Polish Medical Doctors’ Opinions on Available Resources and Information Campaigns concerning Antibiotics and Antibiotic Resistance, a Cross-Sectional Study
Abstract
:1. Introduction
2. Results
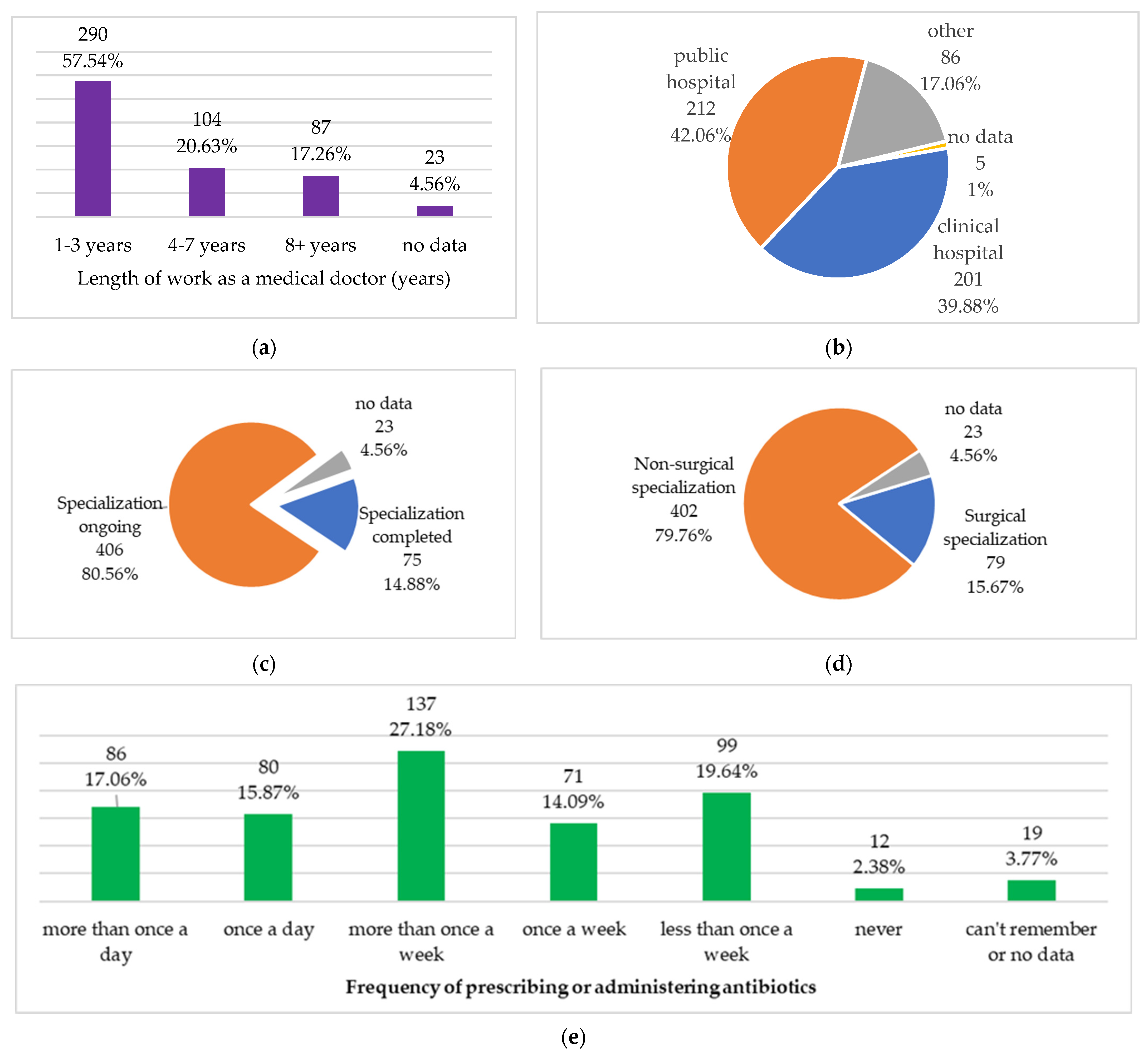
2.1. Characteristics of the Study Group
2.2. Resources Used by Medical Doctors in the Management of Infections
2.3. Campaigns and Training
2.4. Awareness of the National Action Plan on Antimicrobial Resistance, European Antibiotic Awareness Day and World Antibiotic Awareness Week
3. Discussion
3.1. Resources Used by Medical Doctors in Management of Infections
3.2. Opinion on Social Campaigns and Other Methods of Raising Awareness on Antibiotics
3.3. National Action Plan on Antimicrobial Resistance, EAAD and WAAW
3.4. Limitations
4. Materials and Methods
4.1. Study Group
4.2. Survey Questionnaire
4.2.1. Construction of the Questionnaire
4.2.2. Dissemination Process and Data Collection
4.3. Statistical Methods
4.4. Ethical Statement
5. Conclusions
Recommendations and Future Directions
- <1>
- Clinical practice guidelines are highly quoted as a preferred resource but Polish doctors’ adherence may vary. This topic should be explored further in research.
- <2>
- It is necessary to encourage doctors to regularly update their knowledge on the innovations in antibiotic therapy (specific to a field of medicine). Methods of knowledge dissemination and awareness raising should be adjusted to the needs of Polish prescribers (e.g., leaflets, workshops, quizzes, higher CME/CPD scoring system).
- <3>
- Doctors should be better acquainted with educational opportunities such as World Antimicrobial Awareness Week, European Antibiotic Awareness Day and National Programme for the Protection of Antibiotics. Ways to promote those campaigns more effectively should be explored in the Polish context (e.g., bringing it up in undergraduate medical education).
- <4>
- Keeping physicians educated, engaged and eloquent about antibiotics and antibiotic resistance should be a priority for public health agencies and training institutions in Poland.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bassetti, M.; Poulakou, G.; Ruppe, E.; Bouza, E.; Van Hal, S.; Brink, A. Antimicrobial resistance in the next 30 years, humankind, bugs and drugs: A visionary approach. Intensive Care Med. 2017, 43, 1464–1475. [Google Scholar] [CrossRef] [PubMed]
- Wall, S. Prevention of antibiotic resistance—An epidemiological scoping review to identify research categories and knowledge gaps. Glob. Health Action 2019, 12, 1756191. [Google Scholar] [CrossRef]
- Lee, C.; Cho, I.; Jeong, B.; Lee, S. Strategies to Minimize Antibiotic Resistance. Int. J. Environ. Res. Public Health 2013, 10, 4274–4305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barchitta, M.; Sabbatucci, M.; Furiozzi, F.; Iannazzo, S.; Maugeri, A.; Maraglino, F.; Prato, B.; Agodi, A.; Pantosti, A. Knowledge, attitudes and behaviors on antibiotic use and resistance among healthcare workers in Italy, 2019: Investigation by a clustering method. Antimicrob. Resist. Infect. Control 2021, 10, 134. [Google Scholar] [CrossRef] [PubMed]
- Gyssens, I. Role of Education in Antimicrobial Stewardship. Med. Clin. N. Am. 2018, 102, 855–871. [Google Scholar] [CrossRef]
- Majumder, M.; Rahman, S.; Cohall, D.; Bharatha, A.; Singh, K.; Haque, M.; Hilaire, M.G.-S. Antimicrobial Stewardship: Fighting Antimicrobial Resistance and Protecting Global Public Health. Infect. Drug Resist. 2020, 13, 4713–4738. [Google Scholar] [CrossRef]
- Madhumathi, J.; Sinha, R.; Veeraraghavan, B.; Walia, K. Use of “Social Media”—An Option for Spreading Awareness in Infection Prevention. Curr. Treat. Options Infect. Dis. 2021, 13, 14–31. [Google Scholar] [CrossRef]
- Finset, A.; Bosworth, H.; Butow, P.; Gulbrandsen, P.; Hulsman, R.; Pieterse, A.; Street, R.; Tschötschel, R.; van Weert, J. Effective health communication—A key factor in fighting the COVID-19 pandemic. Patient Educ. Couns. 2020, 103, 873–876. [Google Scholar] [CrossRef]
- Chase, A.; Clark, M.; Rogalska, A.; Musselman, M. Cultivating Patient-Physician Communication about Vaccination through Vaccine Metaphors. Med. Sci. Educ. 2020, 30, 1015–1017. [Google Scholar] [CrossRef]
- Broniatowski, D.; Dredze, M.; Ayers, J. “First Do No Harm”: Effective Communication about COVID-19 Vaccines. Am. J. Public Health 2021, 111, 1055–1057. [Google Scholar] [CrossRef]
- Marotta, S.; McNally, V. Increasing Vaccine Confidence through Parent Education and Empowerment Using Clear and Comprehensible Communication. Acad. Pediatr. 2021, 21, S30–S31. [Google Scholar] [CrossRef] [PubMed]
- Dadgostar, P. Antimicrobial Resistance: Implications and Costs. Infect. Drug Resist. 2019, 12, 3903–3910. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sakeena, M.; Bennett, A.; McLachlan, A. Enhancing pharmacists’ role in developing countries to overcome the challenge of antimicrobial resistance: A narrative review. Antimicrob. Resist. Infect. Control 2018, 7, 63. [Google Scholar] [CrossRef] [Green Version]
- Cribb, A.; Entwistle, V. Shared decision making: Trade-offs between narrower and broader conceptions. Health Expect. 2011, 14, 210–219. [Google Scholar] [CrossRef] [PubMed]
- Borek, A.; Anthierens, S.; Allison, R.; Mcnulty, C.; Anyanwu, P.; Costelloe, C.; Walker, A.; Butler, C.; Tonkin-Crine, S.; on behalf of the STEP-UP Study Team. Social and Contextual Influences on Antibiotic Prescribing and Antimicrobial Stewardship: A Qualitative Study with Clinical Commissioning Group and General Practice Professionals. Antibiotics 2020, 9, 859. [Google Scholar] [CrossRef]
- Karobari, M.I.; Khijmatgar, S.; Bhandary, R.; Krishna Nayak, U.S.; Del Fabbro, M.; Horn, R.; Marya, A. A Multicultural Demographic Study to Analyze Antibiotic Prescription Practices and the Need for Continuing Education in Dentistry. BioMed Res. Int. 2021, 2021, 5599724. [Google Scholar] [CrossRef]
- Littmann, J.; Viens, A. The Ethical Significance of Antimicrobial Resistance. Public Health Ethics 2015, 8, 209–224. [Google Scholar] [CrossRef] [Green Version]
- Littmann, J.; Buyx, A.; Cars, O. Antibiotic resistance: An ethical challenge. Int. J. Antimicrob. Agents 2015, 46, 359–361. [Google Scholar] [CrossRef]
- Parsonage, B.; Hagglund, P.; Keogh, L.; Wheelhouse, N.; Brown, R.; Dancer, S. Control of Antimicrobial Resistance Requires an Ethical Approach. Front. Microbiol. 2017, 8, 2124. [Google Scholar] [CrossRef] [Green Version]
- Abimbola, S.; Otieno, M.; Cole, J. Reducing the Use of Antimicrobials as a Solution to the Challenge of Antimicrobial Resistance (AMR): Approaching an Ethical Dilemma through the Lens of Planetary Health. Challenges 2021, 12, 23. [Google Scholar] [CrossRef]
- Mackenzie, J.; McKinnon, M.; Jeggo, M. One Health: From Concept to Practice. Confront. Emerg. Zoonoses 2014, 19, 163–189. [Google Scholar]
- Antimicrobial Resistance Tackling the Burden in the European Union. 2019. Available online: https://www.oecd.org/health/health-systems/AMR-Tackling-the-Burden-in-the-EU-OECD-ECDC-Briefing-Note-2019.pdf (accessed on 20 June 2022).
- Surveillance Atlas of Infectious Diseases. 2022. Available online: https://atlas.ecdc.europa.eu/public/index.aspx?Dataset=27&HealthTopic=4 (accessed on 20 June 2022).
- Wojkowska-Mach, J.; Godman, B.; Glassman, A.; Kurdi, A.; Pilc, A.; Rozanska, A.; Skoczyński, S.; Wałaszek, M.; Bochenek, T. Antibiotic consumption and antimicrobial resistance in Poland; findings and implications. Antimicrob. Resist. Infect. Control 2018, 7, 136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rostkowska, O.M.; Kuthan, R.; Burban, A.; Salińska, J.; Ciebiera, M.; Młynarczyk, G.; Durlik, M. Analysis of Susceptibility to Selected Antibiotics in Klebsiella pneumoniae, Escherichia coli, Enterococcus faecalis and Enterococcus faecium Causing Urinary Tract Infections in Kidney Transplant Recipients over 8 Years: Single-Center Study. Antibiotics 2020, 9, 284. [Google Scholar] [CrossRef] [PubMed]
- Mazińska, B.; Hryniewicz, W. Polish Physicians’ Attitudes Towards Antibiotic Prescription and Antimicrobial Resistance. Pol. J. Microbiol. 2017, 66, 309–319. [Google Scholar] [CrossRef] [Green Version]
- Zgliczyński, W.S.; Bartosiński, J.; Rostkowska, O.M. Knowledge and Practice of Antibiotic Management and Prudent Prescribing among Polish Medical Doctors. Int. J. Environ. Res. Public Health 2022, 19, 3739. [Google Scholar] [CrossRef]
- European Antibiotic Awareness Day. 2022. Available online: https://antibiotic.ecdc.europa.eu/en/european-antibiotic-awareness-day-eaad-2021 (accessed on 20 April 2022).
- Podstawy Utworzenia Programu—Narodowy Program Ochrony Antybiotyków. Narodowy Program Ochrony Antybiotyków. 2022. Available online: http://antybiotyki.edu.pl/program/podstawy-utworzenia-programu/ (accessed on 26 June 2022).
- Ashiru-Oredope, D.; Hopkins, S.; Vasandani, S.; Umoh, E.; Oloyede, O.; Nilsson, A. Healthcare workers’ knowledge, attitudes and behaviours with respect to antibiotics, antibiotic use and antibiotic resistance across 30 EU/EEA countries in 2019. Eurosurveillance 2021, 26, 1900633. [Google Scholar] [CrossRef]
- Ashiru-Oredope, D.; Kinsman, J.; Vasandani, S.; Umoh, E.; Oloyede, O.; Hopkins, S.; Nilsson, A.; Elsert, L.; Monnet, D.L.; the #ECDCAntibioticSurvey Project Advisory Group. Survey of Healthcare Workers’ Knowledge, Attitudes and Behaviours on Antibiotics, Antibiotic Use and Antibiotic Resistance in the EU/EEA. 2019. Available online: https://www.ecdc.europa.eu/en/publications-data/survey-healthcare-workers-knowledge-attitudes-and-behaviours-antibiotics (accessed on 20 April 2022).
- Ventola, C.L. The antibiotic resistance crisis: Part 1: Causes and threats. Pharm. Ther. 2015, 40, 277–283. [Google Scholar]
- Fleming, A. Penicillin. 1945. Available online: https://www.nobelprize.org/uploads/2018/06/fleming-lecture.pdf (accessed on 20 April 2022).
- Machowska, A.; Stålsby Lundborg, C. Drivers of Irrational Use of Antibiotics in Europe. Int. J. Environ. Res. Public Health 2018, 16, 27. [Google Scholar] [CrossRef] [Green Version]
- Atif, M.; Asghar, S.; Mushtaq, I.; Malik, I.; Amin, A.; Babar, Z.; Scahill, S. What drives inappropriate use of antibiotics? A mixed methods study from Bahawalpur, Pakistan. Infect. Drug Resist. 2019, 12, 687–699. [Google Scholar] [CrossRef] [Green Version]
- Ofori-Asenso, R.; Agyeman, A. Irrational Use of Medicines—A Summary of Key Concepts. Pharmacy 2016, 4, 35. [Google Scholar] [CrossRef] [Green Version]
- Ezebuenyi, M.C.; Brakta, F.; Onor, I.O.; Sarpong, D.F.; Bryant-Burks, K.; Figueroa, J.E., 2nd. Evaluation of Physician Prescribing Patterns For Antibiotics in the Treatment of Nonnecrotizing Skin and Soft Tissue Infections. Pharm. Ther. 2018, 43, 287–292. [Google Scholar]
- Pechère, J. Le médecin, le malade et les antibiotiques. Bull. L’académie Natl. Méd. 2004, 188, 1257–1267. [Google Scholar] [CrossRef]
- Wester, C.; Durairaj, L.; Evans, A.; Schwartz, D.; Husain, S.; Martinez, E. Antibiotic Resistance. Arch. Intern. Med. 2002, 162, 2210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Labi, A.; Obeng-Nkrumah, N.; Bjerrum, S.; Aryee, N.; Ofori-Adjei, Y.; Yawson, A. Physicians’ knowledge, attitudes, and perceptions concerning antibiotic resistance: A survey in a Ghanaian tertiary care hospital. BMC Health Serv. Res. 2018, 18, 126. [Google Scholar] [CrossRef]
- Calva, J. Antibiotic use in a periurban community in Mexico: A household and drugstore survey. Soc. Sci. Med. 1996, 42, 1121–1128. [Google Scholar] [CrossRef]
- Sahra, S.; Jahangir, A.; De Chavez, V. Antimicrobial Stewardship: A Review for Internal Medicine Physicians. Cureus 2021, 13, e14385. [Google Scholar] [CrossRef]
- Barlam, T.; Childs, E.; Zieminski, S.; Meshesha, T.; Jones, K.; Butler, J.; Damschroder, L.J.; Goetz, M.B.; Madaras-Kelly, K.; Reardon, C.M.; et al. Perspectives of Physician and Pharmacist Stewards on Successful Antibiotic Stewardship Program Implementation: A Qualitative Study. Open Forum Infect. Dis. 2020, 7, ofaa229. [Google Scholar] [CrossRef]
- Lubwama, M.; Onyuka, J.; Ayazika, K.; Ssetaba, L.; Siboko, J.; Daniel, O.; Mushi, M.F. Knowledge, attitudes, and perceptions about antibiotic use and antimicrobial resistance among final year undergraduate medical and pharmacy students at three universities in East Africa. PLoS ONE 2021, 16, e0251301. [Google Scholar] [CrossRef]
- Higuita-Gutiérrez, L.; Roncancio Villamil, G.; Jiménez Quiceno, J. Knowledge, attitude, and practice regarding antibiotic use and resistance among medical students in Colombia: A cross-sectional descriptive study. BMC Public Health 2020, 20, 1861. [Google Scholar] [CrossRef]
- Tiong, T.W.; Chua, S.S. Knowledge and Attitude of University Students on Antibiotics: A Cross-sectional Study in Malaysia. Drug Healthc. Patient Saf. 2020, 12, 135–144. [Google Scholar] [CrossRef]
- Sobierajski, T.; Mazińska, B.; Wanke-Rytt, M.; Hryniewicz, W. Knowledge-Based Attitudes of Medical Students in Antibiotic Therapy and Antibiotic Resistance. A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 3930. [Google Scholar] [CrossRef] [PubMed]
- Biezen, R.; Roberts, C.; Buising, K.; Thursky, K.; Boyle, D.; Lau, P.; Clark, M.; Manski-Nankervis, J.-A. How do general practitioners access guidelines and utilise electronic medical records to make clinical decisions on antibiotic use? Results from an Australian qualitative study. BMJ Open 2019, 9, e028329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vincent, Y.; Frachon, A.; Buffeteau, C.; Conort, G. Construction of a patient decision aid for the treatment of uncomplicated urinary tract infection in primary care. BMC Fam. Pract. 2021, 22, 26. [Google Scholar] [CrossRef] [PubMed]
- Radošević Quadranti, N.; Vlahović-Palčevski, V.; Popović, B.; Diminić-Lisica, I. Impact of guidelines on antibiotic prescribing approach in primary care—A 10-year study. Fam. Pract. 2020, 38, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Pulcini, C.; Botelho-Nevers, E.; Dyar, O.; Harbarth, S. The impact of infectious disease specialists on antibiotic prescribing in hospitals. Clin. Microbiol. Infect. 2014, 20, 963–972. [Google Scholar] [CrossRef] [Green Version]
- Yapar, N.; Erdenizmenli, M.; Oğuz, V.; Kuruüzüm, Z.; Senger, S.; Çakır, N.; Yüce, A. Infectious disease consultations and antibiotic usage in a Turkish university hospital. Int. J. Infect. Dis. 2006, 10, 61–65. [Google Scholar] [CrossRef] [Green Version]
- de With, K.; Allerberger, F.; Amann, S.; Apfalter, P.; Brodt, H.; Eckmanns, T.; Fellhauer, M.; Geiss, H.K.; Janata, O.; Krause, R.; et al. Strategies to enhance rational use of antibiotics in hospital: A guideline by the German Society for Infectious Diseases. Infection 2016, 44, 395–439. [Google Scholar] [CrossRef] [Green Version]
- Dellit, T. Summary of the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America Guidelines for Developing an Institutional Program to Enhance Antimicrobial Stewardship. Infect. Dis. Clin. Pract. 2007, 15, 263–264. [Google Scholar] [CrossRef] [Green Version]
- Spurling, G.; Mansfield, P.; Montgomery, B.; Lexchin, J.; Doust, J.; Othman, N.; Vitry, A. Information from Pharmaceutical Companies and the Quality, Quantity, and Cost of Physicians’ Prescribing: A Systematic Review. PLoS Med. 2010, 7, e1000352. [Google Scholar] [CrossRef] [Green Version]
- Lieb, K.; Scheurich, A. Contact between Doctors and the Pharmaceutical Industry, Their Perceptions, and the Effects on Prescribing Habits. PLoS ONE 2014, 9, e110130. [Google Scholar] [CrossRef] [Green Version]
- Karasneh, R.; Al-Azzam, S.; Ababneh, M.; Basheti, I.; Al-Azzeh, O.; Al Sharie, S.; Conway, B.R.; Aldeyab, M.A. Exploring Information Available to and Used by Physicians on Antibiotic Use and Antibiotic Resistance in Jordan. Antibiotics 2021, 10, 963. [Google Scholar] [CrossRef] [PubMed]
- Sychareun, V.; Sihavong, A.; Machowska, A.; Onthongdee, X.; Chaleunvong, K.; Keohavong, B.; Eriksen, J.; Hanson, C.; Vongsouvath, M.; Marrone, G.; et al. Knowledge, Attitudes, Perception and Reported Practices of Healthcare Providers on Antibiotic Use and Resistance in Pregnancy, Childbirth and Children under Two in Lao PDR: A Mixed Methods Study. Antibiotics 2021, 10, 1462. [Google Scholar] [CrossRef] [PubMed]
- Hohmann, C.; Eickhoff, C.; Radziwill, R.; Schulz, M. Adherence to guidelines for antibiotic prophylaxis in surgery patients in German hospitals: A multicentre evaluation involving pharmacy interns. Infection 2011, 40, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Øhrstrøm, M.T.; Danstrup, C.S.; Klug, T.E. Adherence to antibiotic guidelines in the treatment of acute pharyngeal infections. Dan. Med. J. 2019, 66, A5530. [Google Scholar] [PubMed]
- Hek, K.; van Esch, T.; Lambooij, A.; Weesie, Y.; van Dijk, L. Guideline Adherence in Antibiotic Prescribing to Patients with Respiratory Diseases in Primary Care: Prevalence and Practice Variation. Antibiotics 2020, 9, 571. [Google Scholar] [CrossRef]
- Harris, A.; Hicks, L.; Qaseem, A. Appropriate Antibiotic Use for Acute Respiratory Tract Infection in Adults: Advice for High-Value Care from the American College of Physicians and the Centers for Disease Control and Prevention. Ann. Intern. Med. 2016, 164, 425. [Google Scholar] [CrossRef] [Green Version]
- Ivanovska, V.; Hek, K.; Mantel Teeuwisse, A.; Leufkens, H.; Nielen, M.; van Dijk, L. Antibiotic prescribing for children in primary care and adherence to treatment guidelines. J. Antimicrob. Chemother. 2016, 71, 1707–1714. [Google Scholar] [CrossRef]
- Roope, L.; Tonkin-Crine, S.; Herd, N.; Michie, S.; Pouwels, K.; Castro-Sanchez, E.; Sallis, A.; Hopkins, S.; Robotham, J.V.; Crook, D.W.; et al. Reducing expectations for antibiotics in primary care: A randomised experiment to test the response to fear-based messages about antimicrobial resistance. BMC Med. 2020, 18, 110. [Google Scholar] [CrossRef]
- Shetty, A.; Thakolkaran, N.; D′Souza, N.; Shetty, A. Antibiotic prescribing knowledge, attitudes, and practice among physicians in teaching hospitals in South India. J. Fam. Med. Prim. Care 2017, 6, 526. [Google Scholar] [CrossRef]
- Fiore, D.C.; Fettic, L.P.; Wright, S.D.; Ferrara, B.R. Antibiotic overprescribing: Still a major concern. J. Fam. Pract. 2017, 66, 730–736. [Google Scholar]
- Antibiotics’ Resistance: Report on European Doctors’ Knowledge and Attitudes. 2020. Available online: https://www.cpme.eu/api/documents/adopted/2020/11/PR_CPME.Report.on_.doctors.knowledge.on_.antibiotics.and_.AMR_.pdf (accessed on 21 April 2022).
- Sharma, R.; Chopra, V.; Kour, G. Use of Antibiotics for Respiratory Illnesses in Rural India. J. Clin. Diagn. Res. 2009, 3, 1557–1561. [Google Scholar]
- Pulcini, C.; Williams, F.; Molinari, N.; Davey, P.; Nathwani, D. Junior doctors’ knowledge and perceptions of antibiotic resistance and prescribing: A survey in France and Scotland. Clin. Microbiol. Infect. 2011, 17, 80–87. [Google Scholar] [CrossRef] [Green Version]
- Nicholson, A.; Tennant, I.; White, L.; Thoms-Rodriguez, C.; Cook, L.; Johnson, S.; Thompson, T.; Barnett, J.; Richards, L. The knowledge, attitudes and practices of doctors regarding antibiotic resistance at a tertiary care institution in the Caribbean. Antimicrob. Resist. Infect. Control 2018, 7, 23. [Google Scholar] [CrossRef] [Green Version]
- Trikha, S.; Dalpath, S.; Sharma, M.; Shafiq, N. Antibiotic prescribing patterns and knowledge of antibiotic resistance amongst the doctors working at public health facilities of a state in northern India: A cross sectional study. J. Fam. Med. Prim. Care 2020, 9, 3937. [Google Scholar] [CrossRef]
- Huttner, B.; Goossens, H.; Verheij, T.; Harbarth, S. Characteristics and outcomes of public campaigns aimed at improving the use of antibiotics in outpatients in high-income countries. Lancet Infect. Dis. 2010, 10, 17–31. [Google Scholar] [CrossRef]
- Bhattacharya, A.; Hopkins, S.; Sallis, A.; Budd, E.; Ashiru-Oredope, D. A process evaluation of the UK-wide Antibiotic Guardian campaign: Developing engagement on antimicrobial resistance. J. Public Health 2017, 39, e40–e47. [Google Scholar] [CrossRef] [Green Version]
- Lokhorst, A.; Werner, C.; Staats, H.; van Dijk, E.; Gale, J. Commitment and Behavior Change. Environ. Behav. 2011, 45, 3–34. [Google Scholar] [CrossRef]
- Pinder, R.; Berry, D.; Sallis, A.; Chadborn, T. Behaviour Change and Antibiotic Prescribing in Healthcare Settings: Literature Review and Behavioural Analysis; Public Health England: London, UK, 2015.
- Tonna, A.; Weidmann, A.; Sneddon, J.; Stewart, D. Views and experiences of community pharmacy team members on antimicrobial stewardship activities in Scotland: A qualitative study. Int. J. Clin. Pharm. 2020, 42, 1261–1269. [Google Scholar] [CrossRef]




| Resource | n (%) |
|---|---|
| clinical practice guidelines | 451 (89.48) |
| previous clinical experience | 369 (73.21) |
| continuing education training courses | 226 (44.84) |
| infection specialists | 184 (36.51) |
| scientific journals | 167 (33.13) |
| industry materials/publications | 101 (20.04) |
| documentation from pharmaceutical companies | 45 (8.93) |
| representatives from pharmaceutical companies | 9 (1.79) |
| social media | 8 (1.59) |
| none of the above/other | 23 (4.56) |
| Question | Yes | No | Unsure |
|---|---|---|---|
| In the last 12 months, do you remember receiving any information about avoiding unnecessary prescribing or administering or dispensing of antibiotics? (n = 504) | 270 (53.57) | 206 (40.87) | 28 (5.56) |
| Did the information contribute to changing your views about avoiding unnecessary prescribing or administering or dispensing of antibiotics? (n = 270) | 150 (55.56) | 68 (25.19) | 52 (19.26) |
| On the basis of the information you received, have you changed your practice on prescribing or administering or dispensing antibiotics? (n = 270) | 113 (41.85) | 112 (41.48) | 45 (16.67) |
| Source of Information | Sources of Information about Avoiding Unnecessary Prescribing/Dispensing/Administering of Antibiotics (n = 270) 1 | Sources of Information Which Had the Most Influence on Changing the Respondent’s Views (n = 150) 2 |
|---|---|---|
| Published guidelines | 181 (67.04) | 102 (68.00) |
| Colleague or peer | 153 (56.67) | 37 (24.67) |
| Training—conference group | 148 (54.81) | 58 (38.67) |
| Employer | 75 (27.78) | 16 (10.67) |
| Training—individual/specialized | 62 (22.96) | 26 (17.33) |
| Newspaper | 42 (15.56) | 6 (4.00) |
| Scientific organization | 33 (12.22) | 10 (6.67) |
| Social media | 31 (11.48) | 0 (0.00) |
| Media advertising (TV/radio) | 20 (7.41) | 0 (0.00) |
| Audit and feedback | 17 (6.30) | 7 (4.67) |
| Professional body (e.g., doctors/pharmacists/nurses) | 12 (4.44) | 2 (1.33) |
| Public policy | 7 (2.59) | 3 (2.00) |
| Other | 9 (3.33) | 4 (2.67) |
| Level | n (%) |
|---|---|
| Action is needed at all levels | 299 (59.33) |
| Individual (by medical doctors prescribing drugs) | 141 (27.98) |
| Individual (by all healthcare workers) | 116 (23.02) |
| Regional/National | 55 (10.91) |
| EU/Global | 43 (8.53) |
| Related to environment/animal health | 36 (7.14) |
| Individual (in public) | 18 (3.57) |
| I don’t know | 8 (1.59) |
| Initiatives | n (%) |
|---|---|
| National or regional guidelines on infection control | 286 (56.75) |
| Conferences/events focused on tackling antibiotic resistance | 207 (41.07) |
| Toolkits of educational materials, including on-line and regional guidelines for healthcare workers | 191 (37.90) |
| National or regional posters or leaflets on antibiotic awareness | 165 (32.74) |
| Articles on antibiotic resistance in the (national) press | 132 (26.19) |
| Awareness raising by professional organizations | 115 (22.82) |
| World Antibiotic Awareness Week (WAAW)/European Antibiotic Awareness Day (EAAD) | 86 (17.06) |
| Television and radio advertising for the public | 83 (16.47) |
| National campaigns | 60 (11.90) |
| I don’t know of any initiatives | 63 (12.50) |
| Other | 6 (1.19) |
| Answer | There Had Been Good Promotion of Prudent Antibiotic Use and Information about Antibiotic Resistance in Their Country (n = 494 Responses Given) | The National Campaign Had Been Effective in Reducing Unnecessary Antibiotic Use and Controlling Antibiotic Resistance in Their Country (n = 489 Responses Given) |
|---|---|---|
| strongly disagree (1) | 136 (27.53) | 99 (20.25) |
| disagree (2) | 233 (47.17) | 199 (40.70) |
| undecided (3) | 68 (13.77) | 91 (18.61) |
| agree (4) | 49 (9.92) | 85 (17.38) |
| strongly agree (5) | 8 (1.62) | 15 (3.07) |
| Question | Yes | No | Unsure |
|---|---|---|---|
| Antimicrobial Resistance National Action Plan | 202 (40.08) | 35 (6.94) | 267 (52.98) |
| European Antibiotic Awareness Day | 120 (23.81) | 336 (66.67) | 48 (9.52) |
| World Antibiotic Awareness Week | 100 (19.84) | 353 (70.04) | 51 (10.12) |
| Answer | European Antibiotic Awareness Day (n = 441 Responses Given) | World Antibiotic Awareness Week (n = 440 Responses Given) |
|---|---|---|
| very ineffective (1) | 47 (10.66) | 45 (10.23) |
| ineffective (2) | 69 (15.65) | 69 (15.68) |
| undecided (3) | 306 (69.39) | 303 (68.86) |
| effective (4) | 17 (3.85) | 21 (4.77) |
| very effective (5) | 2 (0.45) | 2 (0.45) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rostkowska, O.M.; Raczkiewicz, D.; Knap-Wielgus, W.; Zgliczyński, W.S. Polish Medical Doctors’ Opinions on Available Resources and Information Campaigns concerning Antibiotics and Antibiotic Resistance, a Cross-Sectional Study. Antibiotics 2022, 11, 882. https://doi.org/10.3390/antibiotics11070882
Rostkowska OM, Raczkiewicz D, Knap-Wielgus W, Zgliczyński WS. Polish Medical Doctors’ Opinions on Available Resources and Information Campaigns concerning Antibiotics and Antibiotic Resistance, a Cross-Sectional Study. Antibiotics. 2022; 11(7):882. https://doi.org/10.3390/antibiotics11070882
Chicago/Turabian StyleRostkowska, Olga Maria, Dorota Raczkiewicz, Weronika Knap-Wielgus, and Wojciech Stefan Zgliczyński. 2022. "Polish Medical Doctors’ Opinions on Available Resources and Information Campaigns concerning Antibiotics and Antibiotic Resistance, a Cross-Sectional Study" Antibiotics 11, no. 7: 882. https://doi.org/10.3390/antibiotics11070882
APA StyleRostkowska, O. M., Raczkiewicz, D., Knap-Wielgus, W., & Zgliczyński, W. S. (2022). Polish Medical Doctors’ Opinions on Available Resources and Information Campaigns concerning Antibiotics and Antibiotic Resistance, a Cross-Sectional Study. Antibiotics, 11(7), 882. https://doi.org/10.3390/antibiotics11070882







