapane, S.; Kern, W.V. A regional analysis of outpatient antibiotic prescribing in Germany in 2010. Eur. J. Public Health 2015, 25, 397–399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walle-Hansen, M.M.; Hoye, S. Geographic Variation in Antibiotic Consumption-Is It Due to Doctors’ Prescribing or Patients’ Consulting? Antibiotics 2018, 7, 26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saatchi, A.; Reid, J.N.; Povitz, M.; Shariff, S.Z.; Silverman, M.; Morris, A.M.; Reyes, R.C.; Patrick, D.M.; Marra, F. Appropriateness of Outpatient Antibiotic Use in Seniors across Two Canadian Provinces. Antibiotics 2021, 10, 1484. [Google Scholar] [CrossRef] [PubMed]
- Okumura, Y.; Sakata, N.; Takahashi, K.; Nishi, D.; Tachimori, H. Epidemiology of overdose episodes from the period prior to hospitalization for drug poisoning until discharge in Japan: An exploratory descriptive study using a nationwide claims database. J. Epidemiol. 2017, 27, 373–380. [Google Scholar] [CrossRef] [PubMed]
| Japan | Kyoto | |||||||
|---|---|---|---|---|---|---|---|---|
| <15 Years | 15–64 Years | >64 Years | All Ages | <15 Years | 15–64 Years | >64 Years | All Ages | |
| Third-generation cephalosporins | ↓ | ↑ | ↑ | ↑ | ↓ | ↑ | ↑ | ↑ |
| Quinolones | ↑ | ↑ | ↓ | ↑ | ↑ | ↑ | ↓ | ↑ |
| Macrolides | ↑ | ↑ | ↓ | ↑ | ↑ | ↑ | ↑ | ↑ |
| Total | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ | ↑ |
| Inpatients | Outpatients | |||||||
|---|---|---|---|---|---|---|---|---|
| Third−Generation Cephalosporins | <15 Years | 15−64 Years | >64 Years | All Ages | <15 Years | 15−64 Years | >64 Years | All Ages |
| Big city | −0.0066 | −0.0074 | −0.025 | −0.013 | −0.017 | 0.018 | 0.074 | 0.000029 |
| Small city−1 | 0.0034 | 0.0030 | 0.017 | 0.0059 | 0.020 | 0.023 | 0.054 | 0.0083 |
| Small city−2 | −0.0046 | −0.00058 | 0.013 | −0.00099 | −0.28 | −0.044 | 0.027 | −0.086 |
| Small city−3 | −0.0089 | −0.0029 | −0.034 | −0.013 | −0.25 | 0.024 | 0.11 | −0.018 |
| Small city−4 | −0.00074 | −0.0024 | 0.00074 | −0.0022 | −0.10 | −0.0053 | 0.061 | −0.029 |
| Small city−5 | −0.0047 | −0.0088 | −0.0084 | −0.011 | −0.51 | −0.065 | −0.025 | −0.13 |
| Quinolones | ||||||||
| Big city | 0.00062 | −0.0019 | −0.0013 | −0.0028 | 0.089 | 0.041 | 0.065 | 0.035 |
| Small city−1 | 0.0021 | 0.00090 | 0.0040 | 0.0017 | 0.039 | 0.012 | 0.053 | 0.016 |
| Small city−2 | −0.0023 | −0.0012 | 0.0045 | −0.0017 | 0.0094 | 0.0021 | 0.039 | −0.0037 |
| Small city−3 | 0.00 | −0.00081 | −0.0034 | −0.0026 | 0.027 | 0.026 | 0.054 | 0.021 |
| Small city−4 | 0.0037 | −0.00043 | −0.022 | −0.0045 | 0.018 | −0.0091 | 0.0012 | −0.016 |
| Small city−5 | −0.0028 | −0.00051 | −0.0078 | −0.0047 | 0.00012 | −0.053 | −0.025 | −0.054 |
| Macrolides | ||||||||
| Big city | −0.0019 | −0.00044 | −0.0019 | −0.0015 | 0.11 | 0.082 | 0.097 | 0.067 |
| Small city−1 | 0.0025 | 0.0024 | 0.0066 | 0.0033 | 0.18 | 0.054 | 0.062 | 0.059 |
| Small city−2 | 0.0058 | 0.00077 | 0.0066 | 0.0020 | 0.021 | 0.052 | 0.11 | 0.036 |
| Small city−3 | 0.0053 | 0.00074 | 0.0020 | 0.0012 | 0.091 | −0.0040 | 0.044 | 0.0016 |
| Small city−4 | 0.0086 | 0.00029 | −0.017 | −0.0022 | 0.17 | 0.027 | −0.015 | 0.024 |
| Small city−5 | −0.0030 | −0.0014 | 0.0029 | −0.0012 | −0.26 | 0.025 | 0.062 | −0.023 |
| Total | ||||||||
| Big city | −0.0041 | −0.0077 | −0.0028 | −0.012 | 0.41 | 0.18 | 0.32 | 0.16 |
| Small city−1 | 0.019 | 0.013 | 0.063 | 0.025 | 0.54 | 0.15 | 0.24 | 0.17 |
| Small city−2 | 0.013 | −0.00040 | 0.039 | 0.0030 | −0.031 | 0.047 | 0.30 | 0.013 |
| Small city−3 | 0.0088 | 0.0036 | −0.0087 | −0.0030 | −0.034 | 0.072 | 0.30 | 0.048 |
| Small city−4 | 0.022 | −0.0019 | −0.043 | −0.0081 | 0.042 | 0.032 | 0.037 | −0.028 |
| Small city−5 | 0.018 | −0.0061 | 0.025 | −0.0034 | −0.037 | 0.0061 | 0.20 | −0.037 |
| Japan | Kyoto | |||||||
|---|---|---|---|---|---|---|---|---|
| <15 Years | 15–64 Years | >64 Years | All Ages | <15 Years | 15–64 Years | >64 Years | All Ages | |
| Third-generation cephalosporins | 83.3% | 33.3% | 66.7% | 25.0% | 83.3% | 33.3% | 66.7% | 25.0% |
| Quinolones | 83.3% | 41.7% | 41.7% | 33.3% | 83.3% | 41.7% | 41.7% | 33.3% |
| Macrolides | 75.0% | 75.0% | 25.0% | 66.7% | 75.0% | 75.0% | 75.0% | 66.7% |
| Total | 66.7% | 66.7% | 75.0% | 50.0% | 66.7% | 66.7% | 75.0% | 50.0% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mizuno, K.; Inose, R.; Matsui, Y.; Takata, M.; Yamasaki, D.; Kusama, Y.; Koizumi, R.; Ishikane, M.; Tanabe, M.; Ohge, H.; et al. Search for Indexes to Evaluate Trends in Antibiotic Use in the Sub-Prefectural Regions Using the National Database of Health Insurance Claims and Specific Health Checkups of Japan. Antibiotics 2022, 11, 763. https://doi.org/10.3390/antibiotics11060763
Mizuno K, Inose R, Matsui Y, Takata M, Yamasaki D, Kusama Y, Koizumi R, Ishikane M, Tanabe M, Ohge H, et al. Search for Indexes to Evaluate Trends in Antibiotic Use in the Sub-Prefectural Regions Using the National Database of Health Insurance Claims and Specific Health Checkups of Japan. Antibiotics. 2022; 11(6):763. https://doi.org/10.3390/antibiotics11060763
Chicago/Turabian StyleMizuno, Kanako, Ryo Inose, Yuna Matsui, Mai Takata, Daisuke Yamasaki, Yoshiki Kusama, Ryuji Koizumi, Masahiro Ishikane, Masaki Tanabe, Hiroki Ohge, and et al. 2022. "Search for Indexes to Evaluate Trends in Antibiotic Use in the Sub-Prefectural Regions Using the National Database of Health Insurance Claims and Specific Health Checkups of Japan" Antibiotics 11, no. 6: 763. https://doi.org/10.3390/antibiotics11060763
APA StyleMizuno, K., Inose, R., Matsui, Y., Takata, M., Yamasaki, D., Kusama, Y., Koizumi, R., Ishikane, M., Tanabe, M., Ohge, H., Ohmagari, N., & Muraki, Y. (2022). Search for Indexes to Evaluate Trends in Antibiotic Use in the Sub-Prefectural Regions Using the National Database of Health Insurance Claims and Specific Health Checkups of Japan. Antibiotics, 11(6), 763. https://doi.org/10.3390/antibiotics11060763






