Incidence and Determinants of Piperacillin/Tazobactam-Associated Hypokalemia: A Retrospective Study
Abstract
:1. Introduction
2. Results
2.1. Demographic and Clinical Characteristics of Patients
2.2. Incidence and Severity of Hypokalemia
2.3. Risk Factors of Hypokalemia
2.4. Other Outcomes
3. Discussion
4. Materials and Methods
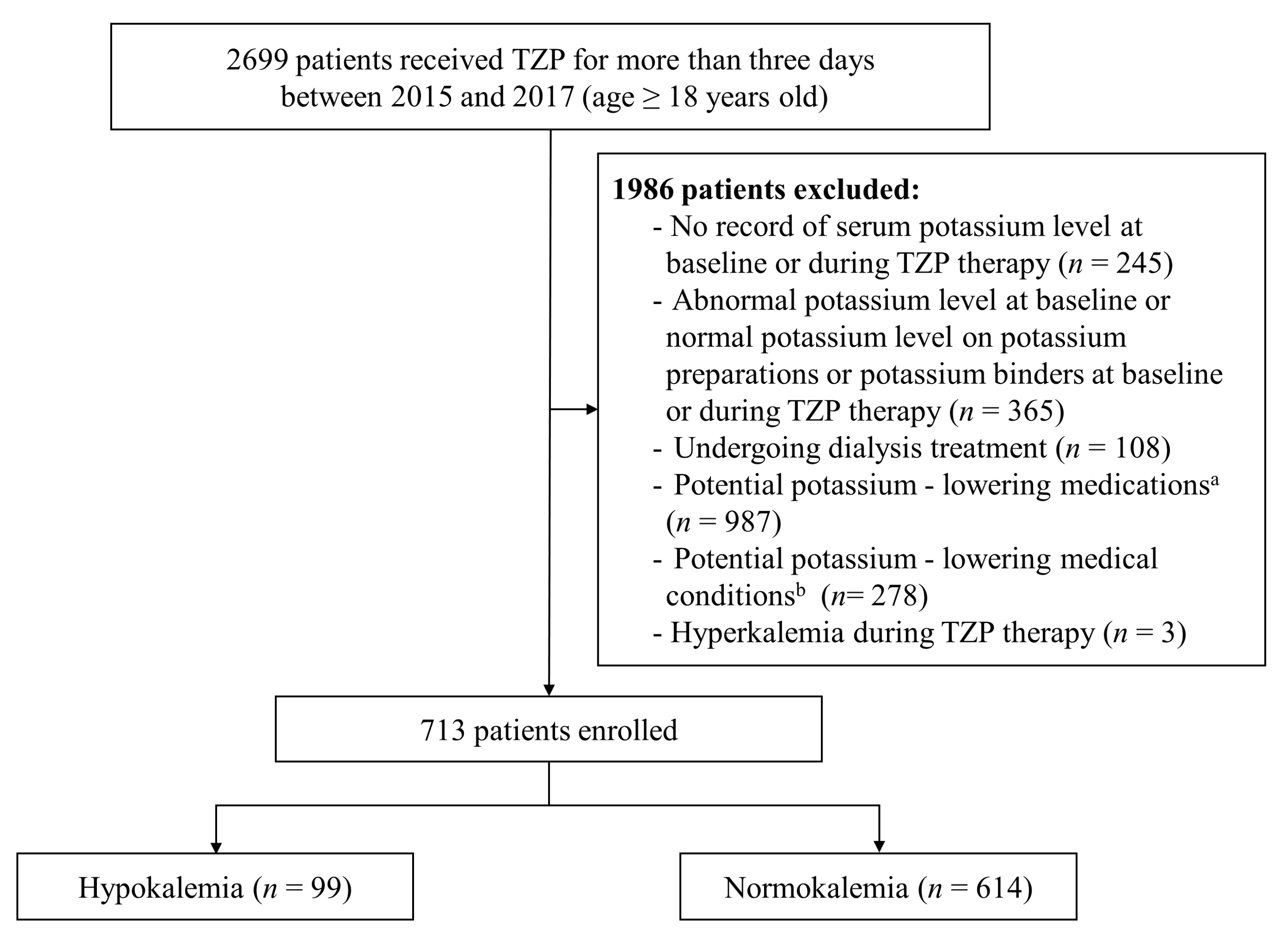
4.1. Study Design and Population
4.2. Variables and Definitions
4.3. Clinical Outcomes
4.4. Statistical Analyses
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Weiner, I.D.; Wingo, C.S. Hypokalemia––consequences, causes, and correction. J. Am. Soc. Nephrol. 1997, 8, 1179–1188. [Google Scholar] [CrossRef] [PubMed]
- Kardalas, E.; Paschou, S.A.; Anagnostis, P.; Muscogiuri, G.; Siasos, G.; Vryonidou, A. Hypokalemia: A clinical update. Endocr. Connect. 2018, 7, R135–R146. [Google Scholar] [CrossRef] [PubMed]
- Gennari, F.J. Hypokalemia. N. Engl. J. Med. 1998, 339, 451–458. [Google Scholar] [CrossRef] [PubMed]
- Hoskote, S.S.; Joshi, S.R.; Ghosh, A.K. Disorders of potassium homeostasis: Pathophysiology and management. J. Assoc. Phys. India 2008, 56, 685–693. [Google Scholar]
- Ahmed, A.; Zannad, F.; Love, T.E.; Tallaj, J.; Gheorghiade, M.; Ekundayo, O.J.; Pitt, B. A propensity–matched study of the association of low serum potassium levels and mortality in chronic heart failure. Eur. Heart. J. 2007, 28, 1334–1343. [Google Scholar] [CrossRef] [Green Version]
- Krogager, M.L.; Eggers-Kaas, L.; Aasbjerg, K.; Mortensen, R.N.; Køber, L.; Gislason, G.; Torp-Pedersen, C.; Søgaard, P. Short–term mortality risk of serum potassium levels in acute heart failure following myocardial infarction. Eur. Heart J. Cardiovasc. Pharmacother. 2015, 1, 245–251. [Google Scholar] [CrossRef] [Green Version]
- Luo, J.; Brunelli, S.M.; Jensen, D.E.; Yang, A. Association between serum potassium and outcomes in patients with reduced kidney function. Clin. J. Am. Soc. Nephrol. 2016, 11, 90–100. [Google Scholar] [CrossRef] [Green Version]
- Collins, A.J.; Pitt, B.; Reaven, N.; Funk, S.; McGaughey, K.; Wilson, D.; Bushinsky, D.A. Association of serum potassium with all–cause mortality in patients with and without heart failure, chronic kidney disease, and/or diabetes. Am. J. Nephrol. 2017, 46, 213–221. [Google Scholar] [CrossRef]
- Smith, N.L.; Lemaitre, R.N.; Heckbert, S.R.; Kaplan, R.C.; Tirschwell, D.L.; Longstreth, W.T.; Psaty, B.M. Serum potassium and stroke risk among treated hypertensive adults. Am. J. Hypertens. 2003, 16, 806–813. [Google Scholar] [CrossRef] [Green Version]
- Mattsson, N.; Kumarathurai, P.; Larsen, B.S.; Nielsen, O.W.; Sajadieh, A. Mild hypokalemia and supraventricular ectopy increases the risk of stroke in community–dwelling wubjects. Stroke 2017, 48, 537–543. [Google Scholar] [CrossRef]
- Kieneker, L.M.; Eisenga, M.F.; Joosten, M.M.; de Boer, R.A.; Gansevoort, R.T.; Kootstra-Ros, J.E.; Navis, G.; Bakker, S.J. Plasma potassium, diuretic use and risk of developing chronic kidney disease in a predominantly White population. PLoS ONE 2017, 12, e0174686. [Google Scholar] [CrossRef]
- Perry, C.M.; Markham, A. Piperacillin/tazobactam: An updated review of its use in the treatment of bacterial infections. Drugs 1999, 57, 805–843. [Google Scholar] [CrossRef]
- Kuye, O.; Teal, J.; DeVries, V.G.; Morrow, C.A.; Tally, F.P. Safety profile of piperacillin/tazobactam in phase I and III clinical studies. J. Antimicrob. Chemother. 1993, 31 (Suppl. A), 113–124. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. Drug Approval Package: Zosyn (Piperacillin & Tazobactam). Available online: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2005/050684_S045_050750_s012_ZosynTOC.cfm (accessed on 10 July 2022).
- Tamma, P.D.; Rodriguez-Bano, J. The use of noncarbapenem β–lactams for the treatment of extended–spectrum β–lactamase infections. Clin. Infect. Dis. 2017, 64, 972–980. [Google Scholar] [CrossRef] [Green Version]
- Kaye, K.S.; Bhowmick, T.; Metallidis, S.; Bleasdale, S.C.; Sagan, O.S.; Stus, V.; Vazquez, J.; Zaitsev, V.; Bidair, M.; Chorvat, E.; et al. Effect of meropenem–vaborbactam vs piperacillin–tazobactam on clinical cure or improvement and microbial eradication in complicated urinary tract infection: The TANGO I randomized clinical trial. JAMA 2018, 319, 788–799. [Google Scholar] [CrossRef]
- Kaye, K.S.; Rice, L.B.; Dane, A.L.; Stus, V.; Sagan, O.; Fedosiuk, E.; Das, A.F.; Skarinsky, D.; Eckburg, P.B.; Ellis-Grosse, E.J. Fosfomycin for injection (ZTI-01) versus piperacillin-tazobactam for the treatment of complicated urinary tract infection including acute pyelonephritis: ZEUS, a Phase 2/3 randomized trial. Clin. Infect. Dis. 2019, 69, 2045–2056. [Google Scholar] [CrossRef] [Green Version]
- Kuramoto, H.; Masago, S.; Kashiwagi, Y.; Maeda, M. Incidence and risk factors of hypokalemia in tazobactam/piperacillin–administered patients. Yakugaku Zasshi 2019, 139, 1591–1600. [Google Scholar] [CrossRef] [Green Version]
- Hussain, S.; Syed, S.; Baloch, K. Electrolytes imbalance: A rare side effect of piperacillin/ tazobactam therapy. J. Coll. Phys. Surg. Pak. 2010, 20, 419–420. [Google Scholar]
- Zaki, S.A.; Lad, V. Piperacillin–tazobactam–induced hypokalemia and metabolic alkalosis. Indian J. Pharmacol. 2011, 43, 609–610. [Google Scholar] [CrossRef] [Green Version]
- Kutluturk, F.; Uzun, S.; Tasliyurt, T.; Sahin, S.; Barut, S.; Ozturk, B.; Yilmaz, A. A rare complication of antibiotic (piperacillin/tazobactam) therapy: Resistant hypokalemia. J. Med. Cases 2012, 3, 355–357. [Google Scholar] [CrossRef] [Green Version]
- Kunder, S.K.; Chogtu, B.; Avinash, A.; Pathak, A.; Patil, N.; Adiga, S. A case series of piperacillin–tazobactam induced hypokalemia in a tertiary care hospital in South India. Online J. Health Allied Sci. 2015, 14, 17. [Google Scholar]
- Kumar, V.; Khosla, S.; Stancu, M. Torsade de Pointes induced by hypokalemia from imipenem and piperacillin. Case Rep. Cardiol. 2017, 2017, 4565182. [Google Scholar] [CrossRef] [PubMed]
- Pandya, A.D.; Gupta, S.; Malhotra, S.D.; Patel, P. Piperacillin-tazobactam induced hypokalaemia. Int. J. Basic Clin. Pharmacol. 2018, 7, 2459–2461. [Google Scholar] [CrossRef]
- Tai, C.C.; Chou, R.Y.; Guo, J.Y.; Chen, H.P. Severe acute hypokalaemia associated with piperacillin/tazobactam in an HIV–infected patient under antiretroviral therapy with tenofovir alafenamide: Case report and literature review. Sex. Health 2020, 17, 194–197. [Google Scholar] [CrossRef]
- van der Heijden, C.; Duizer, M.L.; Fleuren, H.; Veldman, B.A.; Sprong, T.; Dofferhoff, A.; Kramers, C. Intravenous flucloxacillin treatment is associated with a high incidence of hypokalaemia. Br. J. Clin. Pharmacol. 2019, 85, 2886–2890. [Google Scholar] [CrossRef]
- Kleinfeld, M.; Borra, S.; Gavani, S.; Corcoran, A. Hypokalemia: Are elderly females more vulnerable? J. Natl. Med. Assoc. 1993, 85, 861–864. [Google Scholar]
- Paice, B.J.; Paterson, K.R.; Onyanga-Omara, F.; Donnelly, T.; Gray, J.M.; Lawson, D.H. Record linkage study of hypokalaemia in hospitalized patients. Postgrad. Med. J. 1986, 62, 187–191. [Google Scholar] [CrossRef] [Green Version]
- Fukui, S.; Otani, N.; Katoh, H.; Tsuzuki, N.; Ishihara, S.; Ohnuki, A.; Miyazawa, T.; Nawashiro, H.; Shima, K. Female gender as a risk factor for hypokalemia and QT prolongation after subarachnoid hemorrhage. Neurology 2002, 59, 134–136. [Google Scholar] [CrossRef]
- Rundo, J.; Sagild, U. Total and exchangeable potassium in humans. Nature 1955, 175, 774. [Google Scholar] [CrossRef]
- Gerçek, A.; Umuroğlu, T.; İnci, F.; Göğüs, Y. The etiology and incidence of hypokalemia in intensive care unit. Marmara Med. J. 2003, 16, 32–35. [Google Scholar]
- Brunner, F.P.; Frick, P.G. Hypokalaemia, metabolic alkalosis, and hypernatraemia due to “massive” sodium penicillin therapy. Br. Med. J. 1968, 4, 550–552. [Google Scholar] [CrossRef] [Green Version]
- Viehman, J.A.; Oleksiuk, L.M.; Sheridan, K.R.; Byers, K.E.; He, P.; Falcione, B.A.; Shields, R.K. Adverse events lead to drug discontinuation more commonly among patients who receive nafcillin than among those who receive oxacillin. Antimicrob. Agents Chemother. 2016, 60, 3090–3095. [Google Scholar] [CrossRef] [Green Version]
- Gennari, F.J. Disorders of potassium homeostasis. Hypokalemia and hyperkalemia. Crit. Care Clin. 2002, 18, 273–288. [Google Scholar] [CrossRef]
- Liamis, G.; Filippatos, T.D.; Elisaf, M.S. Electrolyte disorders associated with the use of anticancer drugs. Eur. J. Pharmacol. 2016, 777, 78–87. [Google Scholar] [CrossRef]
- Perazella, M.A. Drug-induced hyperkalemia: Old culprits and new offenders. Am. J. Med. 2000, 109, 307–314. [Google Scholar] [CrossRef]
| Variable | Total | Hypokalemia | Normokalemia | p Value |
|---|---|---|---|---|
| n = 713 | n = 99 | n = 614 | ||
| Age (years) | 67 (56–77) | 74 (61.5–79.0) | 66 (56–76) | <0.001 |
| Female sex | 245 (34.4) | 46 (46.5) | 199 (32.4) | 0.006 |
| ICU residence | 42 (5.9) | 5 (5.1) | 37 (6.0) | 0.702 |
| Serum potassium (mEq/L) | 4.2 (3.9–4.5) | 3.9 (3.7–4.1) | 4.2 (4.0–4.5) | <0.001 |
| Serum creatinine (mEq/L) | 0.7 (0.5–0.9) | 0.7 (0.5–0.9) | 0.7 (0.5–0.9) | 0.707 |
| Serum magnesium (mEq/L) | 2.0 (1.9–2.2) | 1.9 (1.8–2.1) | 2.0 (1.9–2.2) | 0.493 |
| ALB (g/L) | 3.2 (2.9–3.6) | 3.1 (2.8–3.6) | 3.2 (2.9–3.7) | 0.675 |
| AST (IU/L) | 27 (18–44) | 34 (18.8–53.5) | 26 (17–43) | 0.511 |
| ALT (IU/L) | 22 (18–38) | 21 (11–38) | 22 (15–38) | 0.885 |
| Duration of TZP therapy (days) | 7 (5–11) | 8 (5.5–13.0) | 7 (5–11) | 0.008 |
| TZP daily dose (g) | 14.3 (12.8–16.9) | 15.8 (13.5–17.2) | 13.5 (12.7–16.8) | 0.019 |
| BW (kg) | 58 (50–66) | 56 (50–64) | 58.3 (50.2–66.1) | 0.115 |
| BMI (kg/m2) | 21.9 (19.6–24.5) | 22.2 (19.7–24.2) | 21.9 (19.6–24.6) | 0.824 |
| Indication for TZP treatment | ||||
| Pneumonia | 266 (37.3) | 29 (29.3) | 237 (38.6) | 0.076 |
| Intra–abdominal infection | 197 (27.6) | 35 (35.4) | 162 (26.4) | 0.064 |
| Urinary tract infection | 76 (10.7) | 12 (12.1) | 64 (10.4) | 0.611 |
| Neutropenic fever | 42 (5.9) | 5 (5.1) | 37 (6.0) | 0.702 |
| Bacteremia/Sepsis | 38 (5.3) | 8 (8.1) | 30 (4.9) | 0.189 |
| Skin and soft tissue infection | 38 (5.3) | 7 (7.1) | 31 (5.1) | 0.406 |
| Others | 81 (11.4) | 8 (8.1) | 73 (11.9) | 0.268 |
| Drugs that may increase serum potassium | ||||
| NSAIDs | 189 (26.5) | 32 (32.3) | 157 (25.6) | 0.158 |
| ARBs | 104 (14.6) | 18 (18.2) | 86 (14.0) | 0.275 |
| β blockers | 28 (3.9) | 2 (2.0) | 26 (4.2) | 0.293 |
| Potassium-sparing diuretics | 24 (3.4) | 1 (1.0) | 23 (3.8) | 0.161 |
| ACEIs | 16 (2.2) | 2 (2.0) | 14 (2.3) | 0.909 |
| Sulfamethoxazole/trimethoprim | 14 (2.0) | 1 (1.0) | 13 (2.1) | 0.461 |
| Digoxin | 12 (1.7) | 2 (2.0) | 10 (1.6) | 0.779 |
| Variable | Univariate Analysis | Multivariate Analysis a | ||
|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Age (year) | 1.03 (1.01–1.05) | 0.001 | 1.03 (1.02–1.05) | <0.001 |
| Female sex | 1.81 (1.18–2.78) | 0.007 | 1.88 (1.18–3.00) | 0.008 |
| ICU residence | 0.83 (0.32–2.16) | 0.702 | ||
| Serum potassium (mEq/L) | 0.15 (0.08–0.27) | <0.001 | 0.13 (0.07–0.26) | <0.001 |
| Serum creatinine (mEq/L) | 1.05 (0.64–1.71) | 0.850 | ||
| Serum magnesium (mEq/L) | 0.32 (0.02–7.05) | 0.471 | ||
| ALB (g/L) | 1.00 (0.61–1.65) | 0.998 | ||
| AST (IU/L) | 1.00 (0.99–1.00) | 0.930 | ||
| ALT (IU/L) | 1.00 (0.99–1.01) | 0.943 | ||
| Duration of TZP therapy (days) | 1.07 (1.03–1.11) | <0.001 | 1.08 (1.04–1.13) | <0.001 |
| TZP daily dose (g) | 1.10 (1.01–1.20) | 0.024 | 1.10 (1.01–1.20) | 0.049 |
| Body weight (kg) | 0.99 (0.97–1.0) | 0.128 | ||
| BMI (kg/m2) | 1.01 (0.95–1.07) | 0.730 | ||
| Indication for TZP treatment | ||||
| Pneumonia | 0.66 (0.42–1.05) | 0.077 | ||
| Intra–abdominal infection | 1.53 (0.97–2.39) | 0.065 | ||
| Urinary tract infection | 1.19 (0.62–2.29) | 0.612 | ||
| Neutropenic fever | 0.83 (0.32–2.16) | 0.702 | ||
| Bacteremia/Sepsis | 1.71 (0.76–3.85) | 0.194 | ||
| Skin and soft tissue infection | 1.43 (0.61–3.35) | 0.408 | ||
| Others | 0.65 (0.30–1.40) | 0.271 | ||
| Drugs that may increase serum potassium | ||||
| NSAIDs | 1.39 (0.88–2.20) | 0.159 | ||
| ARBs | 1.36 (0.78–2.39) | 0.276 | ||
| β blockers | 0.47 (0.11–2.0) | 0.304 | ||
| Potassium-sparing diuretics | 0.26 (0.04–1.96) | 0.193 | ||
| ACEIs | 0.89 (0.11–7.27) | 0.909 | ||
| Sulfamethoxazole/trimethoprim | 0.47 (0.06–3.65) | 0.472 | ||
| Digoxin | 1.25 (0.27–5.77) | 0.779 | ||
| Characteristics | Value |
|---|---|
| Elapsed time to onset of hypokalemia (days) | 4.0 (2.5–6.0) |
| Serum potassium at the onset time of hypokalemia (mEq/L) | 3.3 (3.1–3.4) |
| Elapsed time to nadir of hypokalemia (days) | 5.0 (3.0–7.0) |
| Serum potassium at the nadir time of hypokalemia (mEq/L) | 3.2 (3.0–3.3) |
| Characteristics | Hypokalemia | Normokalemia | p Value |
|---|---|---|---|
| n = 99 | n = 614 | ||
| Difference between baseline and nadir serum potassium level | 0.7 (0.5–1.0) | 0.2 (0.0–0.5) | <0.001 a |
| Patients with ≥0.5 mEq/L decrease in serum potassium level from baseline | 82 (82.8) | 177 (28.8) | <0.001 b |
| Monitoring of serum potassium levels | 4 (3–6) | 3 (2–4) | <0.001 a |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seo, H.; Kim, E. Incidence and Determinants of Piperacillin/Tazobactam-Associated Hypokalemia: A Retrospective Study. Antibiotics 2022, 11, 1138. https://doi.org/10.3390/antibiotics11081138
Seo H, Kim E. Incidence and Determinants of Piperacillin/Tazobactam-Associated Hypokalemia: A Retrospective Study. Antibiotics. 2022; 11(8):1138. https://doi.org/10.3390/antibiotics11081138
Chicago/Turabian StyleSeo, Heenam, and Eunyoung Kim. 2022. "Incidence and Determinants of Piperacillin/Tazobactam-Associated Hypokalemia: A Retrospective Study" Antibiotics 11, no. 8: 1138. https://doi.org/10.3390/antibiotics11081138
APA StyleSeo, H., & Kim, E. (2022). Incidence and Determinants of Piperacillin/Tazobactam-Associated Hypokalemia: A Retrospective Study. Antibiotics, 11(8), 1138. https://doi.org/10.3390/antibiotics11081138






