Prevalence and Predictors of Antibiotic Prescriptions at Primary Healthcare Facilities in the Dodoma Region, Central Tanzania: A Retrospective, Cross-Sectional Study
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design, Sites and Settings
2.2. Data Sources and Study Population
2.3. Sample Size Calculation
2.4. Sampling Technique
2.5. Data Collection
2.6. Inclusion and Exclusion Criteria
2.7. Data Analysis
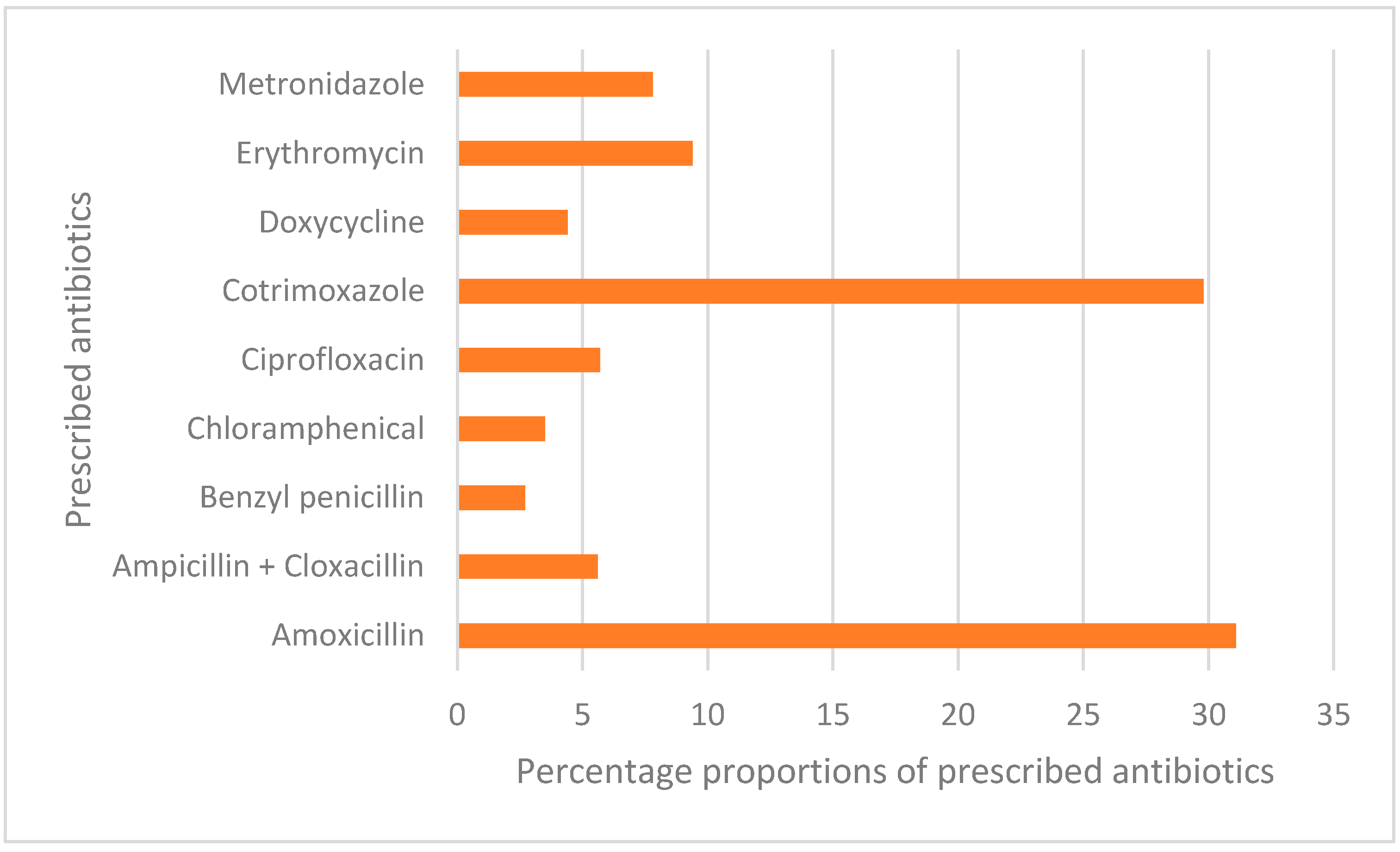
3. Results
3.1. Patient and Prescriber Characteristics
3.2. Stratification of Social, Demographic and Clinical Predictors for Antibiotic Prescription Status
3.3. Binary Logistic Regression Analysis of Antibiotic Prescriptions by Social, Demographic and Clinical Predictors
3.3.1. Univariate Logistic Regression Analysis
3.3.2. Multivariate Logistic Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Antimicrobial Resistance. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance (accessed on 20 July 2021).
- WHO. Global Antimicrobial Resistance Surveillance System (GLASS) Report. 2018. Available online: https://reliefweb.int/report/world/global-antimicrobial-resistance-surveillance-system-glass-report-early-implementation (accessed on 18 March 2021).
- O’Connor, R.; O’Doherty, J.; O’Regan, A.; Dunne, C. Antibiotic use for acute respiratory tract infections (ARTI) in primary care; what factors affect prescribing and why is it important? A narrative review. Ir. J. Med. Sci. 2018, 187, 969–986. [Google Scholar] [CrossRef] [PubMed]
- Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- WHO. New Report Calls for Urgent Action to Avert Antimicrobial Resistance Crisis. 2019. Available online: https://www.who.int/news/item/29-04-2019-new-report-calls-for-urgent-action-to-avert-antimicrobial-resistance-crisis (accessed on 12 January 2021).
- WHO. WHO Report on Surveillance of Antibiotic Consumption. 2018. Available online: https://www.who.int/publications/i/item/who-report-on-surveillance-of-antibiotic-consumption (accessed on 9 May 2019).
- Ntizala, A.; Mulume, T.; Runyeruka, B.; Sadiki, A. Antibiotic dispensing practices in community pharmacies: A major health concern in the eastern democratic republic of Congo. J. Pharm. Res. Int. 2020, 32, 33–44. [Google Scholar] [CrossRef]
- Founou, R.C.; Founou, L.L.; Essack, S.Y. Clinical and economic impact of antibiotic resistance in developing countries: A systematic review and meta-analysis. PLoS ONE 2017, 12, 1–18. [Google Scholar] [CrossRef] [PubMed]
- MoHCDEC. National Health Policy. Dar es Salaam: Ministry of Health. 2003. Available online: https://www.healthresearchweb.org/files/Tanzania National Health Policy 2003.pdf (accessed on 19 August 2021).
- Emgård, M.; Mwangi, R.; Mayo, C.; Mshana, E.; Nkini, G.; Andersson, R.; Msuya, E.; Lepp, M.; Muro, F.; Skovbjerg, S. Tanzanian primary healthcare workers’ experiences of antibiotic prescription and understanding of antibiotic resistance in common childhood infections: A qualitative phenomenographic study. Antimicrob. Resist. Infect. Control. 2021, 10, 1–15. [Google Scholar] [CrossRef]
- Irunde, H.; Minzi, O.; Moshiro, C. Assessment of rational medicines prescribing in healthcare facilities in four regions of Tanzania. J. Pharm. Pr. Community Med. 2017, 3, 225–231. [Google Scholar] [CrossRef]
- Khalfan, M.A.; Sasi, P.G.; Mugusi, S.F. The prevalence and pattern of antibiotic prescription among insured patients in Dar es Salaam Tanzania. Pan Afr. Med. J. 2021, 40, 140. [Google Scholar] [CrossRef]
- MoHCGEC. National Action Plan on Antimicrobial Resistance 2017–2022 (Issue April). 2017. Available online: https://www.flemingfund.org/wp-content/uploads/8b8fc897c422e11504c8c2ba126fac02.pdf (accessed on 28 May 2022).
- Frumence, G.; Mboera, L.; Sindato, C.; Katale, B.; Kimera, S.; Metta, E.; Durrance-Bagale, A.; Jung, A.-S.; Mshana, S.; Clark, T.; et al. The governance and implementation of the national action plan on antimicrobial resistance in Tanzania: A qualitative study. Antibiotics 2021, 10, 273. [Google Scholar] [CrossRef]
- Aboud, S.; Mdegela, R. Antibiotic Use and Resistance in Tanzania: Situation Analysis and Recommendantions. 2015. Available online: https://cddep.org/wp-content/uploads/2017/06/garp-tz_situation_analysis-1.pdf (accessed on 27 May 2021).
- NBS. The United Republic of Tanzania Dodoma Region Basic Demographic and Socio-Economic Profile 2012 Population and Housing Census. Dodoma. 2016. Available online: www.nbs.go.tz. (accessed on 11 April 2022).
- WHO. How to Investigate Drug Use in Health Facilities: Selected Drug Use Indicators. 1993. Available online: http://apps.who.int/medicinedocs/en/d/Js2289e/4.2.html (accessed on 21 January 2021).
- MoHCDEC. Standard Treatment Guideline and National Essential Medicines list, MoHCDEC. 2019. Available online: File https://hssrc.tamisemi.go.tz/storage/app/uploads/public/5ab/e9b/b21/5abe9bb216267130384889.pdf (accessed on 15 April 2021).
- Kothari, C.R. Research Methodology: Methods and Techniques; New Age International: New Delhi, India, 2004. [Google Scholar]
- Austin, P.C.; Steyerberg, E.W. The number of subjects per variable required in linear regression analyses. J. Clin. Epidemiol. 2015, 68, 627–636. [Google Scholar] [CrossRef]
- Burmeister, E.; Aitken, L.M. Sample size: How many is enough? Aust. Crit. Care 2012, 25, 271–274. [Google Scholar] [CrossRef]
- Worku, F.; Tewahido, D. Retrospective assessment of antibiotics prescribing at public primary healthcare facilities in addis ababa, Ethiopia. Interdiscip. Perspect. Infect. Dis. 2018, 2018, 1–9. [Google Scholar] [CrossRef]
- Chem, E.D.; Anong, D.N.; Akoachere, J.K.T. Prescribing patterns and associated factors of antibiotic prescription in primary health care facilities of Kumbo East and Kumbo West health districts, North West Cameroon. PLoS ONE 2018, 13, e0193353. [Google Scholar] [CrossRef]
- Sulis, G.; Adam, P.; Nafade, V.; Gore, G.; Daniels, B.; Daftary, A.; Das, J.; Gandra, S.; Pai, M. Antibiotic prescription practices in primary care in low- and middle-income countries: A systematic review and meta-analysis. PLoS Med. 2020, 17, e1003139. [Google Scholar] [CrossRef]
- Wiedenmayer, K.; Ombaka, E.; Kabudi, B.; Canavan, R.; Rajkumar, S.; Chilunda, F.; Sungi, S.; Stoermer, M. Adherence to standard treatment guidelines among prescribers in primary healthcare facilities in the Dodoma region of Tanzania. BMC Health Serv. Res. 2021, 21, 1–10. [Google Scholar] [CrossRef]
- Gwimile, J.J.; Shekalaghe, S.A.; Kapanda, G.N.; Kisanga, E.R. Antibiotic prescribing practice in management of cough and/or diarrhoea in Moshi municipality, Northern Tanzania: Cross-sectional descriptive study. Pan Afr. Med. J. 2012, 12, 103. [Google Scholar]
- Kamuhabwa, A.A.R.; Kisoma, S. Factors influencing prescribing practices of medical practitioners in public and private health facilities in dar es salaam, Tanzania. Trop. J. Pharm. Res. 2015, 14, 2107–2113. [Google Scholar] [CrossRef][Green Version]
- Kagashe, G.A.B.; Minzi, O.; Matowe, L. An assessment of dispensing practices in private pharmacies in Dar-es Salaam, Tanzania. Int. J. Pharm. Pract. 2011, 19, 30–35. [Google Scholar] [CrossRef]
- Kutyabami, P.; Munanura, E.I.; Kalidi, R.; Balikuna, S.; Ndagire, M.; Kaggwa, B.; Nambatya, W.; Kamba, P.F.; Musiimenta, A.; Kesi, D.N.; et al. Evaluation of the clinical use of ceftriaxone among in-patients in selected health facilities in Uganda. Antibiotics 2021, 10, 779. [Google Scholar] [CrossRef]
- Marangu, D.; Zar, H.J. Childhood pneumonia in low-and-middle-income countries: An update. Paediatr. Respir. Rev. 2019, 32, 3–9. [Google Scholar] [CrossRef]
- Haynes, D.; Lasarev, M.; Keller, J. Systemic antibiotic use for nonbacterial dermatological conditions among referring providers. Int. J. Dermatol. 2018, 57, 566–571. [Google Scholar] [CrossRef]
- Heal, C.; Gorges, H.; Van Driel, M.L.; Tapley, A.; Davis, J.; Davey, A.; Holliday, L.; Ball, J.; Najib, N.; Spike, N.; et al. Antibiotic stewardship in skin infections: A cross-sectional analysis of early-career GP’s management of impetigo. BMJ Open 2019, 9, e031527. [Google Scholar] [CrossRef]
- Mate, V.H.; Gonarkar, S.B.; Dhamani, A. Drug utilization for common skin diseases: An outpatient based study. Int. J. Basic Clin. Pharmacol. 2019, 8, 2604. [Google Scholar] [CrossRef]
- Hees, C.V.; Naafs, B. Common Skin Diseases in Africa an Illustrated Guide. 2017. Available online: https://plan-g.at/images/pdf/Common_skin_diseases_in_Africa_ver2017.pdf (accessed on 13 June 2021).
- Alkaff, R.N.; Kamigaki, T.; Saito, M.; Ariyanti, F.; Iriani, D.U.; Oshitani, H. Use of antibiotics for common illnesses among children aged under 5 years in a rural community in Indonesia: A cross-sectional study. Trop. Med. Health 2019, 47, 45. [Google Scholar] [CrossRef]
- Xue, F.; Xu, B.; Shen, A.; Shen, K. Antibiotic prescriptions for children younger than 5 years with acute upper respiratory infections in China: A retrospective nationwide claims database study. BMC Infect. Dis. 2021, 21, 339. [Google Scholar] [CrossRef]
- Havers, F.P.; Hicks, L.A.; Chung, J.R.; Gaglani, M.; Murthy, K.; Zimmerman, R.K.; Jackson, L.A.; Petrie, J.G.; McLean, H.Q.; Nowalk, M.P.; et al. Outpatient antibiotic prescribing for acute respiratory infections during influenza seasons. JAMA Netw. Open 2018, 1, e180243. [Google Scholar] [CrossRef]

| Variable | Frequency | Percentage |
|---|---|---|
| Age of patients | ||
| <5 | 474 | 46.43 |
| 5–18 | 140 | 13.71 |
| 19–35 | 175 | 17.14 |
| 36–45 | 60 | 5.88 |
| 46–55 | 39 | 3.82 |
| 56+ | 133 | 13.03 |
| District | ||
| Chemba | 390 | 38.20 |
| Dodoma | 631 | 61.80 |
| Ownership | ||
| Private | 60 | 5.88 |
| Government | 961 | 94.12 |
| Prescribers’ education | ||
| Certificate | 6 | 0.59 |
| Diploma | 966 | 94.61 |
| Degree | 49 | 4.80 |
| Type of health facility | ||
| Dispensary | 748 | 73.26 |
| Health centre | 273 | 26.74 |
| Sex | ||
| Male | 464 | 45.45 |
| Female | 557 | 54.55 |
| Variable | Non-Antibiotics (N = 242) | Antibiotics (N = 779) | X2 | p Value |
|---|---|---|---|---|
| N (%) | N (%) | |||
| Age | 7.1384 | 0.2105 | ||
| <5 | 124 (26.16) | 350 (73.84) | ||
| 5–18 | 38 (27.14) | 102 (72.86) | ||
| 19–35 | 37 (21.14) | 138 (78.86) | ||
| 36–45 | 10 (16.67) | 50 (83.33) | ||
| 46–55 | 9 (23.08) | 30 (76.92) | ||
| 56+ | 24 (18.05) | 109 (81.95) | ||
| District | 1.6815 | 0.1947 | ||
| Chemba | 101 (25.90) | 289 (74.10) | ||
| Dodoma | 141 (22.35) | 490 (77.65) | ||
| Ownership | 0.7560 | 0.3846 | ||
| Private | 17 (28.33) | 43 (71.67) | ||
| Government | 225 (23.41) | 736 (76.59) | ||
| Level of prescriber education | 5.4522 | 0.0195 | ||
| Degree | 19 (37.25) | 32 (62.75) | ||
| Diploma | 223 (22.99) | 747 (77.01) | ||
| Type of health facility | 0.6126 | 0.4338 | ||
| Dispensary | 182 (24.33) | 566 (75.67) | ||
| Health centre | 60 (21.98) | 213 (78.02) | ||
| Sex | 4.2948 | 0.0382 | ||
| Male | 118 (21.18) | 439 (78.82) | ||
| Female | 124 (26.72) | 340 (73.28) | ||
| Dermatological conditions | 14.5453 | 0.0001 | ||
| No | 220 (22.59) | 754 (77.41) | ||
| Yes | 22 (46.81) | 25 (53.19) | ||
| Diarrhoea | 0.3927 | 0.5309 | ||
| No | 221 (23.46) | 721 (76.54) | ||
| Yes | 21 (26.58) | 58 (73.42) | ||
| Malaria | 16.8512 | <.0001 | ||
| No | 215 (22.35) | 747 (77.65) | ||
| Yes | 27 (45.76) | 32 (54.24) | ||
| Other diseases | 6.4661 | 0.0110 | ||
| No | 134 (21.07) | 502 (78.93) | ||
| Yes | 108 (28.05) | 277 (71.95) | ||
| Pneumonia | 14.0314 | 0.0002 | ||
| No | 241 (24.85) | 729 (75.15) | ||
| Yes | 1 (1.96) | 50 (98.04) | ||
| PID | 0.0101 | |||
| No | 235 (23.29) | 774 (76.71) | ||
| Yes | 7 (58.33) | 5 (41.67) | ||
| URTI | 3.7990 | 0.0513 | ||
| No | 212 (24.85) | 641 (75.15) | ||
| Yes | 30 (17.86) | 138 (82.14) | ||
| UTI | 43.8463 | <0.0001 | ||
| No | 242 (26.98) | 655 (73.02) | ||
| Yes | 0 (0.00) | 124 (100.00) |
| Variable | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| cOR [95% CI] | p Value | aOR [95% CI] | p Value | |
| District | ||||
| Chemba | Ref | Ref | ||
| Dodoma | 1.215 [0.905, 1.630] | 0.1951 | 1.142 [0.832, 1.568] | 0.4121 |
| Sex | ||||
| Male | Ref | Ref | ||
| Female | 0.726 [0.552, 0.984] | 0.0376 | 0.768 [0.566, 1.028] | 0.0872 |
| Prescriber education | ||||
| Degree | Ref | Ref | ||
| Diploma | 1.989 [1.106, 3.577] | 0.0217 | 2.511 [1.343, 4.692] | 0.0039 |
| URTI | ||||
| No | Ref | Ref | ||
| Yes | 1.913 [1.354, 2.701] | 0.0002 | 1.709 [1.129, 2.587] | 0.0113 |
| Pneumonia | ||||
| No | Ref | Ref | ||
| Yes | 16.678 [2.271, 120.270] | 0.0055 | 15.918 [2.150, 117.973] | 0.0056 |
| Malaria | ||||
| No | Ref | Ref | ||
| Yes | 0.340 [0.200, 0.582] | <0.0001 | 0.293 [0.160, 0.504] | <.0001 |
| Dermatological conditions | ||||
| No | Ref | Ref | ||
| Yes | 0.341 [0.193, 0.600] | 0.0003 | 0.321 [0.184, 0.631] | 0.0008 |
| Other diseases | ||||
| No | Ref | Ref | ||
| Yes | 0.686 [0.511, 0.908] | 0.0112 | 0.744 [0.510, 1.074] | 0.1190 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mabilika, R.J.; Shirima, G.; Mpolya, E. Prevalence and Predictors of Antibiotic Prescriptions at Primary Healthcare Facilities in the Dodoma Region, Central Tanzania: A Retrospective, Cross-Sectional Study. Antibiotics 2022, 11, 1035. https://doi.org/10.3390/antibiotics11081035
Mabilika RJ, Shirima G, Mpolya E. Prevalence and Predictors of Antibiotic Prescriptions at Primary Healthcare Facilities in the Dodoma Region, Central Tanzania: A Retrospective, Cross-Sectional Study. Antibiotics. 2022; 11(8):1035. https://doi.org/10.3390/antibiotics11081035
Chicago/Turabian StyleMabilika, Richard James, Gabriel Shirima, and Emmanuel Mpolya. 2022. "Prevalence and Predictors of Antibiotic Prescriptions at Primary Healthcare Facilities in the Dodoma Region, Central Tanzania: A Retrospective, Cross-Sectional Study" Antibiotics 11, no. 8: 1035. https://doi.org/10.3390/antibiotics11081035
APA StyleMabilika, R. J., Shirima, G., & Mpolya, E. (2022). Prevalence and Predictors of Antibiotic Prescriptions at Primary Healthcare Facilities in the Dodoma Region, Central Tanzania: A Retrospective, Cross-Sectional Study. Antibiotics, 11(8), 1035. https://doi.org/10.3390/antibiotics11081035






