Ventilator-Associated Pneumonia Due to MRSA vs. MSSA: What Should Guide Empiric Therapy?
Abstract
:1. Introduction
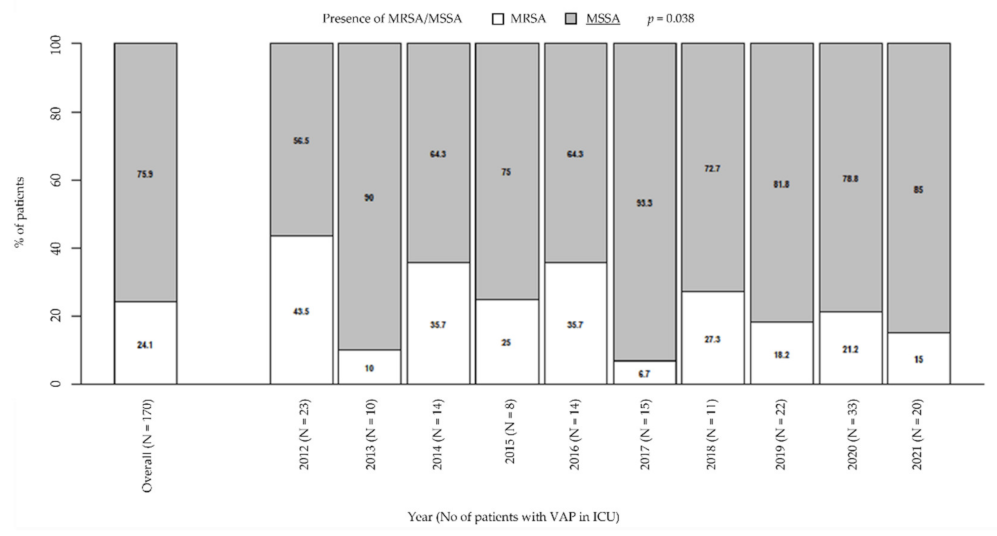
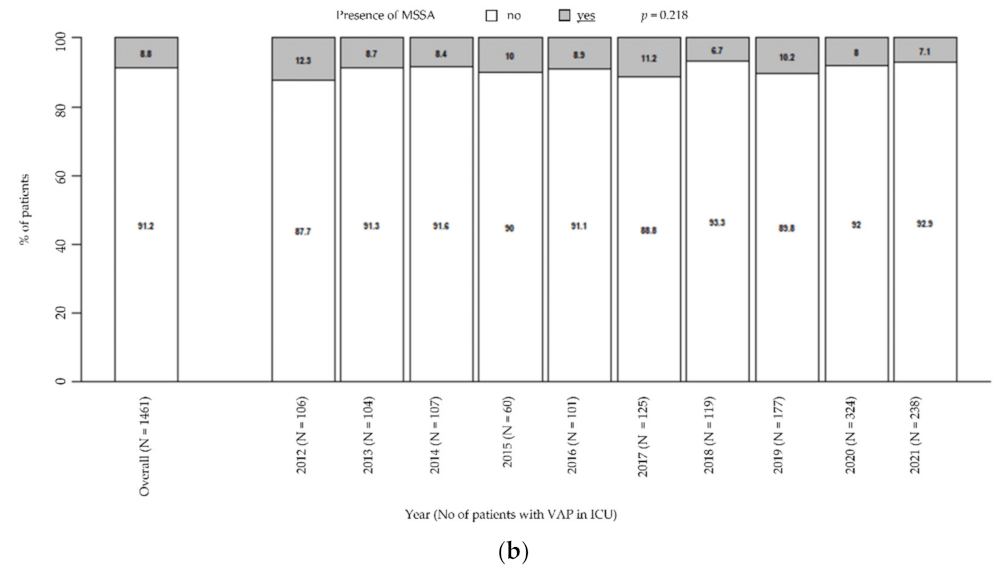
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Design and Participants
4.2. Outcomes
4.3. Statistical Methods
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Koulenti, D.; Tsigou, E.; Rello, J. Nosocomial pneumonia in 27 ICUs in Europe: Perspectives from the EU-VAP/CAP study. Eur. J. Clin. Microbiol. Infect. Dis. 2017, 36, 1999–2006. [Google Scholar] [CrossRef] [PubMed]
- Melsen, W.G.; Rovers, M.M.; Groenwold, R.; Bergmans, D.C.; Camus, C.; Bauer, T.T.; Hanisch, E.; Klarin, B.; Koeman, M.; A Krueger, W.; et al. Attributable mortality of ventilator-associated pneumonia: A meta-analysis of individual patient data from randomised prevention studies. Lancet Infect. Dis. 2013, 13, 665–671. [Google Scholar] [CrossRef]
- Muscedere, J.G.; Shorr, A.F.; Jiang, X.; Day, A.; Heyland, D.K. The adequacy of timely empiric antibiotic therapy for ventilator-associated pneumonia: An important determinant of outcome. J. Crit. Care 2012, 27, 322.e7–322.e14. [Google Scholar] [CrossRef] [PubMed]
- de Bus, L.; Depuydt, P.; Steen, J.; Dhaese, S.; de Smet, K.; Tabah, A.; Akova, M.; Cotta, M.O.; de Pascale, G.; Dimopoulos, G.; et al. Antimicrobial de-escalation in the critically ill patient and assessment of clinical cure: The DIANA study. Intensive Care Med. 2020, 46, 1404–1417. [Google Scholar] [CrossRef] [PubMed]
- Beardsley, J.R.; Williamson, J.C.; Johnson, J.W.; Ohl, C.A.; Karchmer, T.B.; Bowton, D.L. Using local microbiologic data to develop institution-specific guidelines for the treatment of hospital-acquired pneumonia. Chest 2006, 130, 787–793. [Google Scholar] [CrossRef] [PubMed]
- Torres, A.; Niederman, M.S.; Chastre, J.; Ewig, S.; Fernandez-Vandellos, P.; Hanberger, H.; Kollef, M.; Bassi, G.L.; Luna, C.M.; Martin-Loeches, I.; et al. International ERS/ESICM/ESCMID/ALAT guidelines for the management of hospital-acquired pneumonia and ventilator-associated pneumonia. Eur. Respir. J. 2017, 50, 1700582. [Google Scholar] [CrossRef] [PubMed]
- Vandana Kalwaje, E.; Rello, J. Management of ventilator-associated pneumonia: Need for a personalized approach. Expert Rev. Anti. Infect. Ther. 2018, 16, 641–653. [Google Scholar] [CrossRef] [PubMed]
- Laehn, S.; Huang, A.; Carver, T.; Peppard, W. 701: Risk factors for MRSA pneumonia in critically ill trauma/surgical ICU patients. Crit. Care Med. 2016, 44, 251. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Surveillance of antimicrobial resistance in Europe 2018. Stockholm: ECDC. 2019. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/surveillance-antimicrobial-resistance-Europe-2018.pdf (accessed on 14 December 2021).
- Baker, M.A.; Sands, K.E.; Huang, S.S.; Kleinman, K.; Septimus, E.J.; Varma, N.; Blanchard, J.; E Poland, R.; Coady, M.H.; Yokoe, D.S.; et al. The Impact of Coronavirus Disease 2019 (COVID-19) on Healthcare-Associated Infections. Clin. Infect. Dis. 2021, 74, 1748–1754. [Google Scholar] [CrossRef] [PubMed]
- Wee, L.E.I.; Conceicao, E.P.; Tan, J.Y.; Magesparan, K.D.; Amin, I.B.M.; Ismail, B.B.S.; Toh, H.X.; Jin, P.; Zhang, J.; Wee, E.G.L.; et al. Unintended consequences of infection prevention and control measures during COVID-19 pandemic. Am. J. Infect. Control 2020, 49, 469–477. [Google Scholar] [CrossRef] [PubMed]
- Kalil, A.C.; Metersky, M.L.; Klompas, M.; Muscedere, J.; Sweeney, D.A.; Palmer, L.B.; Napolitano, L.M.; O’Grady, N.P.; Bartlett, J.G.; Carratalà, J.; et al. Management of Adults with Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin. Infect. Dis. 2016, 63, e61–e111. [Google Scholar] [CrossRef] [PubMed]
- Mao, P.; Peng, P.; Liu, Z.; Xue, Z.; Yao, C. Risk Factors and Clinical Outcomes of Hospital-Acquired MRSA Infections in Chongqing, China. Infect. Drug Resist. 2019, 12, 3709–3717. [Google Scholar] [PubMed] [Green Version]
- Liu, C.; Bayer, A.; Cosgrove, S.E.; Daum, R.S.; Fridkin, S.K.; Gorwitz, R.J.; Kaplan, S.L.; Karchmer, A.W.; Levine, D.P.; Murray, B.E.; et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin. Infect. Dis. 2011, 52, e18–e55. [Google Scholar] [PubMed] [Green Version]
- Kim, H.J.; Kang, E.-R.; Park, M.Y.; Kim, B.K.; Kim, M.J.; Jung, S.; Roh, K.H.; Sung, N.; Yang, J.-H.; Lee, M.-W.; et al. Development of a multiplex real-time PCR assay for the simultaneous detection of four bacterial pathogens causing pneumonia. PLoS ONE 2021, 16, e0253402. [Google Scholar]
- Butler-Laporte, G.; De L’Étoile-Morel, S.; Cheng, M.P.; McDonald, E.G.; Lee, T.C. MRSA colonization status as a predictor of clinical infection: A systematic review and meta-analysis. J. Infect. 2018, 77, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Ncezid, C.D.C.; DHQP. National Healthcare Safety Network (NHSN) Patient Safety Component Manual. 2021. Available online: https://www.cdc.gov/nhsn/pdfs/validation/2021/pcsmanual_2021-508.pdf (accessed on 14 December 2021).

| Variables | Overall (N = 170) | MRSA (N = 41)-Statistics | MSSA (N = 129)-Statistics | p-Value |
|---|---|---|---|---|
| Age (y), median (IQR) | 61 (50–72.75) | 66 (57–76) | 60 (50–70) | 0.107 |
| Gender (male), n (%) | 114 (67.1%) | 26 (63.4%) | 88 (68.2%) | 0.705 |
| ICU-LOS before VAP onset (days), median (IQR) | 3 (0–8) | 3 (0–11) | 3 (0–6) | 0.314 |
| ICU LOS after VAP onset (days), median (IQR) | 11 (4–26) | 13 (5–23) | 11 (4–27) | 0.806 |
| Polymicrobial infection, n (%) | 81 (47.6%) | 16 (39%) | 65 (50.4%) | 0.276 |
| No. polymicrobial infection, median (IQR) | 1 (1–2) | 1 (1–2) | 2 (1–2) | 0.267 |
| Nasal swab (screening MRSA), n (%) | 95 (55.9%) | 23 (56.1%) | 72 (55.8%) | 1000 |
| MRSA in nasal swab, n (%), [N = 95] | 8 (8.4%) | 8 (34.8%) | 0 (0%) | 0.000 |
| MRSA in blood culture, n (%) | 9 (5.3%) | 7 (17.1%) | 2 (1.6%) | 0.001 |
| MSSA in blood culture, n (%) | 14 (8.2%) | 0 (0%) | 14 (10.9%) | 0.023 |
| MRSA Nasal-Swab Screening | Non-MRSA VAP | MRSA VAP | Total |
|---|---|---|---|
| Negative | 863 | 11 | 874 |
| Positive | 14 | 8 | 22 |
| Total | 877 | 19 | 896 |
| Sensitivity, % | 42.1 |
| Specificity, % | 98.4 |
| PPV, % | 36.4 |
| NPV, % | 98.7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Colaneri, M.; Di Carlo, D.; Amatu, A.; Marvulli, L.N.; Corbella, M.; Petazzoni, G.; Cambieri, P.; Muzzi, A.; Bandi, C.; Di Matteo, A.; et al. Ventilator-Associated Pneumonia Due to MRSA vs. MSSA: What Should Guide Empiric Therapy? Antibiotics 2022, 11, 851. https://doi.org/10.3390/antibiotics11070851
Colaneri M, Di Carlo D, Amatu A, Marvulli LN, Corbella M, Petazzoni G, Cambieri P, Muzzi A, Bandi C, Di Matteo A, et al. Ventilator-Associated Pneumonia Due to MRSA vs. MSSA: What Should Guide Empiric Therapy? Antibiotics. 2022; 11(7):851. https://doi.org/10.3390/antibiotics11070851
Chicago/Turabian StyleColaneri, Marta, Domenico Di Carlo, Alessandro Amatu, Lea Nadia Marvulli, Marta Corbella, Greta Petazzoni, Patrizia Cambieri, Alba Muzzi, Claudio Bandi, Angela Di Matteo, and et al. 2022. "Ventilator-Associated Pneumonia Due to MRSA vs. MSSA: What Should Guide Empiric Therapy?" Antibiotics 11, no. 7: 851. https://doi.org/10.3390/antibiotics11070851
APA StyleColaneri, M., Di Carlo, D., Amatu, A., Marvulli, L. N., Corbella, M., Petazzoni, G., Cambieri, P., Muzzi, A., Bandi, C., Di Matteo, A., Sacchi, P., Mojoli, F., & Bruno, R. (2022). Ventilator-Associated Pneumonia Due to MRSA vs. MSSA: What Should Guide Empiric Therapy? Antibiotics, 11(7), 851. https://doi.org/10.3390/antibiotics11070851







